- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Legionella pneumophila Dr.T.V.Rao MD презентация
Содержание
- 1. Legionella pneumophila Dr.T.V.Rao MD
- 2. History The bacterium got its name after
- 3. Disease Patterns Each year, between 8,000 and
- 4. Legionella pneumophila Legionella pneumophila is a
- 5. Legionella pneumophila Legionella pneumophila is a
- 6. Morphology Thin, Non capsulated Gram negative bacilli
- 8. Culturing Grown on Buffered charcoal
- 9. Bacterial spread Legionella are present in
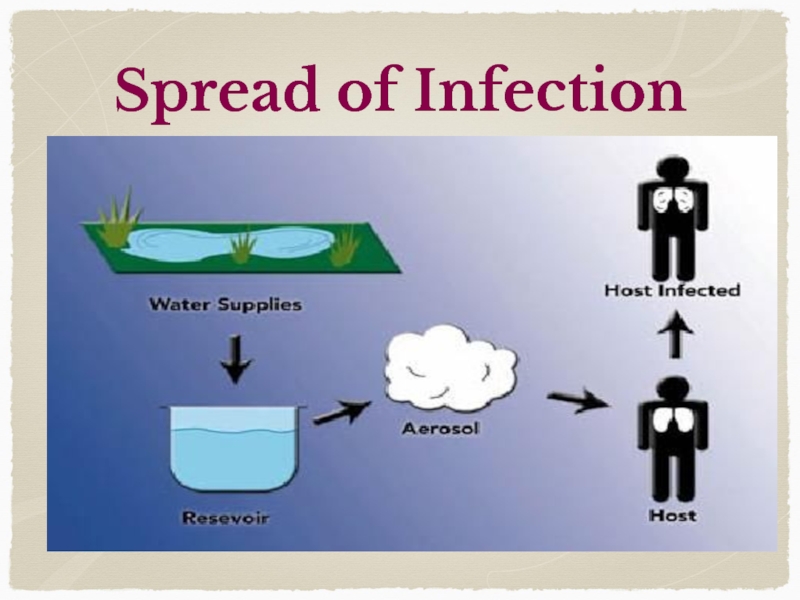
- 10. Spread of Infection
- 11. Transmission Legionella come from natural fresh water
- 12. Pathogenesis In humans, L. pneumophila invades and
- 13. Who are at Risk Most healthy individuals
- 14. Facts on Legionnaires Disease Legionella bacteria
- 15. Pathogenesis Bacteria enter through alveoli Legionella multiply inside the Monocytes and Macrophages CMI effective
- 16. Predisposing factors Smoking Alcohol Age, Hospitalization
- 17. Reservoirs of Infection L. pneumophila is
- 18. Clinically Manifest with Legionnaires Disease Epidemic
- 19. Pontiac fever Pontiac fever is a
- 21. Clinically Pontiac Fever manifests with A
- 22. Laboratory Diagnosis Specimens
- 23. Diagnosis Most people with Legionnaires' disease will
- 24. Urine Antigen Test The most commonly used
- 25. Culture If the Legionella bacteria are cultured
- 26. Blood Specimens Testing the Serum Paired
- 27. Pontiac Fever Pontiac fever can be confirmed
- 28. Detection Sera have been used both for
- 29. Treatment & Complications Treatment Legionnaires' disease requires
- 30. Treatment Respiratory fluoroquinolones and the newer macrolides
- 31. Treatment Macrolides Ciprofloxacin Tetracycline's Rifampicin
- 32. Programme Created and Designed by Dr.T.V.Rao
Слайд 2History
The bacterium got its name after a 1976 outbreak, when many
people who went to a Philadelphia convention of the American Legion suffered from this disease, a type of pneumonia (lung infection). Although this type of bacterium was around before 1976, more illness from Legionnaires' disease is being detected now.
Слайд 3Disease Patterns
Each year, between 8,000 and 18,000 people are hospitalized with
Legionnaires' disease in the U.S. However, many infections are not diagnosed or reported, so this number may be higher. More illness is usually found in the summer and early fall, but it can happen any time of year.
Слайд 4Legionella pneumophila
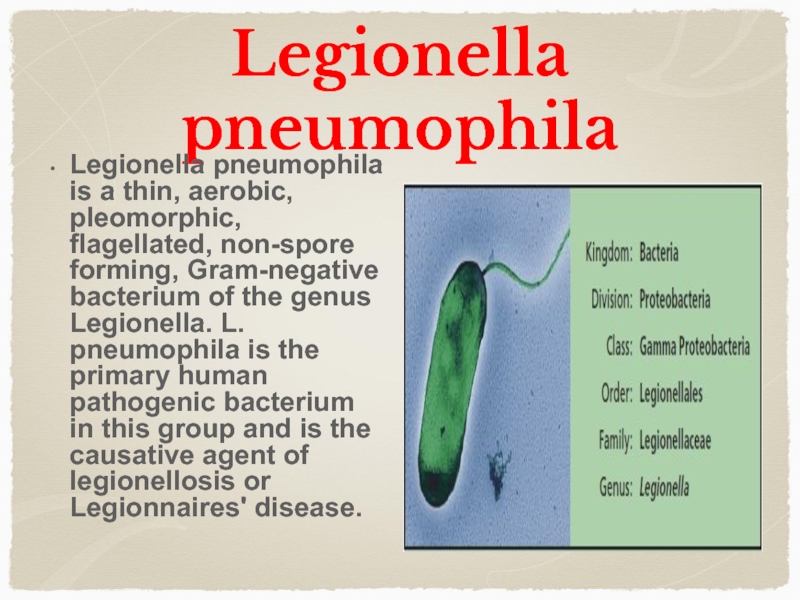
Legionella pneumophila is a thin, aerobic, pleomorphic, flagellated, non-spore
forming, Gram-negative bacterium of the genus Legionella. L. pneumophila is the primary human pathogenic bacterium in this group and is the causative agent of legionellosis or Legionnaires' disease.
Слайд 5Legionella pneumophila
Legionella pneumophila is a thin, aerobic, pleomorphic, flagellated, non-spore
forming, Gram-negative bacterium of the genus Legionella. L. pneumophila is the primary human pathogenic bacterium in this group and is the causative agent of legionellosis or Legionnaires' disease
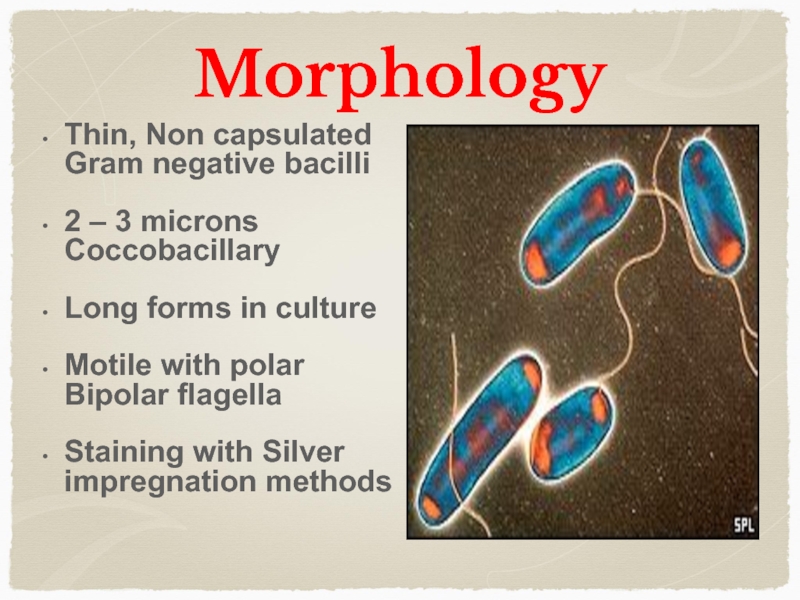
Слайд 6Morphology
Thin, Non capsulated Gram negative bacilli
2 – 3 microns Coccobacillary
Long
forms in culture
Motile with polar Bipolar flagella
Staining with Silver impregnation methods
Motile with polar Bipolar flagella
Staining with Silver impregnation methods
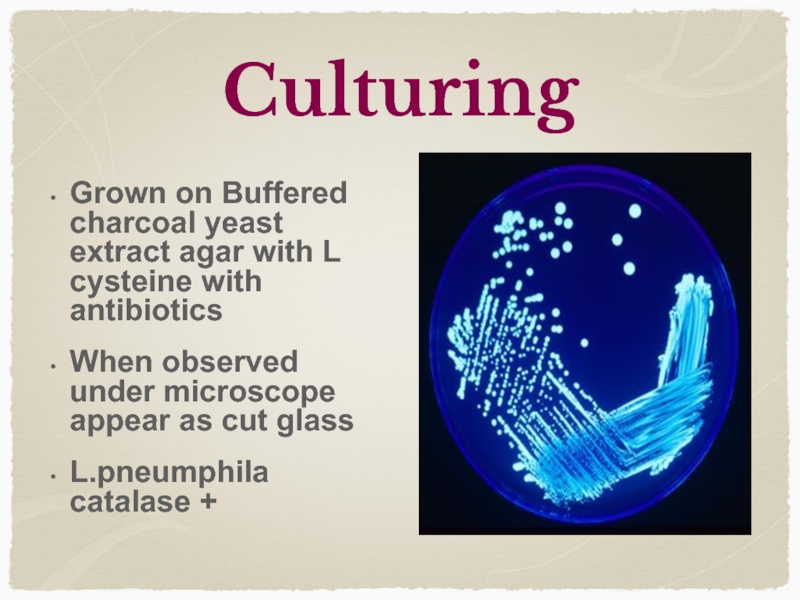
Слайд 8Culturing
Grown on Buffered charcoal yeast extract agar with L cysteine
with antibiotics
When observed under microscope appear as cut glass
L.pneumphila catalase +
When observed under microscope appear as cut glass
L.pneumphila catalase +
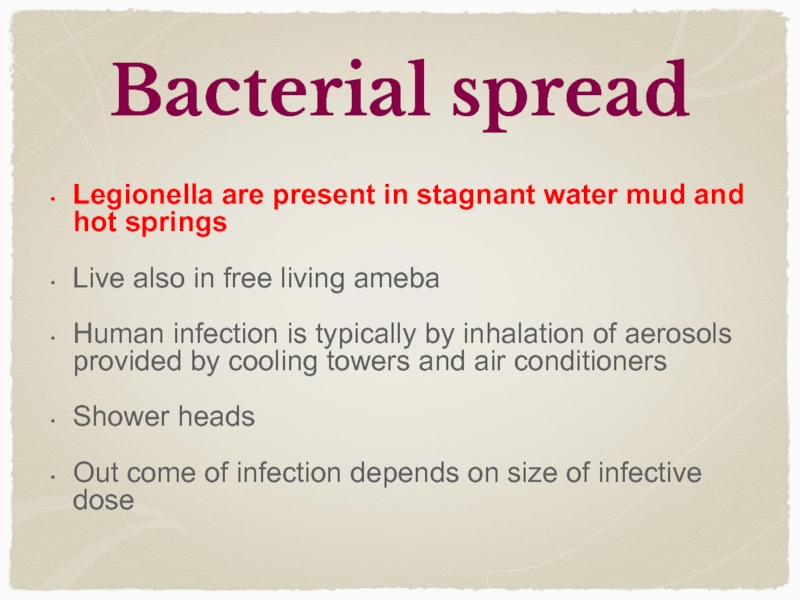
Слайд 9Bacterial spread
Legionella are present in stagnant water mud and hot springs
Live
also in free living ameba
Human infection is typically by inhalation of aerosols provided by cooling towers and air conditioners
Shower heads
Out come of infection depends on size of infective dose
Human infection is typically by inhalation of aerosols provided by cooling towers and air conditioners
Shower heads
Out come of infection depends on size of infective dose
Слайд 11Transmission
Legionella come from natural fresh water reservoirs, such as lakes, ponds,
and puddles, where they parasitize on a broad range of protozoan species as hosts. The availability of the hosts plays a major role in the reproduction and mass release of highly infectious Legionella forms into environments where they can be spread by airborne water caplets and inhaled by people
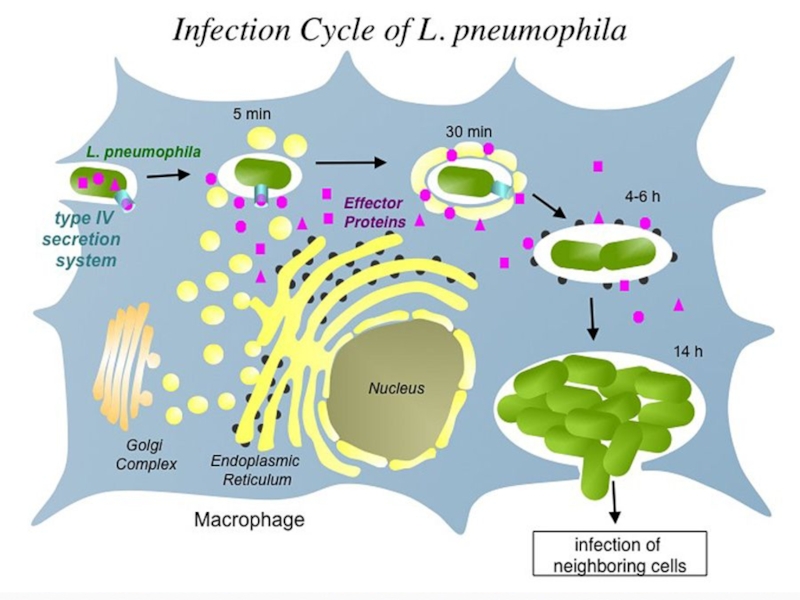
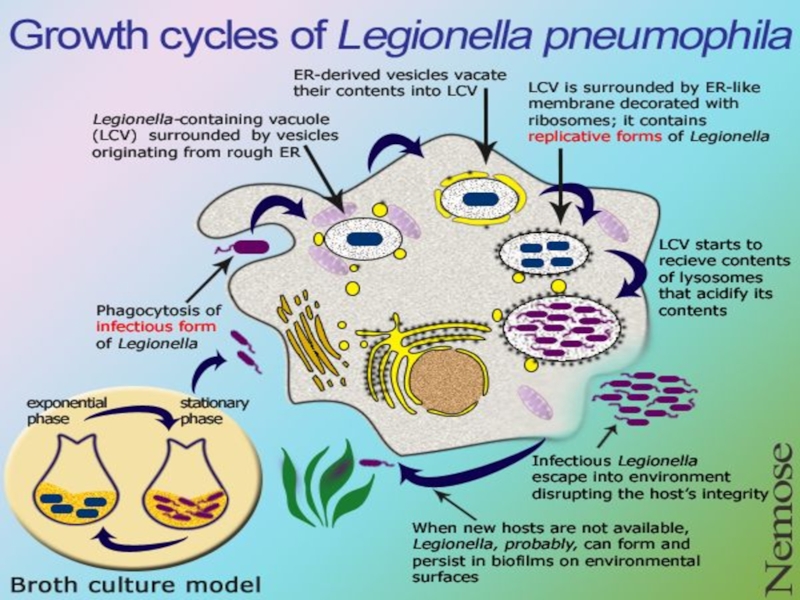
Слайд 12Pathogenesis
In humans, L. pneumophila invades and replicates in macrophages. The internalization
of the bacteria can be enhanced by the presence of antibody and complement, but is not absolutely required. Internalization of the bacteria appears to occur through phagocytosis however L. pneumophila is also capable of infecting non-phagocytic cells through an unknown mechanism. Once internalized, the bacteria surround themselves in a membrane-bound vacuole that does not fuse with lysosomes that would otherwise degrade the bacteria. In this protected compartment, the bacteria multiply.
Слайд 13Who are at Risk
Most healthy individuals do not become infected with
Legionella bacteria after exposure. People at higher risk of getting sick are:
Older people (usually 50 years of age or older)
Current or former smokers
Those with a chronic lung disease (like COPD or emphysema)
Those with a weak immune system from diseases like cancer, diabetes, or kidney failure
People who take drugs that suppress (weaken) the immune system (like after a transplant operation or chemotherapy)
Older people (usually 50 years of age or older)
Current or former smokers
Those with a chronic lung disease (like COPD or emphysema)
Those with a weak immune system from diseases like cancer, diabetes, or kidney failure
People who take drugs that suppress (weaken) the immune system (like after a transplant operation or chemotherapy)
Слайд 14Facts on Legionnaires Disease
Legionella bacteria are not transmitted from person
to person.
People get Legionnaires' disease or Pontiac fever when they breathe in a mist or vapor (small droplets of water in the air) that has been contaminated with Legionella bacteria.
Keeping Legionella bacteria out of water is the key to preventing infection.
Most people with Legionnaires' disease will have pneumonia (lung infection) since the Legionella bacteria grow and thrive in the lungs.
People get Legionnaires' disease or Pontiac fever when they breathe in a mist or vapor (small droplets of water in the air) that has been contaminated with Legionella bacteria.
Keeping Legionella bacteria out of water is the key to preventing infection.
Most people with Legionnaires' disease will have pneumonia (lung infection) since the Legionella bacteria grow and thrive in the lungs.
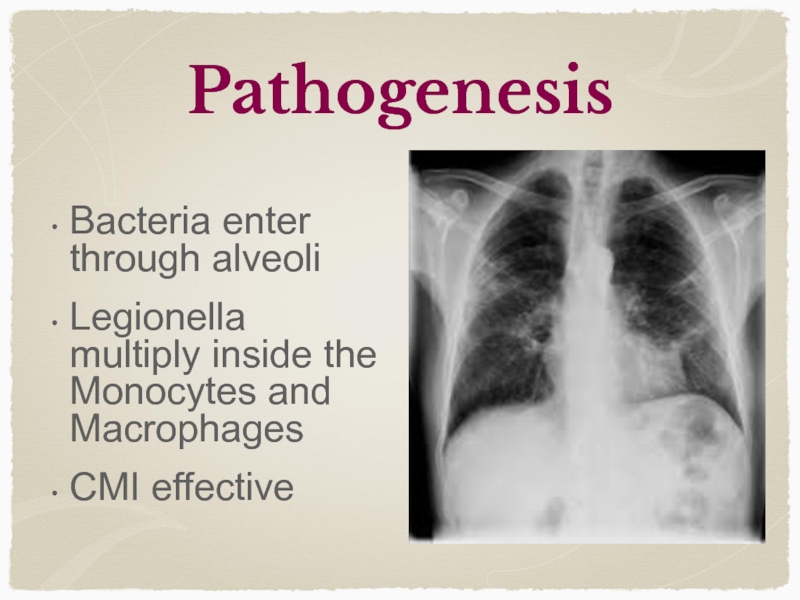
Слайд 15Pathogenesis
Bacteria enter through alveoli
Legionella multiply inside the Monocytes and Macrophages
CMI effective
Слайд 16Predisposing factors
Smoking
Alcohol
Age,
Hospitalization
Immunodeficiency status
Can be Community acquired or Hospital acquired
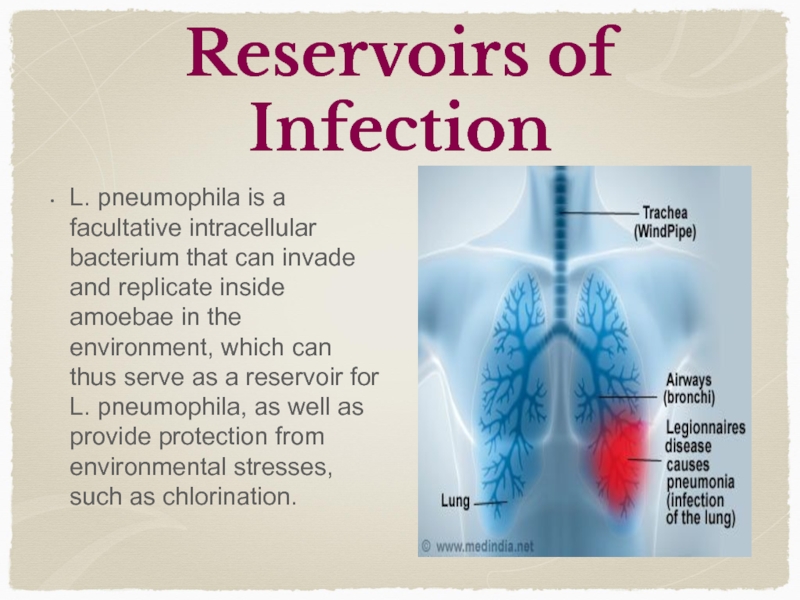
Слайд 17Reservoirs of Infection
L. pneumophila is a facultative intracellular bacterium that
can invade and replicate inside amoebae in the environment, which can thus serve as a reservoir for L. pneumophila, as well as provide protection from environmental stresses, such as chlorination.
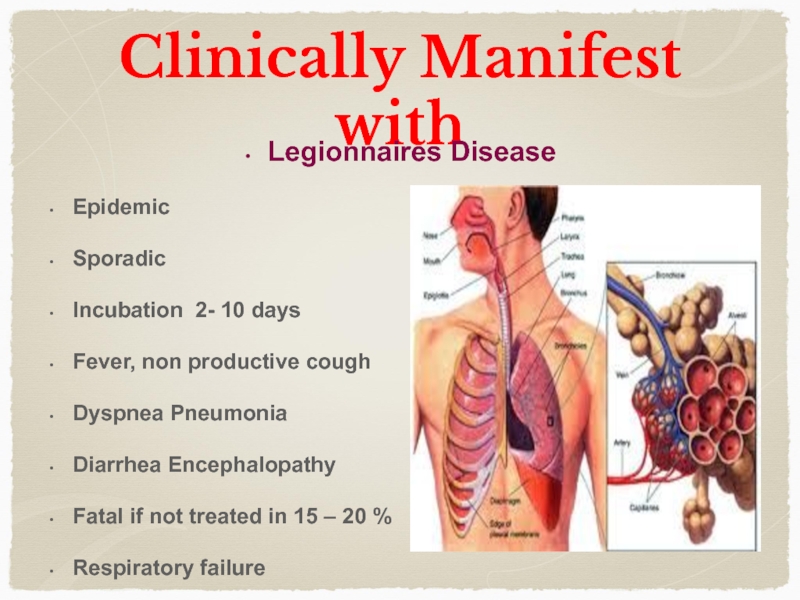
Слайд 18Clinically Manifest with
Legionnaires Disease
Epidemic
Sporadic
Incubation 2- 10 days
Fever, non productive cough
Dyspnea
Pneumonia
Diarrhea Encephalopathy
Fatal if not treated in 15 – 20 %
Respiratory failure
Diarrhea Encephalopathy
Fatal if not treated in 15 – 20 %
Respiratory failure
Слайд 19Pontiac fever
Pontiac fever is a non-pneumonic form of L. pneumophila
infection Symptoms are flu-like, including fever, tiredness, myalgia, headache, sore throat, nausea, and cough may or may not be present. Pontiac fever is self limited and requires no hospitalization or antibiotic therapies. There are no reported deaths associated with Pontiac fever.
Слайд 21Clinically Pontiac Fever manifests with
A milder infection, also caused by
Legionella bacteria, is called Pontiac fever. The symptoms of Pontiac fever are similar to those of Legionnaires’ disease and usually last for 2 to 5 days. Pontiac fever is different from Legionnaires' disease because the patient does not have pneumonia.
Symptoms go away on their own without treatment.
Symptoms go away on their own without treatment.
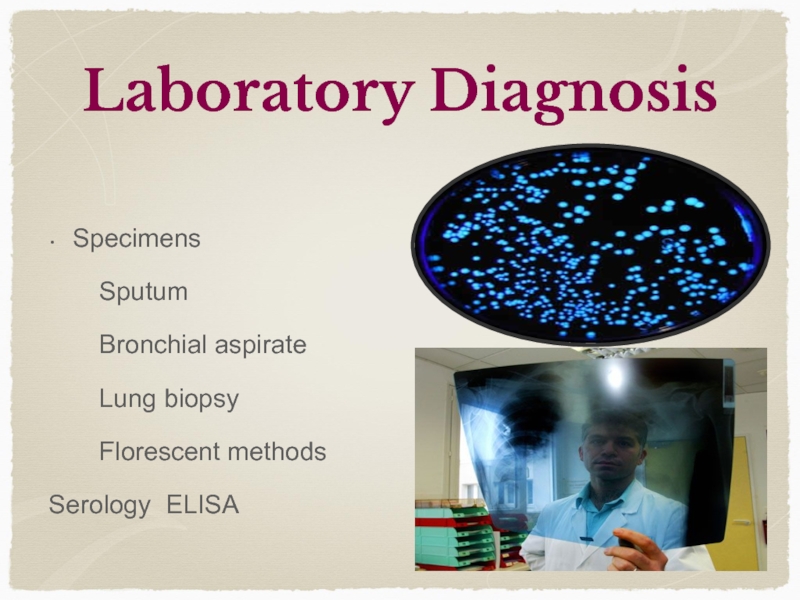
Слайд 22Laboratory Diagnosis
Specimens
Sputum
Bronchial
aspirate
Lung biopsy
Florescent methods
Serology ELISA
Lung biopsy
Florescent methods
Serology ELISA
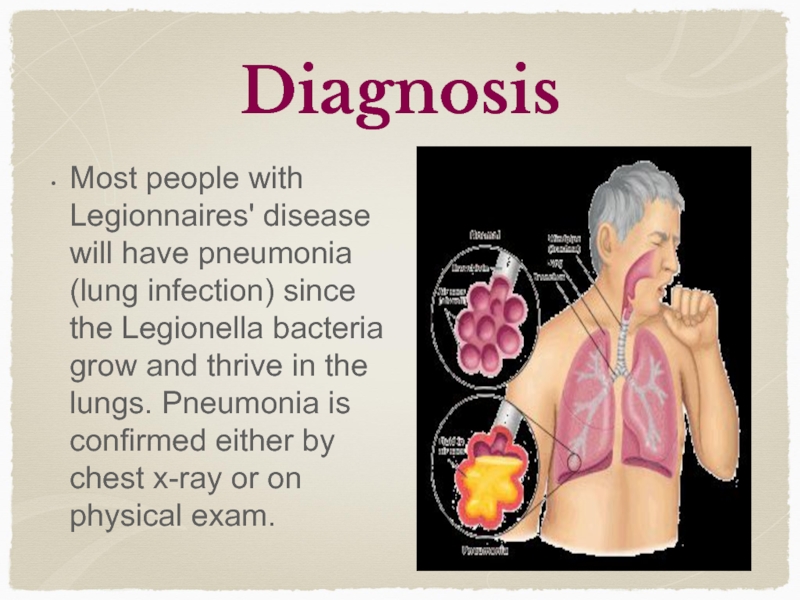
Слайд 23Diagnosis
Most people with Legionnaires' disease will have pneumonia (lung infection) since
the Legionella bacteria grow and thrive in the lungs. Pneumonia is confirmed either by chest x-ray or on physical exam.
Слайд 24Urine Antigen Test
The most commonly used laboratory test for diagnosis is
the urinary antigen test, which detects a part of the Legionella bacteria in urine (pee). If the patient has pneumonia and the test is positive, then the patient is considered to have Legionnaires' disease.
Слайд 25Culture
If the Legionella bacteria are cultured (isolated and grown on special
media) from sputum (phlegm), a lung biopsy specimen, or various other sites, the diagnosis of Legionnaires’ disease is also considered confirmed.
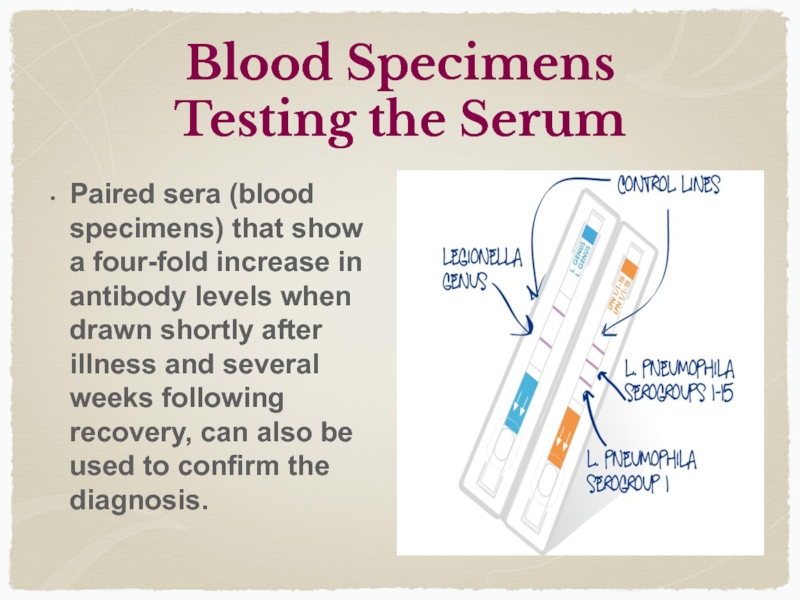
Слайд 26Blood Specimens
Testing the Serum
Paired sera (blood specimens) that show a
four-fold increase in antibody levels when drawn shortly after illness and several weeks following recovery, can also be used to confirm the diagnosis.
Слайд 27Pontiac Fever
Pontiac fever can be confirmed by urine antigen or paired
sera (blood specimens), but a negative test doesn’t rule out the diagnosis. It is often diagnosed clinically in the setting of other laboratory-confirmed legionellosis cases. Culture (isolating and growing the bacteria on special media) cannot be used to diagnose Pontiac fever.
Слайд 28Detection
Sera have been used both for slide agglutination studies as well
as for direct detection of bacteria in tissues using fluorescent-labelled antibody. Specific antibody in patients can be determined by the indirect fluorescent antibody test. ELISA and micro agglutination tests have also been successfully applied
Legionella stains poorly with gram stain, stains positive with silver, and is cultured on charcoal yeast extract with iron and cysteine.
Legionella stains poorly with gram stain, stains positive with silver, and is cultured on charcoal yeast extract with iron and cysteine.
Слайд 29Treatment & Complications
Treatment
Legionnaires' disease requires treatment with antibiotics (drugs that kill
bacteria in the body), and most cases of Legionnaires’ disease can be treated successfully with antibiotics. Healthy people usually get better after being sick with Legionnaires’ disease, but hospitalization is often required. Pontiac fever goes away without specific treatment. Antibiotics provide no benefit for a patient with Pontiac fever.
Слайд 30Treatment
Respiratory fluoroquinolones and the newer macrolides are used to treat L.
pneumophila pneumonia. Treatment typically lasts 7-10 days or in the case of immunosuppressed patients, 21 days. Pontiac fever usually does not require antimicrobial therapy.
Слайд 32
Programme Created and Designed by Dr.T.V.Rao MD for Medical students for
Global education on Infectious Diseases
email
doctortvrao@gmail.com
doctortvrao@gmail.com