- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Precise Patient Registries: The Foundation for Clinical Research & Population Health Management презентация
Содержание
- 1. Precise Patient Registries: The Foundation for Clinical Research & Population Health Management
- 2. Agenda Assertions and criticisms of the current
- 3. Acknowledgements & Thanks Steve Barlow Cessily Johnson Darren Kaiser Anita Parisot Tracy Vayo
- 4. Poll Question Have you ever been directly
- 5. Assertion #1 Without precise definitions and registries
- 6. Assertion #2 We can’t keep building disease
- 7. Healthcare Analytics Adoption Model
- 8. Achieving High Resolution Medicine It starts with precise registries
- 9. Patient Registry Definitions Computer Applications used to
- 10. AHRQ’s Patient Registry Definition A patient
- 11. AHRQ’s Patient Registry Definition The National
- 12. Patient Registry Definitions A database designed to
- 13. History of Patient Registries Historically, the term
- 14. What’s a Diabetic Patient? How do we
- 15. Sources of “Standard” Registry Definitions There
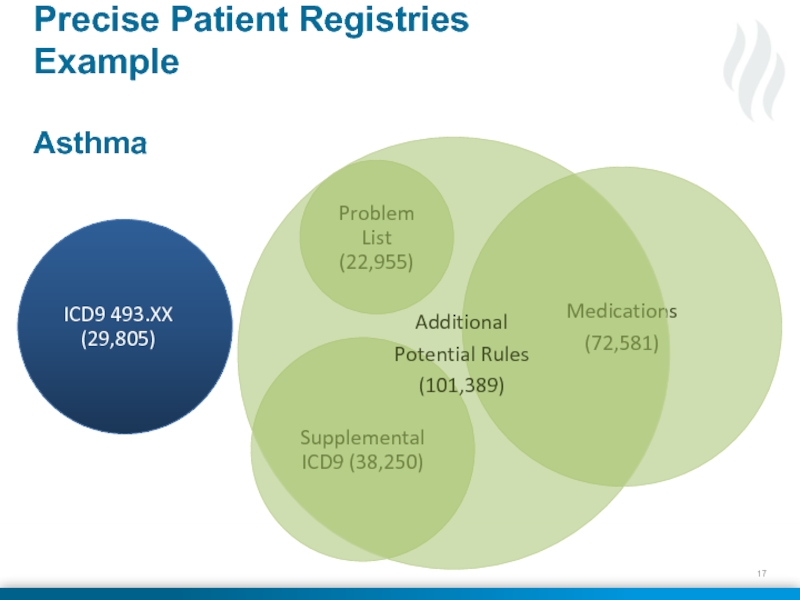
- 17. Precise Patient Registries Example Asthma
- 19. Medscape Summary of Article 11.5 million patient
- 20. Types of Registries, Not Necessarily Disease Oriented
- 21. More Types of Registries Scheduling Events Registry
- 22. Innumerable Uses &
- 23. Patients exist in one of three states,
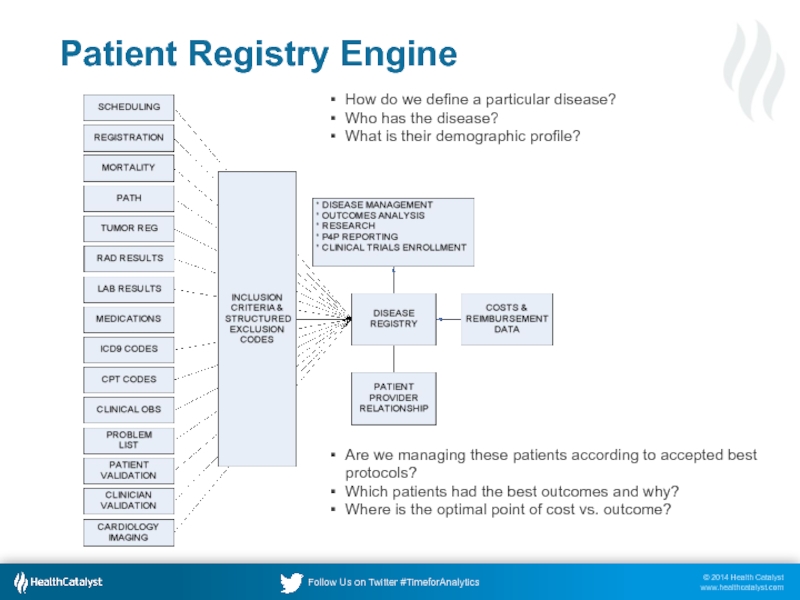
- 25. Patient Registry Engine How do we define
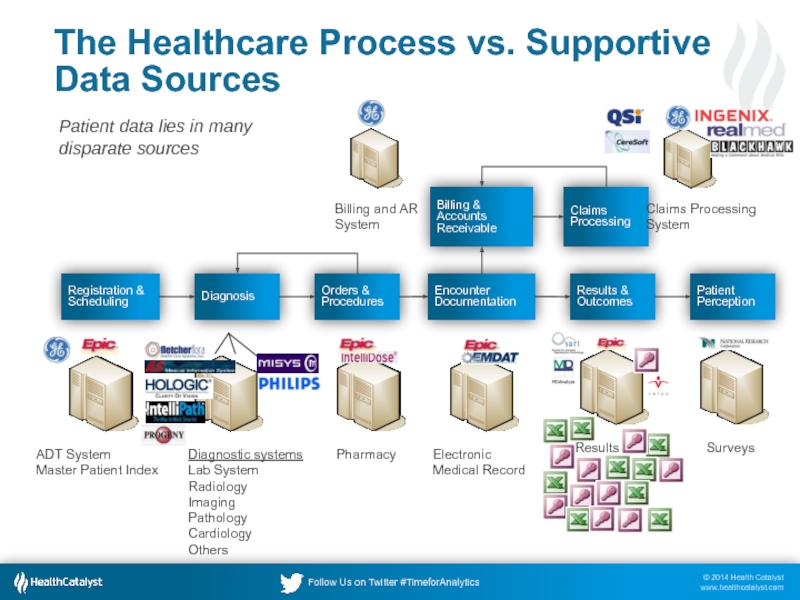
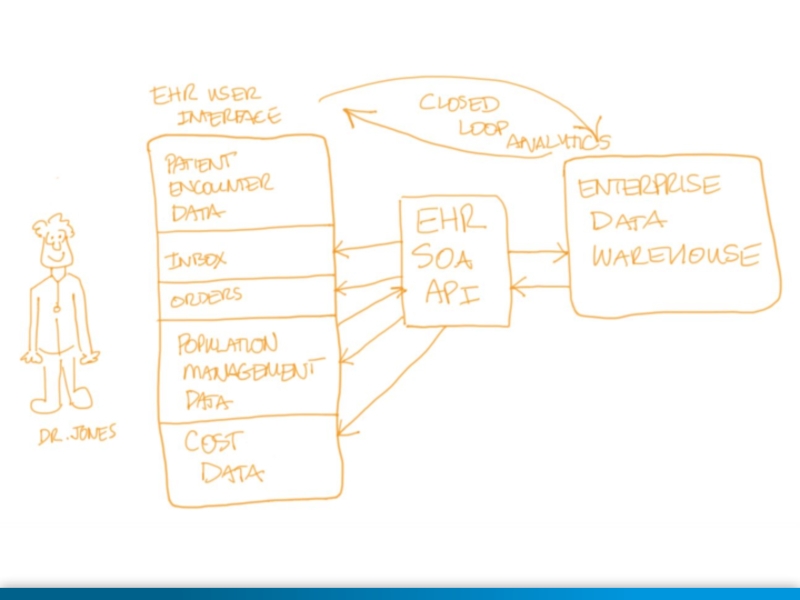
- 26. The Healthcare Process vs. Supportive Data Sources
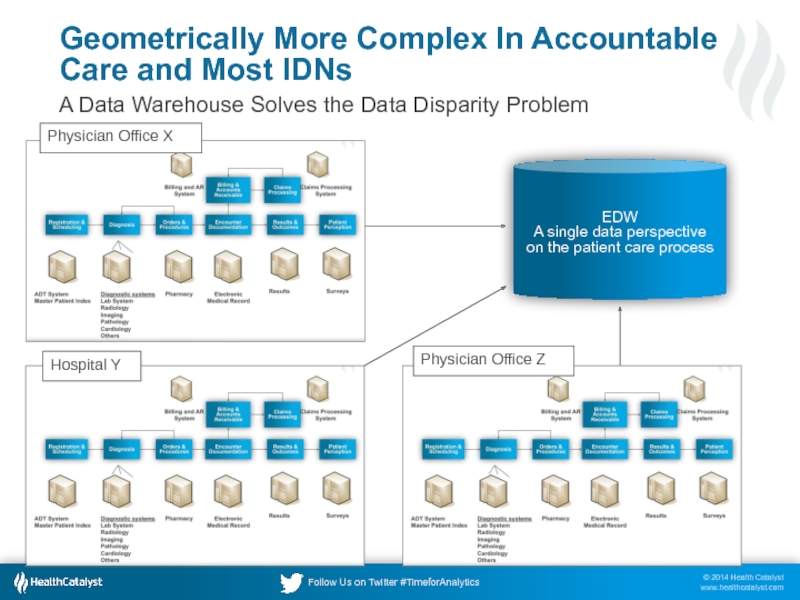
- 27. Geometrically More Complex In Accountable Care and
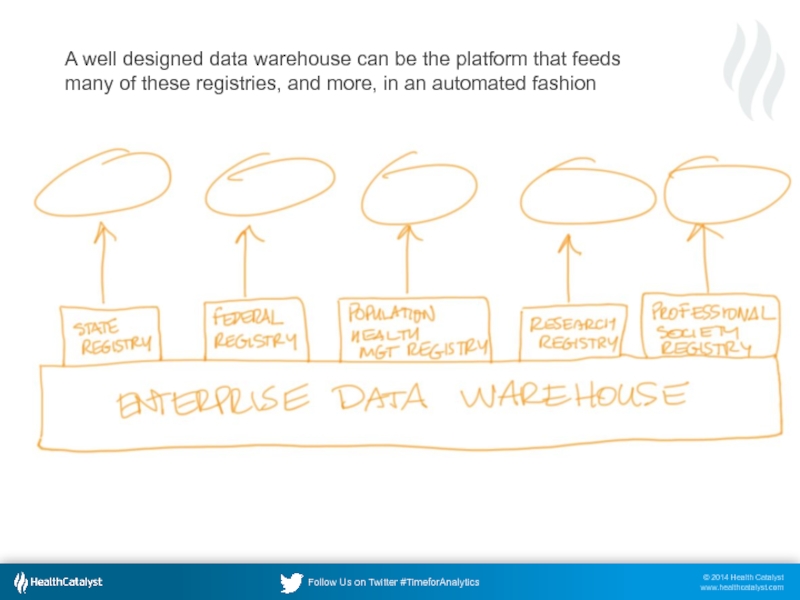
- 28. A well designed data warehouse can be
- 29. Mini-Case Study From Northwestern University Medicine, 2006
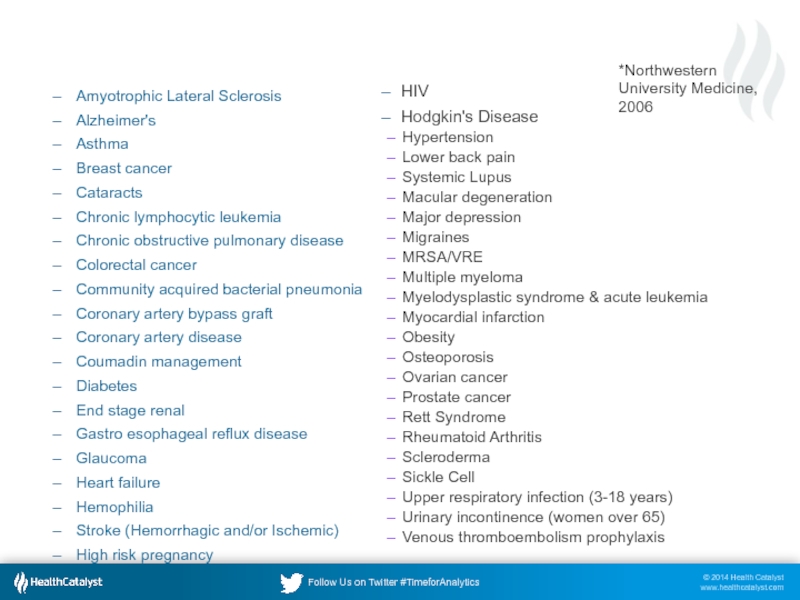
- 30. Target Disease Registries* Amyotrophic Lateral Sclerosis Alzheimer's
- 31. Inclusion & Exclusion for Heart Failure Clinical
- 32. Disease Registry “Exclusions” Our first attempts at
- 33. Not all patients in a registry can
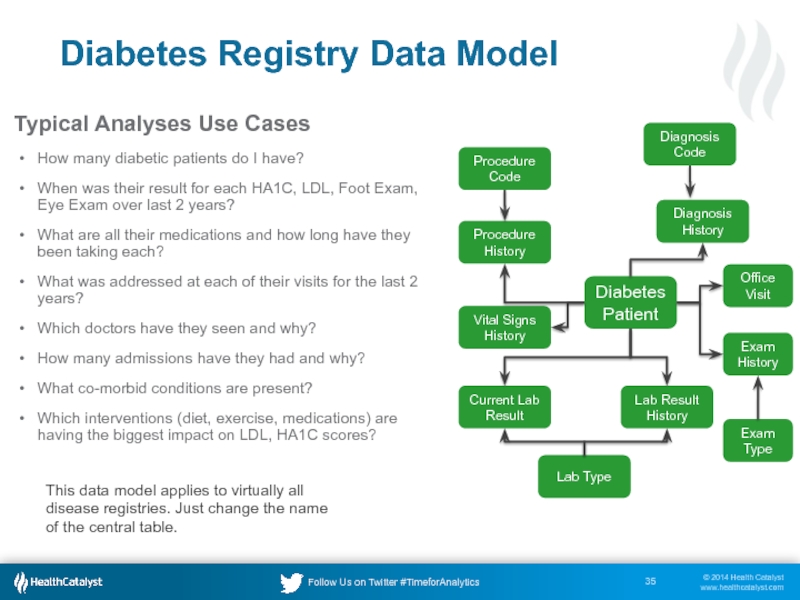
- 35. Diabetes Registry Data Model Diabetes Patient
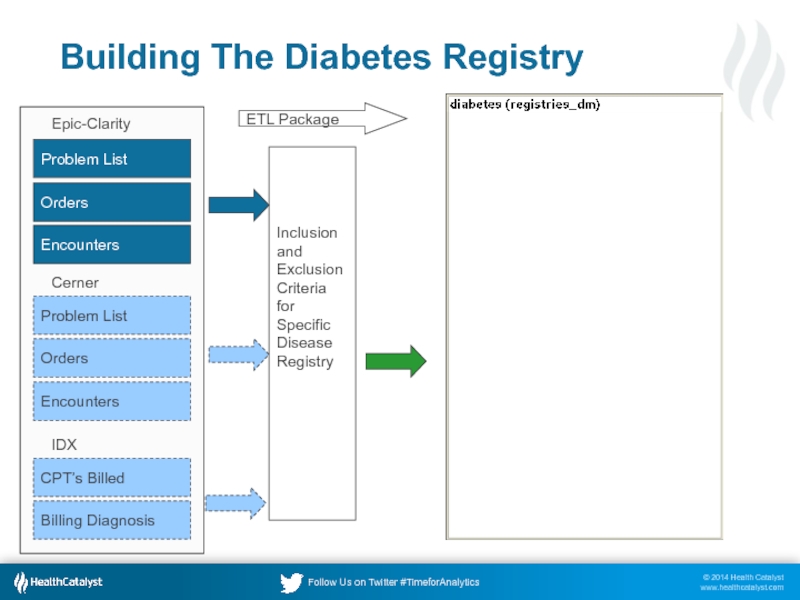
- 36. Building The Diabetes Registry Problem List
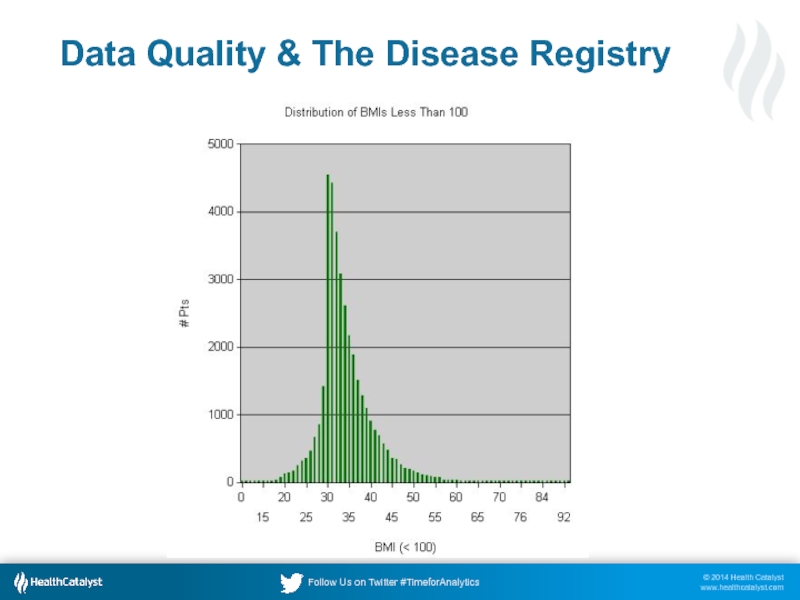
- 37. Data Quality & The Disease Registry
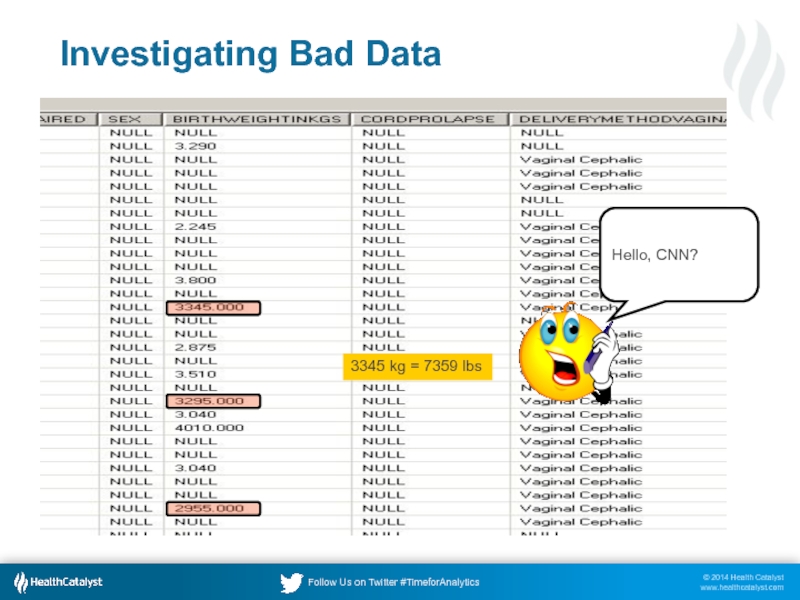
- 38. Investigating Bad Data 3345 kg = 7359 lbs Hello, CNN?
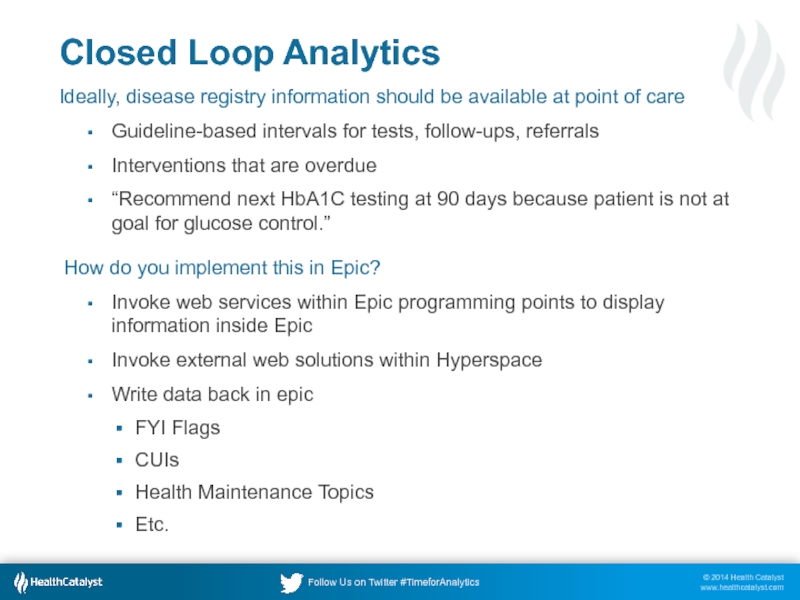
- 39. Closed Loop Analytics Ideally, disease registry information
- 41. Geisinger & Cleveland Clinic Make It Commercially Available
- 42. Nitty Gritty Data Details Thank you, Tracy Vayo
- 43. Poll Question Does your organization have a
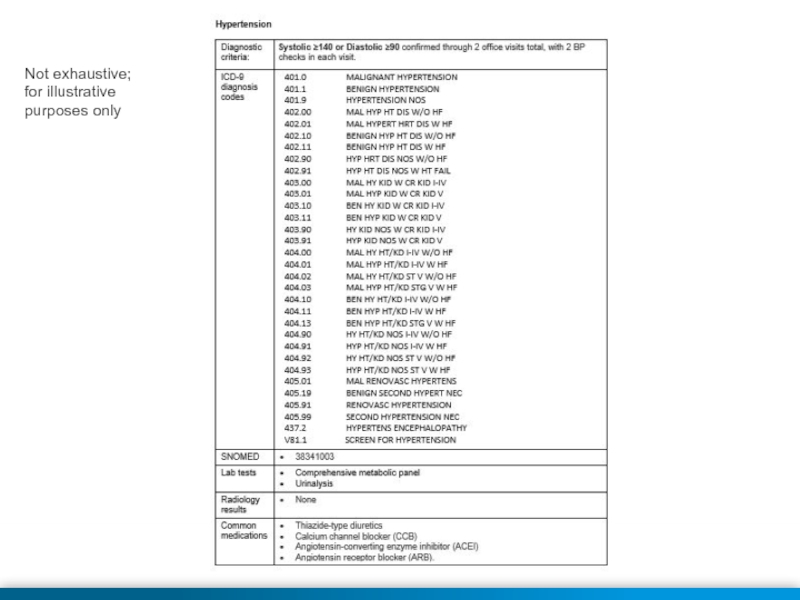
- 44. Not exhaustive; for illustrative purposes only
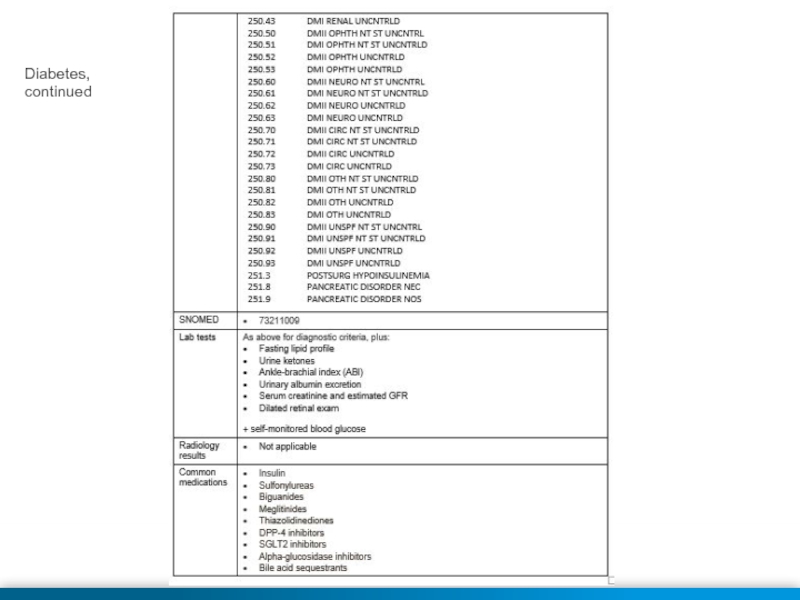
- 45. Diabetes, continued
- 46. Not exhaustive; for illustrative purposes only
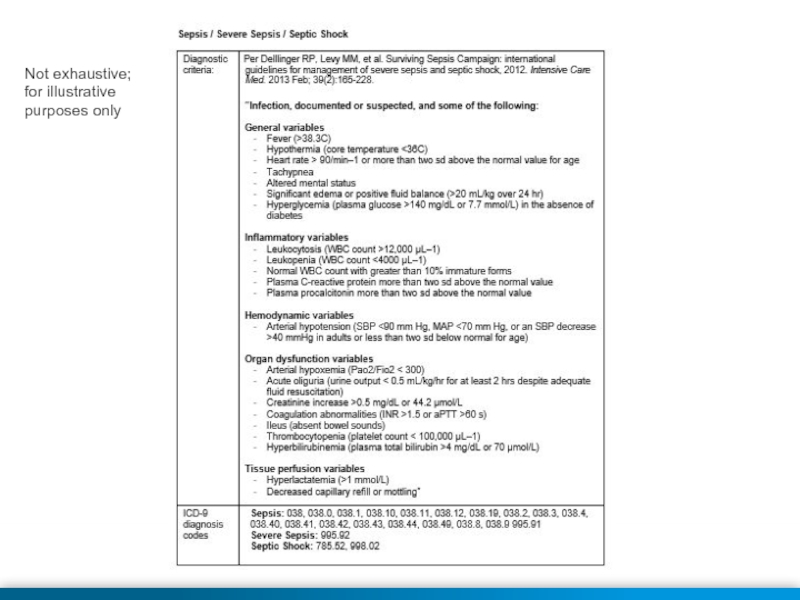
- 47. Not exhaustive; for illustrative purposes only
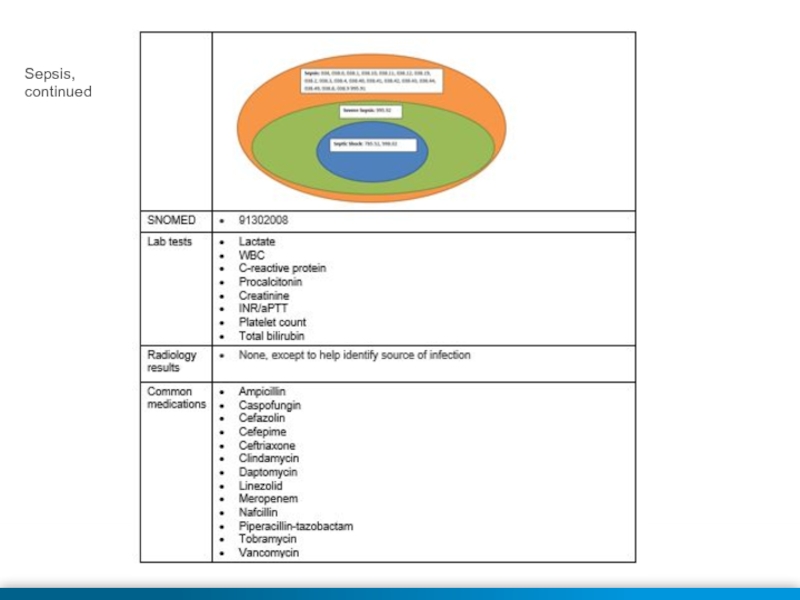
- 48. Sepsis, continued
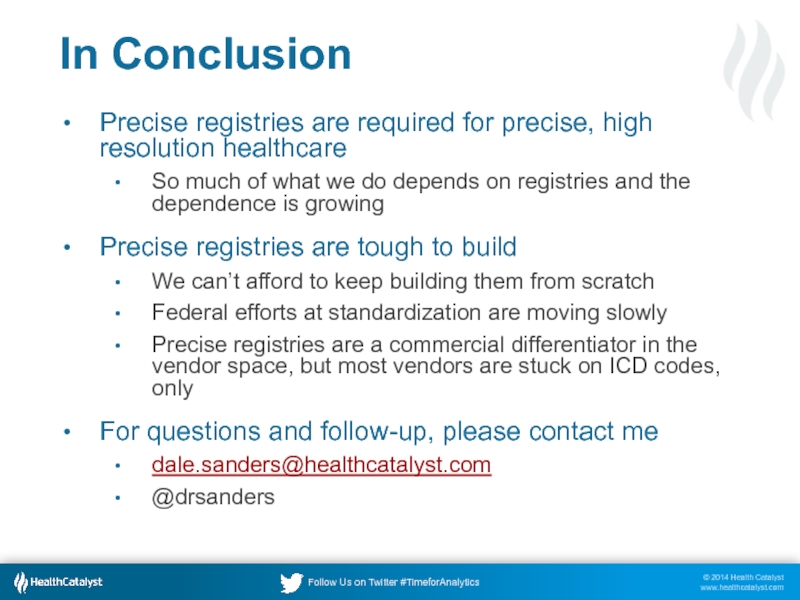
- 49. In Conclusion Precise registries are required for
- 50. Thank You Upcoming Educational Opportunities A Health
Слайд 1Dale Sanders, November 2014
Precise Patient Registries:
The Foundation for Clinical Research
Слайд 2Agenda
Assertions and criticisms of the current state
What is a patient registry?
History
What should we be doing differently?
Designing precise registries
An example from our registry work at Northwestern University
Nitty Gritty data details
Слайд 4Poll Question
Have you ever been directly involved in the design and
Yes
No
Слайд 5Assertion #1
Without precise definitions and registries of patient types, you can’t
Precise clinical research
Precise comparisons across the industry
Precise financial and risk management
Precise, personalized healthcare
Predictable clinical outcomes
Слайд 6Assertion #2
We can’t keep building disease registries at each organization, from
It takes too long, it’s too expensive, it’s not standardized to support disease reporting, surveillance, and comparative medicine
Federal involvement has helped, but projects are moving too slowly
Слайд 9Patient Registry Definitions
Computer Applications used to capture, manage, and provide information
— ”Using Computerized Registries in Chronic Disease Care” California Healthcare Foundation and First Consulting Group, 2004
Слайд 10AHRQ’s Patient Registry Definition
A patient registry is an organized system
Слайд 11AHRQ’s Patient Registry Definition
The National Committee on Vital and Health
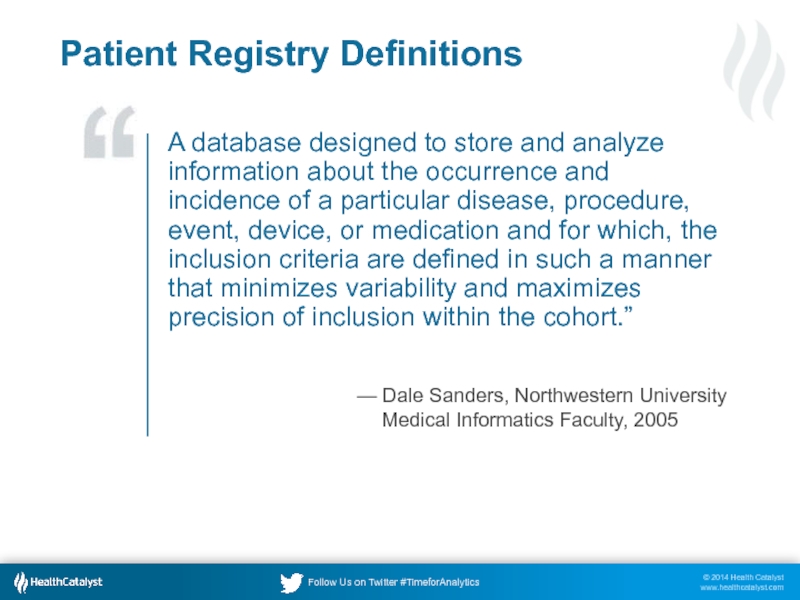
Слайд 12Patient Registry Definitions
A database designed to store and analyze information about
— Dale Sanders, Northwestern University Medical Informatics Faculty, 2005
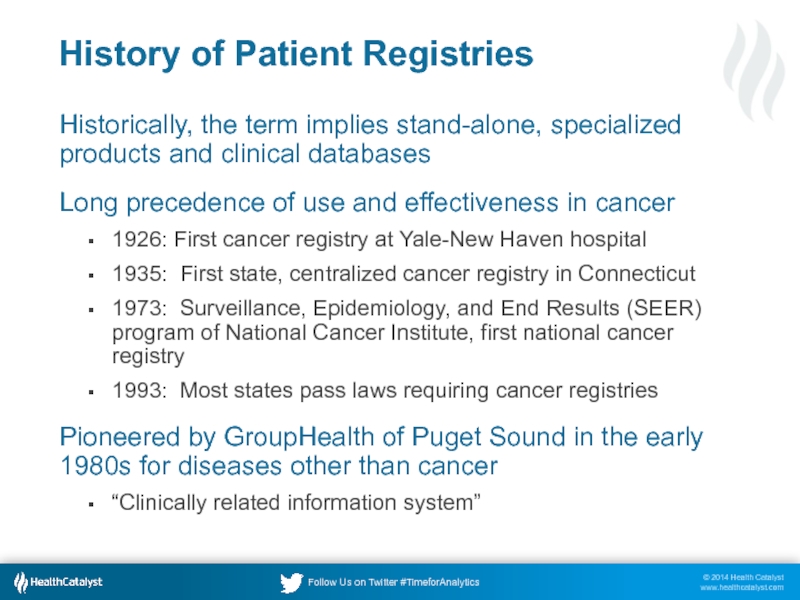
Слайд 13History of Patient Registries
Historically, the term implies stand-alone, specialized products and
Long precedence of use and effectiveness in cancer
1926: First cancer registry at Yale-New Haven hospital
1935: First state, centralized cancer registry in Connecticut
1973: Surveillance, Epidemiology, and End Results (SEER) program of National Cancer Institute, first national cancer registry
1993: Most states pass laws requiring cancer registries
Pioneered by GroupHealth of Puget Sound in the early 1980s for diseases other than cancer
“Clinically related information system”
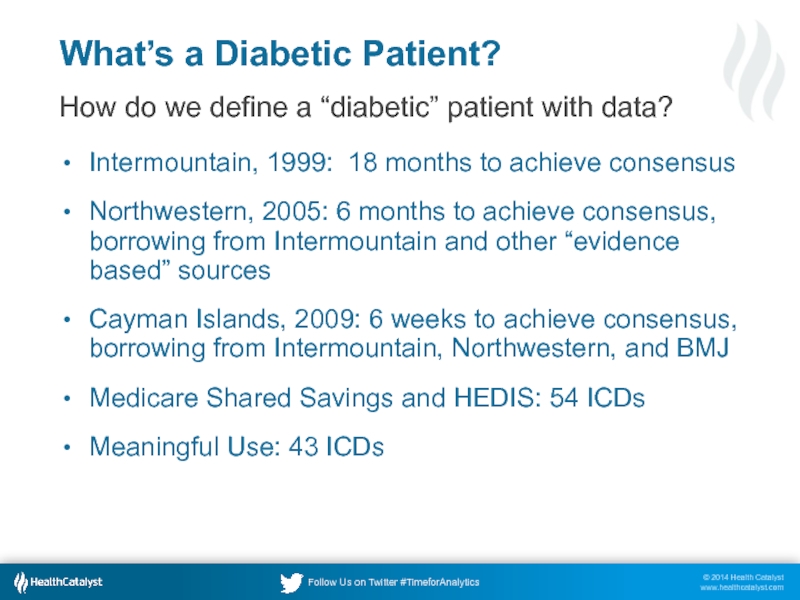
Слайд 14What’s a Diabetic Patient?
How do we define a “diabetic” patient with
Intermountain, 1999: 18 months to achieve consensus
Northwestern, 2005: 6 months to achieve consensus, borrowing from Intermountain and other “evidence based” sources
Cayman Islands, 2009: 6 weeks to achieve consensus, borrowing from Intermountain, Northwestern, and BMJ
Medicare Shared Savings and HEDIS: 54 ICDs
Meaningful Use: 43 ICDs
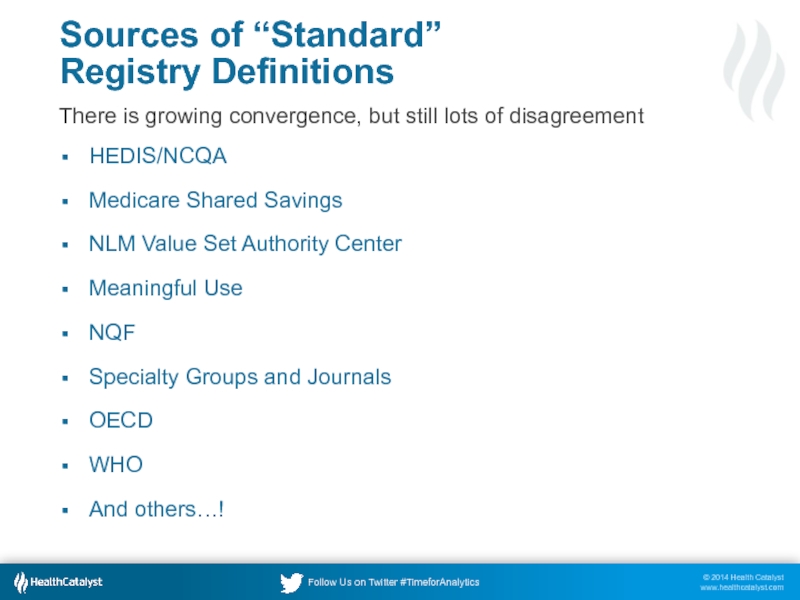
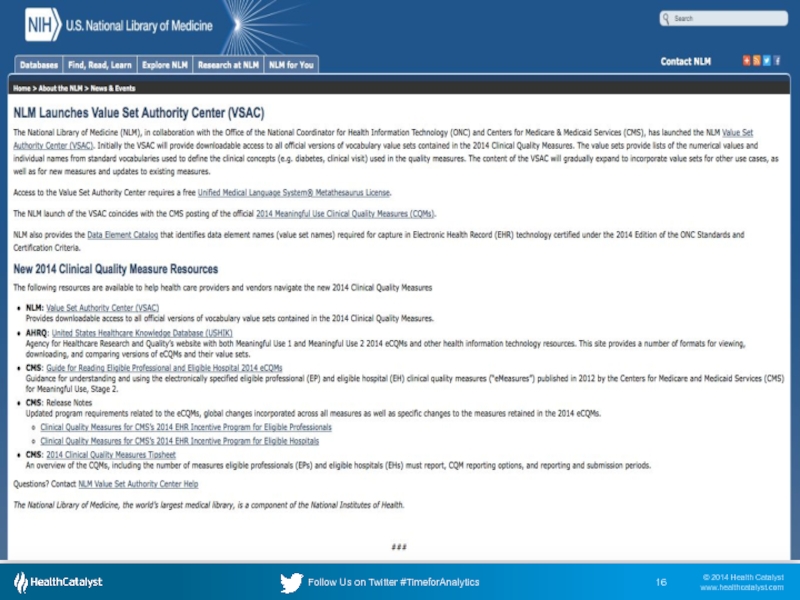
Слайд 15Sources of “Standard”
Registry Definitions
There is growing convergence, but still lots
HEDIS/NCQA
Medicare Shared Savings
NLM Value Set Authority Center
Meaningful Use
NQF
Specialty Groups and Journals
OECD
WHO
And others…!
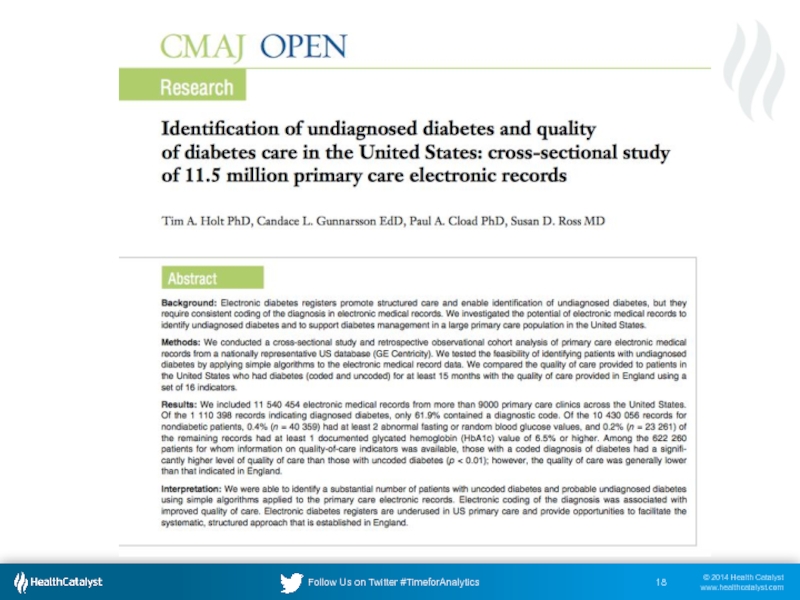
Слайд 19Medscape Summary of Article
11.5 million patient records
9000 primary-care clinics across the
5.4% of those likely to have diabetes in the databases were undiagnosed
Undiagnosed proportion rose to 12% to 16% in "hot spots," including Arizona, North Dakota, Minnesota, South Carolina, and Indiana
Patients without an ICD for diabetes received worse care, had worse outcomes
"It may be that a 'free-text' entry was added to the record, but unless it is coded in electronically, the patient has not been included in the diabetes register and cannot therefore benefit from the structured care that depends on such inclusion." -- Dr. Tim Holt
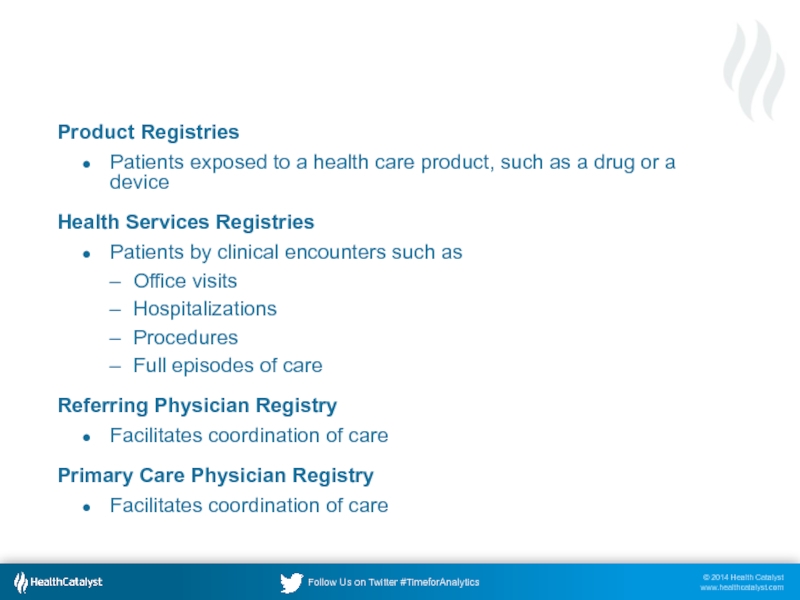
Слайд 20Types of Registries, Not Necessarily Disease Oriented
Product Registries
Patients exposed to a
Health Services Registries
Patients by clinical encounters such as
Office visits
Hospitalizations
Procedures
Full episodes of care
Referring Physician Registry
Facilitates coordination of care
Primary Care Physician Registry
Facilitates coordination of care
Слайд 21More Types of Registries
Scheduling Events Registry
Facilitates analysis for Patient Relationship Management
Can drive reminders for research and standards of care protocols
Mortality registry
An important thing to know about your patients
Research Patient Registry
Clinical Trials
Consent
Disease or Condition Registries
Disease or condition registries use the state of a particular disease or condition as the inclusion criterion.
Combinations
Слайд 22
Innumerable Uses & Benefits
Registries
Clinicians &
Researchers
Physician
Organization
Consumer
Drug
Manufacturer
How does my drug perform in
How well am I managing diseases?
Who else is treating patients like this?
How is this disease expressed in the genome?
How do I analyze patient trends and outcomes for a disease?
How do I know which drug/procedure works best for me?
Who else matches my specific profile for disease, medication, procedure, or device… and can I interact with them?
Слайд 23Patients exist in one of three states, relative to a patient
The patient is a member of a particular registry; i.e., they fit the inclusion criteria
Patient was once a member of a registry and fit the inclusion criteria, but is now excluded. The exclusion could be “disease free.”
The patient fits the profile that could lead to inclusion on the registry, but does not yet meet the formal inclusion criteria, e.g. obesity as a precursor to membership on the diabetes and or hypertension registry.
Слайд 25Patient Registry Engine
How do we define a particular disease?
Who has
What is their demographic profile?
Are we managing these patients according to accepted best protocols?
Which patients had the best outcomes and why?
Where is the optimal point of cost vs. outcome?
Слайд 26The Healthcare Process vs. Supportive Data Sources
Diagnostic systems
Lab System
Radiology
Imaging
Pathology
Cardiology
Others
Diagnosis
Registration &
Scheduling
Patient
Perception
Orders &
Procedures
Results &
Outcomes
Billing &
Accounts
Receivable
Claims
Processing
Encounter
Documentation
Patient data lies in many disparate sources
Слайд 27Geometrically More Complex In Accountable Care and Most IDNs
A Data Warehouse
EDW
A single data perspective
on the patient care process
Physician Office X
Hospital Y
Physician Office Z
Слайд 28A well designed data warehouse can be the platform that feeds
Слайд 30Target Disease Registries*
Amyotrophic Lateral Sclerosis
Alzheimer's
Asthma
Breast cancer
Cataracts
Chronic lymphocytic leukemia
Chronic obstructive pulmonary disease
Colorectal
Community acquired bacterial pneumonia
Coronary artery bypass graft
Coronary artery disease
Coumadin management
Diabetes
End stage renal
Gastro esophageal reflux disease
Glaucoma
Heart failure
Hemophilia
Stroke (Hemorrhagic and/or Ischemic)
High risk pregnancy
HIV
Hodgkin's Disease
Hypertension
Lower back pain
Systemic Lupus
Macular degeneration
Major depression
Migraines
MRSA/VRE
Multiple myeloma
Myelodysplastic syndrome & acute leukemia
Myocardial infarction
Obesity
Osteoporosis
Ovarian cancer
Prostate cancer
Rett Syndrome
Rheumatoid Arthritis
Scleroderma
Sickle Cell
Upper respiratory infection (3-18 years)
Urinary incontinence (women over 65)
Venous thromboembolism prophylaxis
*Northwestern University Medicine, 2006
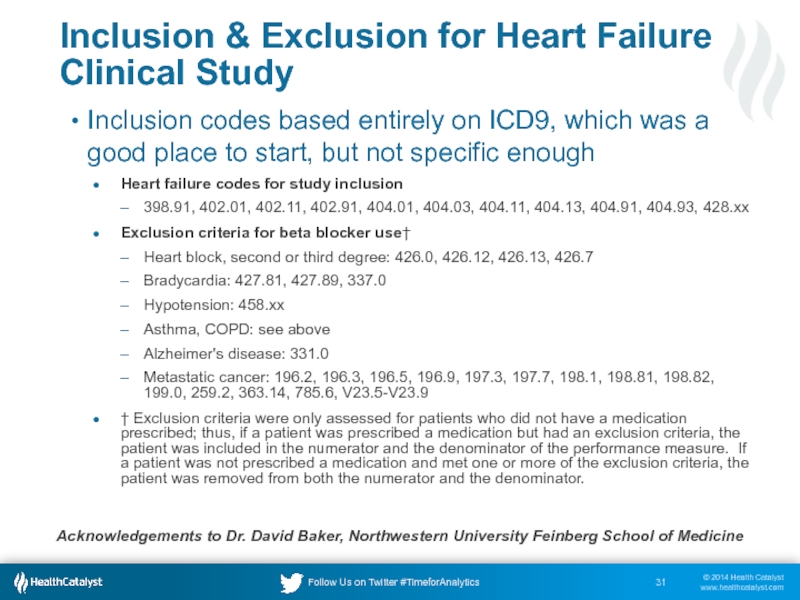
Слайд 31Inclusion & Exclusion for Heart Failure Clinical Study
Inclusion codes based entirely
Heart failure codes for study inclusion
398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.xx
Exclusion criteria for beta blocker use†
Heart block, second or third degree: 426.0, 426.12, 426.13, 426.7
Bradycardia: 427.81, 427.89, 337.0
Hypotension: 458.xx
Asthma, COPD: see above
Alzheimer's disease: 331.0
Metastatic cancer: 196.2, 196.3, 196.5, 196.9, 197.3, 197.7, 198.1, 198.81, 198.82, 199.0, 259.2, 363.14, 785.6, V23.5-V23.9
† Exclusion criteria were only assessed for patients who did not have a medication prescribed; thus, if a patient was prescribed a medication but had an exclusion criteria, the patient was included in the numerator and the denominator of the performance measure. If a patient was not prescribed a medication and met one or more of the exclusion criteria, the patient was removed from both the numerator and the denominator.
Acknowledgements to Dr. David Baker, Northwestern University Feinberg School of Medicine
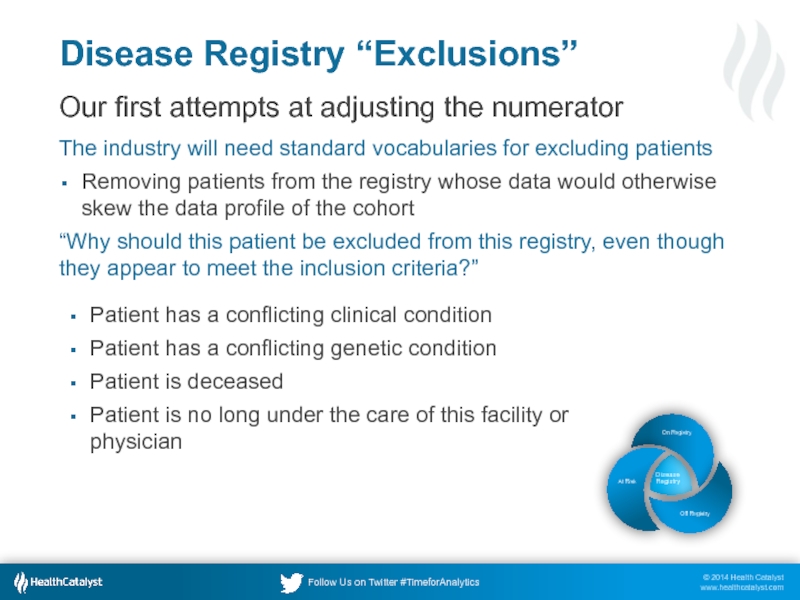
Слайд 32Disease Registry “Exclusions”
Our first attempts at adjusting the numerator
The industry will
Removing patients from the registry whose data would otherwise skew the data profile of the cohort
“Why should this patient be excluded from this registry, even though they appear to meet the inclusion criteria?”
Patient has a conflicting clinical condition
Patient has a conflicting genetic condition
Patient is deceased
Patient is no long under the care of this facility or physician
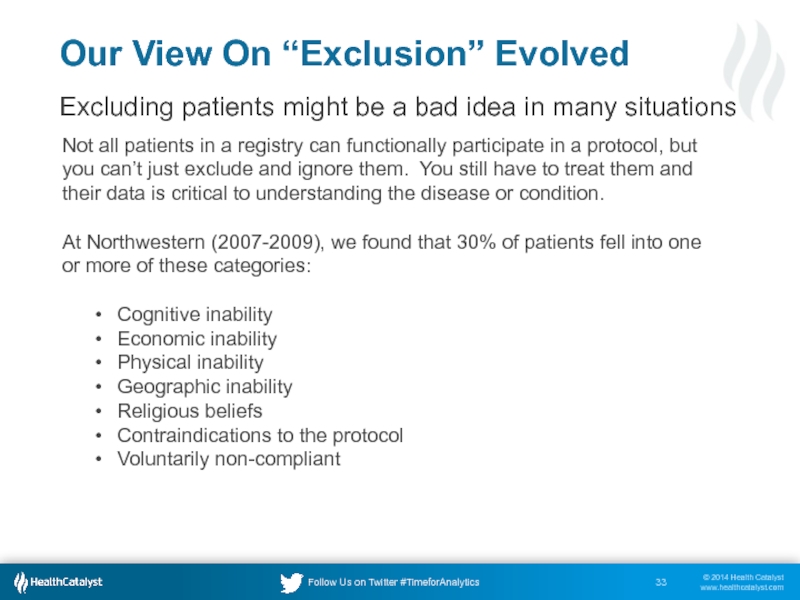
Слайд 33Not all patients in a registry can functionally participate in a
At Northwestern (2007-2009), we found that 30% of patients fell into one or more of these categories:
Cognitive inability
Economic inability
Physical inability
Geographic inability
Religious beliefs
Contraindications to the protocol
Voluntarily non-compliant
Our View On “Exclusion” Evolved
Excluding patients might be a bad idea in many situations
Слайд 35Diabetes Registry Data Model
Diabetes Patient
Typical Analyses Use Cases
How many diabetic
When was their result for each HA1C, LDL, Foot Exam, Eye Exam over last 2 years?
What are all their medications and how long have they been taking each?
What was addressed at each of their visits for the last 2 years?
Which doctors have they seen and why?
How many admissions have they had and why?
What co-morbid conditions are present?
Which interventions (diet, exercise, medications) are having the biggest impact on LDL, HA1C scores?
Procedure History
Vital Signs History
Current Lab Result
Lab Result History
Office Visit
Exam Type
Exam History
Diagnosis History
Diagnosis Code
Procedure Code
Lab Type
This data model applies to virtually all disease registries. Just change the name of the central table.
Слайд 36
Building The Diabetes Registry
Problem List
Orders
Encounters
Epic-Clarity
Problem List
Orders
Encounters
Cerner
CPT’s Billed
Billing Diagnosis
IDX
Inclusion and Exclusion Criteria
ETL Package
Слайд 39Closed Loop Analytics
Ideally, disease registry information should be available at point
Guideline-based intervals for tests, follow-ups, referrals
Interventions that are overdue
“Recommend next HbA1C testing at 90 days because patient is not at goal for glucose control.”
How do you implement this in Epic?
Invoke web services within Epic programming points to display information inside Epic
Invoke external web solutions within Hyperspace
Write data back in epic
FYI Flags
CUIs
Health Maintenance Topics
Etc.
Слайд 43Poll Question
Does your organization have a patient registry data governance and
Yes and it’s very active
Yes, somewhat
No, but we are talking about it
No, not at all
I’m not part of an organization that manages patient registries
Слайд 49In Conclusion
Precise registries are required for precise, high resolution healthcare
So much
Precise registries are tough to build
We can’t afford to keep building them from scratch
Federal efforts at standardization are moving slowly
Precise registries are a commercial differentiator in the vendor space, but most vendors are stuck on ICD codes, only
For questions and follow-up, please contact me
dale.sanders@healthcatalyst.com
@drsanders
Слайд 50Thank You
Upcoming Educational Opportunities
A Health Catalyst Overview: An Introduction to Healthcare
Date: November 20, 1-2pm, EST
Presenter: Vice President Jared Crapo & Senior Solutions Consultant Sriraman Rajamani
http://www.healthcatalyst.com/knowledge-center/webinars-presentations