- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
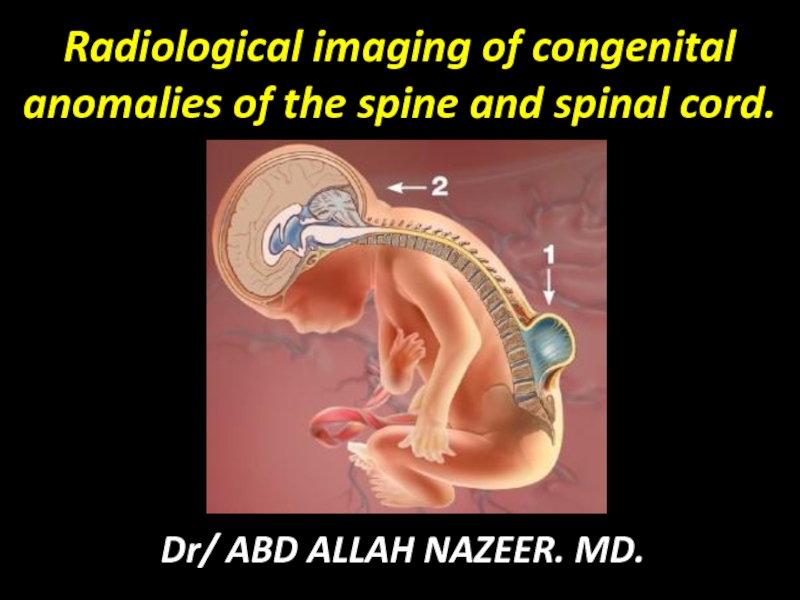
Radiological imaging of congenital anomalies of the spine and spinal cord. презентация
Содержание
- 1. Radiological imaging of congenital anomalies of the spine and spinal cord.
- 2. Congenital abnormalities of the spine and spinal
- 3. Radiological imaging techniques: Plain Radiography. Ultrasonography. Computed tomography(CT Scan). Magnetic resonance imaging(MRI). Nuclear Imaging.
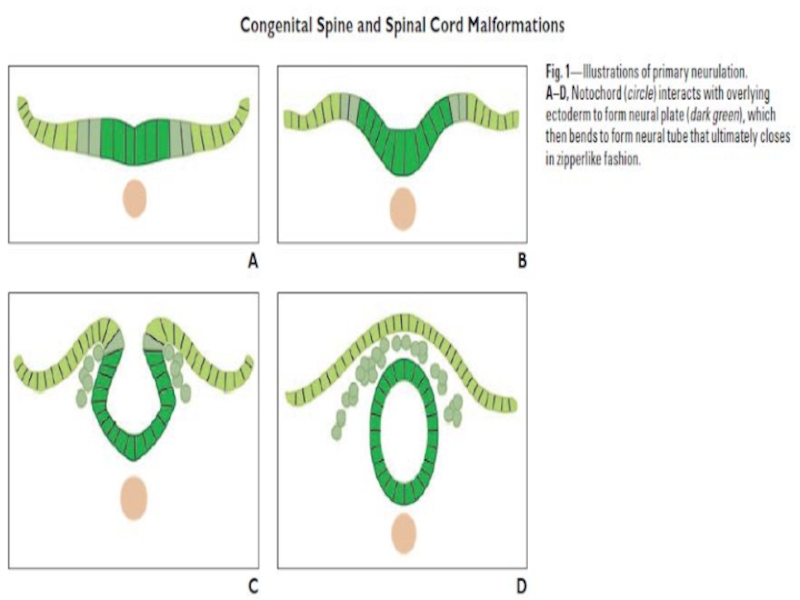
- 4. Spinal Cord Development Spinal development can be
- 6. Neurulation and derangement of neurulation: Four stages
- 7. Categorization of Spinal Dysraphisms: Spinal dysraphisms can
- 8. Closed Spinal Dysraphisms: covered by intact skin
- 9. Open Spinal Dysraphisms: Myelomeningocele and myelocele—Myelomeningoceles and
- 10. Deranged neurulation: Spina Bifida aperta: Myelocele and
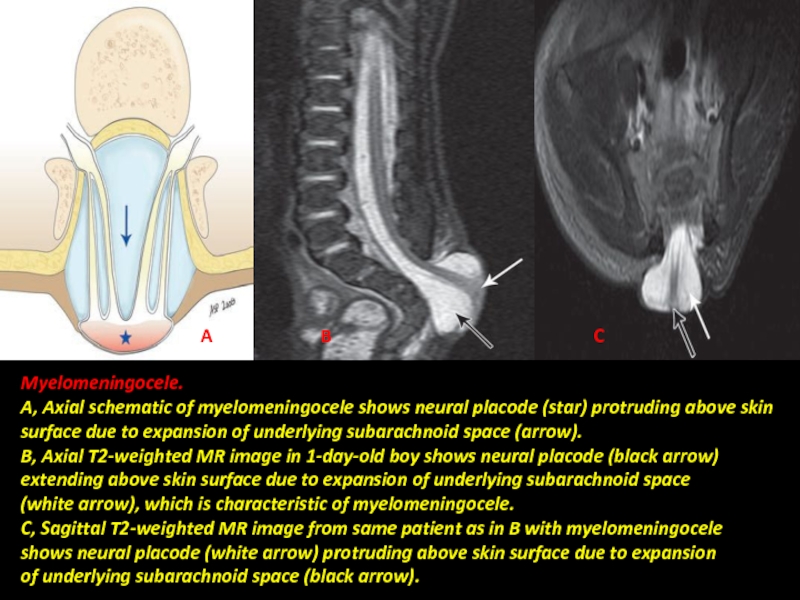
- 11. Myelomeningocele. A, Axial schematic of myelomeningocele shows
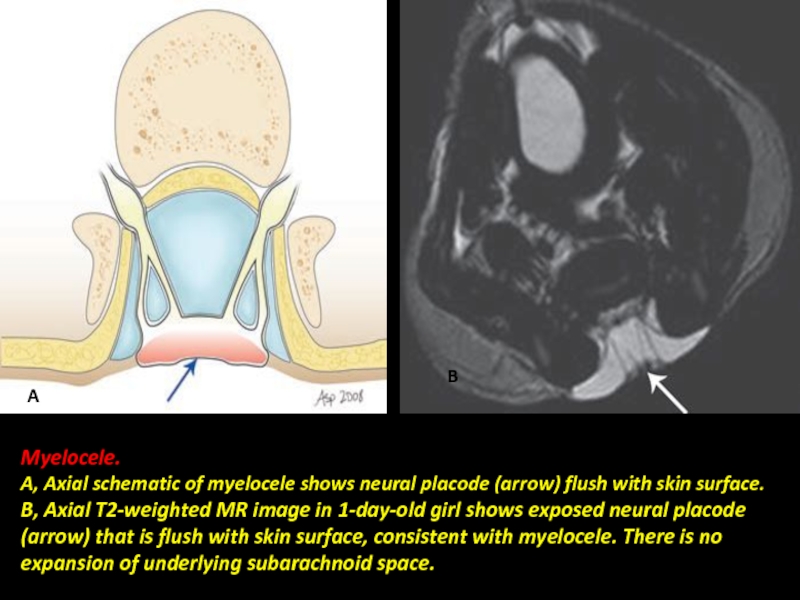
- 12. Myelocele. A, Axial schematic of myelocele shows
- 13. Chiari malformation, also known as Arnold–Chiari malformation,
- 14. Chiaric-1 malformation: A congenital malformation. Is generally
- 15. Chiari -1 Malformation.
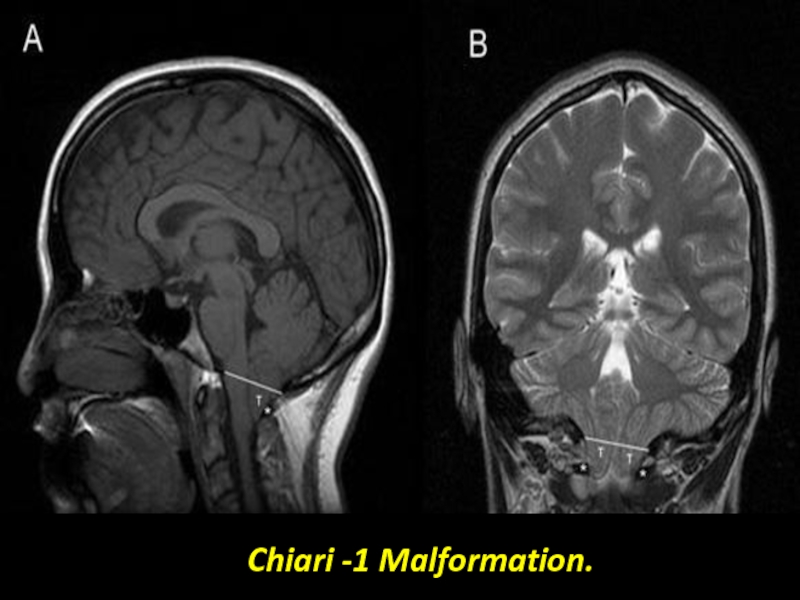
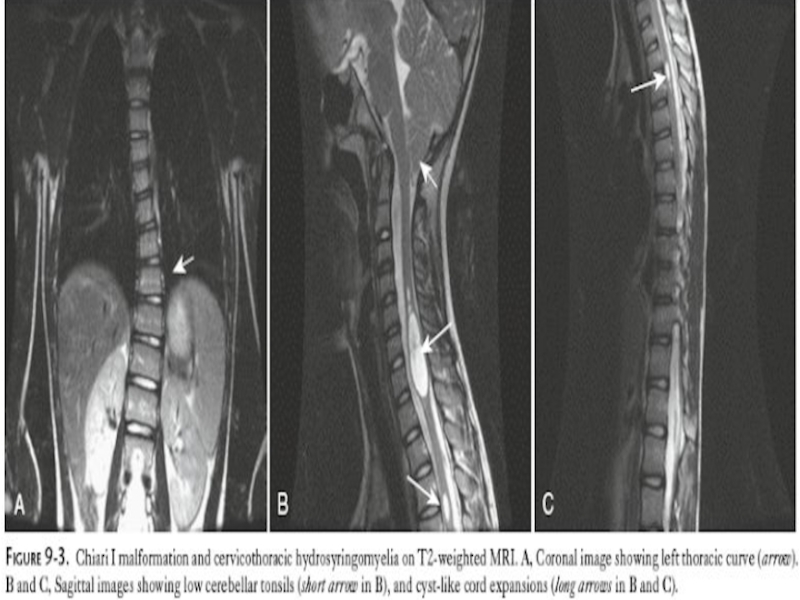
- 16. Chiari Type 1 Malformation.
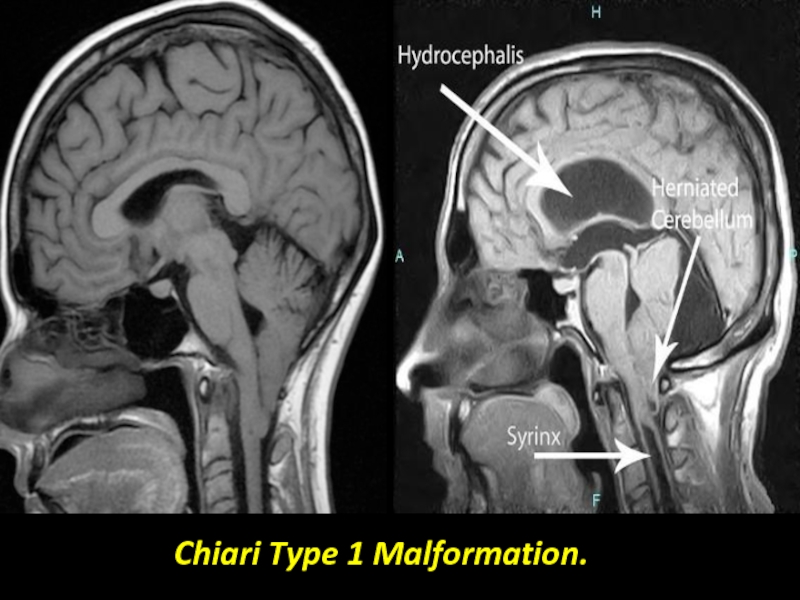
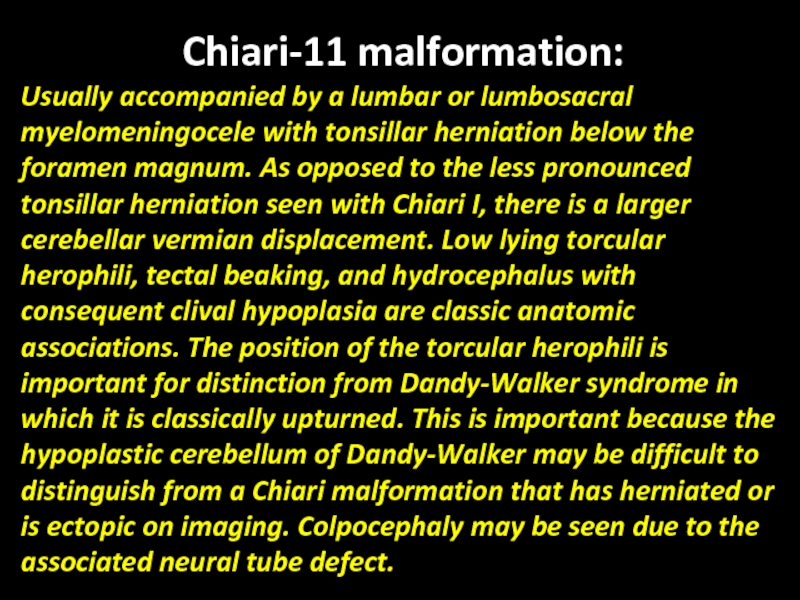
- 18. Chiari-11 malformation: Usually accompanied by a
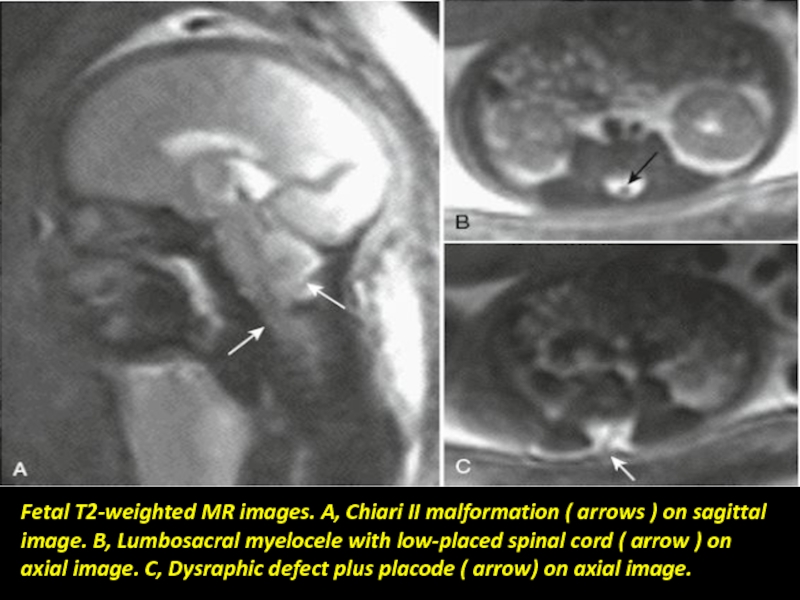
- 19. Fetal T2-weighted MR images. A, Chiari II
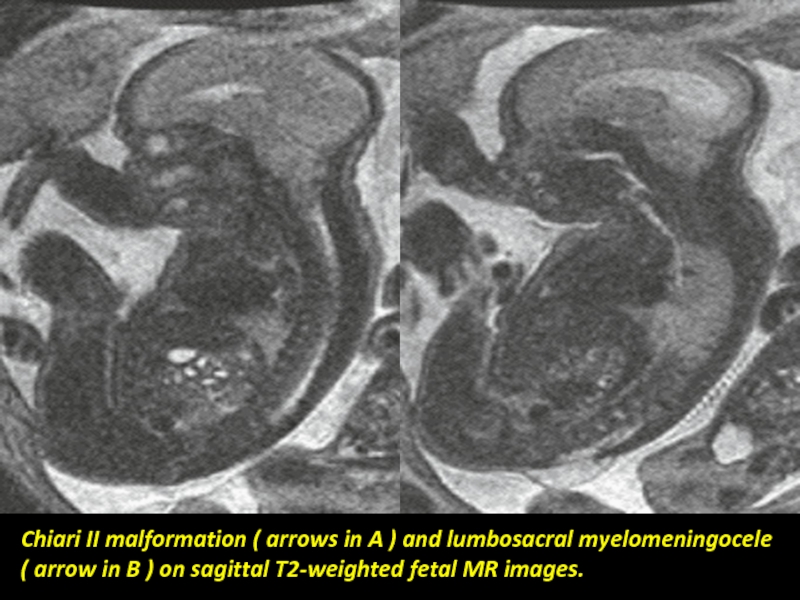
- 20. Chiari II malformation ( arrows in A
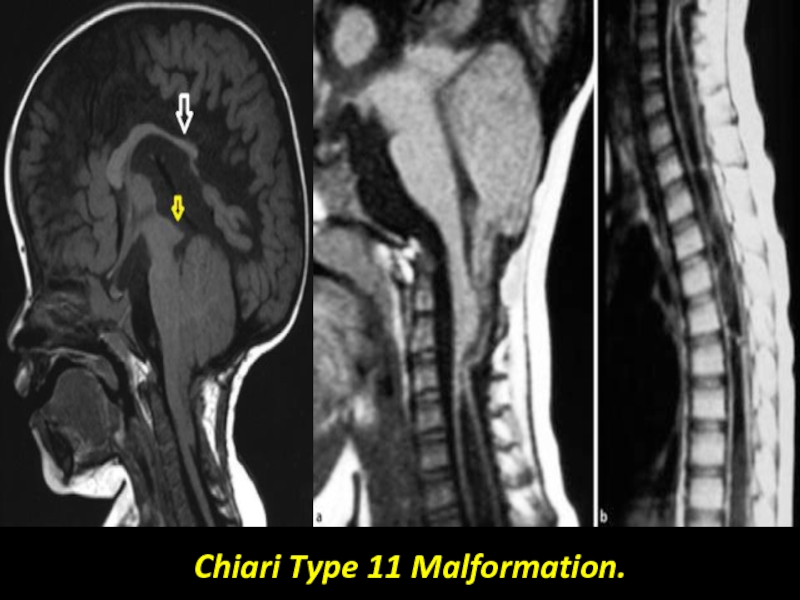
- 21. Chiari Type 11 Malformation.
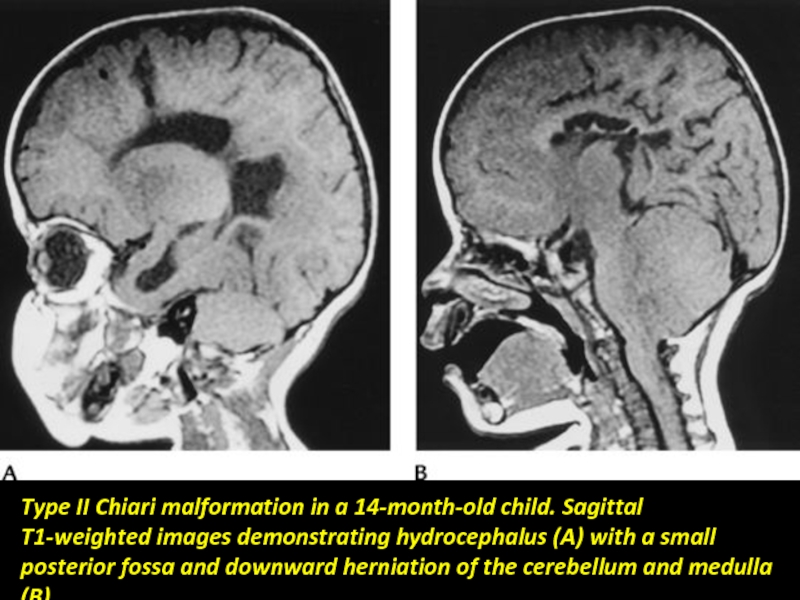
- 22. Type II Chiari malformation in a 14-month-old
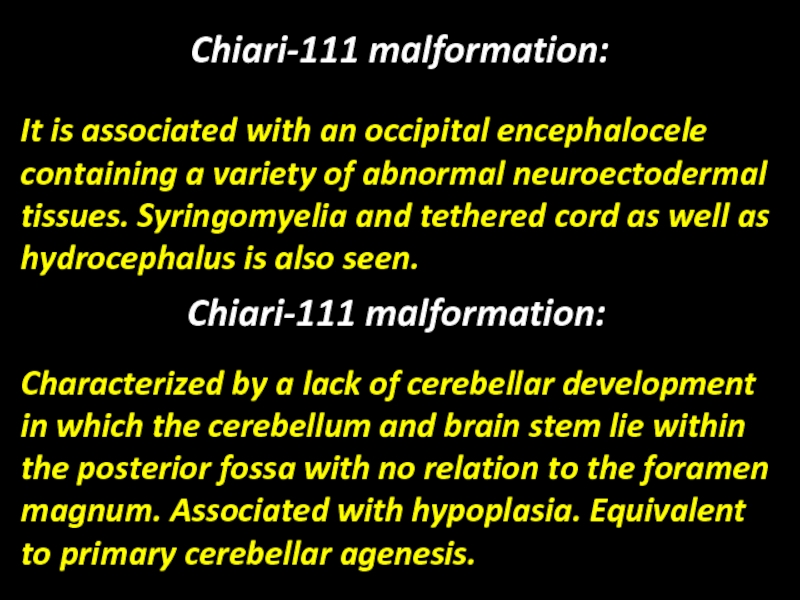
- 23. Chiari-111 malformation: It is associated with
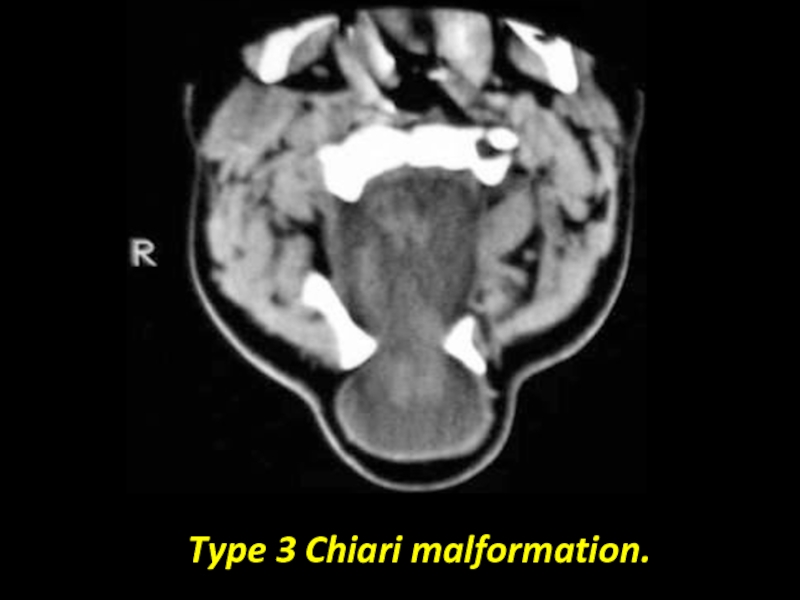
- 24. Type 3 Chiari malformation.
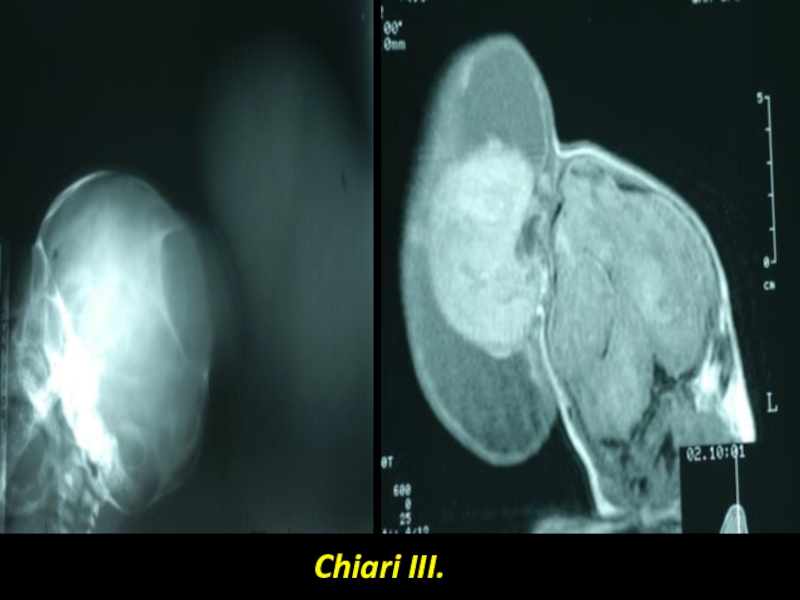
- 25. Chiari III.
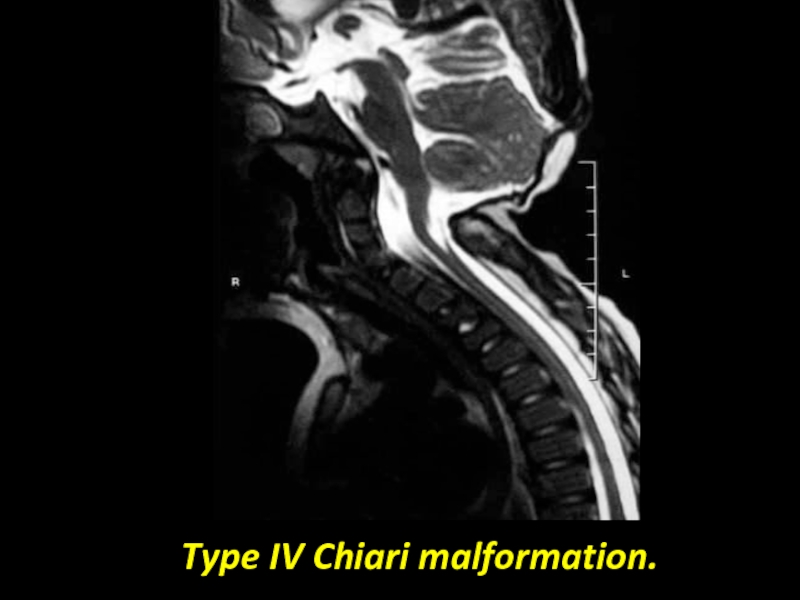
- 26. Type IV Chiari malformation.
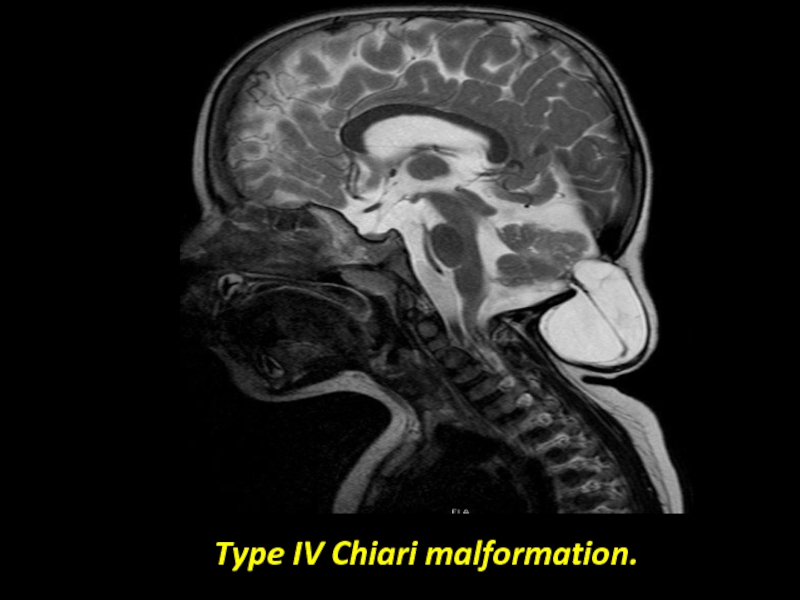
- 27. Type IV Chiari malformation.
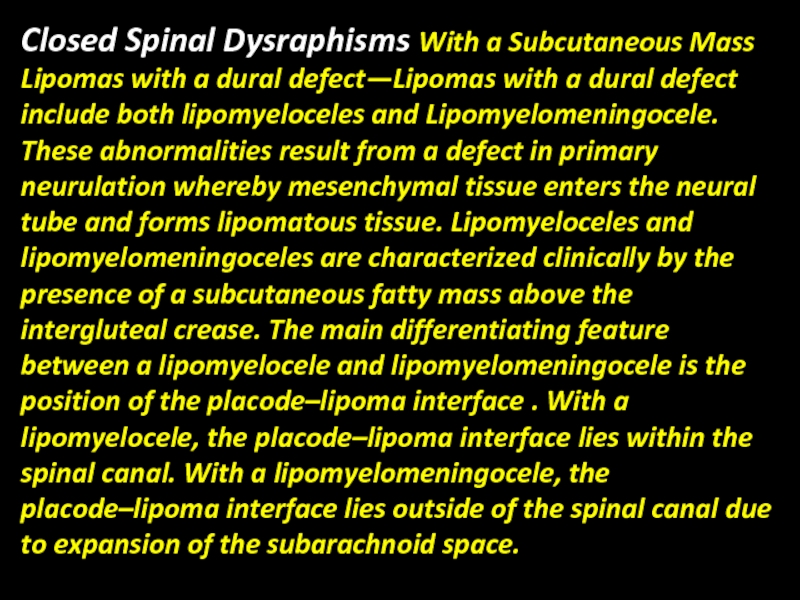
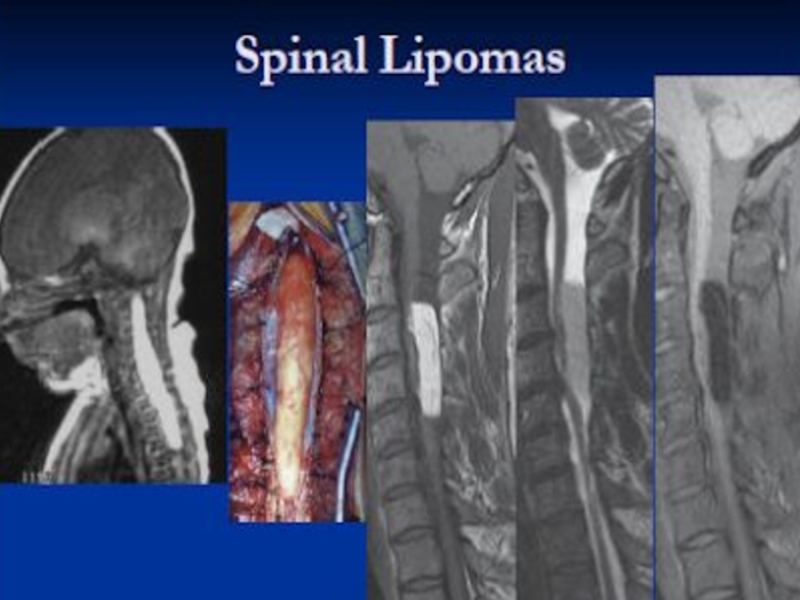
- 28. Closed Spinal Dysraphisms With a Subcutaneous Mass
- 29. Meningocele—Herniation of a CSF-filled sac lined by
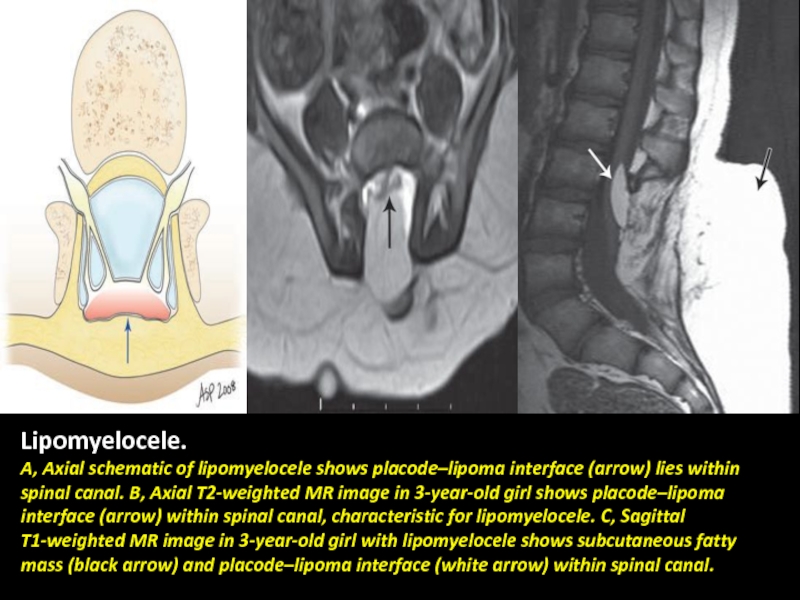
- 30. Lipomyelocele. A, Axial schematic of lipomyelocele shows
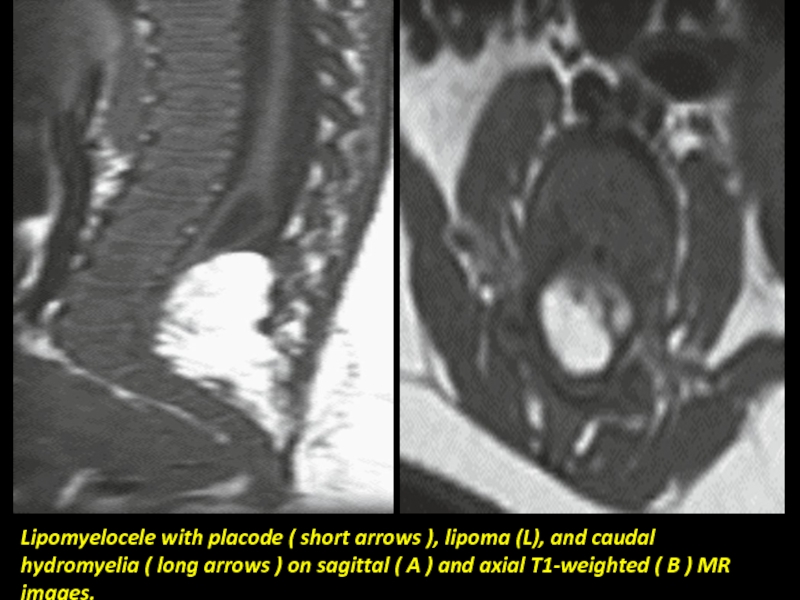
- 31. Lipomyelocele with placode ( short arrows ),
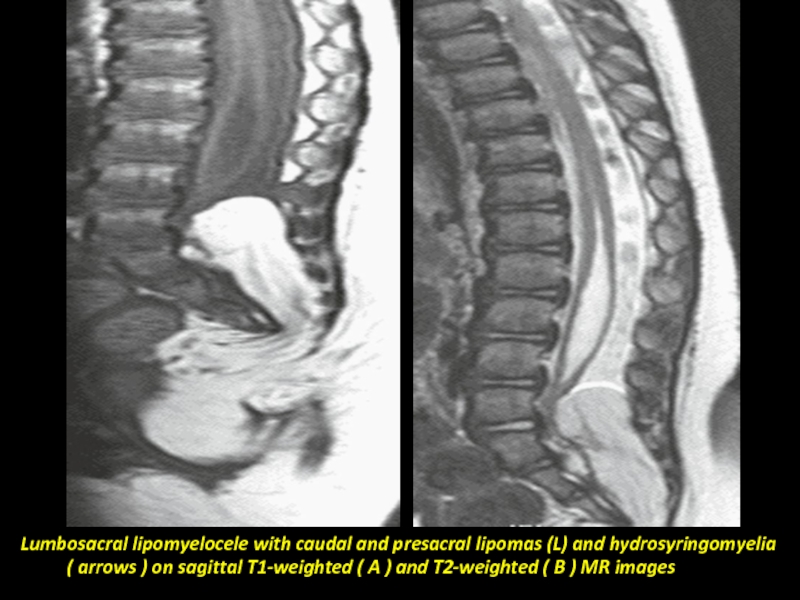
- 32. Lumbosacral lipomyelocele with caudal and presacral lipomas
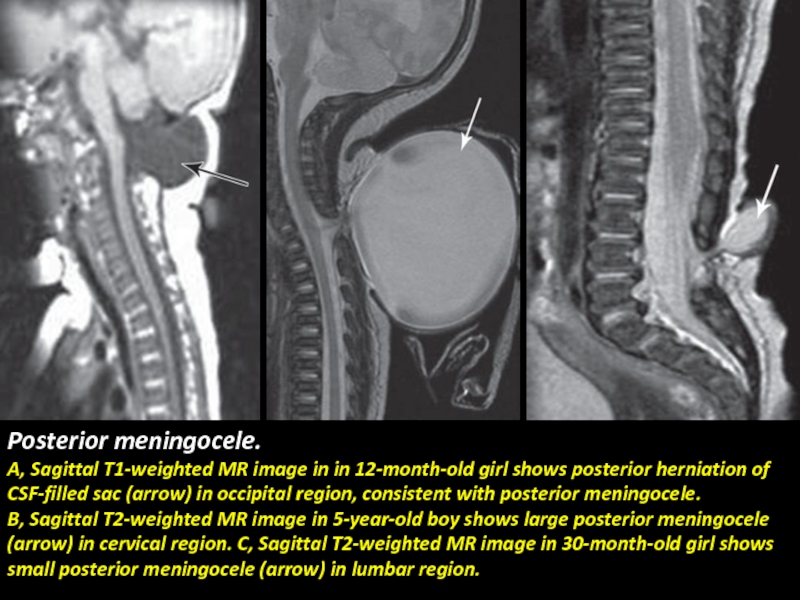
- 33. Posterior meningocele. A, Sagittal T1-weighted MR image
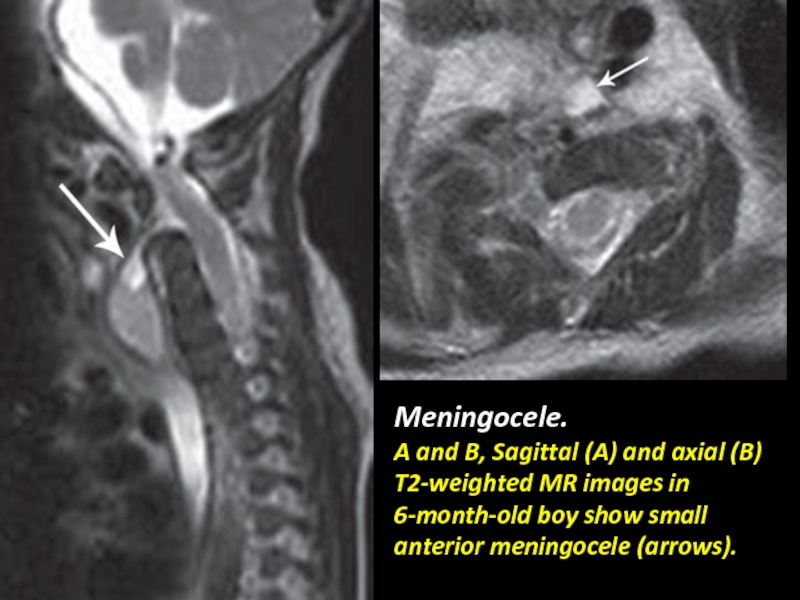
- 34. Meningocele. A and B, Sagittal (A) and
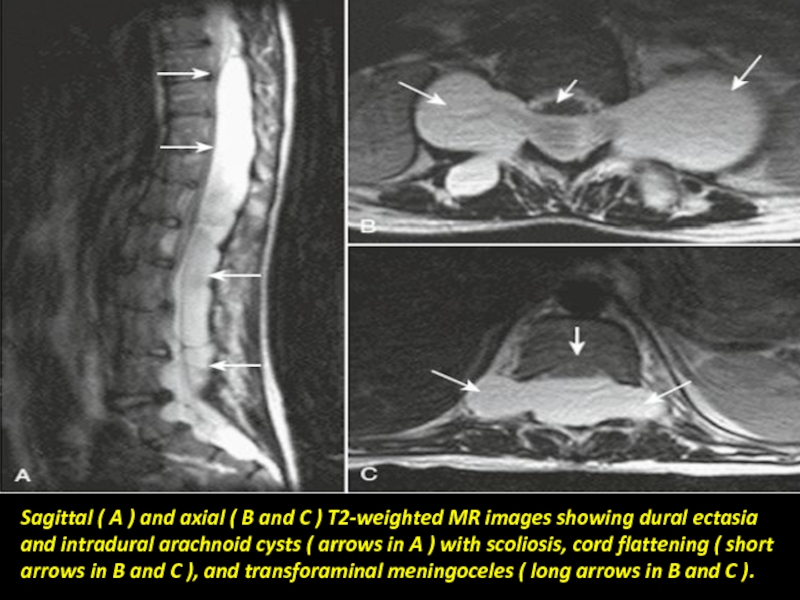
- 35. Sagittal ( A ) and axial (
- 36. Thoracic Meningocele.
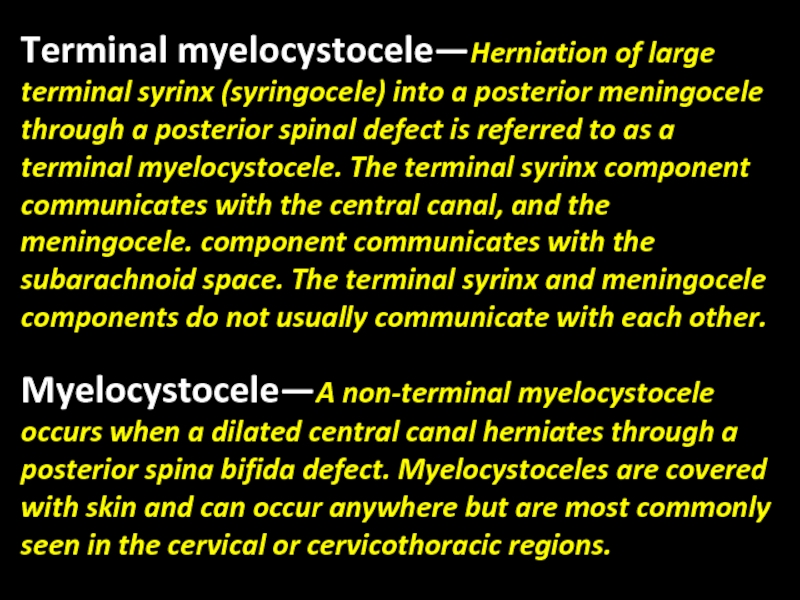
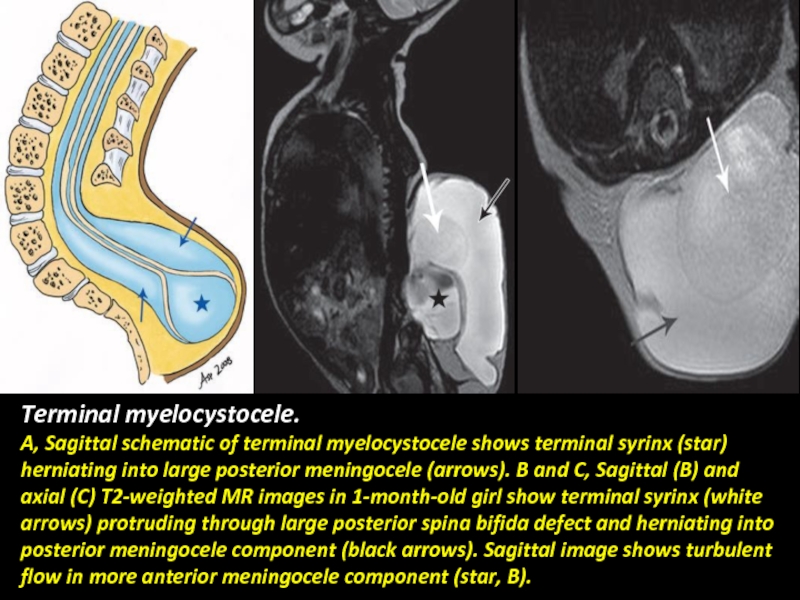
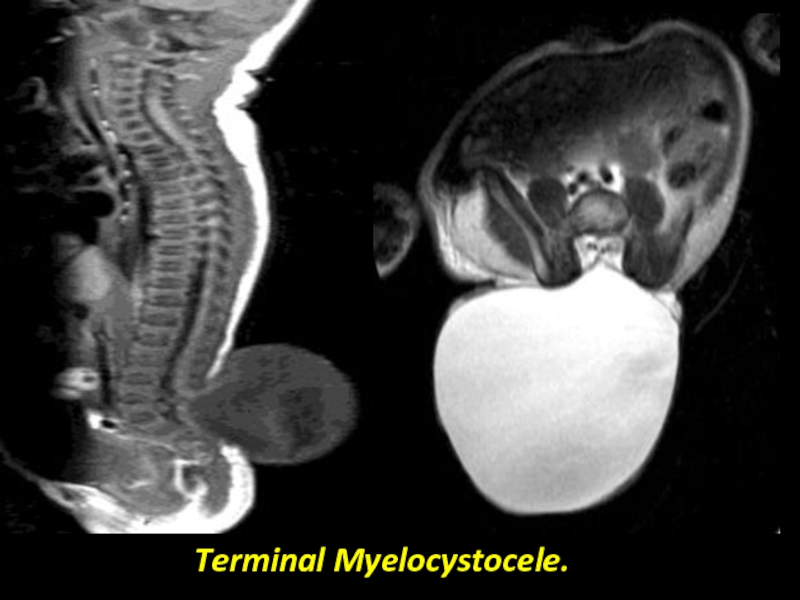
- 37. Terminal myelocystocele—Herniation of large terminal syrinx (syringocele)
- 38. Terminal myelocystocele. A, Sagittal schematic of terminal
- 39. Terminal Myelocystocele.
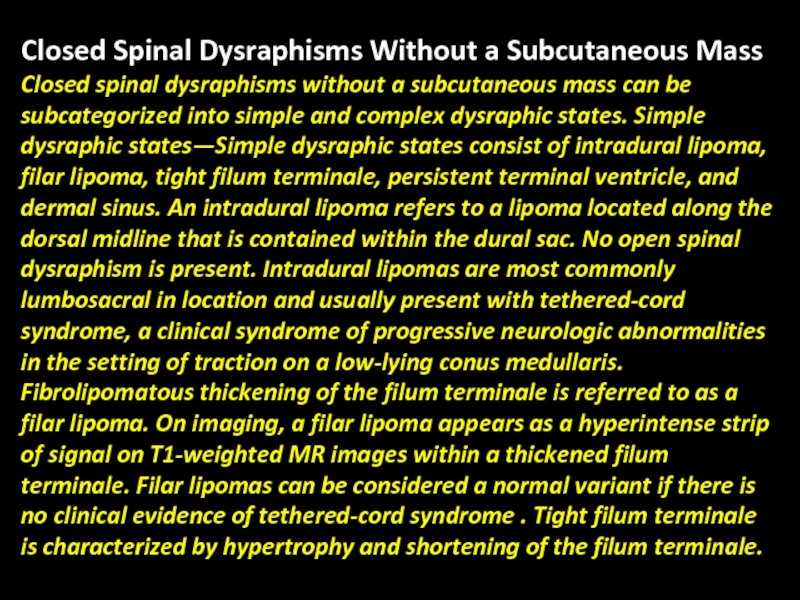
- 40. Closed Spinal Dysraphisms Without a Subcutaneous Mass
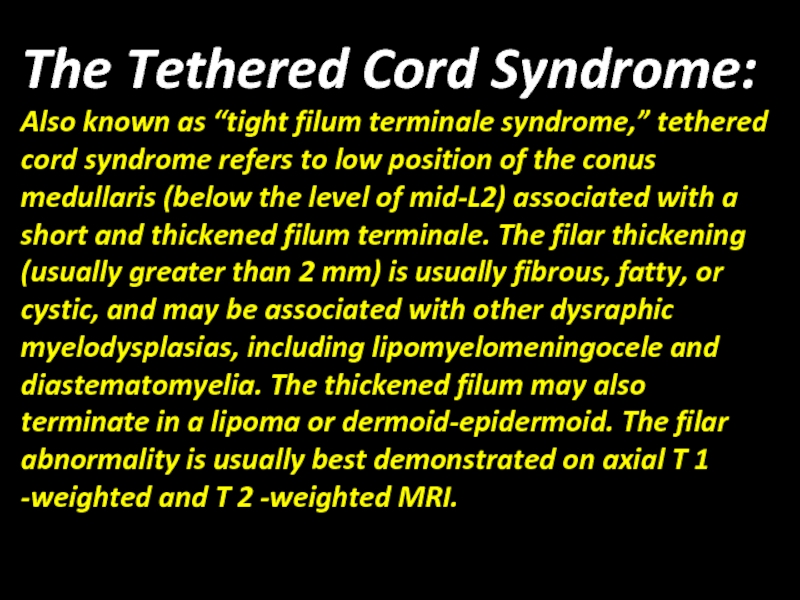
- 41. The Tethered Cord Syndrome: Also known as
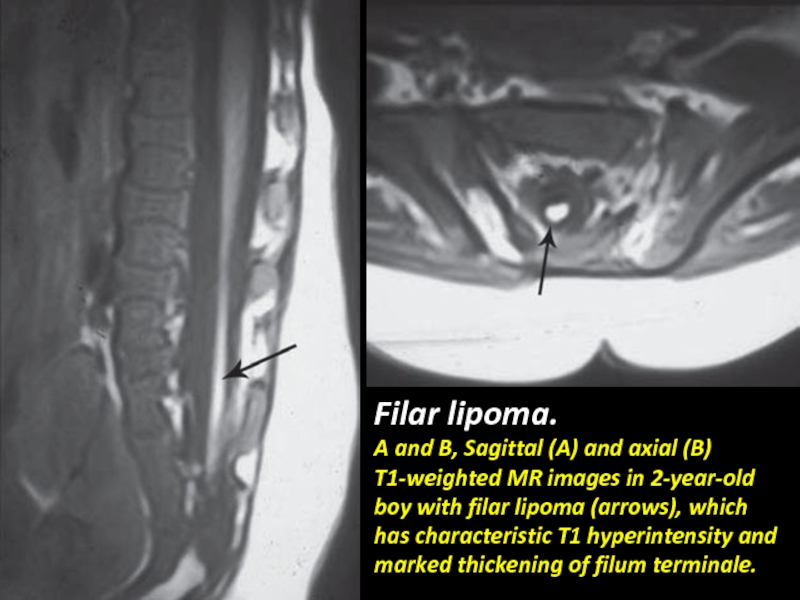
- 42. Filar lipoma. A and B, Sagittal (A)
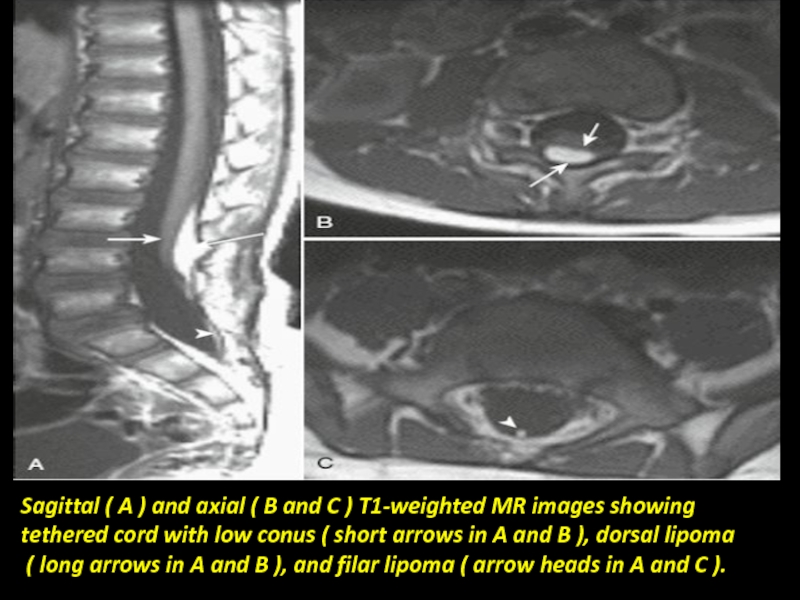
- 43. Sagittal ( A ) and axial (
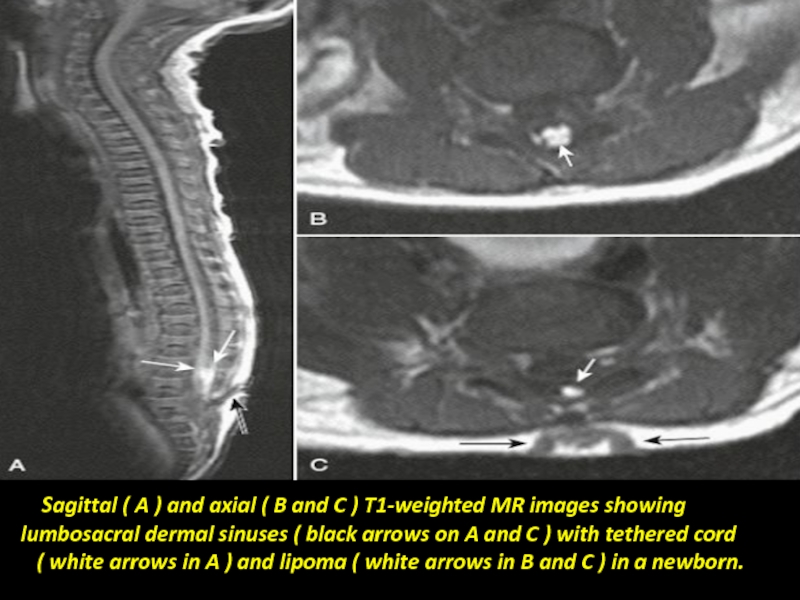
- 44. Sagittal ( A ) and
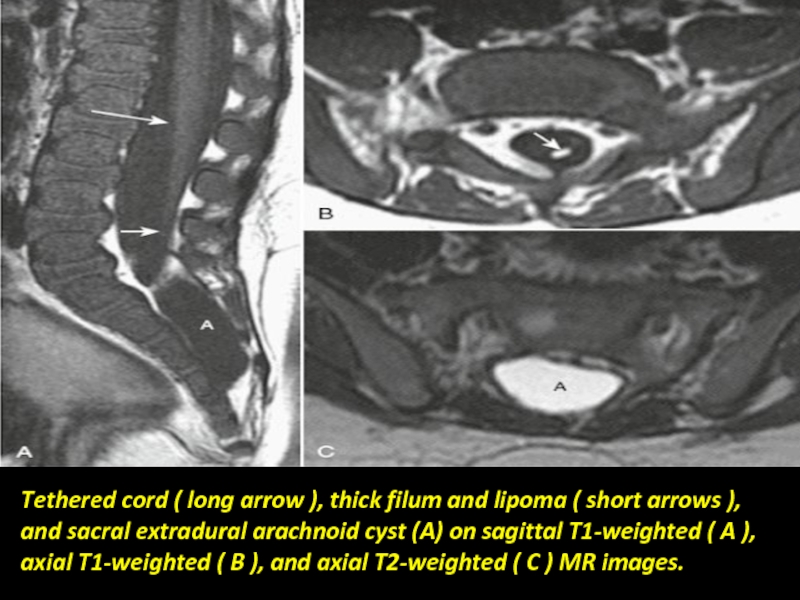
- 45. Tethered cord ( long arrow ), thick
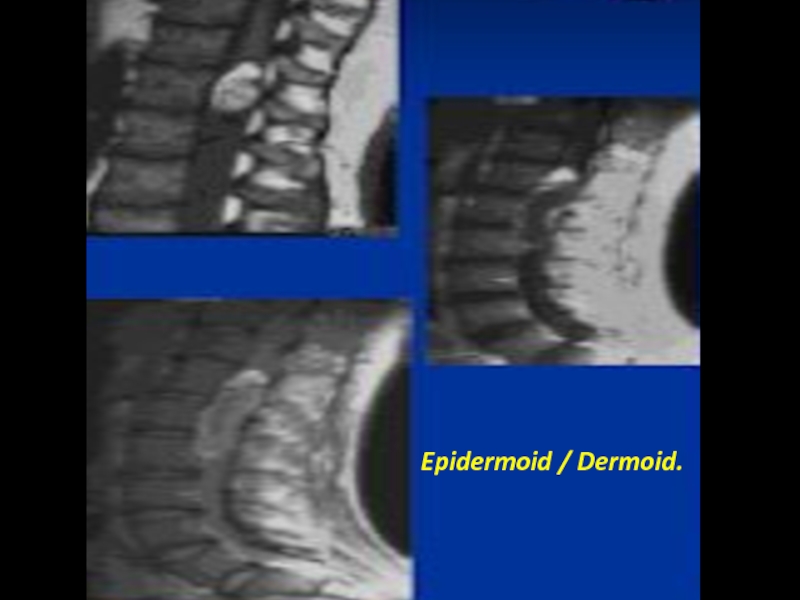
- 47. Epidermoid / Dermoid.
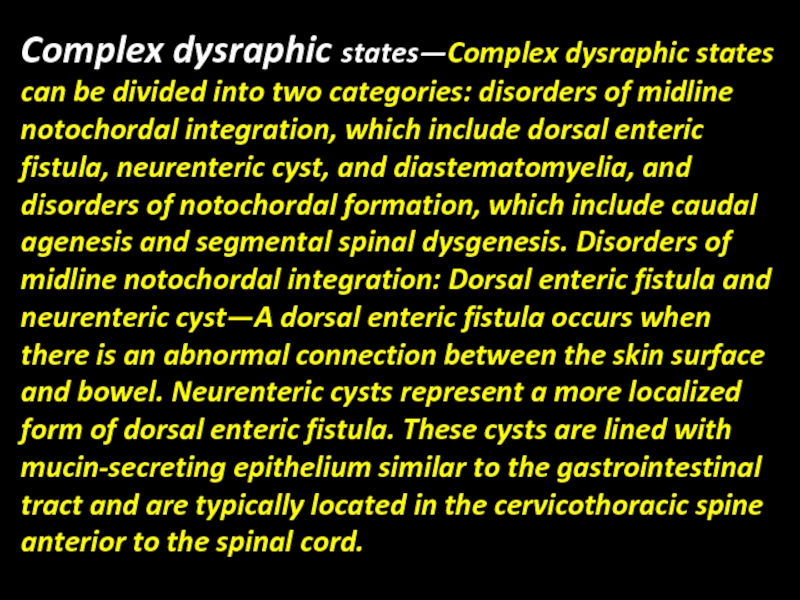
- 48. Complex dysraphic states—Complex dysraphic states can be
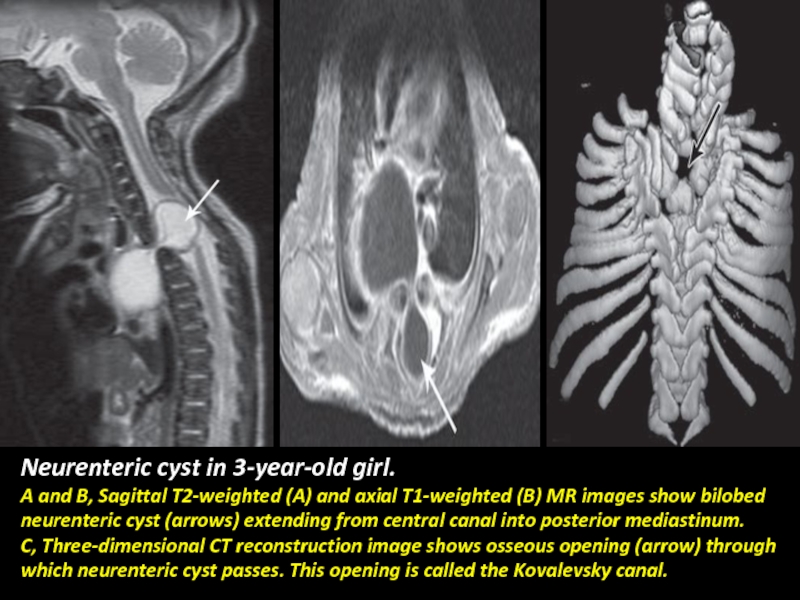
- 49. Neurenteric cyst in 3-year-old girl. A and
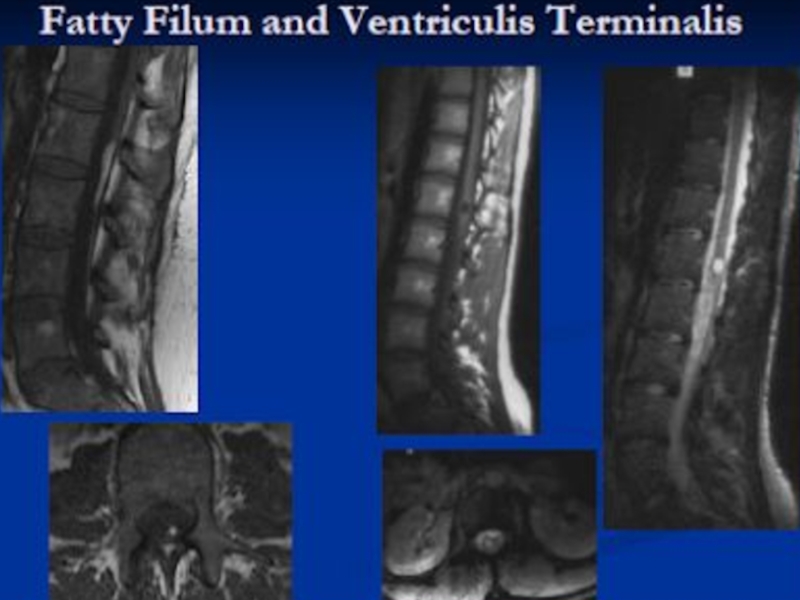
- 50. Terminal ventricle: Persistence of a small, ependymal
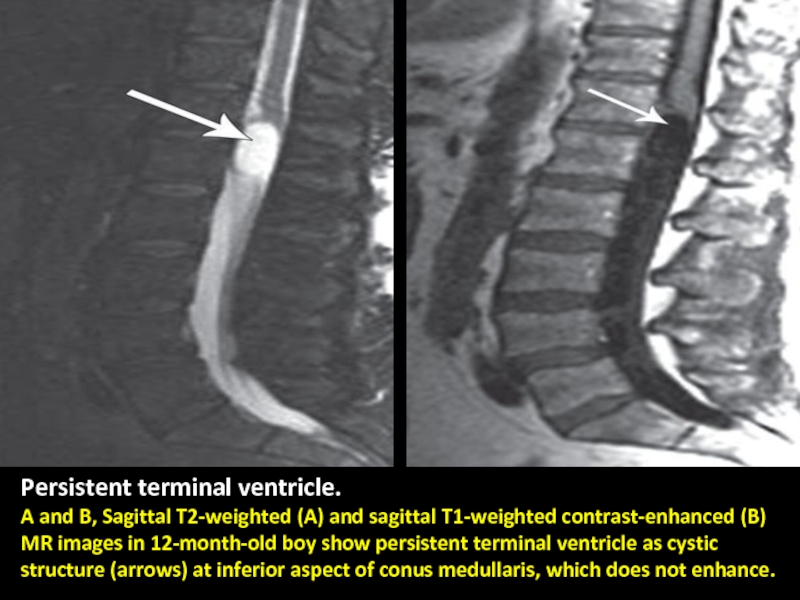
- 51. Persistent terminal ventricle. A and B, Sagittal
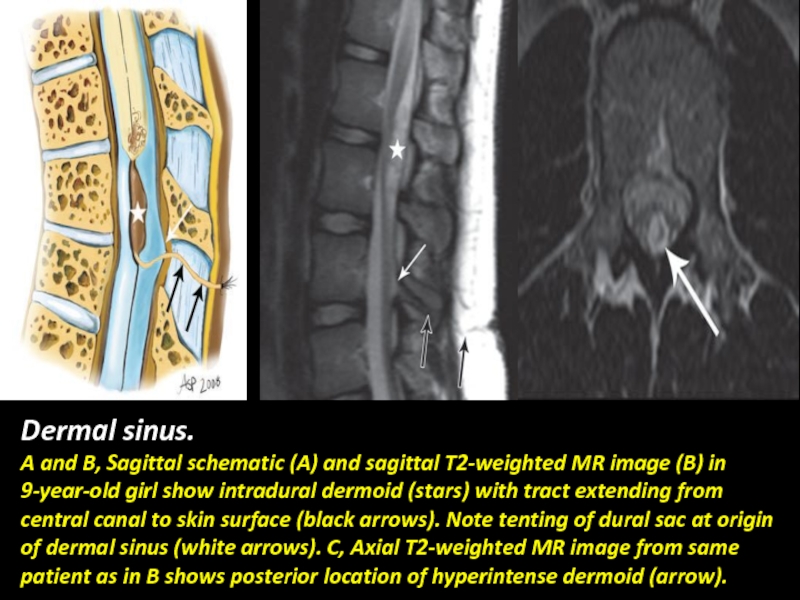
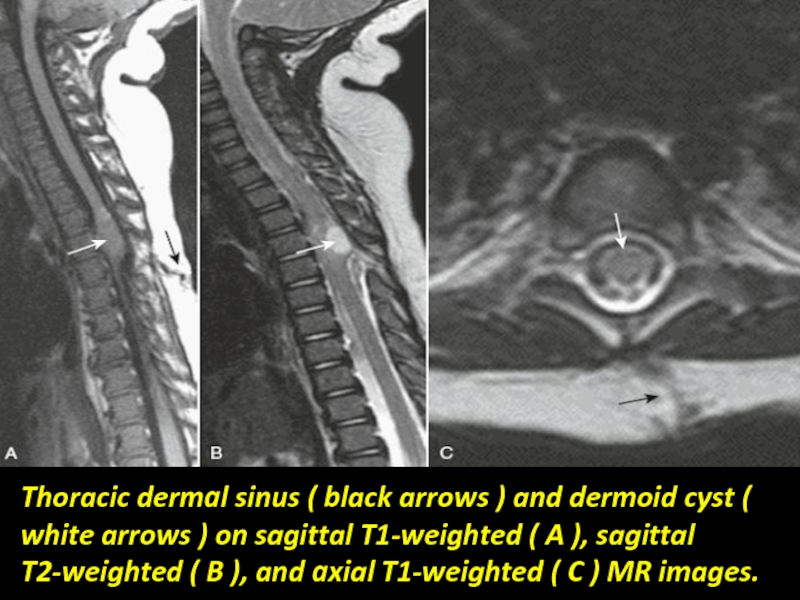
- 53. Dermal sinus. A and B, Sagittal schematic
- 54. Thoracic dermal sinus ( black arrows )
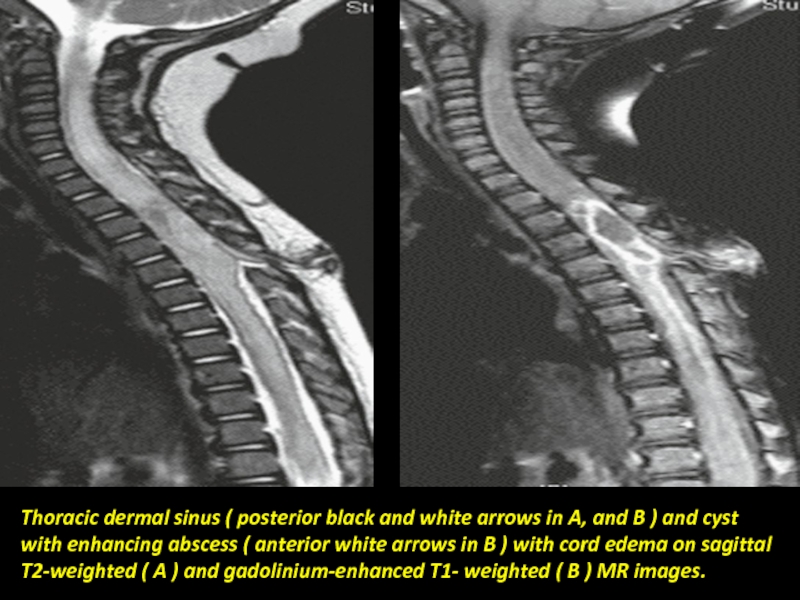
- 55. Thoracic dermal sinus ( posterior black and
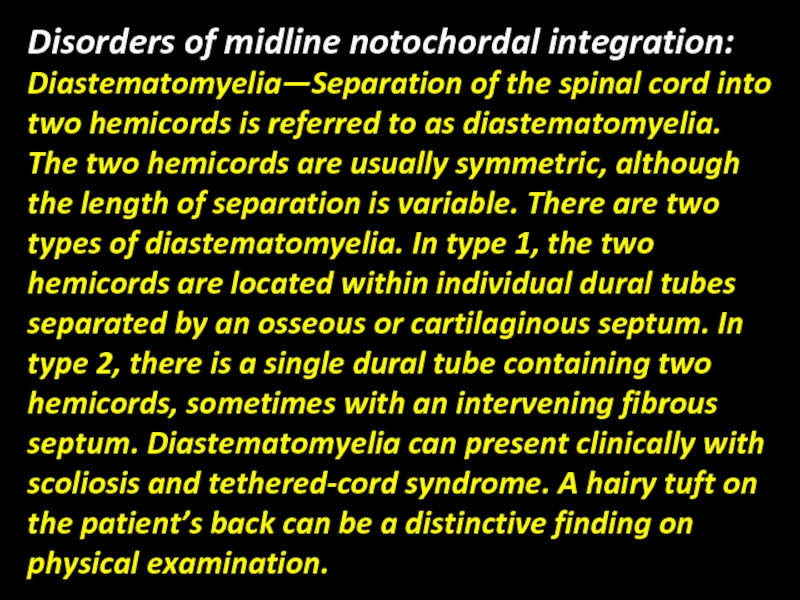
- 56. Disorders of midline notochordal integration: Diastematomyelia—Separation of
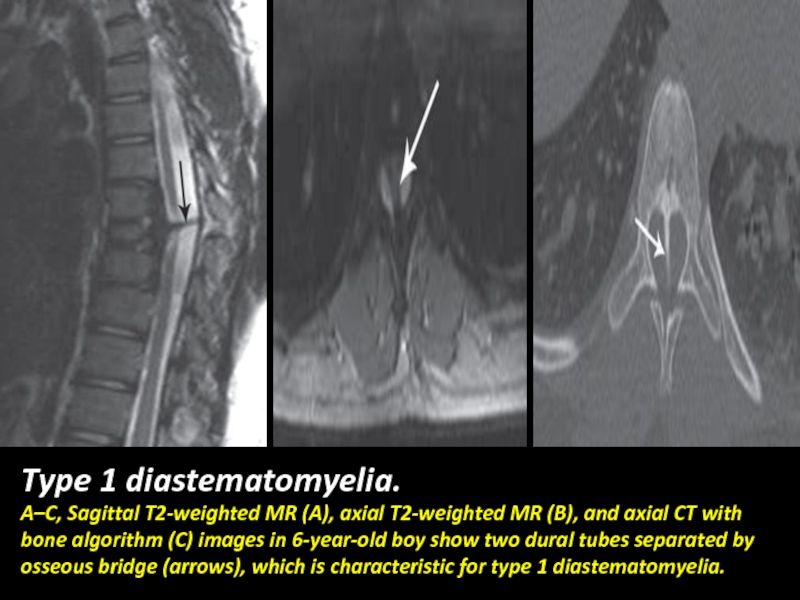
- 57. Type 1 diastematomyelia. A–C, Sagittal T2-weighted MR
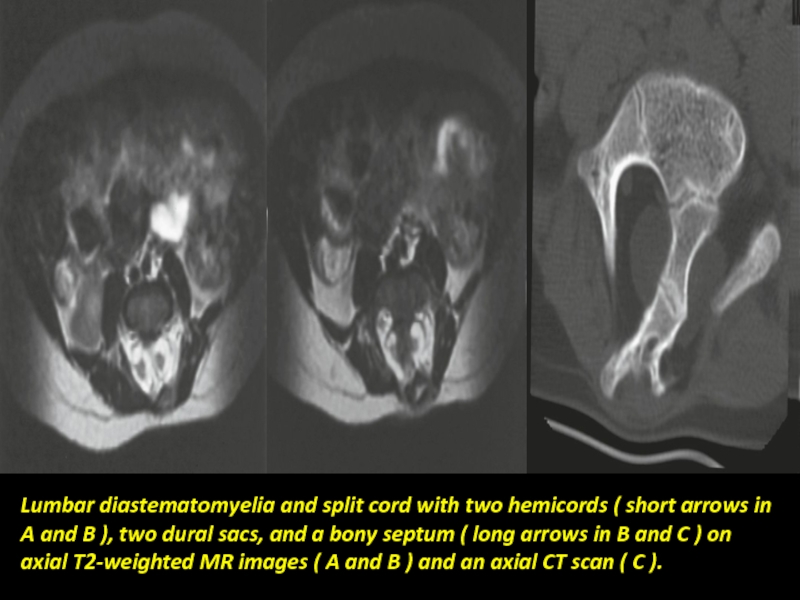
- 58. Lumbar diastematomyelia and split cord with two
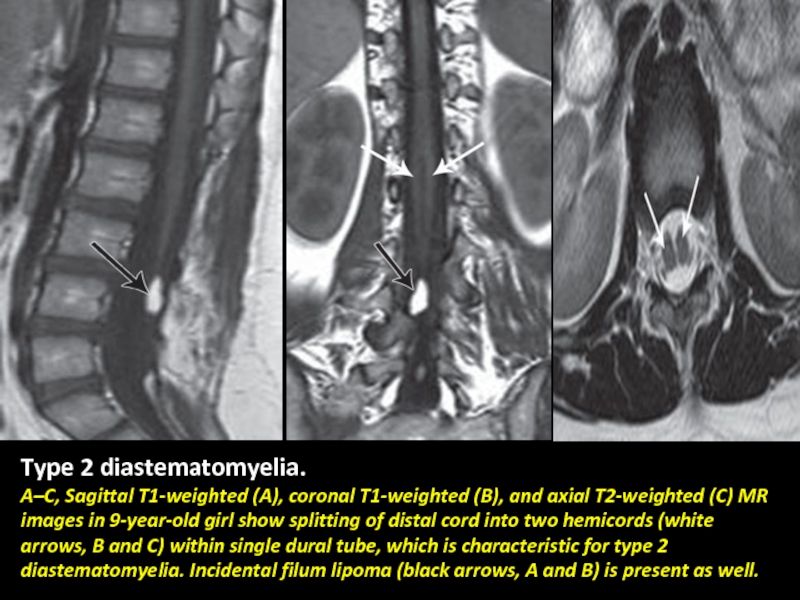
- 59. Type 2 diastematomyelia. A–C, Sagittal T1-weighted (A),
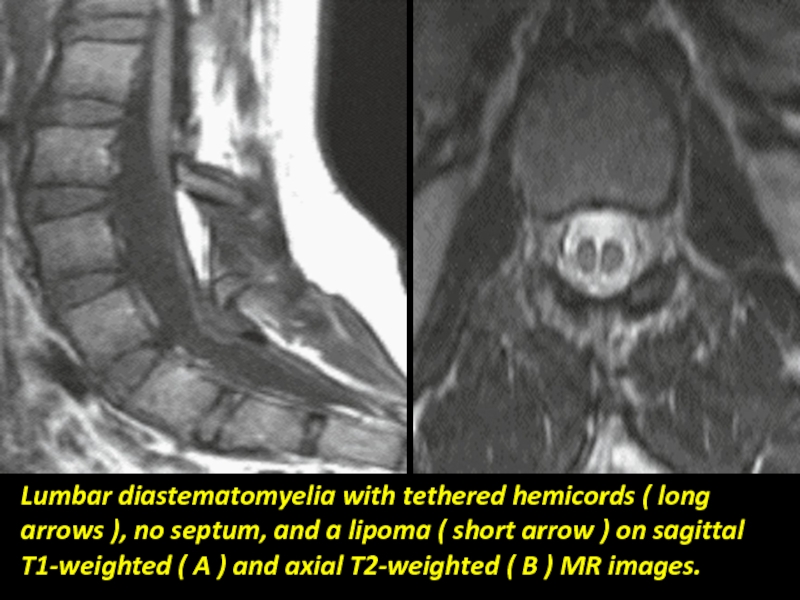
- 60. Lumbar diastematomyelia with tethered hemicords ( long
- 61. Disorders of notochordal formation: Caudal agenesis—Caudal agenesis
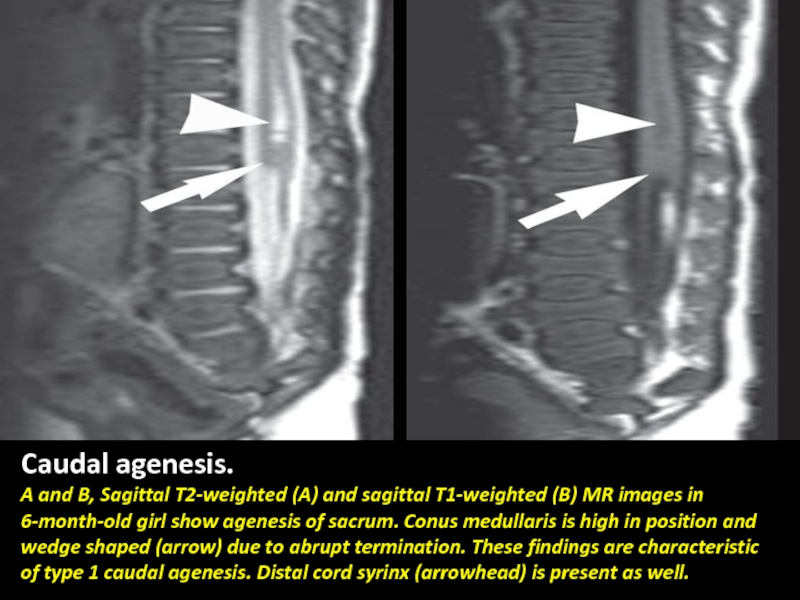
- 62. Caudal agenesis. A and B, Sagittal T2-weighted
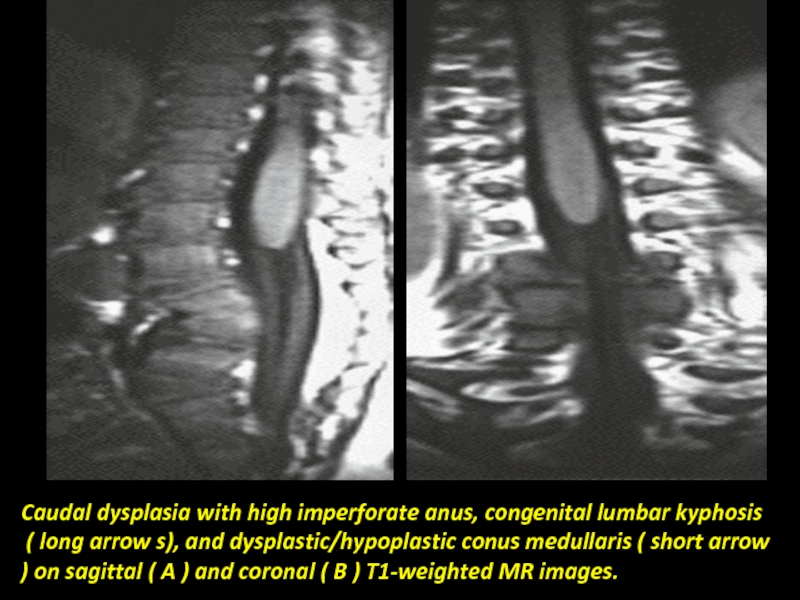
- 63. Caudal dysplasia with high imperforate anus, congenital
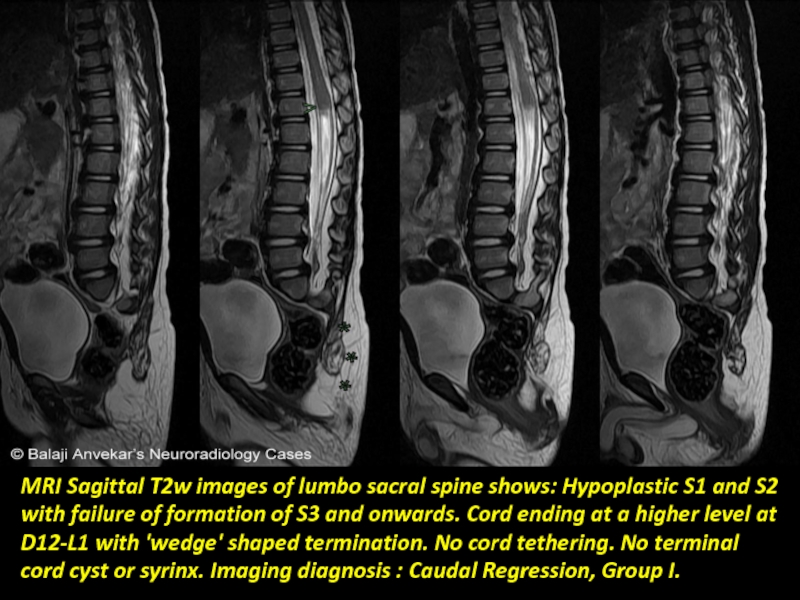
- 64. MRI Sagittal T2w images of lumbo sacral
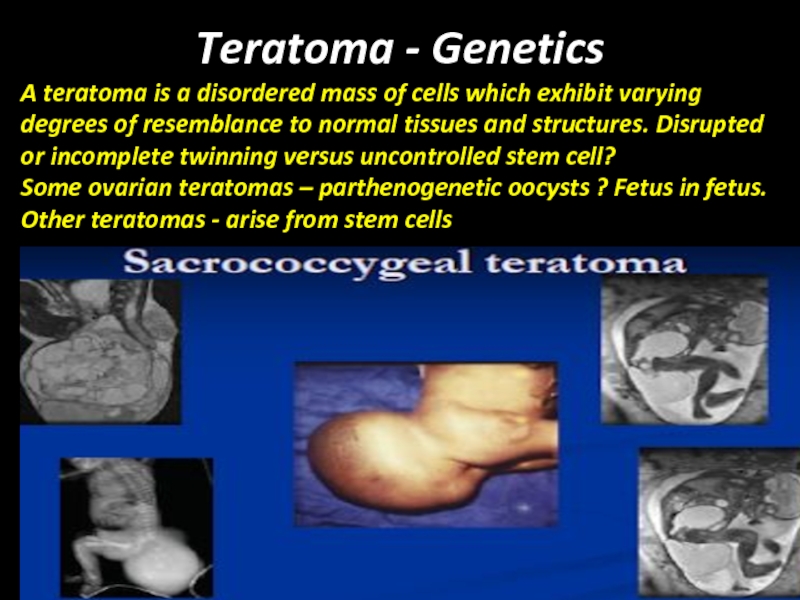
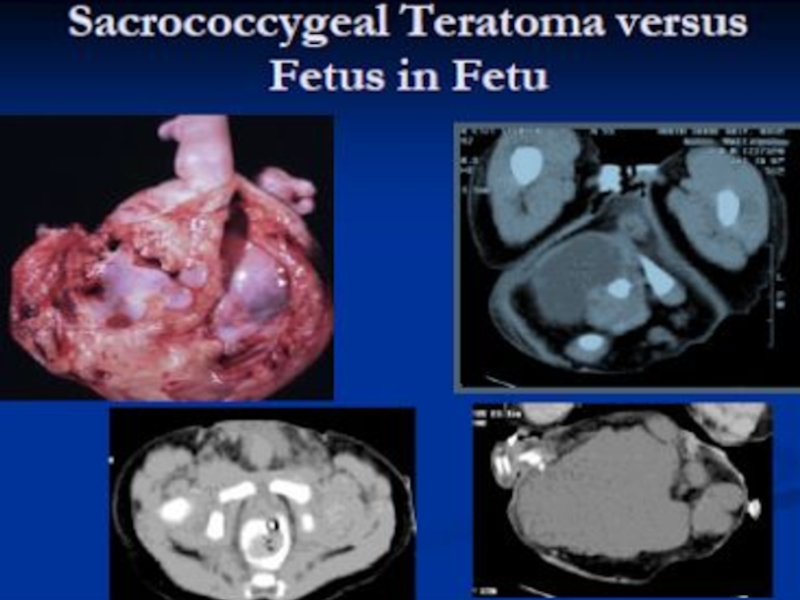
- 65. Teratoma - Genetics A teratoma is
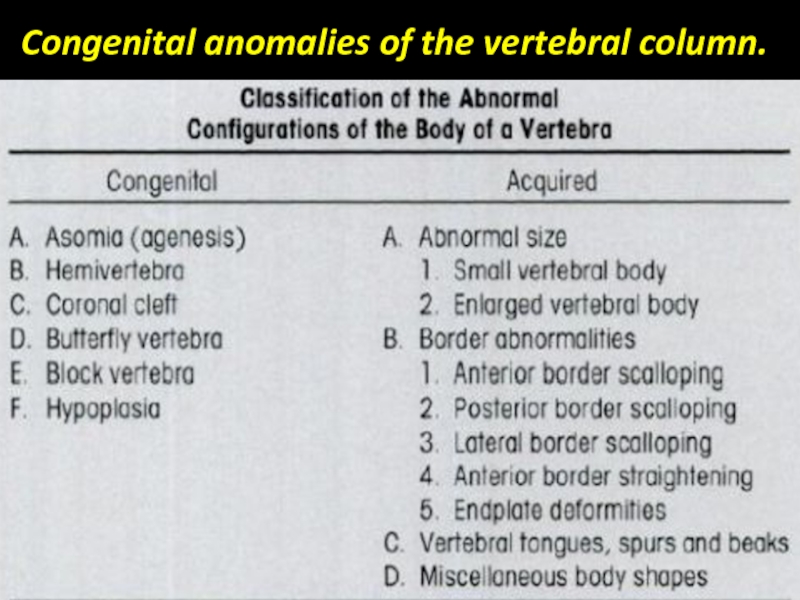
- 68. Congenital anomalies of the vertebral column.
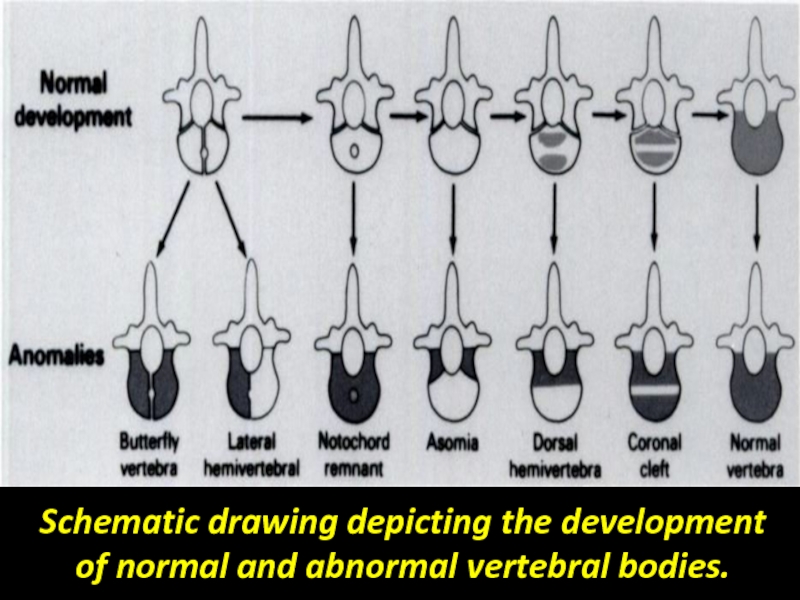
- 69. Schematic drawing depicting the development of normal and abnormal vertebral bodies.
- 70. Asomia Congenital absence of the body of
- 71. Butterfly vertebra. Coronal reformatted (A) and anterior
- 72. Butterfly vertebra.
- 73. Block vertebra. Sagittal reformatted (A) and anterior
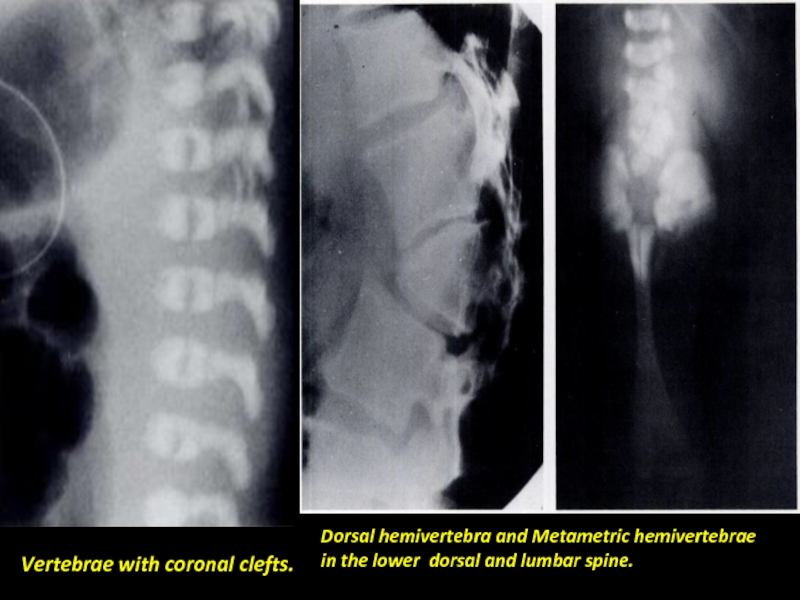
- 74. Dorsal hemivertebra and Metametric hemivertebrae in the
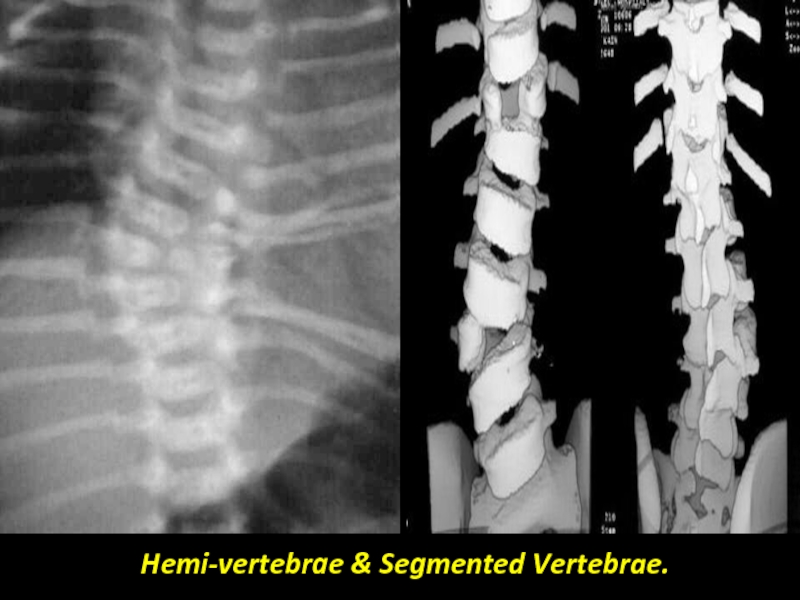
- 75. Hemi-vertebrae & Segmented Vertebrae.
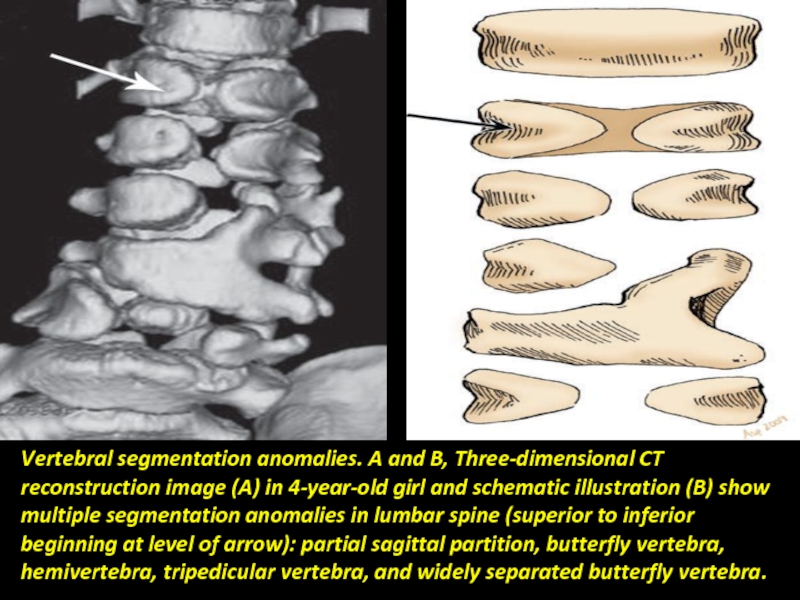
- 76. Vertebral segmentation anomalies. A and B, Three-dimensional
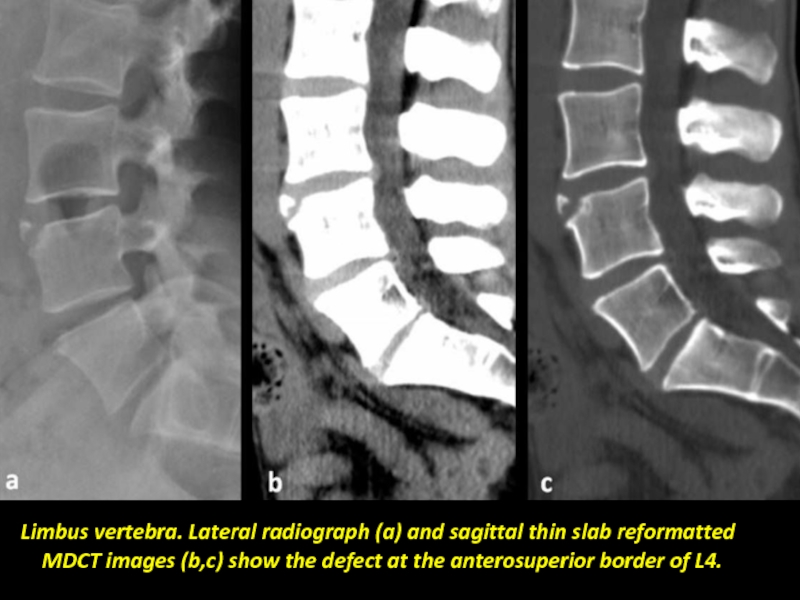
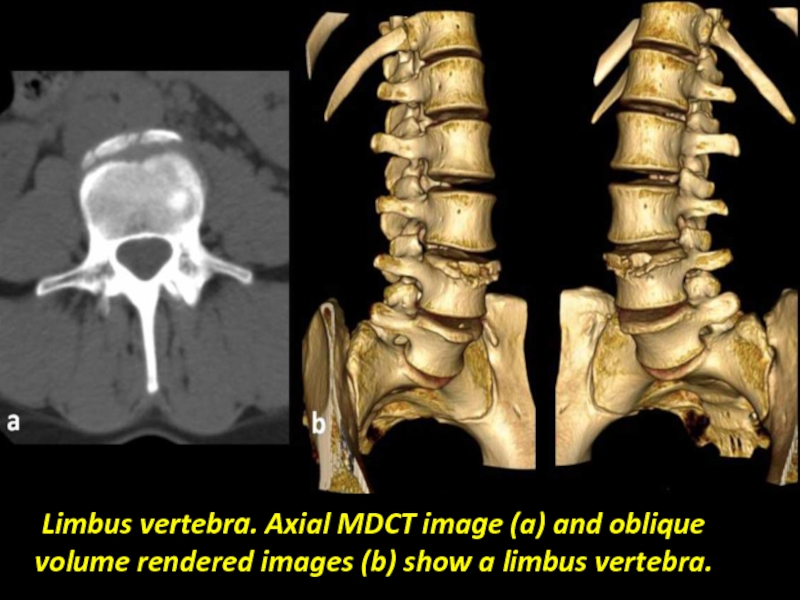
- 77. Limbus vertebra. Lateral radiograph (a) and sagittal
- 78. Limbus vertebra. Axial MDCT image (a)
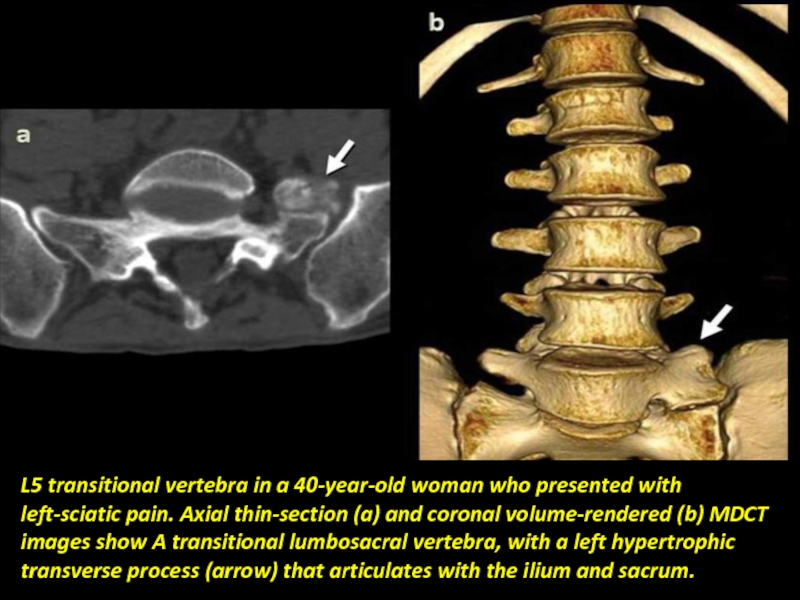
- 79. L5 transitional vertebra in a 40-year-old woman
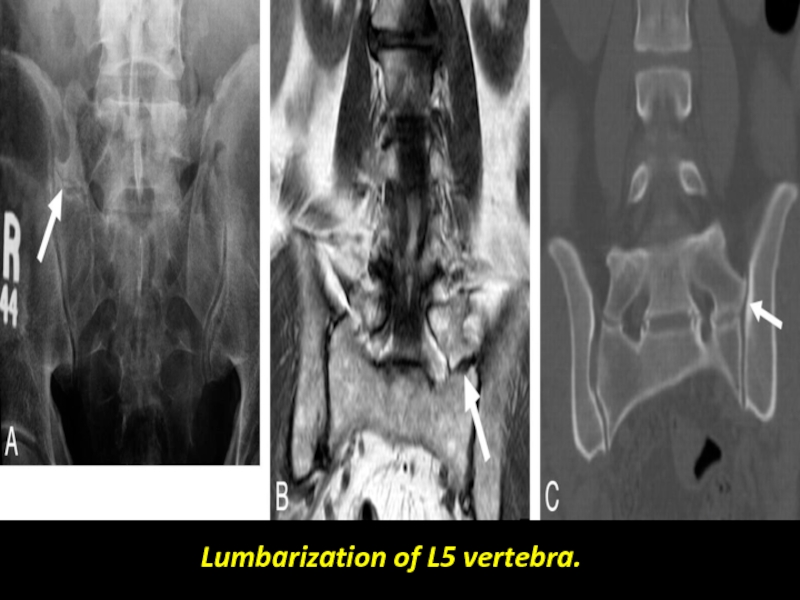
- 80. Lumbarization of L5 vertebra.
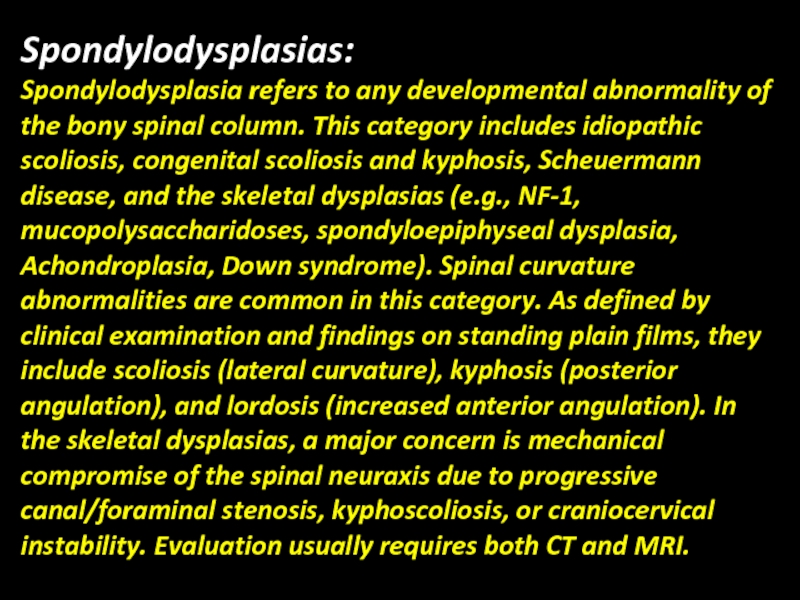
- 81. Spondylodysplasias: Spondylodysplasia refers to any developmental abnormality
- 82. Spondylodysplasias Idiopathic scoliosis. Congenital scoliosis and kyphosis.
- 83. Idiopathic Scoliosis Idiopathic scoliosis is the most
- 84. Idiopathic scoliosis with typical rightward thoracic lateral
- 85. A and B, Congenital lumbar scoliosis with
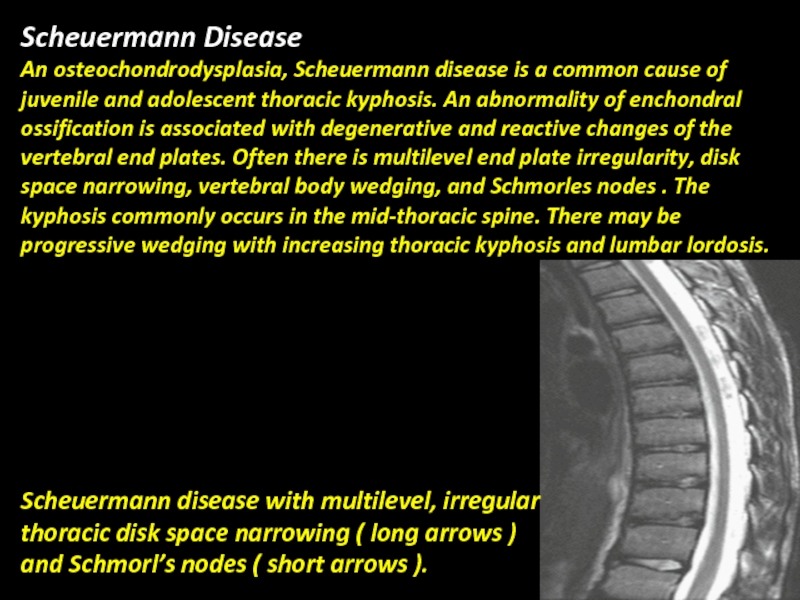
- 86. Scheuermann Disease An osteochondrodysplasia, Scheuermann disease is
- 87. Neurofibromatosis Type 1: NF-1 is a common
- 88. A, Neurofibromatosis-1 with short-segment right lumbar scoliosis
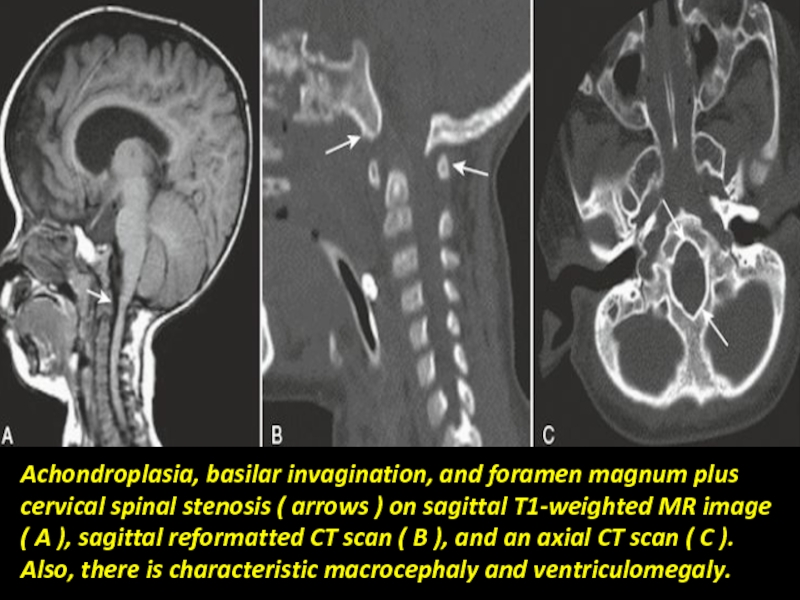
- 89. Achondroplasia Achondroplasia is one of the osteochondrodysplasia
- 90. Achondroplasia, basilar invagination, and foramen magnum plus
- 91. Mucopolysaccharidosis: Mucopolysaccharidosis may be associated with craniocervical
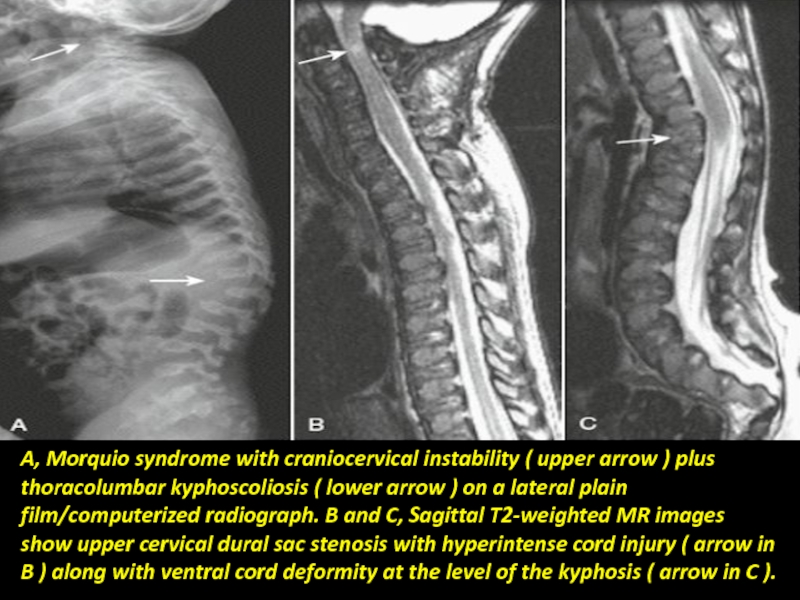
- 92. A, Morquio syndrome with craniocervical instability (
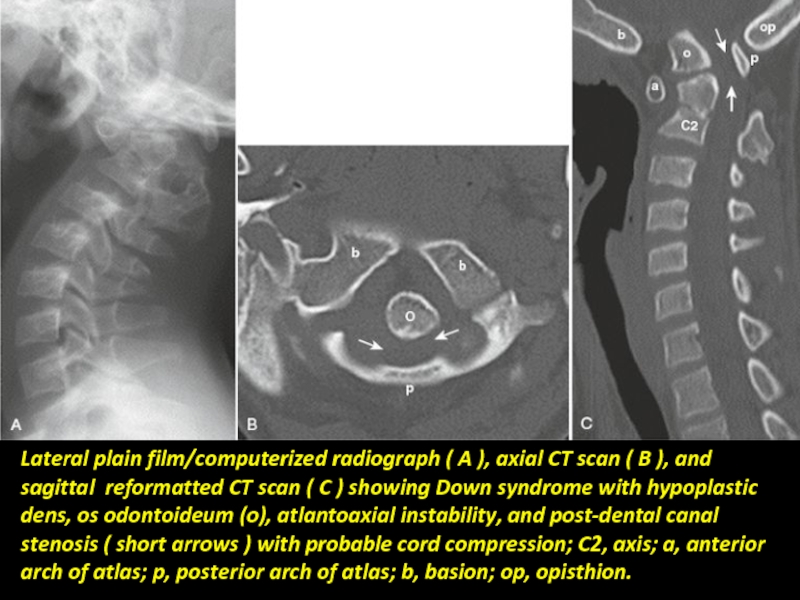
- 93. Lateral plain film/computerized radiograph ( A ),
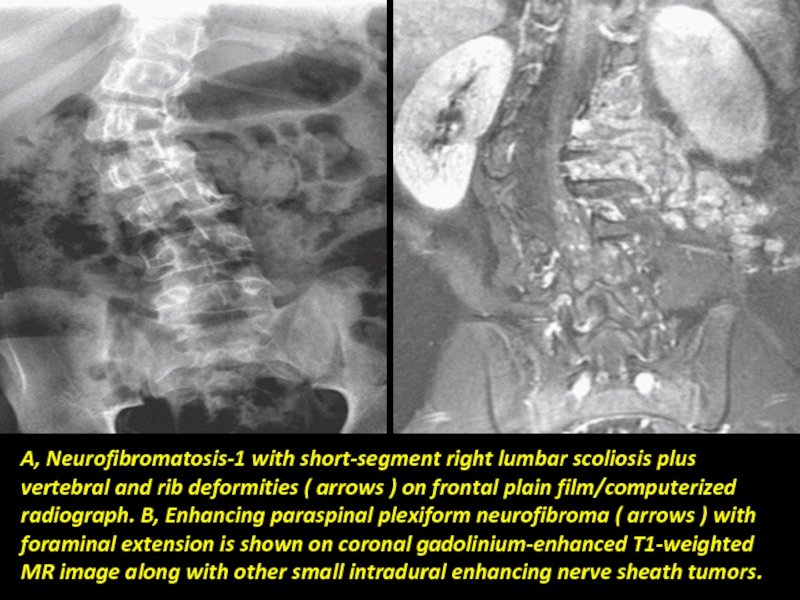
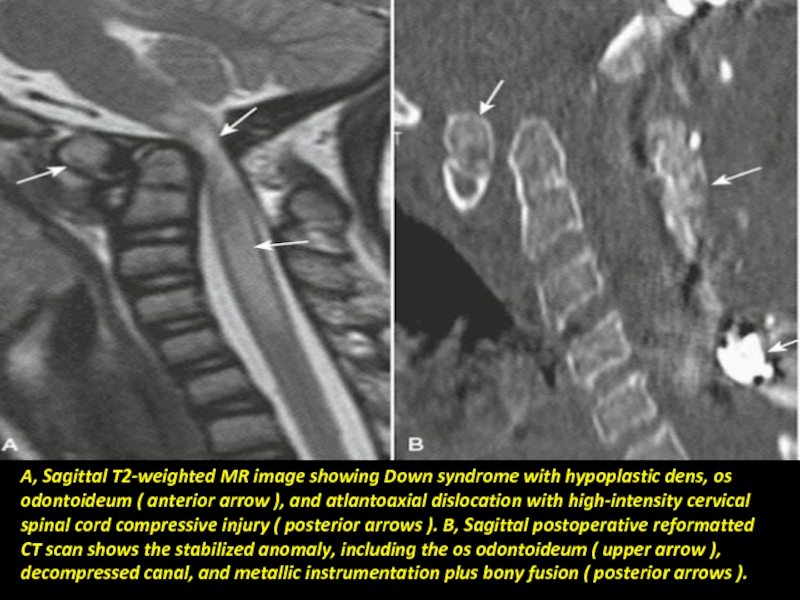
- 94. A, Sagittal T2-weighted MR image showing Down
- 95. Basilar Invagination: Basilar invagination refers to an
- 96. Basilar invagination and Chiari I malformation on
- 97. Klippel-Feil Anomaly and Syndrome: The Klippel-Feil anomaly
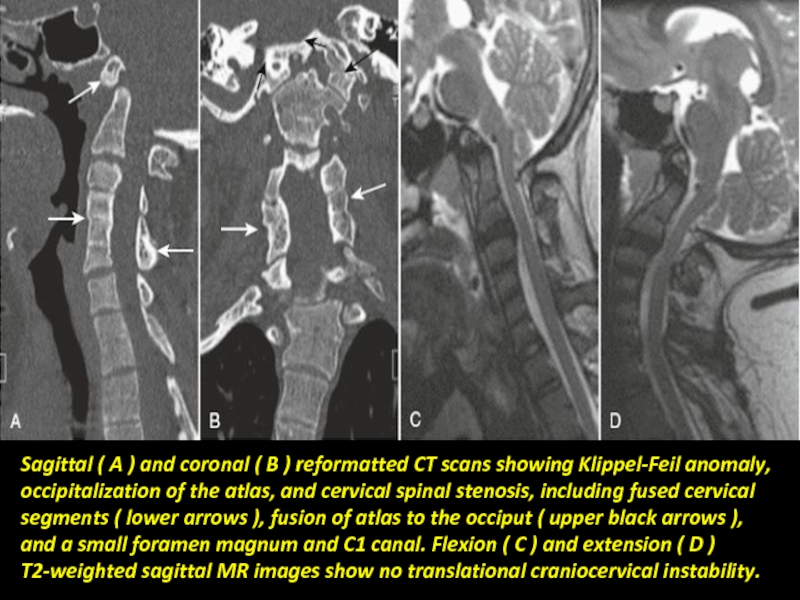
- 98. Sagittal ( A ) and coronal (
- 99. Craniocervical Instability: Craniocervical instability includes translational or
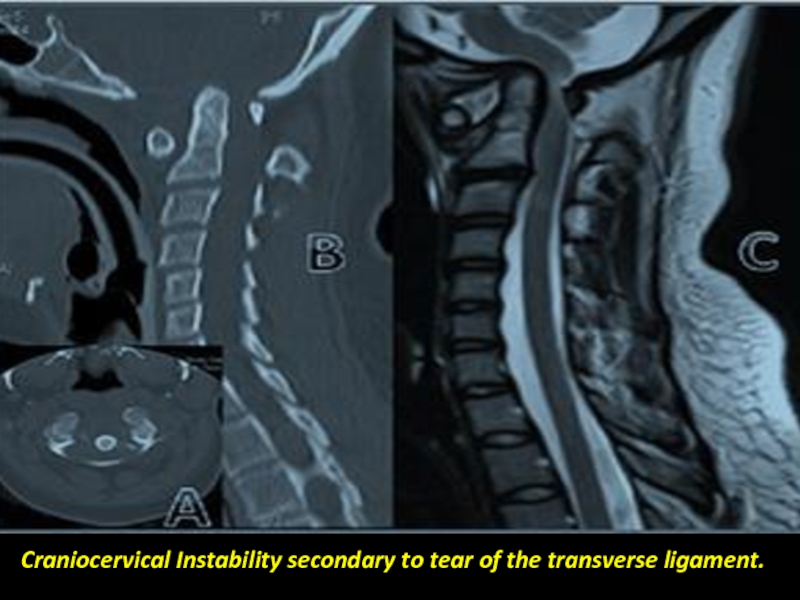
- 100. Craniocervical Instability secondary to tear of the transverse ligament.
- 101. Congenital spondylolisthesis Spondylolisthesis is a condition that
- 103. Spinal Vascular Anomalies: Vascular anomalies of childhood
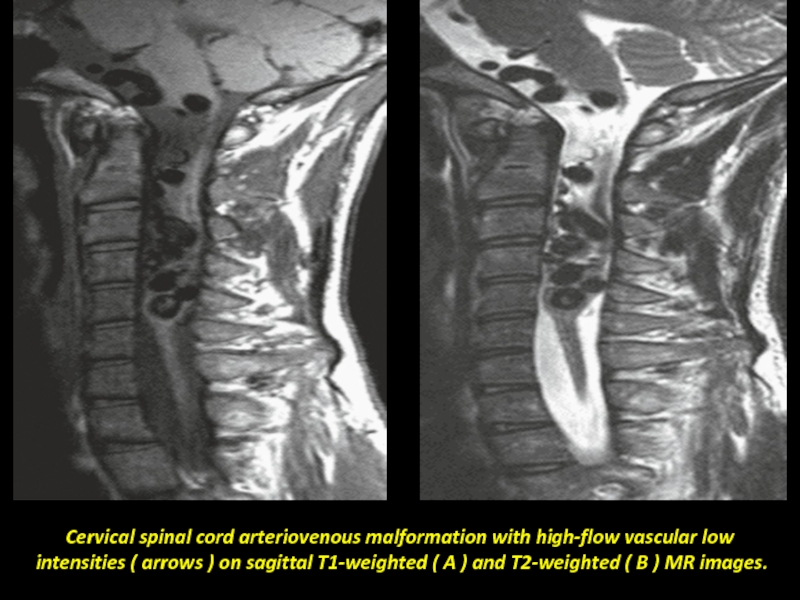
- 104. Cervical spinal cord arteriovenous malformation with high-flow
- 105. Spina bifida (Latin : "split spine") is
- 106. Spina bifida of lumbar and cervical spines.
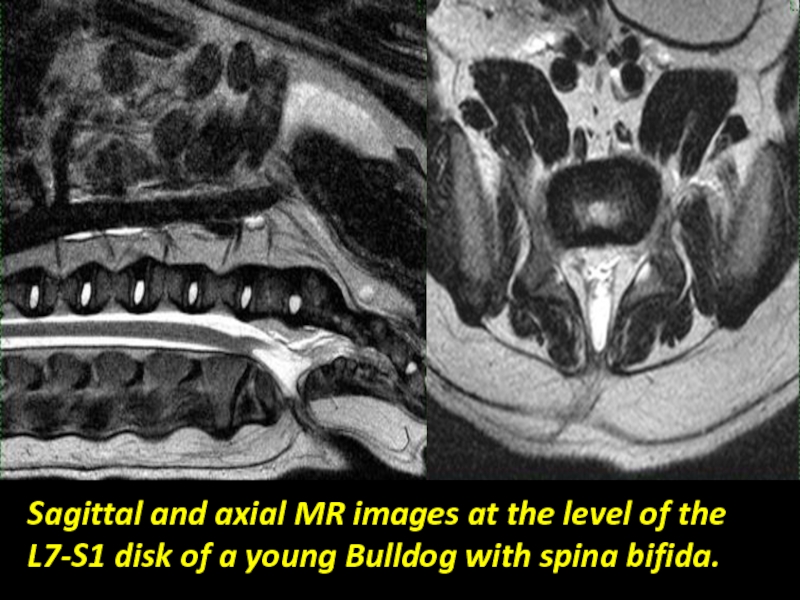
- 108. Sagittal and axial MR images at the
- 109. Conclusion Congenital malformations of the spine and
- 110. Thank You.
Слайд 1Radiological imaging of congenital anomalies of the spine and spinal cord.
Dr/
Слайд 2Congenital abnormalities of the spine and spinal cord are referred to
Etiology: Multifactorial, Genetic, environmental factor and folic acid deficiency.
The most common congenital anomalies is spinal dysraphism and the caudal spinal anomalies.
The diagnosis is either prenatally by ultrasound, at birth, in the early childhood and in adulthood.
Слайд 3Radiological imaging techniques:
Plain Radiography.
Ultrasonography.
Computed tomography(CT Scan).
Magnetic resonance imaging(MRI).
Nuclear Imaging.
Слайд 4Spinal Cord Development
Spinal development can be summarized in three basic embryologic
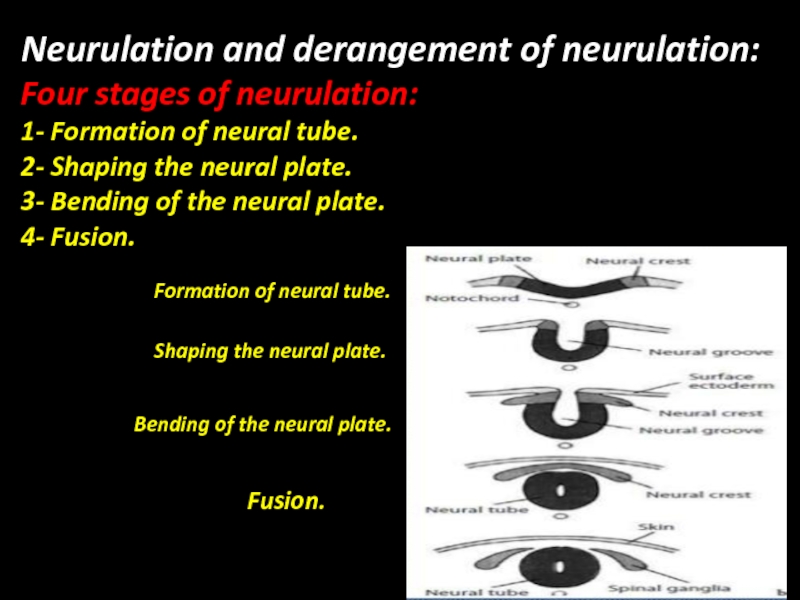
Слайд 6Neurulation and derangement of neurulation:
Four stages of neurulation:
1- Formation of neural
2- Shaping the neural plate.
3- Bending of the neural plate.
4- Fusion.
Formation of neural tube.
Shaping the neural plate.
Bending of the neural plate.
Fusion.
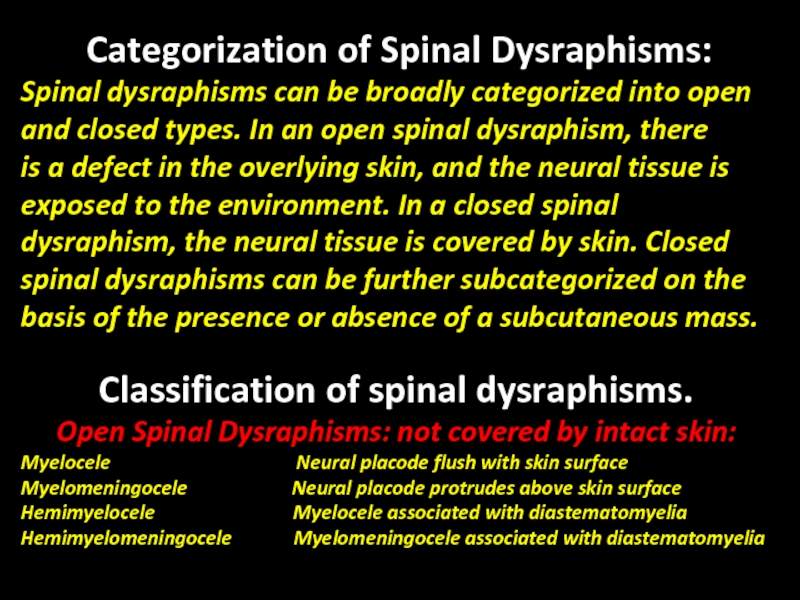
Слайд 7Categorization of Spinal Dysraphisms:
Spinal dysraphisms can be broadly categorized into open
and
is a defect in the overlying skin, and the neural tissue is exposed to the environment. In a closed spinal dysraphism, the neural tissue is covered by skin. Closed spinal dysraphisms can be further subcategorized on the basis of the presence or absence of a subcutaneous mass.
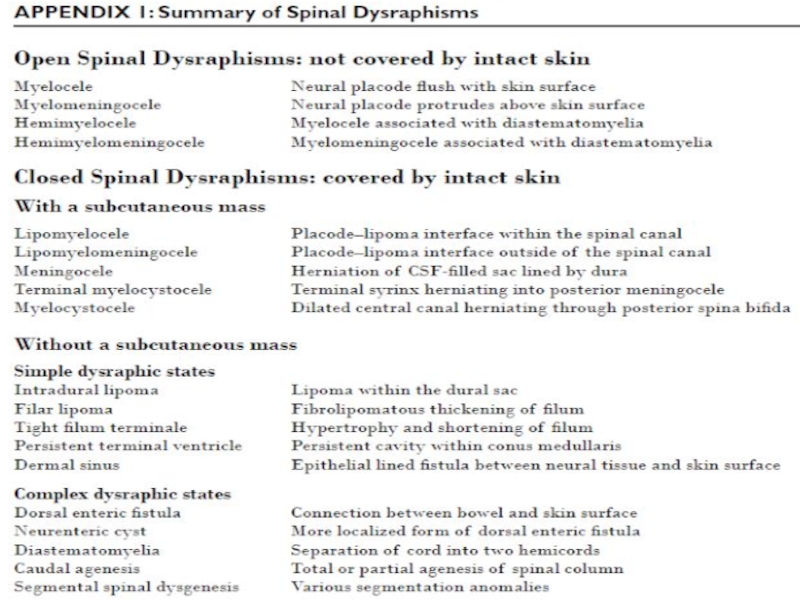
Classification of spinal dysraphisms.
Open Spinal Dysraphisms: not covered by intact skin:
Myelocele Neural placode flush with skin surface
Myelomeningocele Neural placode protrudes above skin surface
Hemimyelocele Myelocele associated with diastematomyelia
Hemimyelomeningocele Myelomeningocele associated with diastematomyelia
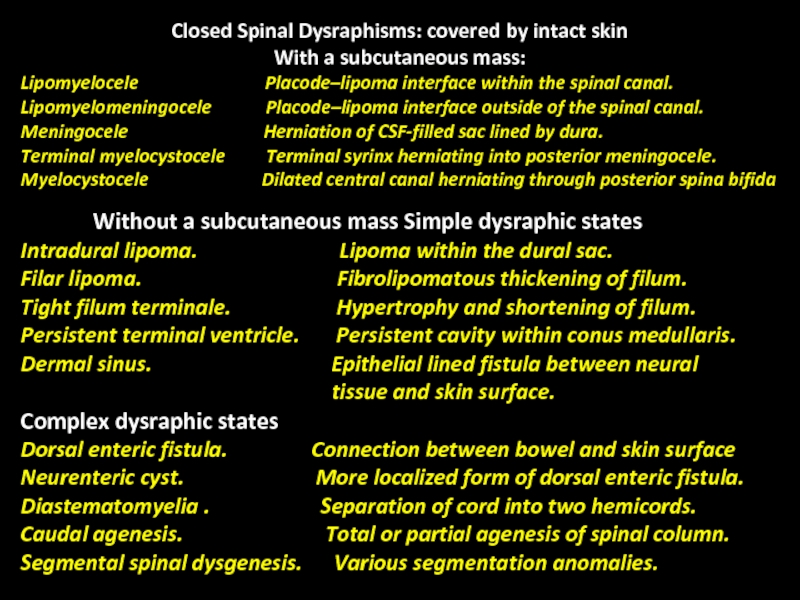
Слайд 8Closed Spinal Dysraphisms: covered by intact skin
With a subcutaneous mass:
Lipomyelocele
Lipomyelomeningocele Placode–lipoma interface outside of the spinal canal.
Meningocele Herniation of CSF-filled sac lined by dura.
Terminal myelocystocele Terminal syrinx herniating into posterior meningocele.
Myelocystocele Dilated central canal herniating through posterior spina bifida
Without a subcutaneous mass Simple dysraphic states
Intradural lipoma. Lipoma within the dural sac.
Filar lipoma. Fibrolipomatous thickening of filum.
Tight filum terminale. Hypertrophy and shortening of filum.
Persistent terminal ventricle. Persistent cavity within conus medullaris.
Dermal sinus. Epithelial lined fistula between neural
tissue and skin surface.
Complex dysraphic states
Dorsal enteric fistula. Connection between bowel and skin surface
Neurenteric cyst. More localized form of dorsal enteric fistula.
Diastematomyelia . Separation of cord into two hemicords.
Caudal agenesis. Total or partial agenesis of spinal column.
Segmental spinal dysgenesis. Various segmentation anomalies.
Слайд 9Open Spinal Dysraphisms:
Myelomeningocele and myelocele—Myelomeningoceles and
myeloceles are caused by defective closure
Слайд 10Deranged neurulation:
Spina Bifida aperta: Myelocele and myelomeningocele.
Spina bifida aperta designates those
Myelocele and Myelomeningocele
Both myelocele and myelomeningocele are the result of nondisjunction of the cutaneous ectoderm from the neural ectoderm and failure of neural tube closure. The nonneurulated cord or placode is exposed through a dural, bony, and cutaneous defect (i.e., myelocele; The dorsal and ventral nerve roots exit from the ventral surface of the placode. With associated dorsal protrusion of the ventral subarachnoid space, the myelodysplasia is termed a myelomeningocele. These defects commonly occur at the lumbar or sacral level. Occasionally there is an associated diastematomyelia (hemimyelomeningocele) or dermal sinus. These defects are surgically closed shortly after birth. Hydrocephalus is often present; if so, shunting is established early. Subsequently, patients who have undergone such procedures may sac stenosis, progressive scoliosis, and cord ischemia or infarction.
Слайд 11Myelomeningocele.
A, Axial schematic of myelomeningocele shows neural placode (star) protruding above
B, Axial T2-weighted MR image in 1-day-old boy shows neural placode (black arrow) extending above skin surface due to expansion of underlying subarachnoid space
(white arrow), which is characteristic of myelomeningocele.
C, Sagittal T2-weighted MR image from same patient as in B with myelomeningocele shows neural placode (white arrow) protruding above skin surface due to expansion
of underlying subarachnoid space (black arrow).
A
B
C
Слайд 12Myelocele.
A, Axial schematic of myelocele shows neural placode (arrow) flush with
B, Axial T2-weighted MR image in 1-day-old girl shows exposed neural placode (arrow) that is flush with skin surface, consistent with myelocele. There is no expansion of underlying subarachnoid space.
A
B
Слайд 13Chiari malformation, also known as Arnold–Chiari malformation, is a malformation of
Classification:
In the late 19th century, Austrian pathologist Hans Chiari described seemingly related anomalies of the hindbrain; the so-called Chiari malformations I, II and III. Later, other investigators added a fourth (Chiari IV) malformation. The scale of severity is rated I - IV, with IV being the most severe. Types III and IV are very rare.
Слайд 14Chiaric-1 malformation:
A congenital malformation. Is generally asymptomatic during childhood, but often
Слайд 18 Chiari-11 malformation:
Usually accompanied by a lumbar or lumbosacral myelomeningocele with
Слайд 19Fetal T2-weighted MR images. A, Chiari II malformation ( arrows )
Слайд 20Chiari II malformation ( arrows in A ) and lumbosacral myelomeningocele
Слайд 22Type II Chiari malformation in a 14-month-old child. Sagittal T1-weighted images
Слайд 23Chiari-111 malformation:
It is associated with an occipital encephalocele containing a variety
Characterized by a lack of cerebellar development in which the cerebellum and brain stem lie within the posterior fossa with no relation to the foramen magnum. Associated with hypoplasia. Equivalent to primary cerebellar agenesis.
Chiari-111 malformation:
Слайд 28Closed Spinal Dysraphisms With a Subcutaneous Mass Lipomas with a dural
Слайд 29Meningocele—Herniation of a CSF-filled sac lined by dura and arachnoid mater
Слайд 30Lipomyelocele.
A, Axial schematic of lipomyelocele shows placode–lipoma interface (arrow) lies within
Слайд 31Lipomyelocele with placode ( short arrows ), lipoma (L), and caudal
Слайд 32Lumbosacral lipomyelocele with caudal and presacral lipomas (L) and hydrosyringomyelia
Слайд 33Posterior meningocele.
A, Sagittal T1-weighted MR image in in 12-month-old girl shows
B, Sagittal T2-weighted MR image in 5-year-old boy shows large posterior meningocele (arrow) in cervical region. C, Sagittal T2-weighted MR image in 30-month-old girl shows small posterior meningocele (arrow) in lumbar region.
Слайд 34Meningocele.
A and B, Sagittal (A) and axial (B) T2-weighted MR images
Слайд 35Sagittal ( A ) and axial ( B and C )
Слайд 37Terminal myelocystocele—Herniation of large terminal syrinx (syringocele) into a posterior meningocele
Myelocystocele—A non-terminal myelocystocele occurs when a dilated central canal herniates through a posterior spina bifida defect. Myelocystoceles are covered with skin and can occur anywhere but are most commonly seen in the cervical or cervicothoracic regions.
Слайд 38Terminal myelocystocele.
A, Sagittal schematic of terminal myelocystocele shows terminal syrinx (star)
Слайд 40Closed Spinal Dysraphisms Without a Subcutaneous Mass Closed spinal dysraphisms without
Слайд 41The Tethered Cord Syndrome:
Also known as “tight filum terminale syndrome,” tethered
diastematomyelia. The thickened filum may also terminate in a lipoma or dermoid-epidermoid. The filar abnormality is usually best demonstrated on axial T 1 -weighted and T 2 -weighted MRI.
Слайд 42Filar lipoma.
A and B, Sagittal (A) and axial (B) T1-weighted MR
marked thickening of filum terminale.
Слайд 43Sagittal ( A ) and axial ( B and C )
( long arrows in A and B ), and filar lipoma ( arrow heads in A and C ).
Слайд 44 Sagittal ( A ) and axial ( B and
( white arrows in A ) and lipoma ( white arrows in B and C ) in a newborn.
Слайд 45Tethered cord ( long arrow ), thick filum and lipoma (
Слайд 48Complex dysraphic states—Complex dysraphic states can be divided into two categories:
Слайд 49Neurenteric cyst in 3-year-old girl.
A and B, Sagittal T2-weighted (A) and
C, Three-dimensional CT reconstruction image shows osseous opening (arrow) through which neurenteric cyst passes. This opening is called the Kovalevsky canal.
Слайд 50Terminal ventricle: Persistence of a small, ependymal lined cavity within the
A dermal sinus is an epithelial lined fistula that connects neural tissue or meninges to the skin surface. It occurs most frequently in the lumbosacral region and is often associated with a spinal dermoid at the level of the cauda equina or conus medullaris. Clinically, patients present with a midline dimple and may also have an associated hairy nevus, hyperpigmented patch, or capillary hemangioma. Surgical repair is of great importance because the fistulous connection between neural tissue and the skin surface can result in infectious complications such as meningitis and abscess.
Слайд 51Persistent terminal ventricle.
A and B, Sagittal T2-weighted (A) and sagittal T1-weighted
Слайд 53Dermal sinus.
A and B, Sagittal schematic (A) and sagittal T2-weighted MR
Слайд 54Thoracic dermal sinus ( black arrows ) and dermoid cyst (
Слайд 55Thoracic dermal sinus ( posterior black and white arrows in A,
Слайд 56Disorders of midline notochordal integration: Diastematomyelia—Separation of the spinal cord into
Слайд 57Type 1 diastematomyelia.
A–C, Sagittal T2-weighted MR (A), axial T2-weighted MR (B),
Слайд 58Lumbar diastematomyelia and split cord with two hemicords ( short arrows
Слайд 59Type 2 diastematomyelia.
A–C, Sagittal T1-weighted (A), coronal T1-weighted (B), and axial
arrows, B and C) within single dural tube, which is characteristic for type 2 diastematomyelia. Incidental filum lipoma (black arrows, A and B) is present as well.
Слайд 60Lumbar diastematomyelia with tethered hemicords ( long arrows ), no septum,
Слайд 61Disorders of notochordal formation: Caudal agenesis—Caudal agenesis refers to total or
Segmental spinal dysgenesis—The clinical–radiologic definition
of segmental spinal dysgenesis includes several entities: segmental agenesis or dysgenesis of the thoracic or lumbar spine, segmental abnormality of the spinal cord or nerve roots, congenital paraparesis or paraplegia, and congenital lower limb deformities. Three-dimensional CT reconstructions can be helpful in showing various vertebral segmentation anomalies
Слайд 62Caudal agenesis.
A and B, Sagittal T2-weighted (A) and sagittal T1-weighted (B)
Слайд 63Caudal dysplasia with high imperforate anus, congenital lumbar kyphosis
( long
Слайд 64MRI Sagittal T2w images of lumbo sacral spine shows: Hypoplastic S1
Слайд 65Teratoma - Genetics
A teratoma is a disordered mass of cells
Some ovarian teratomas – parthenogenetic oocysts ? Fetus in fetus. Other teratomas - arise from stem cells
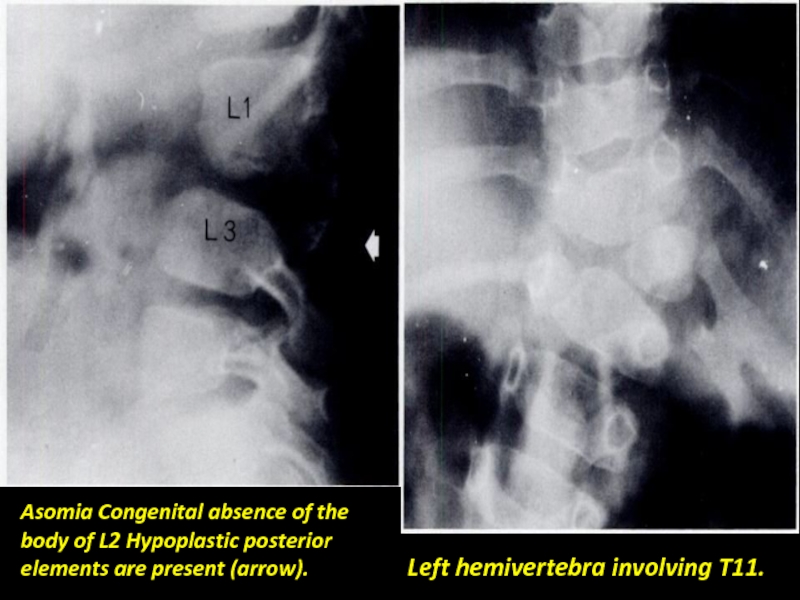
Слайд 70Asomia Congenital absence of the body of L2 Hypoplastic posterior elements
Left hemivertebra involving T11.
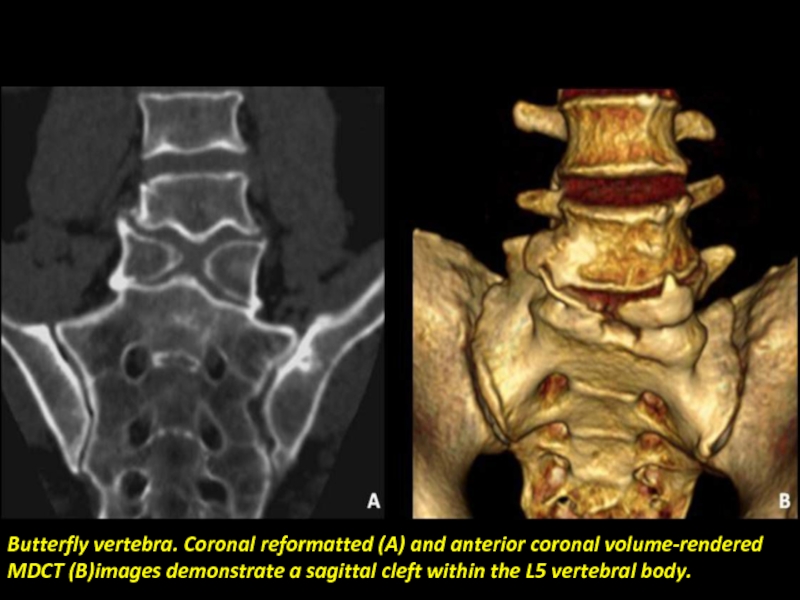
Слайд 71Butterfly vertebra. Coronal reformatted (A) and anterior coronal volume-rendered MDCT (B)images
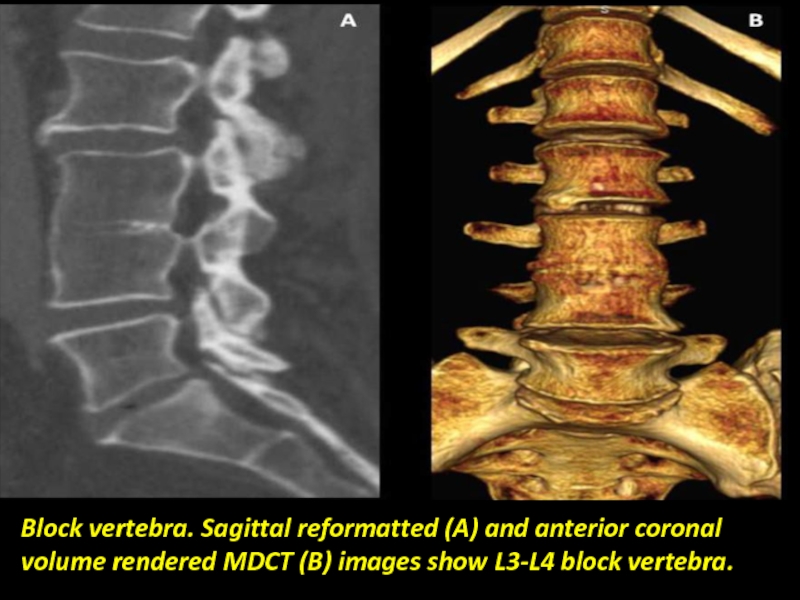
Слайд 73Block vertebra. Sagittal reformatted (A) and anterior coronal volume rendered MDCT
Слайд 74Dorsal hemivertebra and Metametric hemivertebrae in the lower dorsal and lumbar
Vertebrae with coronal clefts.
Слайд 76Vertebral segmentation anomalies. A and B, Three-dimensional CT reconstruction image (A)
Слайд 77Limbus vertebra. Lateral radiograph (a) and sagittal thin slab reformatted
Слайд 78 Limbus vertebra. Axial MDCT image (a) and oblique
volume
Слайд 79L5 transitional vertebra in a 40-year-old woman who presented with left-sciatic
Слайд 81Spondylodysplasias:
Spondylodysplasia refers to any developmental abnormality of the bony spinal column.
Слайд 82Spondylodysplasias
Idiopathic scoliosis.
Congenital scoliosis and kyphosis.
Scheuermann/Schmorl disease.
Neurofibromatosis.
Achondroplasia.
Mucopolysaccharidoses.
Down syndrome.
Spondyloepiphyseal dysplasia.
Craniocervical anomalies.
Klippel-Feil syndrome.
Spinal vascular
Слайд 83Idiopathic Scoliosis
Idiopathic scoliosis is the most common curvature abnormality in childhood.
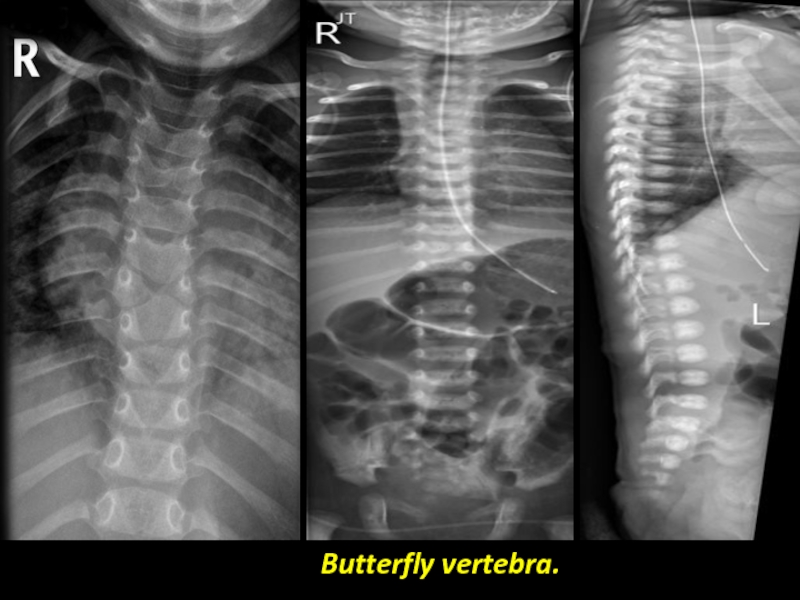
Congenital scoliosis and kyphosis result from formation or segmentation Anomalies . Failure of formation may result in vertebral aplasia or hypoplasia with wedge vertebra, hemivertebra, or butterfly vertebra. Anomalies of segmentation failure include pedicle fusion bars and block vertebra.
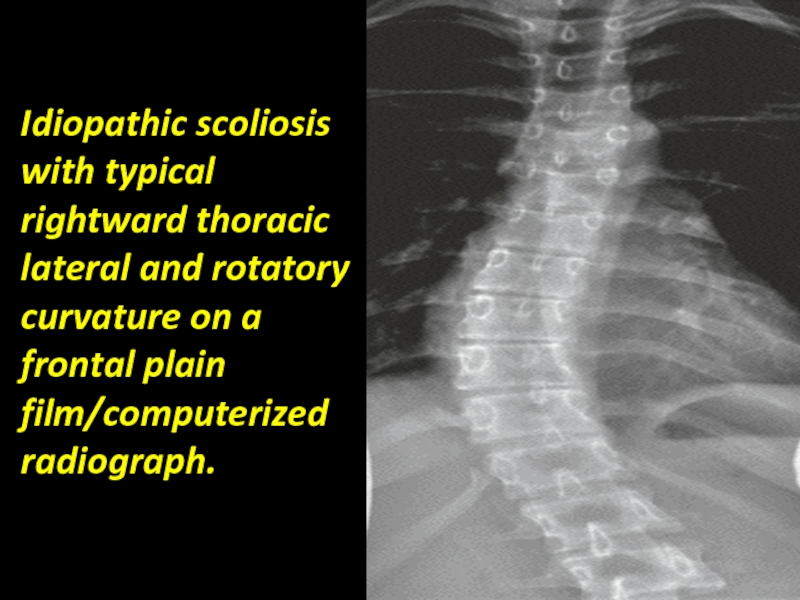
Слайд 84Idiopathic scoliosis with typical rightward thoracic lateral and rotatory curvature on
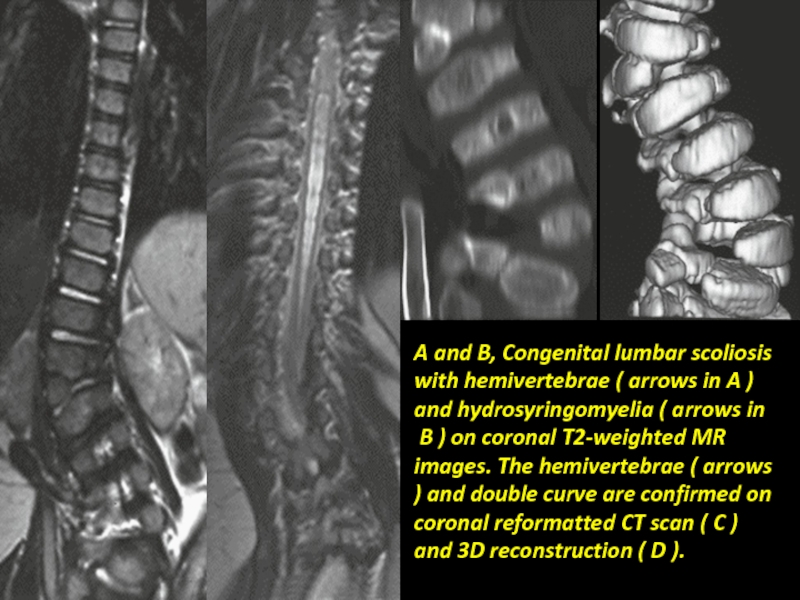
Слайд 85A and B, Congenital lumbar scoliosis with hemivertebrae ( arrows in
B ) on coronal T2-weighted MR images. The hemivertebrae ( arrows ) and double curve are confirmed on coronal reformatted CT scan ( C ) and 3D reconstruction ( D ).
Слайд 86Scheuermann Disease
An osteochondrodysplasia, Scheuermann disease is a common cause of juvenile
Scheuermann disease with multilevel, irregular thoracic disk space narrowing ( long arrows ) and Schmorl’s nodes ( short arrows ).
Слайд 87Neurofibromatosis Type 1:
NF-1 is a common mesodermal dysplasia of childhood
Characteristic anomalies
Слайд 88A, Neurofibromatosis-1 with short-segment right lumbar scoliosis plus vertebral and rib
Слайд 89Achondroplasia
Achondroplasia is one of the osteochondrodysplasia (defective enchondral bone development) resulting
Foramina. Macrocephaly and hydrocephalus (e.g., impaired venous outflow) occur, and there is enlargement of the subarachnoid spaces and ventricles. Other craniocervical abnormalities include odontoid hypoplasia, atlantoaxial (AA) instability, basilar impression, and occipitalization of the atlas. Scoliosis, kyphosis, or kyphoscoliosis may occur in about one third of patients with achondroplasia. Stenosis of the spinal canal may be cervical, thoracolumbar, lumbar, or may occur diffusely. There is platyspondyly with short pedicles, vertebral scalloping, and interpediculate narrowing. There may be associated spinal foraminal and canal compromise.
Слайд 90Achondroplasia, basilar invagination, and foramen magnum plus cervical spinal stenosis (
Слайд 91Mucopolysaccharidosis:
Mucopolysaccharidosis may be associated with craniocervical abnormalities (e.g., Morquio syndrome; They
Down Syndrome:
Down syndrome may be complicated by craniocervical instability,
such as odontoid hypoplasia, os odontoideum, atlanto-occipital
(AO) subluxation, or AA subluxation Scoliosis, degenerative cervical spine disease, tall vertebral bodies, vertebral fusions, and subluxations at other levels may also occur.
Слайд 92A, Morquio syndrome with craniocervical instability ( upper arrow ) plus
Слайд 93Lateral plain film/computerized radiograph ( A ), axial CT scan (
Слайд 94A, Sagittal T2-weighted MR image showing Down syndrome with hypoplastic dens,
spinal cord compressive injury ( posterior arrows ). B, Sagittal postoperative reformatted CT scan shows the stabilized anomaly, including the os odontoideum ( upper arrow ), decompressed canal, and metallic instrumentation plus bony fusion ( posterior arrows ).
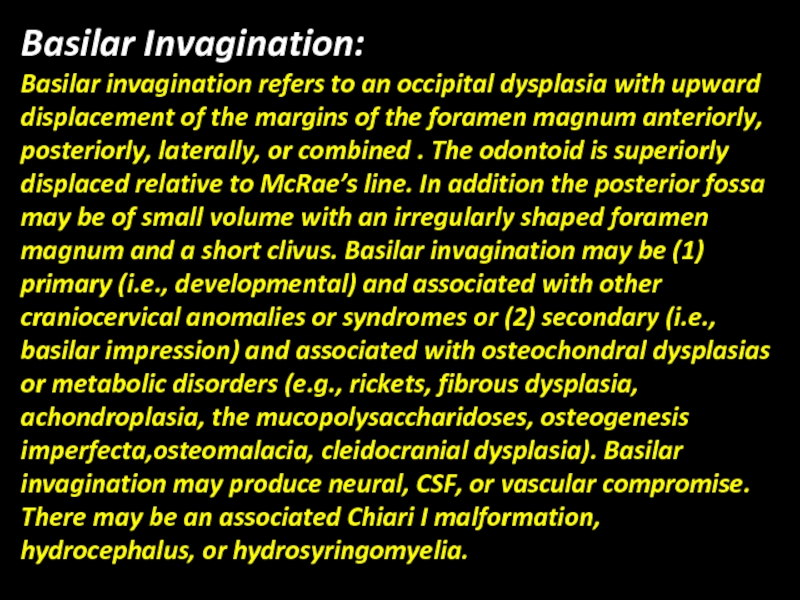
Слайд 95Basilar Invagination:
Basilar invagination refers to an occipital dysplasia with upward displacement
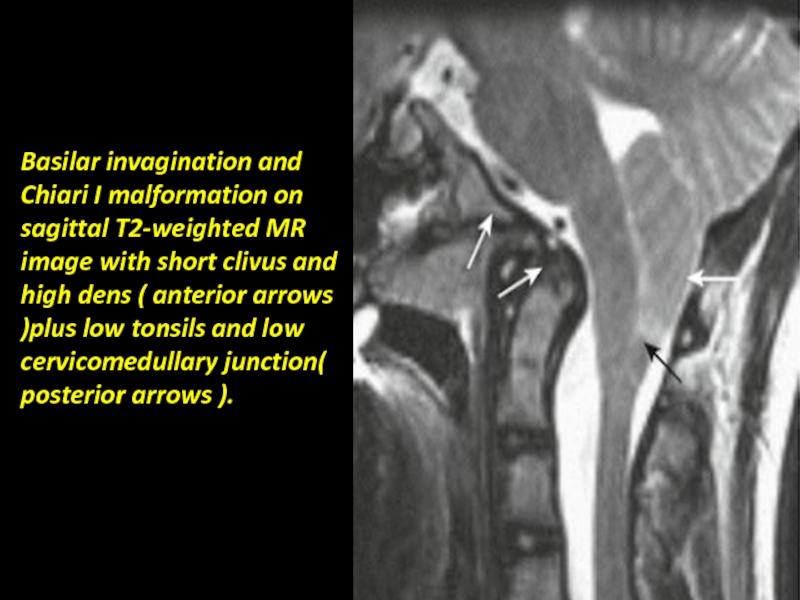
Слайд 96Basilar invagination and Chiari I malformation on sagittal T2-weighted MR image
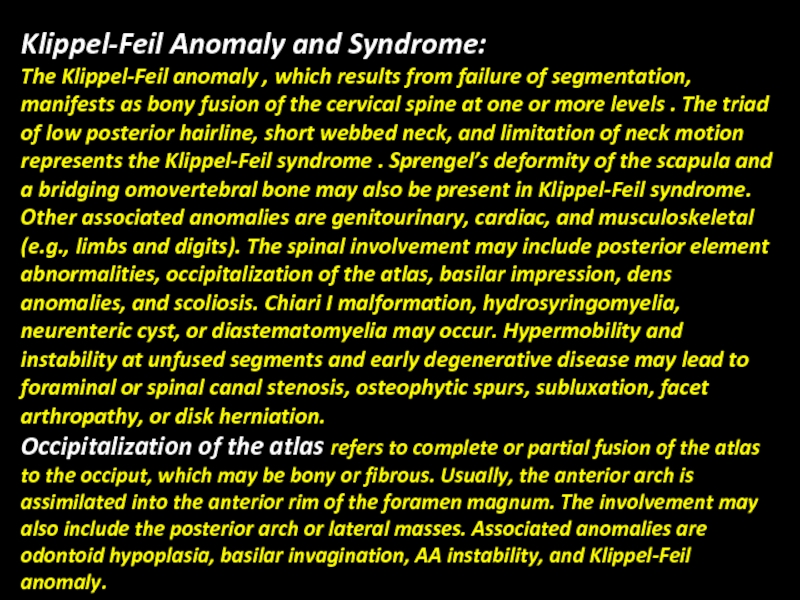
Слайд 97Klippel-Feil Anomaly and Syndrome:
The Klippel-Feil anomaly , which results from failure
Occipitalization of the atlas refers to complete or partial fusion of the atlas to the occiput, which may be bony or fibrous. Usually, the anterior arch is assimilated into the anterior rim of the foramen magnum. The involvement may also include the posterior arch or lateral masses. Associated anomalies are odontoid hypoplasia, basilar invagination, AA instability, and Klippel-Feil anomaly.
Слайд 98Sagittal ( A ) and coronal ( B ) reformatted CT
Слайд 99Craniocervical Instability:
Craniocervical instability includes translational or rotary AA instability and AO
or CCJ anomalies (e.g., odontoid anomalies, Klippel-Feil anomaly).
Odontoid Anomalies:
Anomalies of the odontoid include aplasia, hypoplasia, and the os odontoideum. Aplasia is rare and causes severe AA dislocation. Hypoplasia leads to a short dens. Os odontoideum is a proatlas remnant or represents hypertrophy of the ossiculum terminale. Usually, there is odontoid hypoplasia, and the ossicle is located near the dens tip or the basion and lacks a normal dens fusion line. Hypertrophy of the anterior arch and hypoplasia or clefting of the posterior arch are often present.
AA or occipitoaxial instability commonly occurs. Odontoid anomalies may be idiopathic or may be associated with skeletal dysplasias such as Morquio syndrome, Down syndrome, SED, and Klippel-Feil anomaly.
Слайд 101Congenital spondylolisthesis
Spondylolisthesis is a condition that involves a forward slip of
Слайд 103Spinal Vascular Anomalies:
Vascular anomalies of childhood may involve the paraspinal soft
(subarachnoid or intramedullary), cord edema, infarct, myelomalacia, syrinx, or atrophy. Spinal AVFs may be “high-flow” or “low-flow” malformations. Spinal angiography is necessary for full evaluation of the vascular anomaly in anticipation of surgery or interventional therapy. Cavernous angiomas of the spinal cord are rare and may manifest as hemorrhage (subarachnoid or intramedullary) or myelopathy.
Слайд 104Cervical spinal cord arteriovenous malformation with high-flow vascular low
intensities (
Слайд 105Spina bifida (Latin : "split spine") is a developmental congenital disorder
of the malformations is the lumbar and sacral areas. Myelomeningocele is the most significant and common form, and this leads to disability in most affected individuals. The terms spina bifida and myelomeningocele are usually used interchangeably.
Слайд 108Sagittal and axial MR images at the level of the
L7-S1
Слайд 109Conclusion
Congenital malformations of the spine and spinal cord can be complex
Spinal dysraphism or neural tube defect is a broad term encompassing a heterogenous group of congenital spinal anomalies which result from defective closure of neural tube early in the fetal life and anomalous development of the caudal cell mass.
Neural tube defect exact emotional and economic toll on families and health care systems.