09.06.2017
- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Publications_V4 презентация
Содержание
- 1. Publications_V4
- 2. Peripheral Vascular Disease CONFIDENTIAL │ © Copyright
- 3. Rotarex®S endovascular system 09.06.2017 CONFIDENTIAL │ ©
- 4. There are various clinical and experimental studies,
- 5. Targets for Rotarex®S 09.06.2017 CONFIDENTIAL │ ©
- 6. 1. Native Vessels 09.06.2017 CONFIDENTIAL │ ©
- 7. 1. Native Vessels with Rotarex®S 09.06.2017 CONFIDENTIAL
- 8. Publication: The Leipzig experience – 525
- 9. Publication: The Leipzig experience – 525
- 10. Comment on Stanek et al, p.49-56 4
- 11. Technical and clinical outcomes after treatment with
- 12. 2. In-Stent Restenosis 09.06.2017 CONFIDENTIAL │ ©
- 13. 2. In-Stent Restenosis 09.06.2017 CONFIDENTIAL │ ©
- 14. Publication: In-Stent Reocclusions of Femoropopliteal Arteries
- 15. The treatment of the ISR in the
- 16. The treatment of the ISR in the
- 17. 3. Venous and Synthetic Bypass occlusions 09.06.2017
- 18. Publication: Acute femoropopliteal bypass occlusion 09.06.2017 CONFIDENTIAL
- 19. Publications: Recanalization of Acute and Subacute Venous
- 20. 4. Visceral arteries 09.06.2017 CONFIDENTIAL │ ©
- 21. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical
- 22. 5. Upper limb arteries – Subclavian 09.06.2017
- 23. Combination Therapy
- 24. 1. Rotarex®S + DCB 09.06.2017 CONFIDENTIAL │
- 25. Mechanical Debulking + DEB 22 09.06.2017 CONFIDENTIAL
- 26. Rotarex®S vs. Other therapies Comparison of results with other therapies
- 27. Fogarty catheter 09.06.2017 CONFIDENTIAL │ © Copyright
- 28. Comparison of results of Rotarex®S catheters
- 29. Cost Analysis 09.06.2017 CONFIDENTIAL │ © Copyright
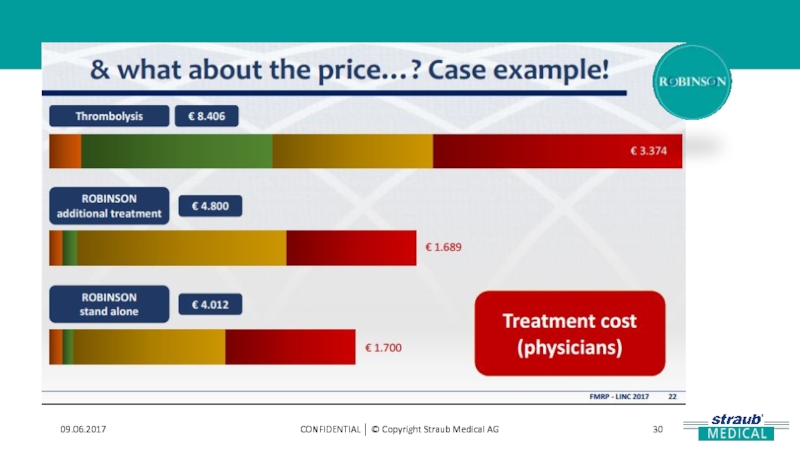
- 30. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
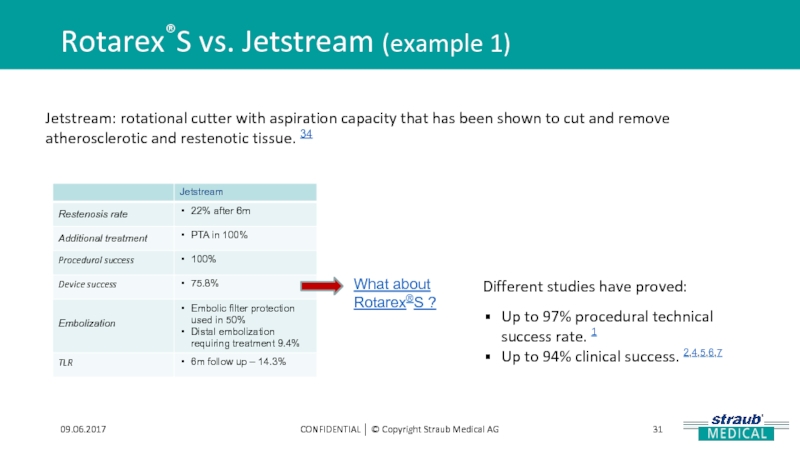
- 31. Rotarex®S vs. Jetstream (example 1) 09.06.2017 CONFIDENTIAL
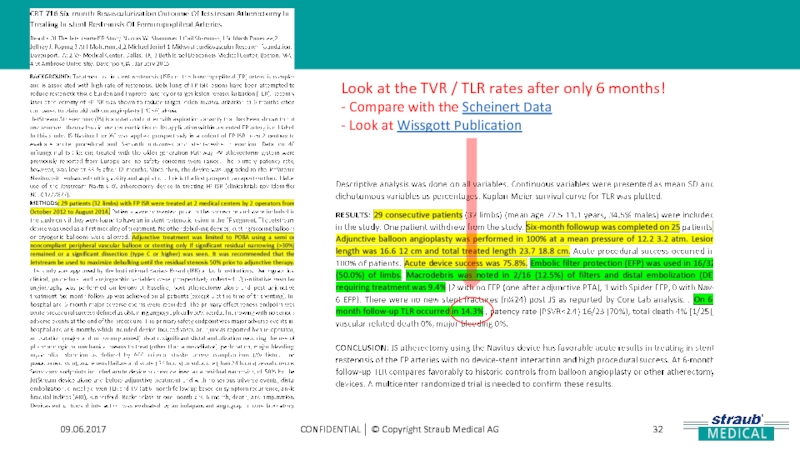
- 32. 09.06.2017 CONFIDENTIAL │ © Copyright Straub
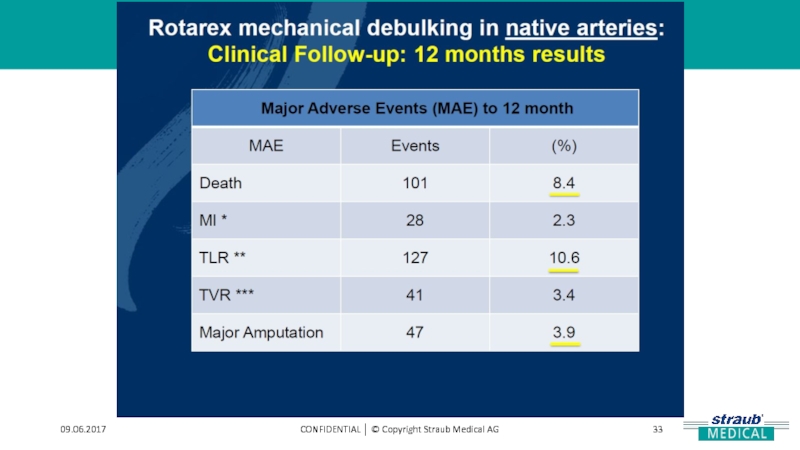
- 33. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
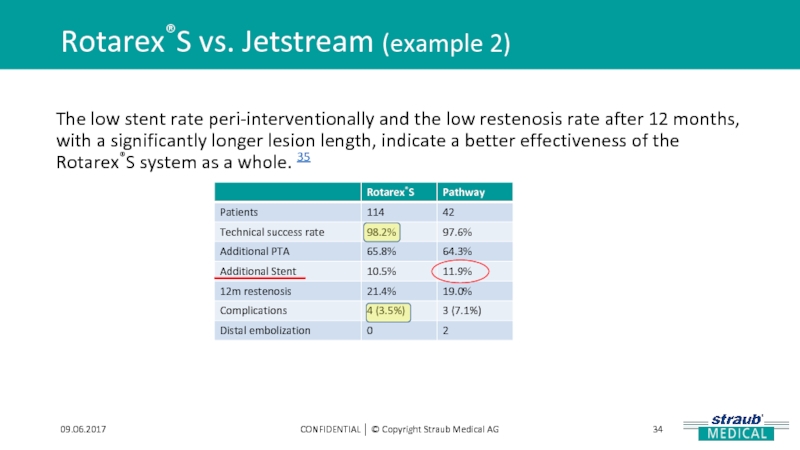
- 34. Rotarex®S vs. Jetstream (example 2) 09.06.2017 CONFIDENTIAL
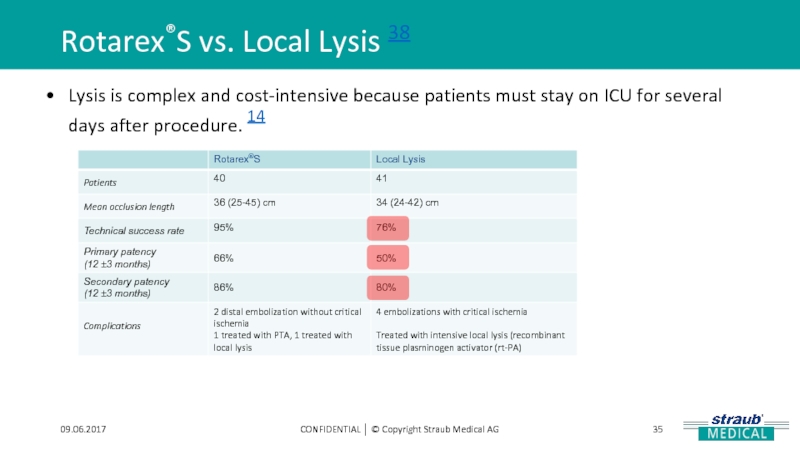
- 35. Rotarex®S vs. Local Lysis 38 09.06.2017 CONFIDENTIAL
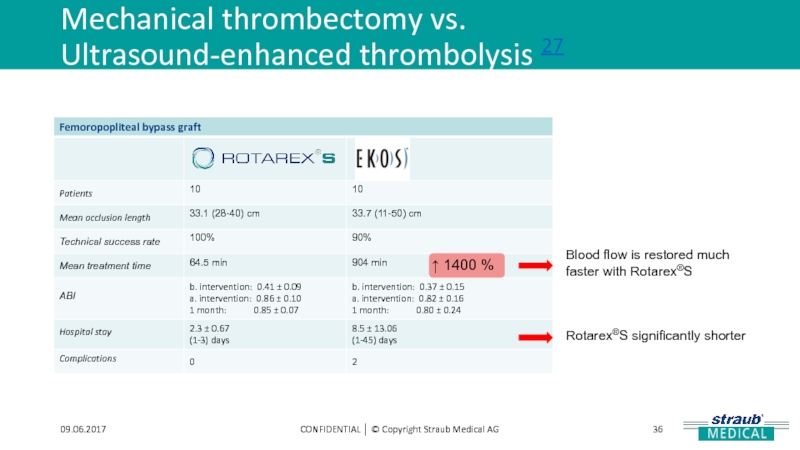
- 36. Mechanical thrombectomy vs. Ultrasound-enhanced thrombolysis 27 09.06.2017
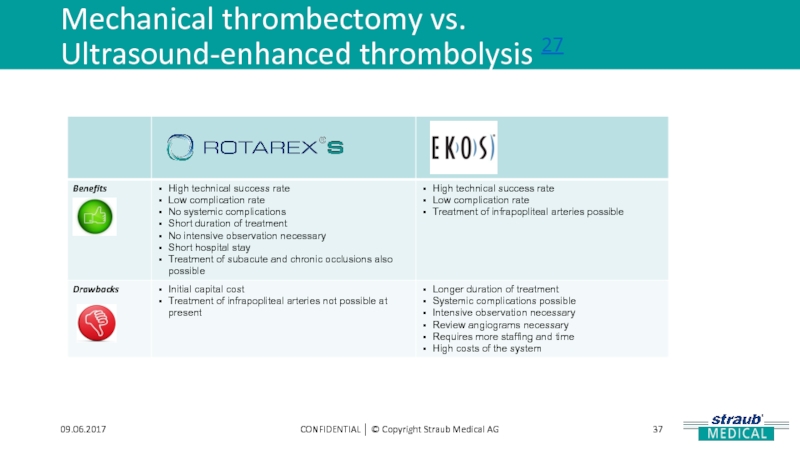
- 37. Mechanical thrombectomy vs. Ultrasound-enhanced thrombolysis 27 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
- 38. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
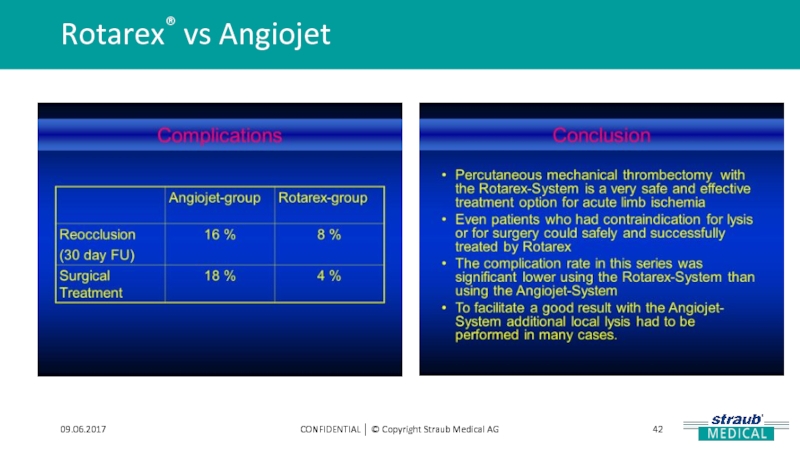
- 39. Rotarex® vs Angiojet 09.06.2017 CONFIDENTIAL │
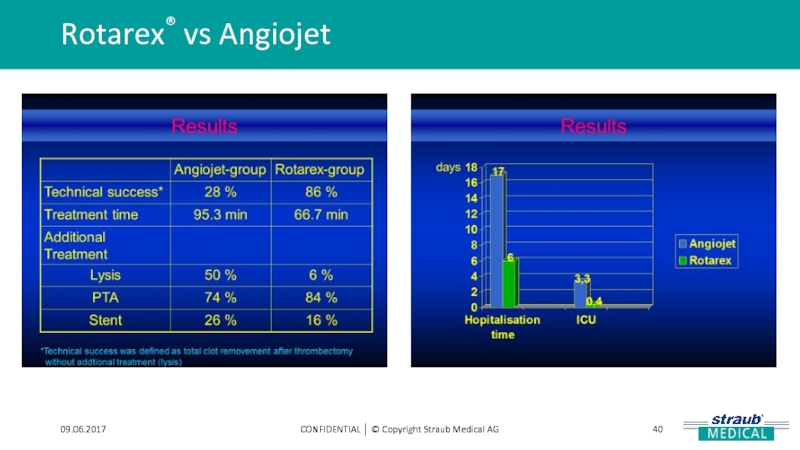
- 40. Rotarex® vs Angiojet 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
- 41. Rotarex® vs Angiojet 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
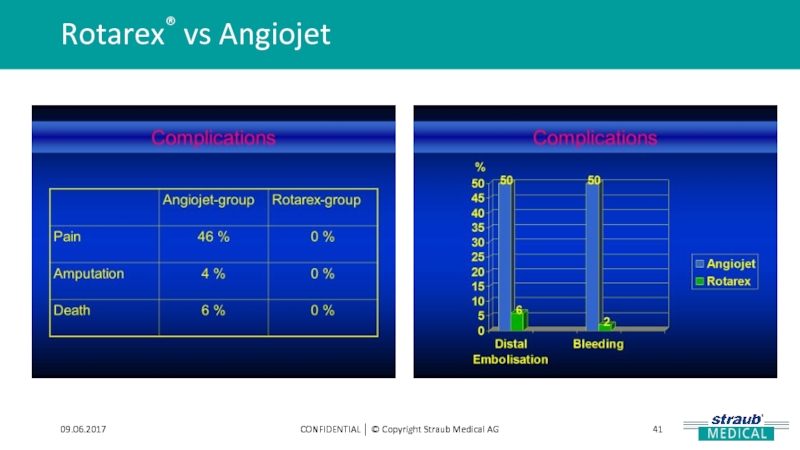
- 42. Rotarex® vs Angiojet 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
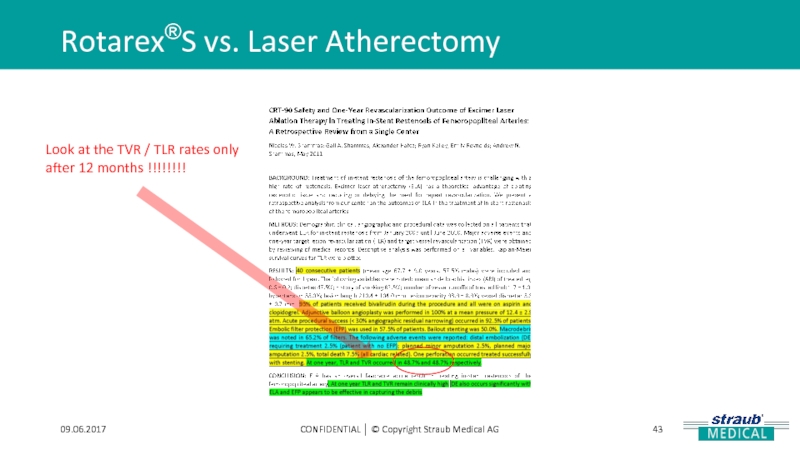
- 43. Rotarex®S vs. Laser Atherectomy 09.06.2017 CONFIDENTIAL │
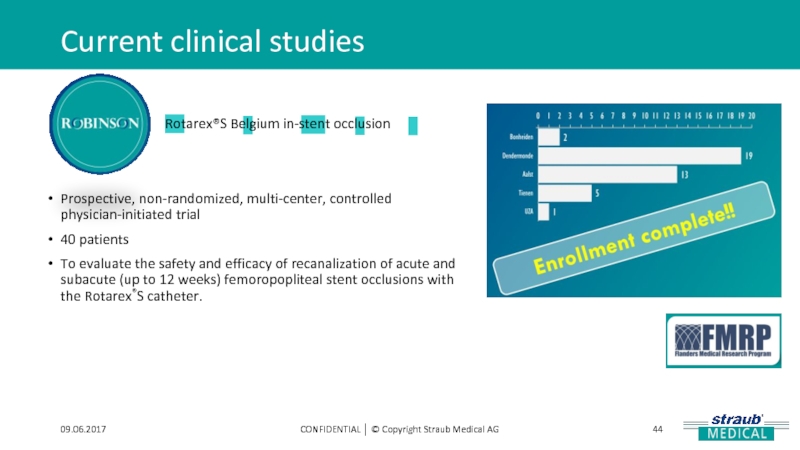
- 44. Current clinical studies 09.06.2017 CONFIDENTIAL │ ©
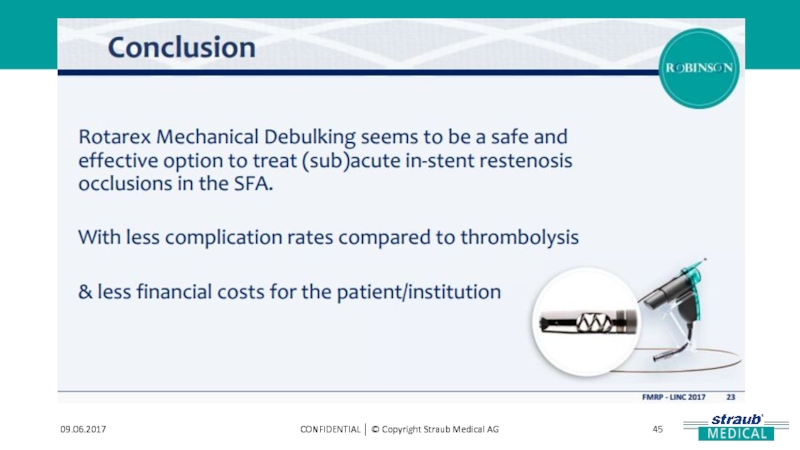
- 45. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
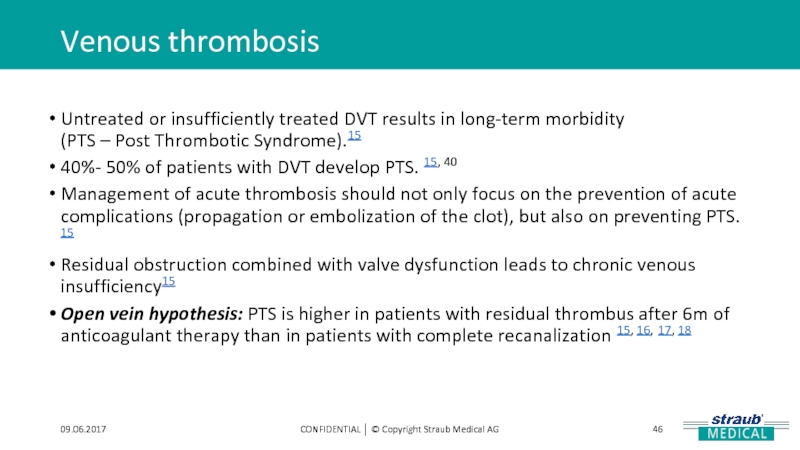
- 46. Venous thrombosis 09.06.2017 CONFIDENTIAL │ © Copyright
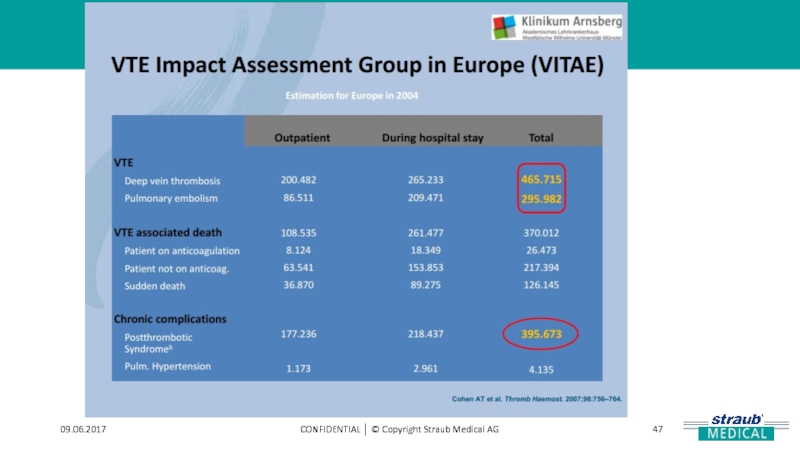
- 47. 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
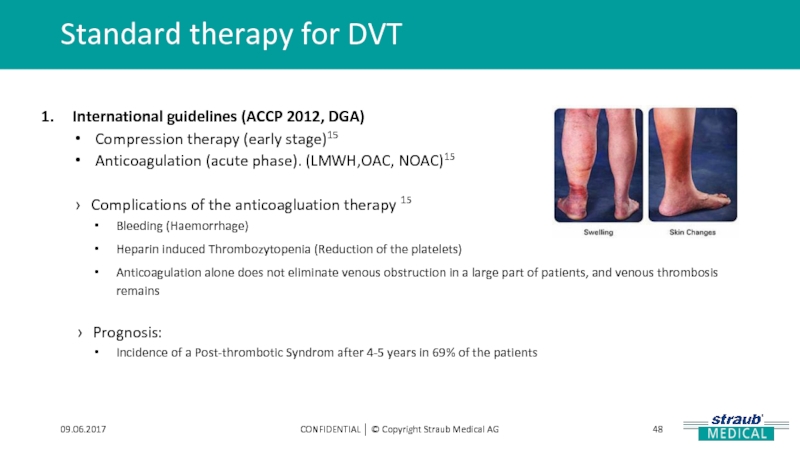
- 48. Standard therapy for DVT 09.06.2017 CONFIDENTIAL │
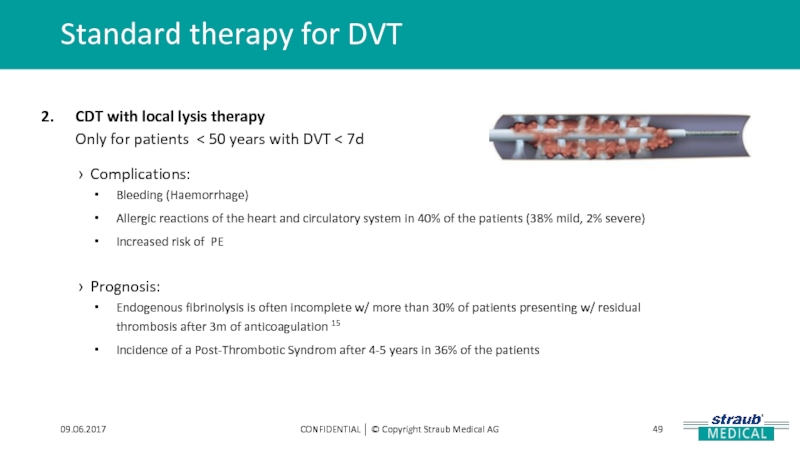
- 49. Standard therapy for DVT 09.06.2017 CONFIDENTIAL │
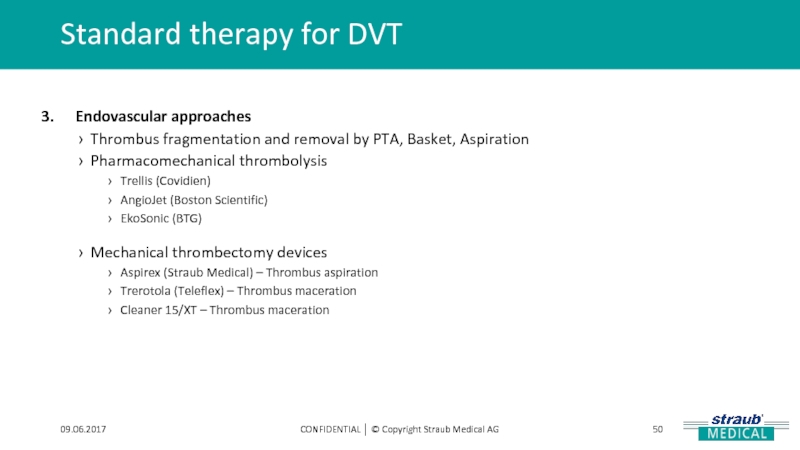
- 50. Standard therapy for DVT 09.06.2017 CONFIDENTIAL │
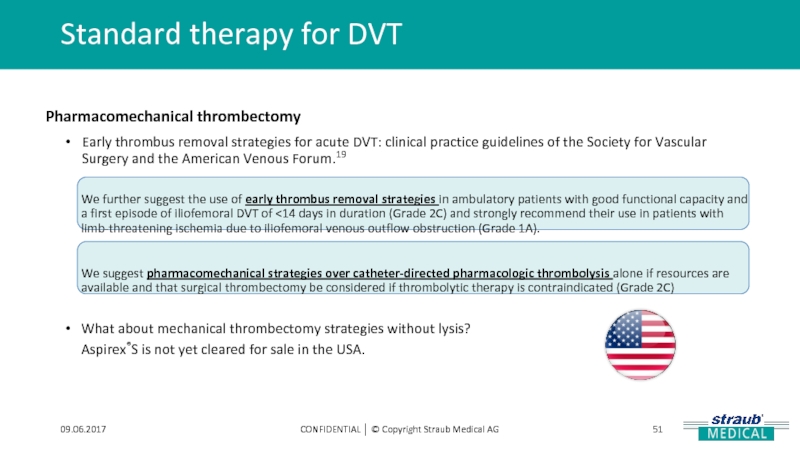
- 51. Standard therapy for DVT 09.06.2017 CONFIDENTIAL │
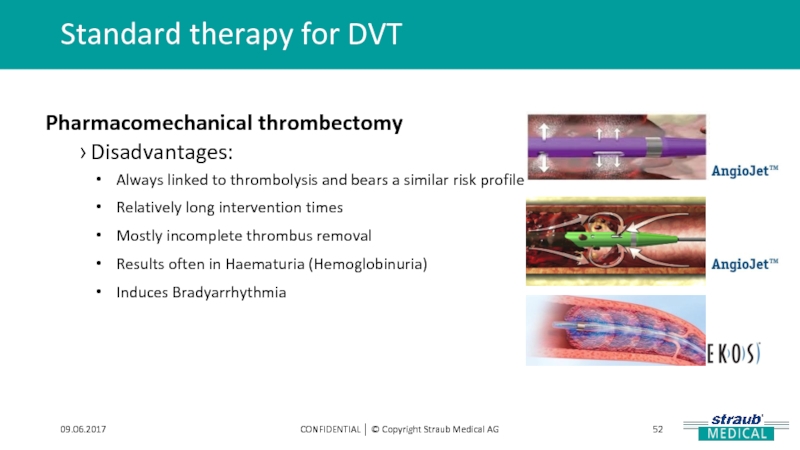
- 52. Standard therapy for DVT 09.06.2017 CONFIDENTIAL │
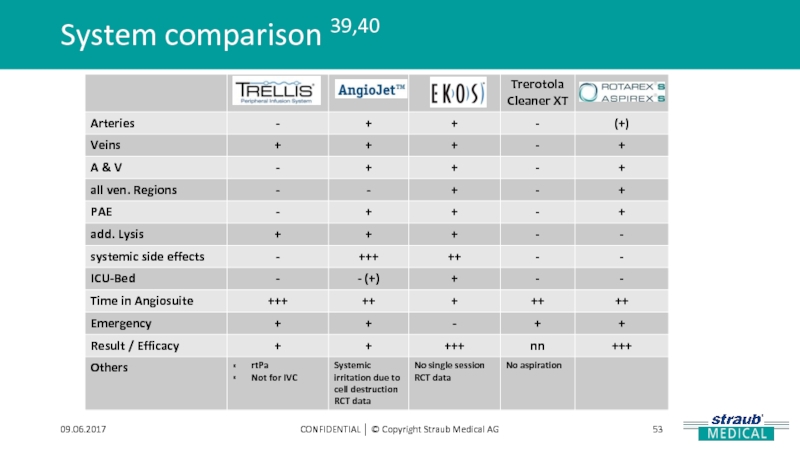
- 53. System comparison 39,40 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
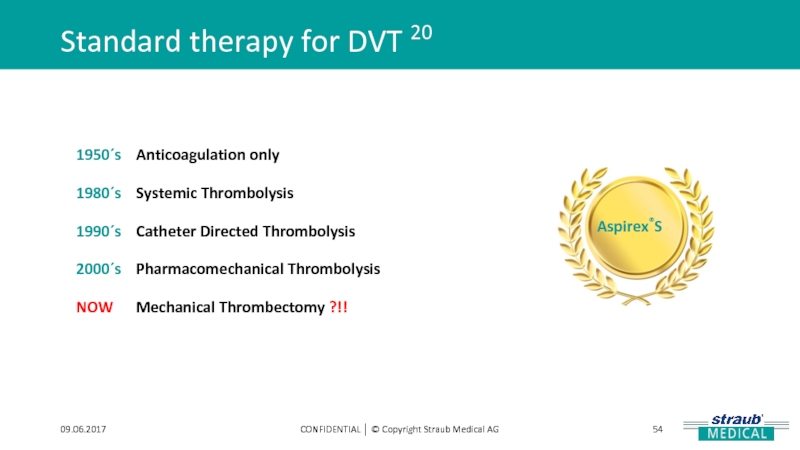
- 54. Standard therapy for DVT 20 09.06.2017 CONFIDENTIAL
- 55. Treatments with Aspirex®S 09.06.2017 CONFIDENTIAL │ ©
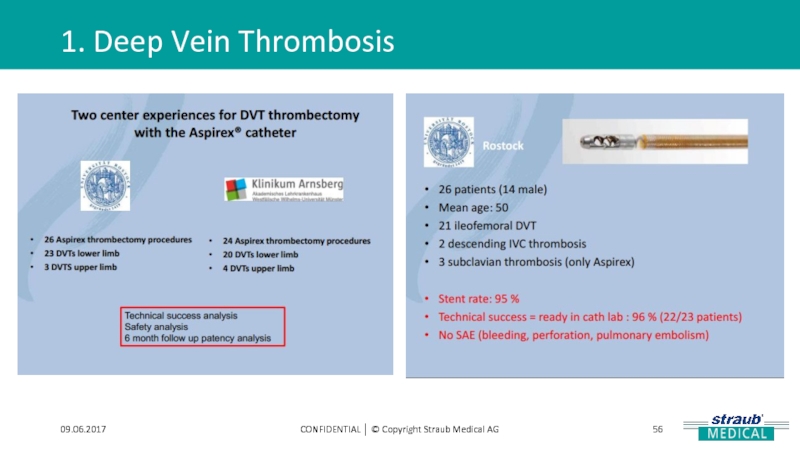
- 56. 1. Deep Vein Thrombosis 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
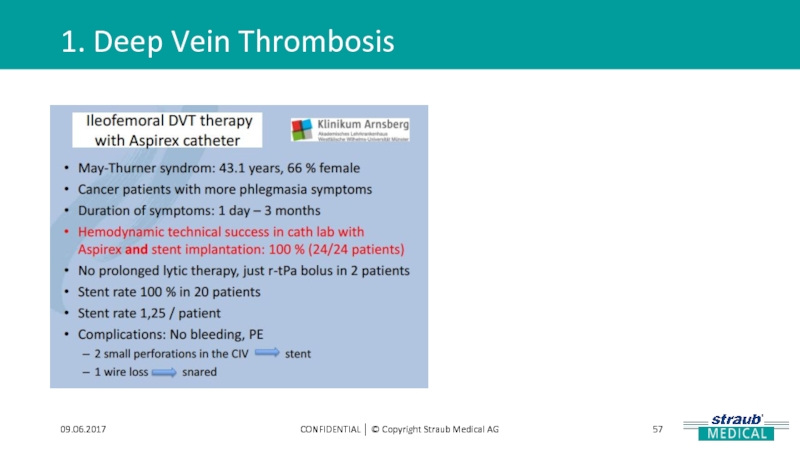
- 57. 1. Deep Vein Thrombosis 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
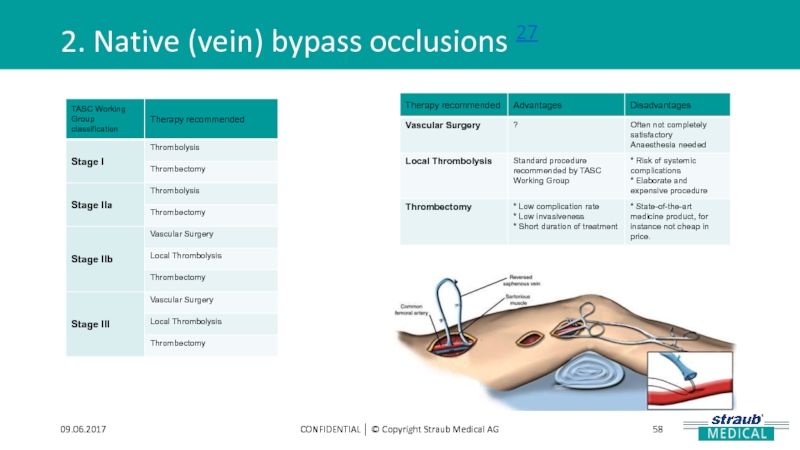
- 58. 2. Native (vein) bypass occlusions 27 09.06.2017 CONFIDENTIAL │ © Copyright Straub Medical AG
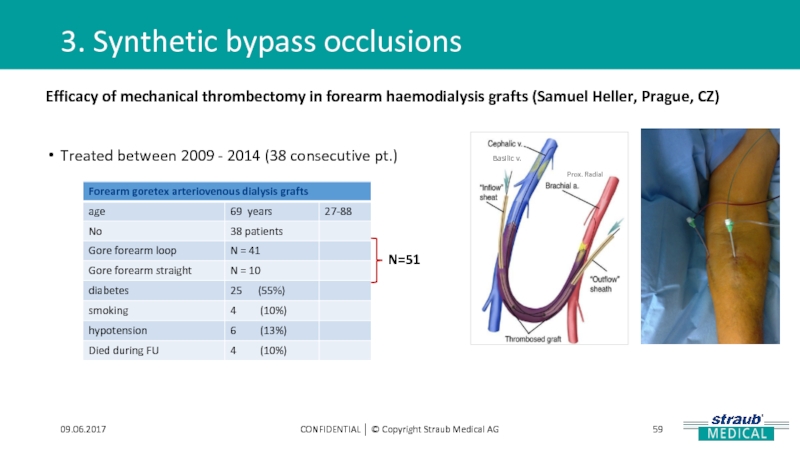
- 59. 3. Synthetic bypass occlusions 09.06.2017 CONFIDENTIAL │
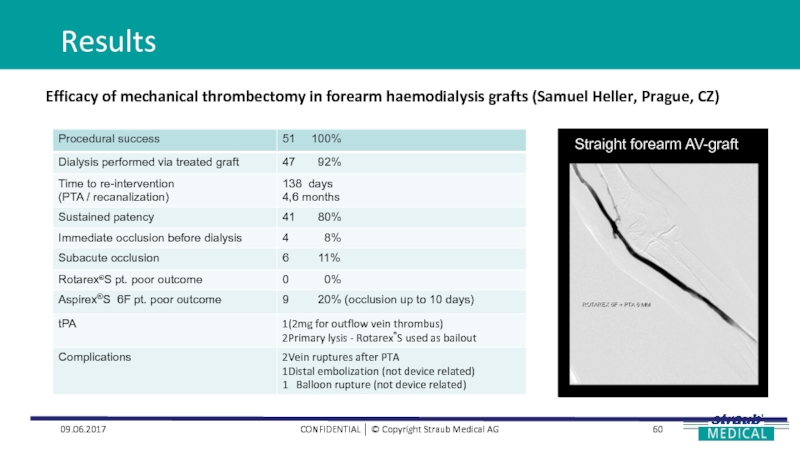
- 60. Results 09.06.2017 CONFIDENTIAL │ © Copyright Straub
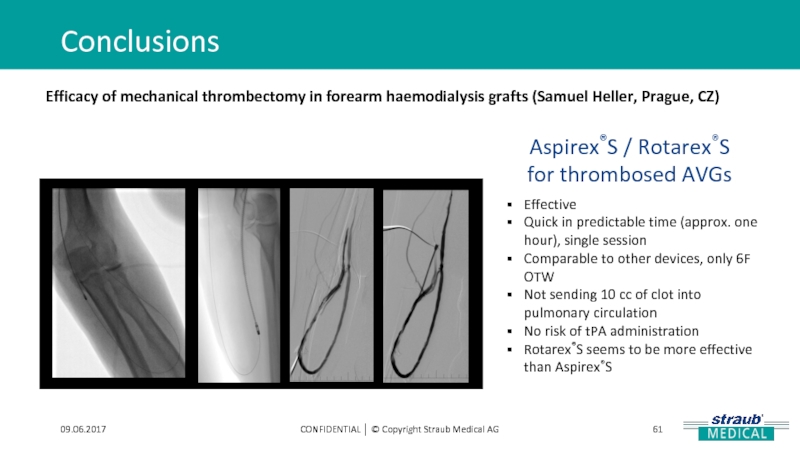
- 61. Conclusions 09.06.2017 CONFIDENTIAL │ © Copyright Straub
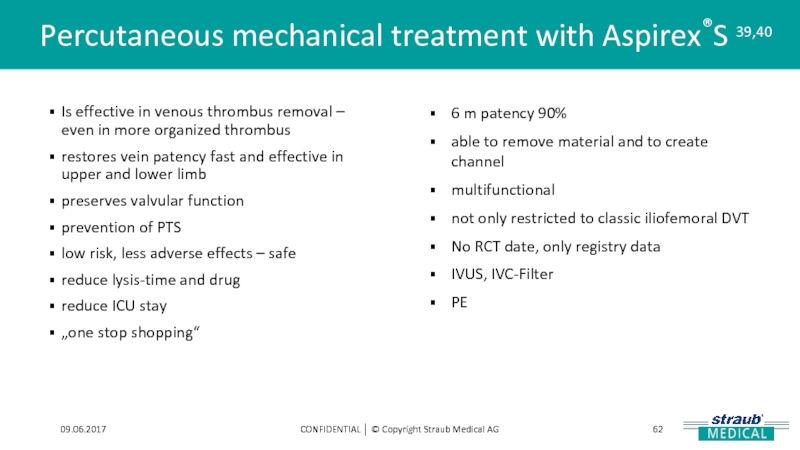
- 62. Percutaneous mechanical treatment with Aspirex®S 39,40 09.06.2017
- 63. Aspirex®S vs. Other therapies Comparison of results with other therapies
- 64. 09.06.2017 CONFIDENTIAL │ © Copyright Straub
- 65. 09.06.2017 CONFIDENTIAL │ © Copyright Straub
- 66. Freitas B, Steiner S, Bausback Y, Branzan
- 67. References: A. Peer, A. Altshuler, Straub Medical’s
Слайд 1Publications on the Straub Endovascular System
Rotarex®S - Aspirex®S - Capturex®
CONFIDENTIAL │
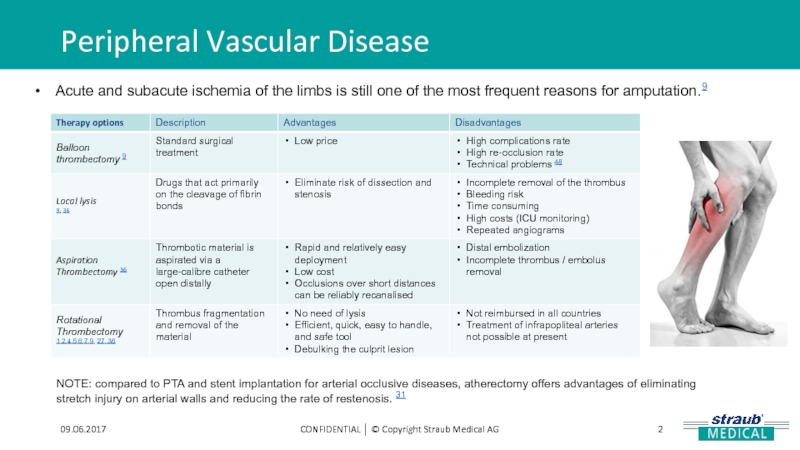
Слайд 2Peripheral Vascular Disease
CONFIDENTIAL │ © Copyright Straub Medical AG
09.06.2017
Acute and subacute
NOTE: compared to PTA and stent implantation for arterial occlusive diseases, atherectomy offers advantages of eliminating stretch injury on arterial walls and reducing the rate of restenosis. 31
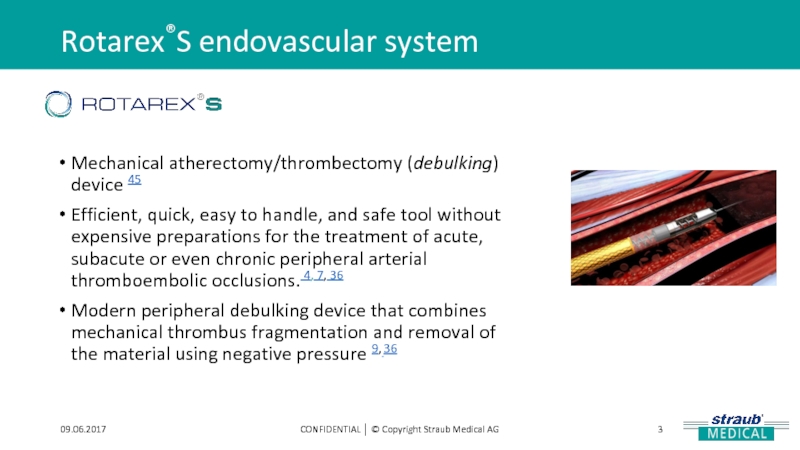
Слайд 3Rotarex®S endovascular system
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Mechanical atherectomy/thrombectomy (debulking)
Efficient, quick, easy to handle, and safe tool without expensive preparations for the treatment of acute, subacute or even chronic peripheral arterial thromboembolic occlusions. 4, 7, 36
Modern peripheral debulking device that combines mechanical thrombus fragmentation and removal of the material using negative pressure 9, 36
Слайд 4There are various clinical and experimental studies, which have shown convincing
Peripheral Vascular Disease
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Several case reports show a variety of effective treatments
(case reports presentation):
Subclavian and axillary arteries.9
In-stent occlusion
SFA-POP chronic occlusion 25
Dialysis access graft
Stent graft
Слайд 5Targets for Rotarex®S
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Native Vessel Occlusions
In-Stent
Venous and Synthetic Bypass occlusions
Visceral artery occlusion
Upper extremity artery occlusion
Combination therapy:
Rotarex®S plus DCB
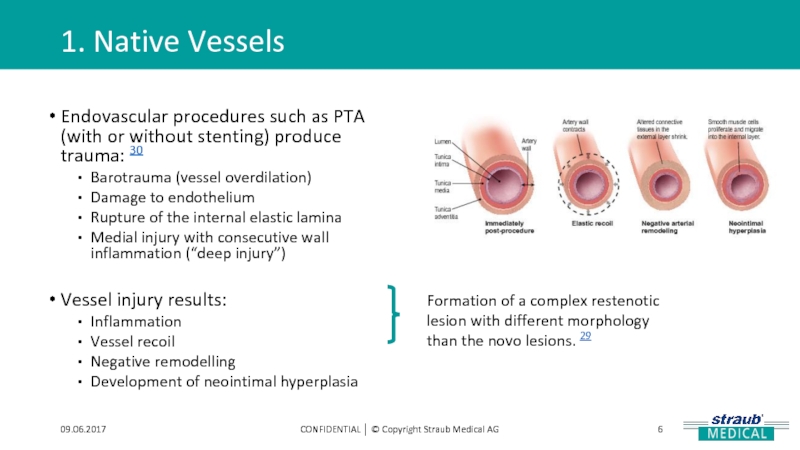
Слайд 61. Native Vessels
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Endovascular procedures such
Barotrauma (vessel overdilation)
Damage to endothelium
Rupture of the internal elastic lamina
Medial injury with consecutive wall inflammation (“deep injury”)
Vessel injury results:
Inflammation
Vessel recoil
Negative remodelling
Development of neointimal hyperplasia
Formation of a complex restenotic lesion with different morphology than the novo lesions. 29
Слайд 71. Native Vessels with Rotarex®S
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
ADVANTAGES
SATISFACTORY
Removes
Shows convincing long-term results.1
Exposes the culprit lesion, if any, for focused treatment.
RESULTS
Up to 90% amputation-free survival after 12m. 4,5,6,7, 36
Up to 97% procedural technical success rate. 1
Up to 94% clinical success. 2,4,5,6,7, 36
Efficient 4, 7
Safe device 4, 7
Simple handling 9
Short intervention time 9
REDUCES
The need for additional treatments. 1
The need for thrombolysis in a significant portion of patients.1
Bleeding complications
Costs (e.g. of monitoring patients at the ICU). 4, 9
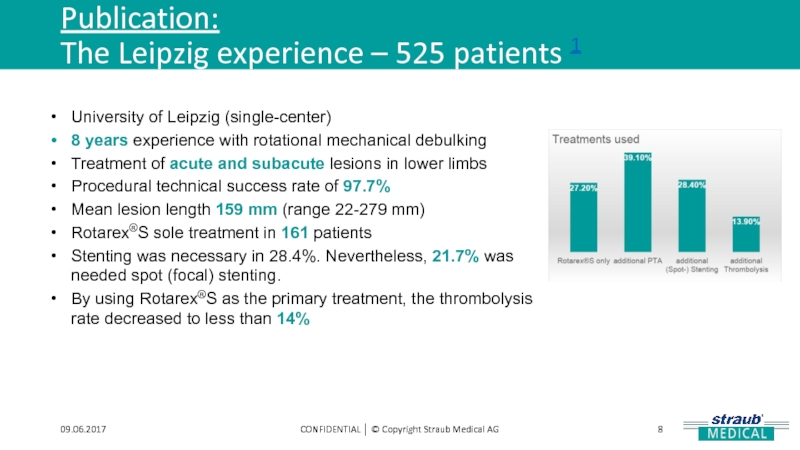
Слайд 8Publication:
The Leipzig experience – 525 patients 1
09.06.2017
CONFIDENTIAL │ © Copyright
University of Leipzig (single-center)
8 years experience with rotational mechanical debulking
Treatment of acute and subacute lesions in lower limbs
Procedural technical success rate of 97.7%
Mean lesion length 159 mm (range 22-279 mm)
Rotarex®S sole treatment in 161 patients
Stenting was necessary in 28.4%. Nevertheless, 21.7% was needed spot (focal) stenting.
By using Rotarex®S as the primary treatment, the thrombolysis rate decreased to less than 14%
Слайд 9Publication:
The Leipzig experience – 525 patients 1
09.06.2017
CONFIDENTIAL │ © Copyright
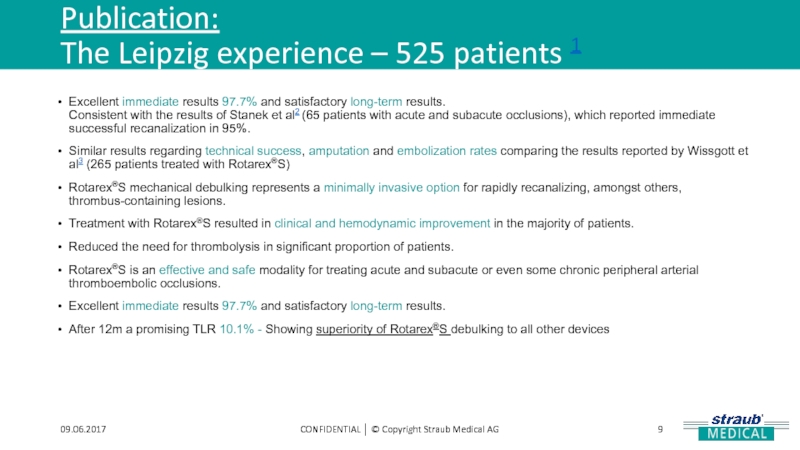
Excellent immediate results 97.7% and satisfactory long-term results.
Consistent with the results of Stanek et al2 (65 patients with acute and subacute occlusions), which reported immediate successful recanalization in 95%.
Similar results regarding technical success, amputation and embolization rates comparing the results reported by Wissgott et al3 (265 patients treated with Rotarex®S)
Rotarex®S mechanical debulking represents a minimally invasive option for rapidly recanalizing, amongst others, thrombus-containing lesions.
Treatment with Rotarex®S resulted in clinical and hemodynamic improvement in the majority of patients.
Reduced the need for thrombolysis in significant proportion of patients.
Rotarex®S is an effective and safe modality for treating acute and subacute or even some chronic peripheral arterial thromboembolic occlusions.
Excellent immediate results 97.7% and satisfactory long-term results.
After 12m a promising TLR 10.1% - Showing superiority of Rotarex®S debulking to all other devices
Слайд 10Comment on Stanek et al, p.49-56 4
09.06.2017
CONFIDENTIAL │ © Copyright Straub
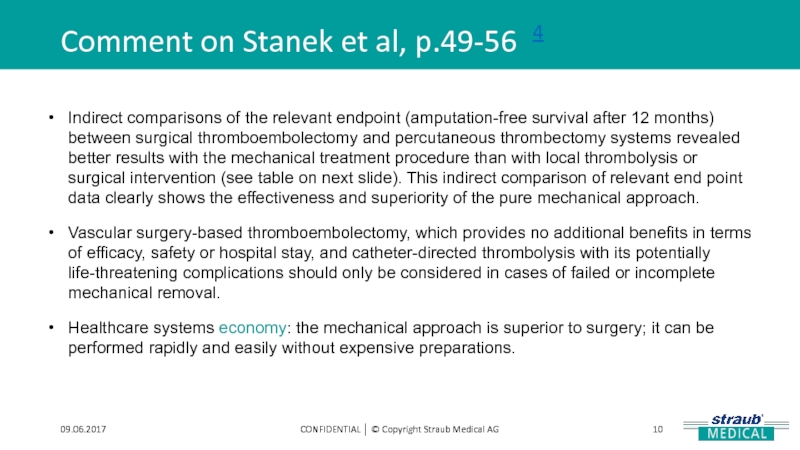
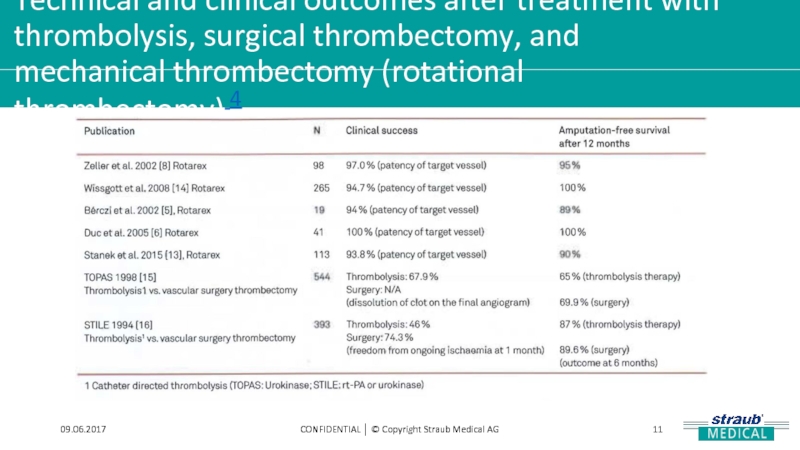
Indirect comparisons of the relevant endpoint (amputation-free survival after 12 months) between surgical thromboembolectomy and percutaneous thrombectomy systems revealed better results with the mechanical treatment procedure than with local thrombolysis or surgical intervention (see table on next slide). This indirect comparison of relevant end point data clearly shows the effectiveness and superiority of the pure mechanical approach.
Vascular surgery-based thromboembolectomy, which provides no additional benefits in terms of efficacy, safety or hospital stay, and catheter-directed thrombolysis with its potentially life-threatening complications should only be considered in cases of failed or incomplete mechanical removal.
Healthcare systems economy: the mechanical approach is superior to surgery; it can be performed rapidly and easily without expensive preparations.
Слайд 11Technical and clinical outcomes after treatment with thrombolysis, surgical thrombectomy, and
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
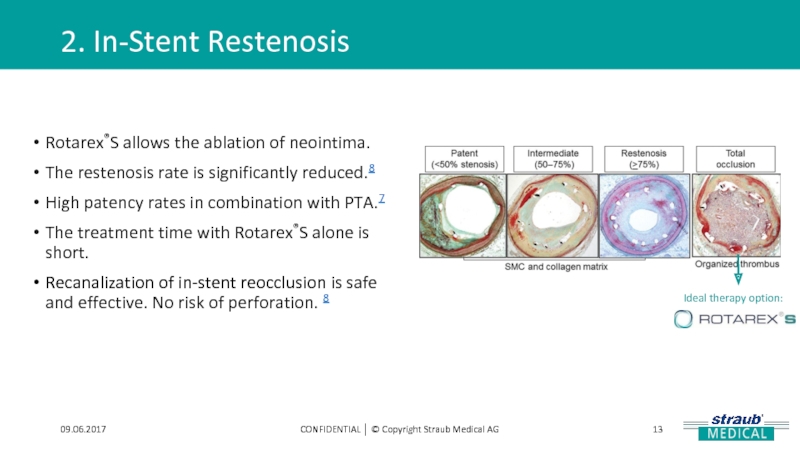
Слайд 122. In-Stent Restenosis
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
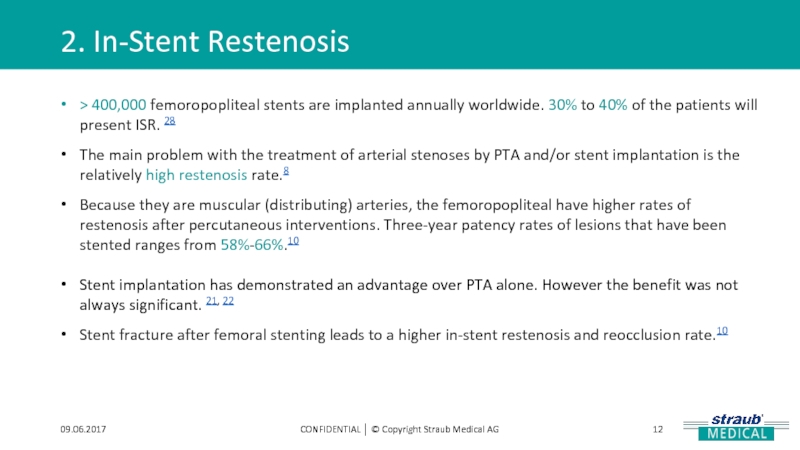
> 400,000 femoropopliteal
The main problem with the treatment of arterial stenoses by PTA and/or stent implantation is the relatively high restenosis rate.8
Because they are muscular (distributing) arteries, the femoropopliteal have higher rates of restenosis after percutaneous interventions. Three-year patency rates of lesions that have been stented ranges from 58%-66%.10
Stent implantation has demonstrated an advantage over PTA alone. However the benefit was not always significant. 21, 22
Stent fracture after femoral stenting leads to a higher in-stent restenosis and reocclusion rate.10
Слайд 132. In-Stent Restenosis
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Rotarex®S allows the
The restenosis rate is significantly reduced.8
High patency rates in combination with PTA.7
The treatment time with Rotarex®S alone is short.
Recanalization of in-stent reocclusion is safe and effective. No risk of perforation. 8
Ideal therapy option:
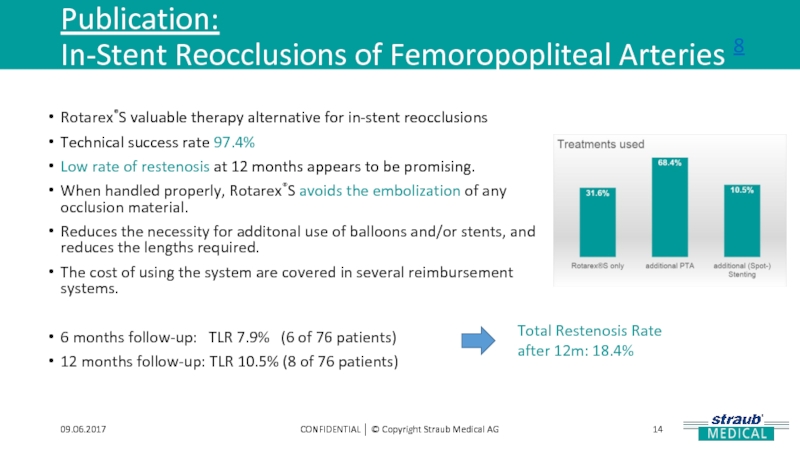
Слайд 14Publication:
In-Stent Reocclusions of Femoropopliteal Arteries 8
09.06.2017
CONFIDENTIAL │ © Copyright Straub
Rotarex®S valuable therapy alternative for in-stent reocclusions
Technical success rate 97.4%
Low rate of restenosis at 12 months appears to be promising.
When handled properly, Rotarex®S avoids the embolization of any occlusion material.
Reduces the necessity for additonal use of balloons and/or stents, and reduces the lengths required.
The cost of using the system are covered in several reimbursement systems.
6 months follow-up: TLR 7.9% (6 of 76 patients)
12 months follow-up: TLR 10.5% (8 of 76 patients)
Total Restenosis Rate
after 12m: 18.4%
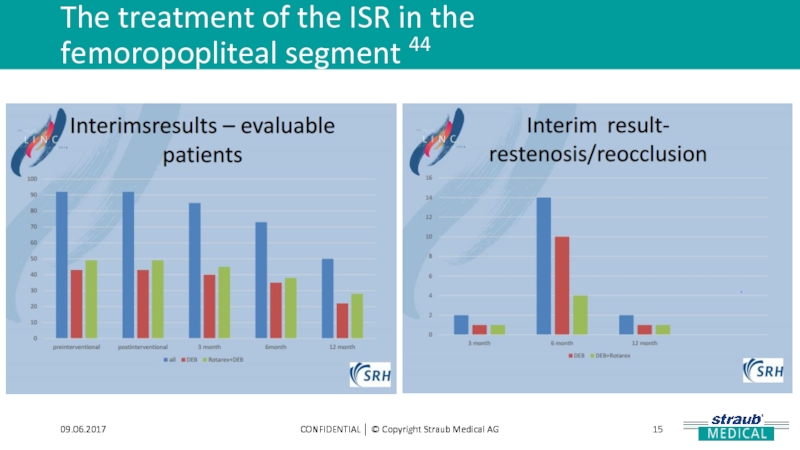
Слайд 15The treatment of the ISR in the
femoropopliteal segment 44
09.06.2017
CONFIDENTIAL │ ©
Слайд 16The treatment of the ISR in the
femoropopliteal segment 44
09.06.2017
CONFIDENTIAL │ ©
Слайд 173. Venous and Synthetic Bypass occlusions
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical
Acute and subacute ischemia of the legs in femoropopliteal bypass occlusion is a dramatic situation that endangers the survival of the limbs. 12
Local lysis has been established as an alternative measure in addition to the established vascular intervention (Fogarty, endarterectomy, another bypass operation). 12
But do we really need lysis? (see presentation Bruno Migliara!!!!) 41
Pure mechanical therapy has been proven as an additional therapy option with less safety risks and more benefits.12
Слайд 18Publication:
Acute femoropopliteal bypass occlusion
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Patency rate 100% 86%
Technical
Complications - -
6 months
follow up 13
12 months
follow up 12
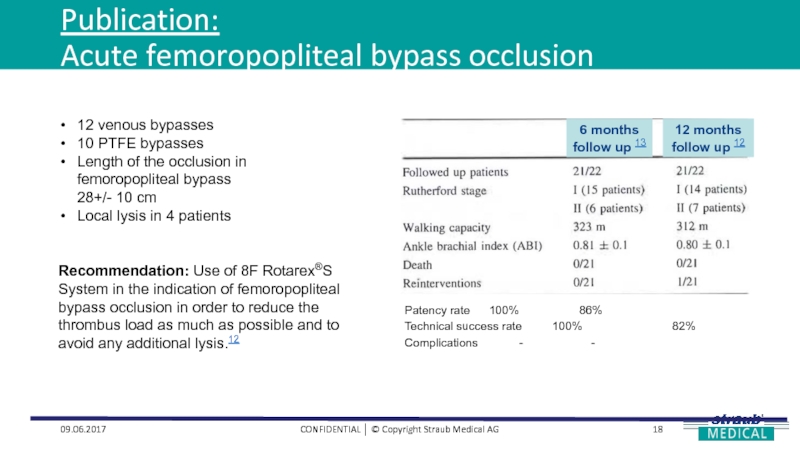
12 venous bypasses
10 PTFE bypasses
Length of the occlusion in femoropopliteal bypass 28+/- 10 cm
Local lysis in 4 patients
Recommendation: Use of 8F Rotarex®S System in the indication of femoropopliteal bypass occlusion in order to reduce the thrombus load as much as possible and to avoid any additional lysis.12
Слайд 19Publications:
Recanalization of Acute and Subacute Venous and Synthetic Bypass-Graft Occlusions 14
09.06.2017
CONFIDENTIAL
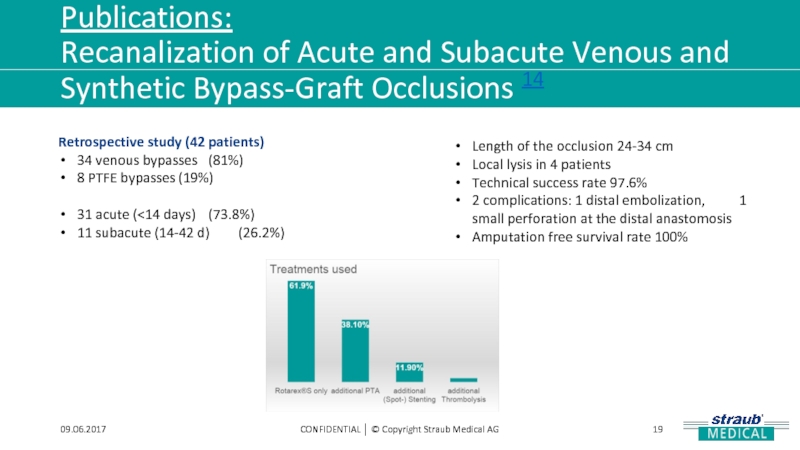
Length of the occlusion 24-34 cm
Local lysis in 4 patients
Technical success rate 97.6%
2 complications: 1 distal embolization, 1 small perforation at the distal anastomosis
Amputation free survival rate 100%
Retrospective study (42 patients)
34 venous bypasses (81%)
8 PTFE bypasses (19%)
31 acute (<14 days) (73.8%)
11 subacute (14-42 d) (26.2%)
Слайд 204. Visceral arteries
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Superior mesenteric artery
Treatment of choice: laparotomy with thrombectomy and percutaneous thrombectomy 37
The two main percutaneous methods are:
Aspiration thrombectomy, in which thrombus is removed by suction
Mechanical thrombectomy, using different automated devices to fragment and remove embolus
Слайд 2109.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Case Report:
Percutaneous mechanical thrombectomy of
Percutaneous Mechanical Thrombectomy showed good results with dramatic improvement of symptoms present immediately in all patients.
No post procedural complications were present in our patients probably due to absence of any additional pharmacologic lysis.
Advantages of mechanical thrombectomy in SMA:
Rapid and effective removal of large thrombus
No need for local thrombolysis and its minimal invasiveness, thus avoiding the complications associated with surgery.
Слайд 225. Upper limb arteries – Subclavian
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical
Proximal subclavian artery occlusion is relatively rare and usually asymptomatic.
In the rare symptomatic cases, surgical or endovascular intervention is indicated:
Fogarty balloon thrombectomy: technical problems and complications can occur. 24
Subclavian bypass operation: open surgery.24
Local lysis infiltration: time-consuming and expensive, requires ICU and angiograms.24
Thrombectomy devices: minimization of bleeding complications, less invasive and time-efficiency, short hospital stay.24, 26
Conclusion: Rotational thrombectomy together with optional local low-dose lysis in an acute occluded subclavian artery is a promising therapeutic option. 24
Слайд 241. Rotarex®S + DCB
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
The high
Restenosis can occur in 40-60% of patients. 22
Regardless of all the technological progresses in balloons, the high rate of restenosis is problematic. 22, 23
DCB is an effective treatment of short ISR lesions, but not efficient in more complex lesions.30
The DCB seems to be a prevention of restenosis at the six-month follow-up.22
THUNDER and PACIFIER study concluded that the restenosis rate is reduced if DCB are used.22
Rotarex®S + DCB: Hemodynamic success demonstrated. 22
Rotarex®S + DCB: is safe and effective and with promising results. 8, 22
Conclusion:
Early data suggest debulking and modifying the plaque before DCB treatment seems to be of key importance in more complex ISR lesions.30
Слайд 25Mechanical Debulking + DEB 22
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
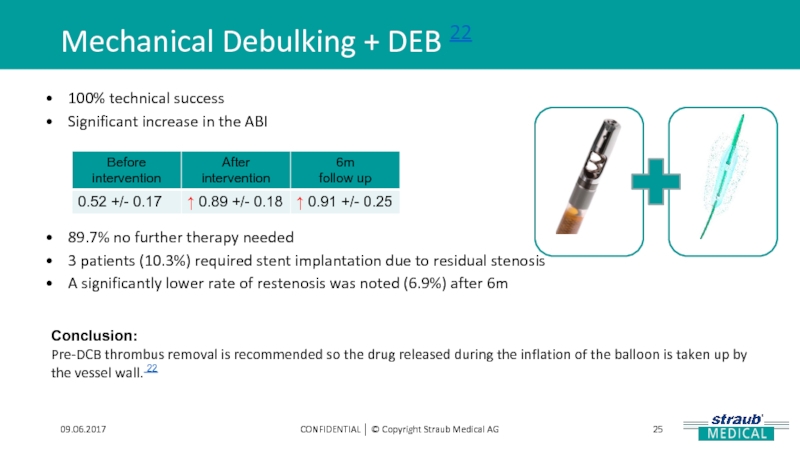
100%
Significant increase in the ABI
89.7% no further therapy needed
3 patients (10.3%) required stent implantation due to residual stenosis
A significantly lower rate of restenosis was noted (6.9%) after 6m
Conclusion:
Pre-DCB thrombus removal is recommended so the drug released during the inflation of the balloon is taken up by the vessel wall. 22
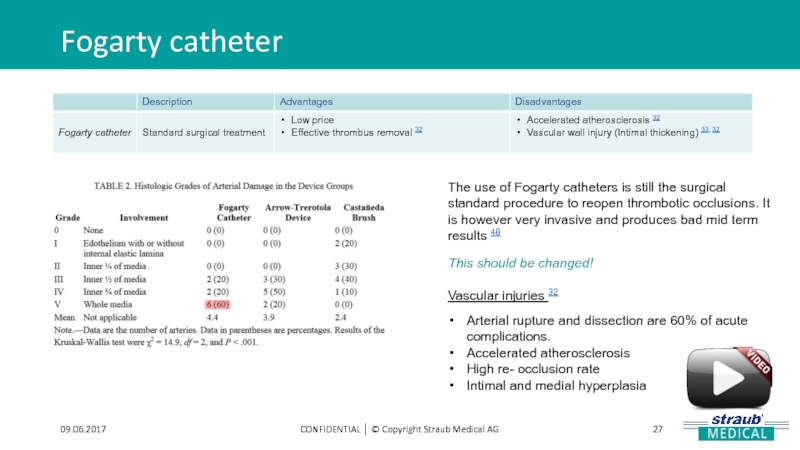
Слайд 27Fogarty catheter
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
The use of Fogarty
This should be changed!
Vascular injuries 32
Arterial rupture and dissection are 60% of acute complications.
Accelerated atherosclerosis
High re- occlusion rate
Intimal and medial hyperplasia
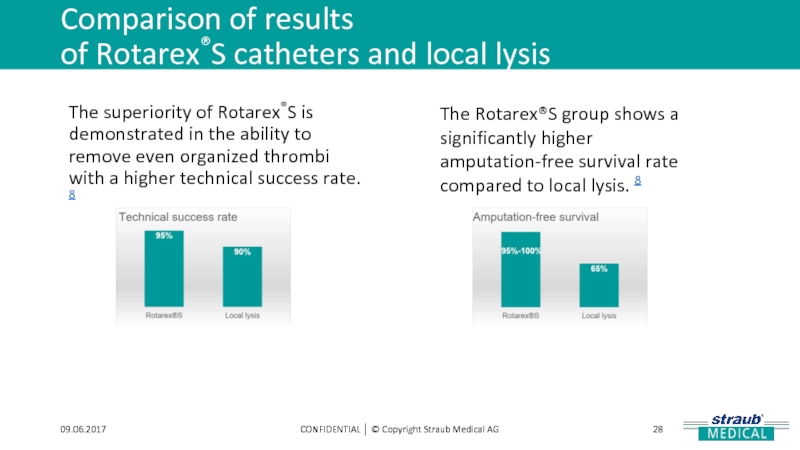
Слайд 28Comparison of results
of Rotarex®S catheters and local lysis
09.06.2017
CONFIDENTIAL │ ©
The superiority of Rotarex®S is demonstrated in the ability to remove even organized thrombi with a higher technical success rate. 8
The Rotarex®S group shows a significantly higher amputation-free survival rate compared to local lysis. 8
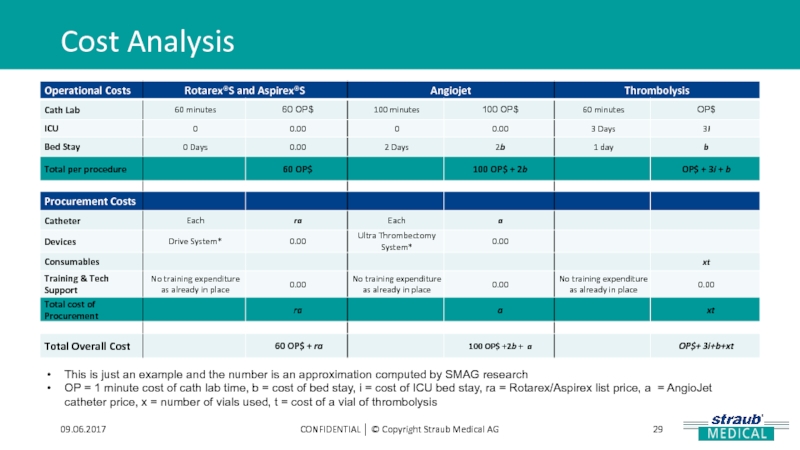
Слайд 29Cost Analysis
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
This is just an
OP = 1 minute cost of cath lab time, b = cost of bed stay, i = cost of ICU bed stay, ra = Rotarex/Aspirex list price, a = AngioJet catheter price, x = number of vials used, t = cost of a vial of thrombolysis
Слайд 31Rotarex®S vs. Jetstream (example 1)
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Jetstream:
What about Rotarex®S ?
Different studies have proved:
Up to 97% procedural technical success rate. 1
Up to 94% clinical success. 2,4,5,6,7
Слайд 32
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Look at the TVR /
- Compare with the Scheinert Data
- Look at Wissgott Publication
Слайд 34Rotarex®S vs. Jetstream (example 2)
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
The
Слайд 35Rotarex®S vs. Local Lysis 38
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Lysis
Слайд 36Mechanical thrombectomy vs.
Ultrasound-enhanced thrombolysis 27
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Blood
Rotarex®S significantly shorter
Слайд 37Mechanical thrombectomy vs.
Ultrasound-enhanced thrombolysis 27
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
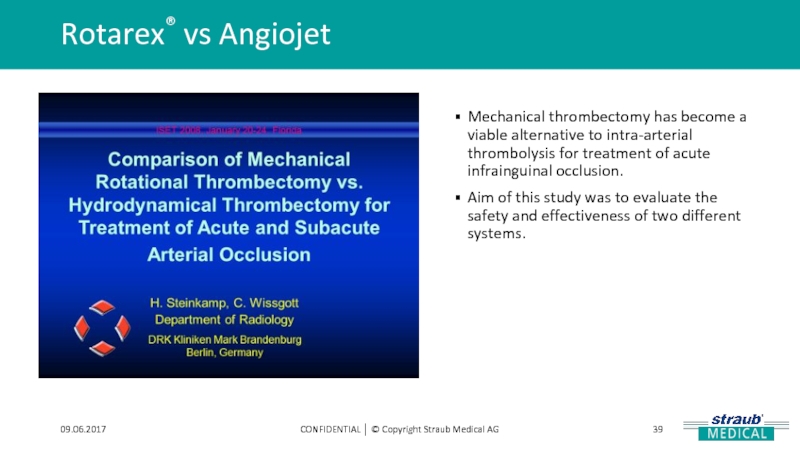
Слайд 39Rotarex® vs Angiojet
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Mechanical thrombectomy has
Aim of this study was to evaluate the safety and effectiveness of two different systems.
Слайд 43Rotarex®S vs. Laser Atherectomy
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Look at
Слайд 44Current clinical studies
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Prospective, non-randomized, multi-center,
40 patients
To evaluate the safety and efficacy of recanalization of acute and subacute (up to 12 weeks) femoropopliteal stent occlusions with the Rotarex®S catheter.
Слайд 46Venous thrombosis
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Untreated or insufficiently treated
40%- 50% of patients with DVT develop PTS. 15, 40
Management of acute thrombosis should not only focus on the prevention of acute complications (propagation or embolization of the clot), but also on preventing PTS. 15
Residual obstruction combined with valve dysfunction leads to chronic venous insufficiency15
Open vein hypothesis: PTS is higher in patients with residual thrombus after 6m of anticoagulant therapy than in patients with complete recanalization 15, 16, 17, 18
Слайд 48Standard therapy for DVT
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
International guidelines
Compression therapy (early stage)15
Anticoagulation (acute phase). (LMWH,OAC, NOAC)15
Complications of the anticoagluation therapy 15
Bleeding (Haemorrhage)
Heparin induced Thrombozytopenia (Reduction of the platelets)
Anticoagulation alone does not eliminate venous obstruction in a large part of patients, and venous thrombosis remains
Prognosis:
Incidence of a Post-thrombotic Syndrom after 4-5 years in 69% of the patients
Слайд 49Standard therapy for DVT
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
CDT with
Only for patients < 50 years with DVT < 7d
Complications:
Bleeding (Haemorrhage)
Allergic reactions of the heart and circulatory system in 40% of the patients (38% mild, 2% severe)
Increased risk of PE
Prognosis:
Endogenous fibrinolysis is often incomplete w/ more than 30% of patients presenting w/ residual thrombosis after 3m of anticoagulation 15
Incidence of a Post-Thrombotic Syndrom after 4-5 years in 36% of the patients
Слайд 50Standard therapy for DVT
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Endovascular approaches
Thrombus
Pharmacomechanical thrombolysis
Trellis (Covidien)
AngioJet (Boston Scientific)
EkoSonic (BTG)
Mechanical thrombectomy devices
Aspirex (Straub Medical) – Thrombus aspiration
Trerotola (Teleflex) – Thrombus maceration
Cleaner 15/XT – Thrombus maceration
Слайд 51Standard therapy for DVT
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Pharmacomechanical thrombectomy
Early
We further suggest the use of early thrombus removal strategies in ambulatory patients with good functional capacity and a first episode of iliofemoral DVT of <14 days in duration (Grade 2C) and strongly recommend their use in patients with limb-threatening ischemia due to iliofemoral venous outflow obstruction (Grade 1A).
We suggest pharmacomechanical strategies over catheter-directed pharmacologic thrombolysis alone if resources are available and that surgical thrombectomy be considered if thrombolytic therapy is contraindicated (Grade 2C)
What about mechanical thrombectomy strategies without lysis?
Aspirex®S is not yet cleared for sale in the USA.
Слайд 52Standard therapy for DVT
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Pharmacomechanical thrombectomy
Disadvantages:
Always
Relatively long intervention times
Mostly incomplete thrombus removal
Results often in Haematuria (Hemoglobinuria)
Induces Bradyarrhythmia
Слайд 54Standard therapy for DVT 20
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
1950´s
1980´s Systemic Thrombolysis
1990´s Catheter Directed Thrombolysis
2000´s Pharmacomechanical Thrombolysis
NOW Mechanical Thrombectomy ?!!
Aspirex®S
Слайд 55Treatments with Aspirex®S
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Patients in the
Deep vein thrombosis
Native (vein) bypass occlusions
Synthetic bypass occlusion
Слайд 593. Synthetic bypass occlusions
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Treated between
N=51
Efficacy of mechanical thrombectomy in forearm haemodialysis grafts (Samuel Heller, Prague, CZ)
Слайд 60Results
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Straight forearm AV-graft
Efficacy of mechanical
Слайд 61Conclusions
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Effective
Quick in predictable time (approx.
Comparable to other devices, only 6F OTW
Not sending 10 cc of clot into pulmonary circulation
No risk of tPA administration
Rotarex®S seems to be more effective than Aspirex®S
Aspirex®S / Rotarex®S
for thrombosed AVGs
Efficacy of mechanical thrombectomy in forearm haemodialysis grafts (Samuel Heller, Prague, CZ)
Слайд 62Percutaneous mechanical treatment with Aspirex®S 39,40
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical
Is effective in venous thrombus removal – even in more organized thrombus
restores vein patency fast and effective in upper and lower limb
preserves valvular function
prevention of PTS
low risk, less adverse effects – safe
reduce lysis-time and drug
reduce ICU stay
„one stop shopping“
6 m patency 90%
able to remove material and to create channel
multifunctional
not only restricted to classic iliofemoral DVT
No RCT date, only registry data
IVUS, IVC-Filter
PE
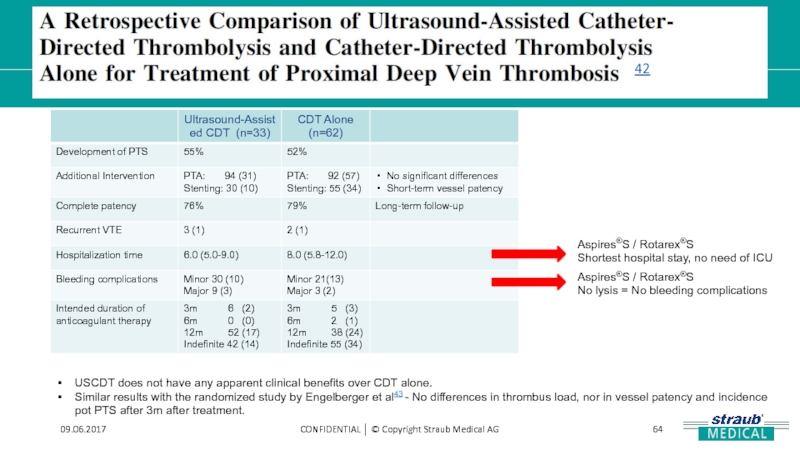
Слайд 64
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Aspires®S / Rotarex®S
No lysis =
Aspires®S / Rotarex®S
Shortest hospital stay, no need of ICU
USCDT does not have any apparent clinical benefits over CDT alone.
Similar results with the randomized study by Engelberger et al43 - No differences in thrombus load, nor in vessel patency and incidence pot PTS after 3m after treatment.
42
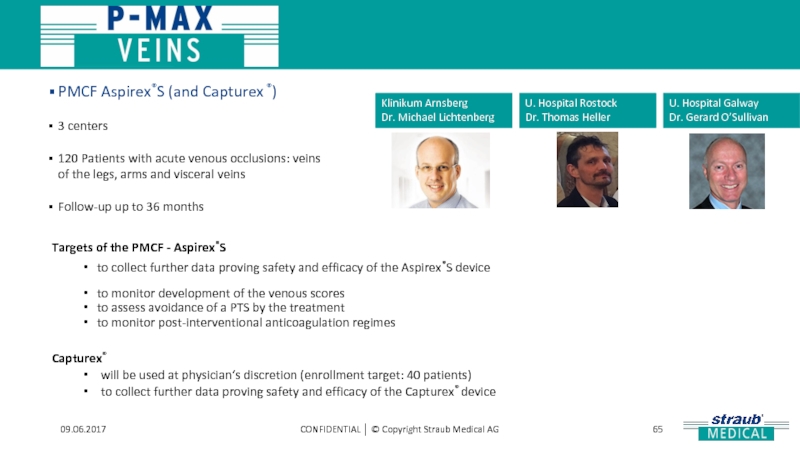
Слайд 65
09.06.2017
CONFIDENTIAL │ © Copyright Straub Medical AG
Targets of the PMCF -
to collect further data proving safety and efficacy of the Aspirex®S device
to monitor development of the venous scores
to assess avoidance of a PTS by the treatment
to monitor post-interventional anticoagulation regimes
Capturex®
will be used at physician‘s discretion (enrollment target: 40 patients)
to collect further data proving safety and efficacy of the Capturex® device
Klinikum Arnsberg
Dr. Michael Lichtenberg
U. Hospital Rostock
Dr. Thomas Heller
U. Hospital Galway
Dr. Gerard O’Sullivan
PMCF Aspirex®S (and Capturex ®)
3 centers
120 Patients with acute venous occlusions: veins of the legs, arms and visceral veins
Follow-up up to 36 months
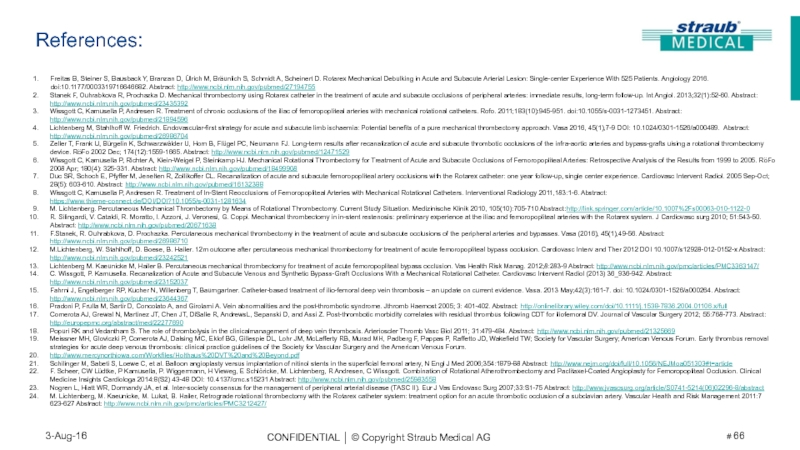
Слайд 66Freitas B, Steiner S, Bausback Y, Branzan D, Ülrich M, Bräunlich
Stanek F, Ouhrabkova R, Prochazka D. Mechanical thrombectomy using Rotarex catheter in the treatment of acute and subacute occlusions of peripheral arteries: immediate results, long-term follow-up. Int Angiol. 2013;32(1):52-60. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/23435392
Wissgott C, Kamusella P, Andresen R. Treatment of chronic occlusions of the iliac of femoropopliteal arteries with mechanical rotational catheters. Rofo. 2011;183(10):945-951. doi:10.1055/s-0031-1273451. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/21894596
Lichtenberg M, Stahlhoff W. Friedrich. Endovascular-first strategy for acute and subacute limb ischaemia: Potential benefits of a pure mechanical thrombectomy approach. Vasa 2016, 45(1),7-9 DOI: 10.1024/0301-1526/a000489. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/26986704
Zeller T, Frank U, Bürgelin K, Schwarzwälder U, Horn B, Flügel PC, Neumann FJ. Long-term results after recanalization of acute and subacute thrombotic occlusions of the infra-aortic arteries and bypass-grafts uising a rotational thrombectomy device. RöFo 2002 Dec; 174(12):1559-1665. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/12471529
Wissgott C, Kamusella P, Richter A, Klein-Weigel P, Steinkamp HJ. Mechanical Rotational Thrombectomy for Treatment of Acute and Subacute Occlusions of Femoropopliteal Arteries: Retrospective Analysis of the Results from 1999 to 2005. RöFo 2008 Apr; 180(4): 325-331. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/18499908
Duc SR, Schoch E, Pfyffer M, Jenelten R, Zollikoffer CL. Recanalization of acute and subacute femoropopliteal artery occlusions with the Rotarex catheter: one year follow-up, single center experience. Cardiovasc Intervent Radiol. 2005 Sep-Oct; 28(5): 603-610. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/16132388
Wissgott C, Kamusella P, Andresen R. Treatment of In-Stent Reocclusions of Femoropopliteal Arteries with Mechanical Rotational Catheters. Interventional Radiology 2011,183:1-6. Abstract: https://www.thieme-connect.de/DOI/DOI?10.1055/s-0031-1281634
M. Lichtenberg. Percutaneous Mechanical Thrombectomy by Means of Rotational Thrombectomy. Current Study Situation. Medizinische Klinik 2010, 105(10):705-710 Abstract:http://link.springer.com/article/10.1007%2Fs00063-010-1122-0
R. Silingardi, V. Cataldi, R. Moratto, I. Azzoni, J. Veronesi, G. Coppi. Mechanical thrombectomy in in-stent restenosis: preliminary experience at the iliac and femoropopliteal arteries with the Rotarex system. J Cardiovasc surg 2010; 51:543-50. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/20671638
F.Stanek, R. Ouhrabkova, D. Prochazka. Percutaneous mechanical thrombectomy in the treatment of acute and subacute occlusions of the peripheral arteries and bypasses. Vasa (2016), 45(1),49-56. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/26986710
M.Lichtenberg, W. Stahlhoff, D. Boese, B. Hailer. 12m outcome after percutaneous mechanical thrombectomy for treatment of acute femoropopliteal bypass occlusion. Cardiovasc Interv and Ther 2012 DOI 10.1007/s12928-012-0152-x Abstract: http://www.ncbi.nlm.nih.gov/pubmed/23242521
Lichtenberg M. Kaeunicke M, Hailer B. Percutaneous mechanical thrombectomy for treatment of acute femoropopliteal bypass occlusion. Vas Health Risk Manag. 2012;8:283-9 Abstract: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3363147/
C. Wissgott, P. Kamusella. Recanalization of Acute and Subacute Venous and Synthetic Bypass-Graft Occlusions With a Mechanical Rotational Catheter. Cardiovasc Intervent Radiol (2013) 36_936-942. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/23152037
Fahrni J, Engelberger RP, Kucher N, Willenberg T, Baumgartner. Catheter-based treatment of ilio-femoral deep vein thrombosis – an update on current evidence. Vasa. 2013 May;42(3):161-7. doi: 10.1024/0301-1526/a000264. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/23644367
Pradoni P, Frulla M, Sartir D, Concolato A, and Girolami A. Vein abnormalities and the post-thrombotic syndrome. Jthromb Haemost 2005; 3: 401-402. Abstract: http://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2004.01106.x/full
Comerota AJ, Grewal N, Martinez JT, Chen JT, DiSalle R, AndrewsL, Sepanski D, and Assi Z. Post-thrombotic morbidity correlates with residual thrombus following CDT for iliofemoral DV. Journal of Vascular Surgery 2012; 55:768-773. Abstract: http://europepmc.org/abstract/med/22277690
Popuri RK and Vedantham S. The role of thrombolysis in the clinicalmanagement of deep vein thrombosis. Arterioscler Thromb Vasc Biol 2011; 31:479-484. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/21325669
Meissner MH, Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Lohr JM, McLafferty RB, Murad MH, Padberg F, Pappas P, Raffetto JD, Wakefield TW; Society for Vascular Surgery; American Venous Forum. Early thrombus removal strategies for acute deep venous thrombosis: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum.
http://www.mercynorthiowa.com/Workfiles/Holthaus%20DVT%20and%20Beyond.pdf
Schilinger M, Sabeti S, Loewe C, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery, N Engl J Med 2006;354:1879-88 Abstract: http://www.nejm.org/doi/full/10.1056/NEJMoa051303#t=article
F. Scheer, CW Lüdtke, P Kamusella, P. Wiggermann, H Vieweg, E Schlöricke, M. Lichtenberg, R Andresen, C Wissgott. Combination of Rotational Atherothrombectomy and Paclitaxel-Coated Angioplasty for Femoropopliteal Occlusion. Clinical Medicine Insights Cardiologa 2014:8(S2) 43-48 DOI: 10.4137/cmc.s15231 Abstract: http://www.ncbi.nlm.nih.gov/pubmed/25983558
Nogren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). Eur J Vas Endovasc Surg 2007;33:S1-75 Abstract: http://www.jvascsurg.org/article/S0741-5214(06)02296-8/abstract
M. Lichtenberg, M. Kaeunicke, M. Lukat, B. Hailer, Retrograde rotational thrombectomy with the Rotarex catheter system: treatment option for an acute thrombotic occlusion of a subclavian artery. Vascular Health and Risk Management 2011:7 623-627 Abstract: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3212427/
References:
Слайд 67References:
A. Peer, A. Altshuler, Straub Medical’s Roratex thrombectomy device used as
R. Silingardi et al. Mechanical thrombectomy in proximal subclavian artery in-stent occlusion.Cardiovascular Interv. And Ther 2014;29:140-145 DOI: 10.1007/s12928-013-0199-3. Abstract: http://link.springer.com/article/10.1007/s12928-013-0199-3
C. Wissgott et al. Treatment of Acute Femoropopliteal Bypass Graft Occlusion: Comparison of Mechanical Rotational Thrombectomy with Ultrasound-Enhanced Lysis. Fortschr Röntgenstr 2008; 180:547-552. Abstract: http://europepmc.org/abstract/med/18484516
US Markets for Peripheral Vascular Devices. Millennium Research Group, 2013 2014.2. Tosaka A, Soga Y, Lida O, ET AL. Classification and clinical impact of restenosis after femoropopliteal stenting, J Am Coll Cardiol. 2012,59:16-23 Abstract: http://www.ncbi.nlm.nih.gov/pubmed/22192663
Inoue S, Koyama H, Miyata T, et al. Pathogenetic heterogeneity of in-stent lesion formation in human peripheral arterial disease. Jvasc Surg. 2002;35:672-678 Abstract: http://www.ncbi.nlm.nih.gov/pubmed/11932661
M. Lichtenberg. Treating In-Stent Restenosis. Supplement to Endovascular Today Europe, 2016;12:15. Abstract: http://evtoday.com/2016/05/supplement2/treating-in-stent-restenosis/
L. Garcia, S. Lyden. Atherectomy for Infrainguinal Peripheral Artery Disease. J Endovascular Ther April 2009;105:115. Abstract: http://jet.sagepub.com/content/16/2_suppl/105.abstract
F. Castañeda, et al. Comparison of Three Mechanical Thrombus Removal Devices in Thrombosed Canine Iliac Arteries. RSNA Radiology. DOI: http://dx.doi.org/10.1148/radiology.219.1.r01ap36153
Van Ommen VG, et al. Comparison of arterial wall reaction after passage of the Hydrolyser device versus a thrombectomy balloon in an animal model. J Vasc Interv Radiol. 1996 May-Jun7(3);451-4. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/8761831?dopt=Abstract
N. Shammas, et al. CRT-716 Six-month Revascularization Outcome Of Jetstream Atherectomy in Treating In-Stent Restenosis Of Femoropopliteal Arteries: Results Of the Jetstream- ISR Study. J Am Coll Cardiol Intv. 2015;8(2_S):S3-S3. doi:10.1016/j.jcin.2014.12.015. Abstract: http://interventions.onlinejacc.org/article.aspx?articleid=2118748
Reference: Wissgott C, Kamusella P, Andresen R. Treatment of femoropopliteal stenosis and occlusions with mechanical rotational catheters: comparison of results with the Rotarex and Pathway devices. J Cardiovasc Surg 2012 Apr,53(2):177-86. Abstract: http://www.ncbi.nlm.nih.gov/pubmed/22456640
M. Lichtenberg, et al. Thrombectomy Procedures. UniMed Science ISBN 978-3-8374-1444-8
D. Kuhelj, et al. Percutaneous mechanical thrombectomy of superior mesenteric artery embolism. Radiol Oncol. 2013 Sep; 47(3): 239–243. Abstract: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794879/
Wissgott C, Steinkamp HJ. Acute occlusion of femoripopliteal bypass: comparison of results of rotational thrombectomy catheters and local lysis. RöFo 2005; 177 DOI:10.1055/S-2005-867768 Abstract: https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-2005-867768
T. Heller. Mechanical rotational Thrombectomy in the venous system. SMAG distributor meeting 2015.
M. Lichtenberg. Successful recanalisation of venous thrombotic occlusions with Aspirex mechanical thrombectomy. LINC 2016.
B. Migliara. Mechanical debulking in bypass occlusions, Fast and Effective. Charing Cross 2016.
Vladimir Y. Et al. A retrospective Comparison of Ultrasound-Assisted Catheter Directed Thrombolysis and Catheter-Directed Thrombolysis Alone for Treatment of Proximal DVT. Cardiovasc. Intervent. Radiol (2016) 39:1115-1121. DOI 10.1007/s00270-016-1367-5. Abstract: http://link.springer.com/article/10.1007/s00270-016-1367-5
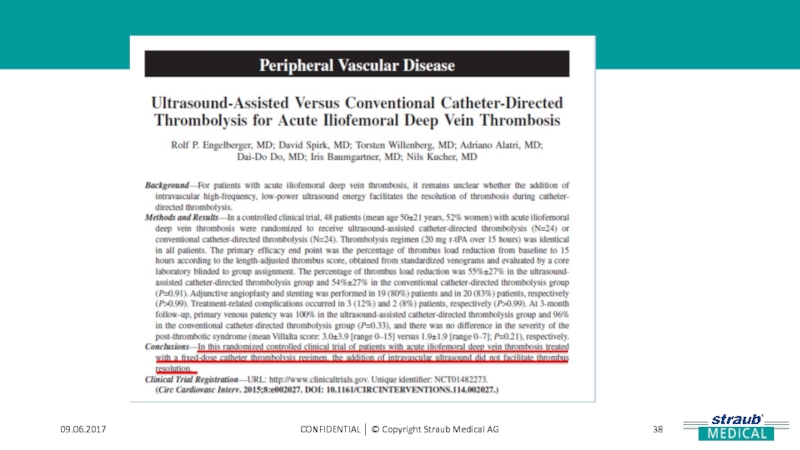
Engelberger RP, et al. Ultrasound-assisted versus conventional catheter-directed thrombolysis for acute iliofemoral DVT. Cris Cardiovascular Interv. 2015;8:1-10, DOI: 10.1161/CIRCINTERVENTIONS.114.002027-00909655-y. Abstract: http://circinterventions.ahajournals.org/content/8/1/e002027.short
Torsten Fuss. LINC 2016. The treatment of the ISR in the femoropopliteal segment.
Wissgott C, Kamusella P, Andresen R. Treatment of chronic occlusions of the iliac of femoropopliteal arteries with mechanical rotational catheters. 183(10); 945-951 http://www.ncbi.nlm.nih.gov/pubmed/21894596
Straub Medical Publication Liste http://www.straubmedical.com/publications_en.html
X
Fogarty Catheter. Complications encountered during arterial embolectomy with the Fogarty balloon catheter. https://www.ncbi.nlm.nih.gov/pubmed/961039