- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Confidentiality in Healthcare презентация
Содержание
- 1. Confidentiality in Healthcare
- 2. Session Objectives What is confidentiality? /Why respect
- 3. Confidentiality ‘Most people consider health information
- 4. What information is confidential? All identifiable patient
- 5. When does a matter become confidential? Broadly
- 6. Why respect confidentiality? Trust is an important
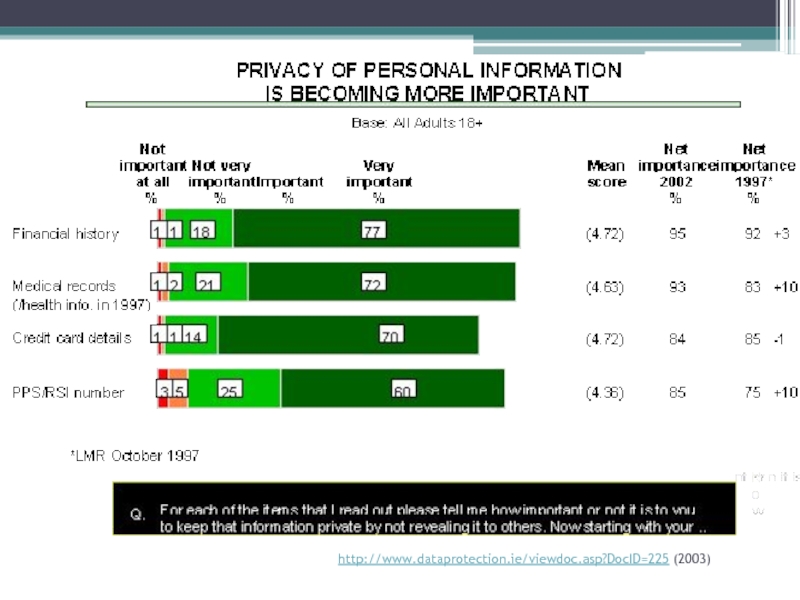
- 7. http://www.dataprotection.ie/viewdoc.asp?DocID=225 (2003)
- 8. Why respect confidentiality?
- 9. Why respect confidentiality? Hospital policy Contained within
- 10. Why respect confidentiality? Professional Code of Conduct
- 11. The Irish Medical Council – Guide to
- 12. Why respect confidentiality? The Data Protection Commissioner
- 13. Confidentiality Ethics and Law
- 14. Is the duty of confidentiality absolute?
- 15. Is confidentiality an absolute right? In Ireland
- 16. The exceptions to confidentiality There are four
- 17. When necessary to protect the interests of
- 18. Case ‘Against all the odds, and despite
- 19. How can healthcare providers insure confidentiality is
- 20. Summary Confidentiality is VITAL in healthcare –
Слайд 2Session Objectives
What is confidentiality? /Why respect confidentiality?
The law
Is confidentiality absolute/Exceptions to
confidentiality/Breeching confidentiality
Confidentiality –Death, incapacity and minors
Confidentiality - Palliative care case study
Confidentiality –Death, incapacity and minors
Confidentiality - Palliative care case study
Слайд 3Confidentiality
‘Most people consider health information to be highly personal and, therefore,
need to be confident that their privacy will be protected whenever they use a health service ... Clear and open communication between the health service provider and health consumer is integral to good privacy’
Radwanshi (2001)
Radwanshi (2001)
Generally, if institution/person ‘A’ holds information about person ‘B’ then person ‘C’ cannot obtain that information in the normal course of events without the consent of person ‘B’
Слайд 4What information is confidential?
All identifiable patient information, whether written, computerised, visual
or audio recorded or simply held in the memory of health professionals, is subject to the duty of confidentiality.
It covers:
Any clinical information about an individual’s diagnosis or treatment
A picture, photograph, video, audiotape or other images of the patient
Who the patient’s doctor is and what clinics patients attend and when
Anything else that may be used to identify patients directly or indirectly.
(BMA 2008)
It covers:
Any clinical information about an individual’s diagnosis or treatment
A picture, photograph, video, audiotape or other images of the patient
Who the patient’s doctor is and what clinics patients attend and when
Anything else that may be used to identify patients directly or indirectly.
(BMA 2008)
Слайд 5When does a matter become confidential?
Broadly speaking the courts have recognised
three elements to deciding whether a matter is confidential:
The nature of the information
Nature of the encounter
Nature of any disclosure
The nature of the information
Nature of the encounter
Nature of any disclosure
Слайд 6Why respect confidentiality?
Trust is an important aspect between patients and healthcare
professionals. Patients without fear of a breech of confidentiality should be able to communicate symptoms that often they may feel are embarrassing, stigmatising, or indeed trivial
Without this trusting relationship patients may not divulge information which may make treating them impossible
Patients may not seek medical attention at all
Has important role in a professional patient relationship establishing a sense of security, freedom of action and self respect for patients
Without this trusting relationship patients may not divulge information which may make treating them impossible
Patients may not seek medical attention at all
Has important role in a professional patient relationship establishing a sense of security, freedom of action and self respect for patients
Слайд 9Why respect confidentiality?
Hospital policy
Contained within each member of staff contract of
employment
Can result in disciplinary action
Can result in disciplinary action
Слайд 10Why respect confidentiality?
Professional Code of Conduct – An Bord Altranais
‘Information regarding
a patient’s history, treatment and state of health is privileged and confidential...’
‘Professional judgement and responsibility should be exercised in the sharing of such information with professional colleagues. The confidentiality of patient’s records must be safeguarded.’
(http://www.nursingboard.ie/en/publications_current.aspx?page=4 )
‘Professional judgement and responsibility should be exercised in the sharing of such information with professional colleagues. The confidentiality of patient’s records must be safeguarded.’
(http://www.nursingboard.ie/en/publications_current.aspx?page=4 )
Слайд 11The Irish Medical Council – Guide to Professional Conduct and Ethics
‘Confidentiality
is a fundamental principle of medical ethics and is central to the trust between patients and doctors’
‘Patient information remains confidential even after death’
‘You should ensure as far as possible that the patient’s privacy is maintained at all times and that accidental disclosure of confidential information does not occur’
‘You should ensure as far as possible that confidential information in relation to patients is maintained securely and in compliance with data protection legislation’.
‘Patient information remains confidential even after death’
‘You should ensure as far as possible that the patient’s privacy is maintained at all times and that accidental disclosure of confidential information does not occur’
‘You should ensure as far as possible that confidential information in relation to patients is maintained securely and in compliance with data protection legislation’.
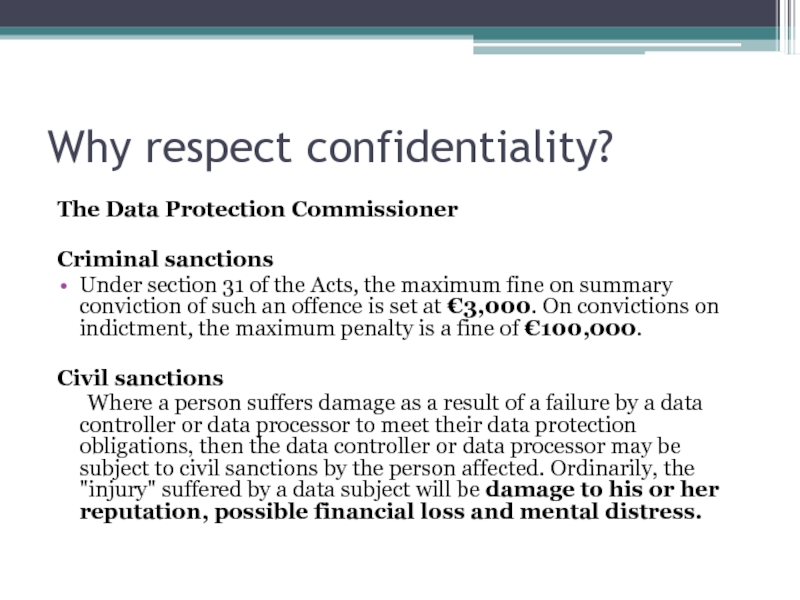
Слайд 12Why respect confidentiality?
The Data Protection Commissioner
Criminal sanctions
Under section 31 of the
Acts, the maximum fine on summary conviction of such an offence is set at €3,000. On convictions on indictment, the maximum penalty is a fine of €100,000.
Civil sanctions
Where a person suffers damage as a result of a failure by a data controller or data processor to meet their data protection obligations, then the data controller or data processor may be subject to civil sanctions by the person affected. Ordinarily, the "injury" suffered by a data subject will be damage to his or her reputation, possible financial loss and mental distress.
Civil sanctions
Where a person suffers damage as a result of a failure by a data controller or data processor to meet their data protection obligations, then the data controller or data processor may be subject to civil sanctions by the person affected. Ordinarily, the "injury" suffered by a data subject will be damage to his or her reputation, possible financial loss and mental distress.
Слайд 15Is confidentiality an absolute right?
In Ireland confidentiality or privacy is recognised
by the courts as a right, but not an absolute right
The belief that confidentiality is not absolute is also the model which our two closest neighbours the U.S. and the U.K. subscribe to
In France and Belgium confidentiality is considered as an absolute requirement to protect the patient’s interests
The belief that confidentiality is not absolute is also the model which our two closest neighbours the U.S. and the U.K. subscribe to
In France and Belgium confidentiality is considered as an absolute requirement to protect the patient’s interests
Слайд 16The exceptions to confidentiality
There are four circumstances where exceptions may be
justified in the absence of permission from the patient:
(1) When ordered by a Judge in a Court of Law, or by a Tribunal established by an Act of the Oireachtas.
(2) When necessary to protect the interests of the patient.
(3) When necessary to protect the welfare of society.
(4) When necessary to safeguard the welfare of another individual or patient.
(https://medicalcouncil.ie/Media-Centre/Publications/Older/Ethical%20Guide%202004.pdf )
(1) When ordered by a Judge in a Court of Law, or by a Tribunal established by an Act of the Oireachtas.
(2) When necessary to protect the interests of the patient.
(3) When necessary to protect the welfare of society.
(4) When necessary to safeguard the welfare of another individual or patient.
(https://medicalcouncil.ie/Media-Centre/Publications/Older/Ethical%20Guide%202004.pdf )
Слайд 17When necessary to protect the interests of the patient
Children or adults
who are subject to abuse - Child Care Act 1991, furnishes the Garda Siochana with the power to evoke an emergency care order if they believe there is an immediate and serious risk to the health or welfare of a child
The protection of an individual from themselves, in cases of suicide could also be broadly placed in this category; this is where the limits of this exception become vague
The protection of an individual from themselves, in cases of suicide could also be broadly placed in this category; this is where the limits of this exception become vague
Слайд 18Case
‘Against all the odds, and despite being referred to a hospice,
Collette showed signs of recovering from bowel cancer. After several months, the consultant decided that Collette was no longer terminally ill, although he could not be certain that she would not become ill again in the future. Accordingly, he felt she no longer required the extensive support supplied by the hospice and discharged her. Collette was very upset by this, partly because she did not want to loose her terminally ill status, which had generated her more attention from her family than she had become accustomed to in the past.
The hospice staff were not unsympathetic. They had promised that they would not abandon her and would care for her until she died. The staff also widely believed that her family had rather neglected her previously. Because they did not wish to let Collette down, she was given radically reduced honorary status as an out-patient. For instance she still attended social events and had her hair set by the hair dresser who donated some of her spare time to the hospice. It quickly became obvious that Collette’s family did not realise that she was no longer thought to be terminally ill. The nurse manager attempted to talk to Collette about this, but she was politely and firmly told to mind her own business.’
(Webb 2005)
The hospice staff were not unsympathetic. They had promised that they would not abandon her and would care for her until she died. The staff also widely believed that her family had rather neglected her previously. Because they did not wish to let Collette down, she was given radically reduced honorary status as an out-patient. For instance she still attended social events and had her hair set by the hair dresser who donated some of her spare time to the hospice. It quickly became obvious that Collette’s family did not realise that she was no longer thought to be terminally ill. The nurse manager attempted to talk to Collette about this, but she was politely and firmly told to mind her own business.’
(Webb 2005)
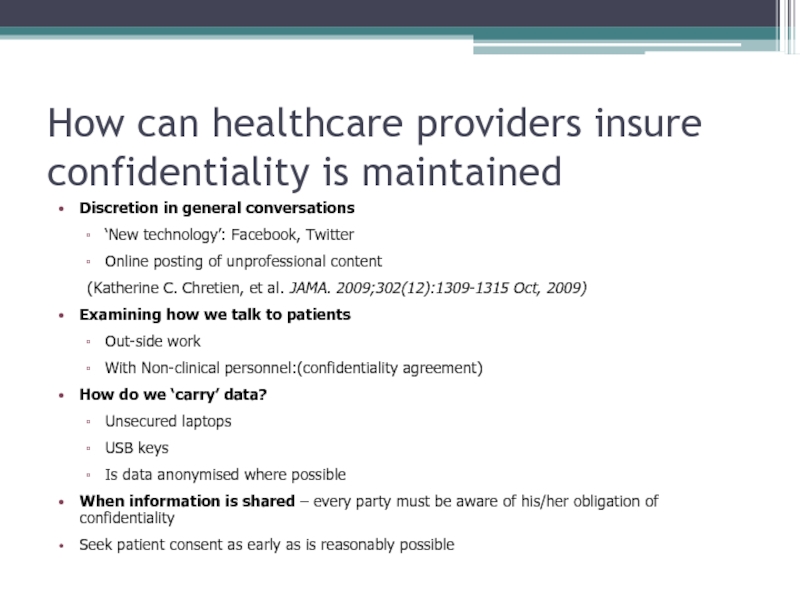
Слайд 19How can healthcare providers insure confidentiality is maintained
Discretion in general conversations
‘New
technology’: Facebook, Twitter
Online posting of unprofessional content
(Katherine C. Chretien, et al. JAMA. 2009;302(12):1309-1315 Oct, 2009)
Examining how we talk to patients
Out-side work
With Non-clinical personnel:(confidentiality agreement)
How do we ‘carry’ data?
Unsecured laptops
USB keys
Is data anonymised where possible
When information is shared – every party must be aware of his/her obligation of confidentiality
Seek patient consent as early as is reasonably possible
Online posting of unprofessional content
(Katherine C. Chretien, et al. JAMA. 2009;302(12):1309-1315 Oct, 2009)
Examining how we talk to patients
Out-side work
With Non-clinical personnel:(confidentiality agreement)
How do we ‘carry’ data?
Unsecured laptops
USB keys
Is data anonymised where possible
When information is shared – every party must be aware of his/her obligation of confidentiality
Seek patient consent as early as is reasonably possible
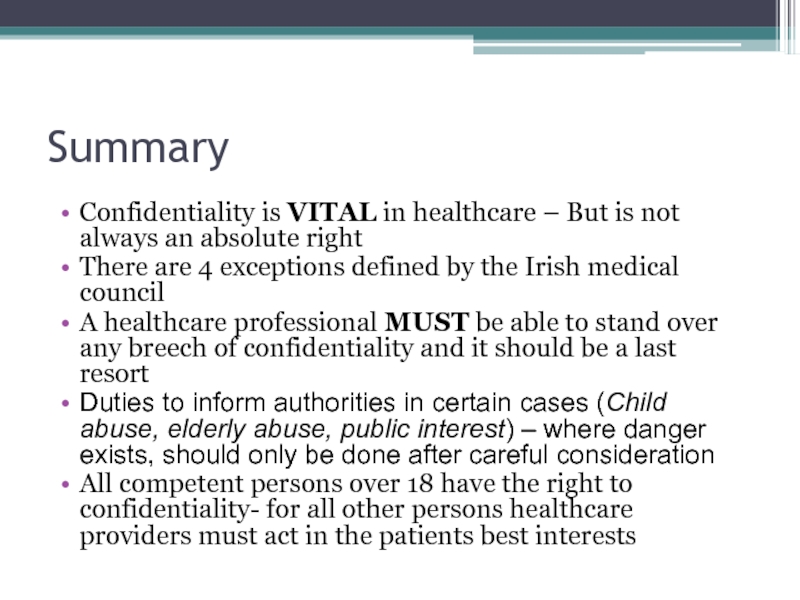
Слайд 20Summary
Confidentiality is VITAL in healthcare – But is not always an
absolute right
There are 4 exceptions defined by the Irish medical council
A healthcare professional MUST be able to stand over any breech of confidentiality and it should be a last resort
Duties to inform authorities in certain cases (Child abuse, elderly abuse, public interest) – where danger exists, should only be done after careful consideration
All competent persons over 18 have the right to confidentiality- for all other persons healthcare providers must act in the patients best interests
There are 4 exceptions defined by the Irish medical council
A healthcare professional MUST be able to stand over any breech of confidentiality and it should be a last resort
Duties to inform authorities in certain cases (Child abuse, elderly abuse, public interest) – where danger exists, should only be done after careful consideration
All competent persons over 18 have the right to confidentiality- for all other persons healthcare providers must act in the patients best interests