- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Purulent surgical infection презентация
Содержание
- 1. Purulent surgical infection
- 2. Overall manifestations Signs of
- 3. 3. Respiratory disturbances - apnea, tachypnea (respirations
- 4. Hematogenous Osteomyelitis Hematogenous infection begins
- 5. PATHOPHYSIOLOGY Microorganisms enter bone (Phagocytosis).
- 6. PATHOPHYSIOLOGY Bacteria escape host defenses by:
- 7. PATHOLOGY Acute ? Congested or thrombosed vessels
- 8. Stages Toxic (adynamic) stage Septicopyemic stage Local stage
- 9. Forms Acute Osteomyelitis Sub-acute Osteomyelitis Chronic Osteomyelitis
- 10. Symptoms in newborn Clinical of septicemia :
- 11. Symptoms in infant Drowsy Irritable History of
- 12. Symptoms in child Severe pain Malaise Fever
- 13. Outcomes Suppuration: 4-5 days Pus formation
- 14. Necrosis Bone death by the end of
- 16. New bone formation By the end of
- 18. Joint capsule of 4 metaphysis cause of
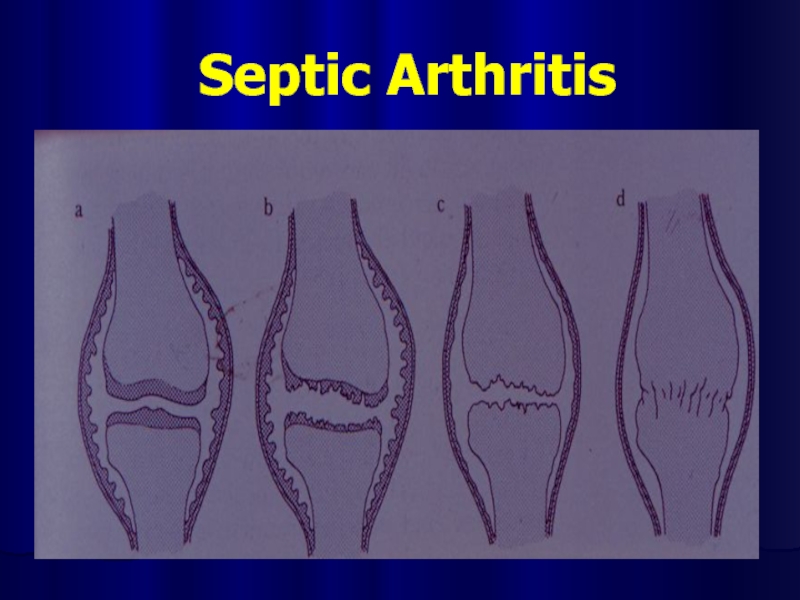
- 20. Septic Arthritis
- 21. Differential diagnosis Toxic synovitis Juvenile rheumatoid arthritis Cellulitis Pyomyositis Psoas abscess
- 22. Investigation Laboratory tests Plain film Ultrasonic diagnosis Aspirate bone liquid CT-scan
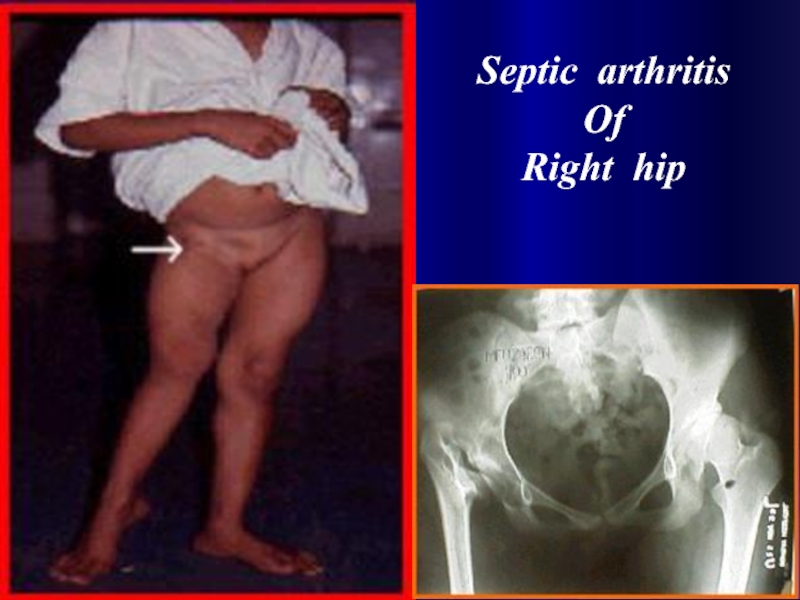
- 26. Septic arthritis Of Right hip
- 27. Investigation : Aspiration confirm diagnosis smear for
- 28. HEMATOGENOUS OSTEOMYELITIS Microbiologic features Staphylococci
- 29. TREATMENT Initial treatment shoud be aggressive.
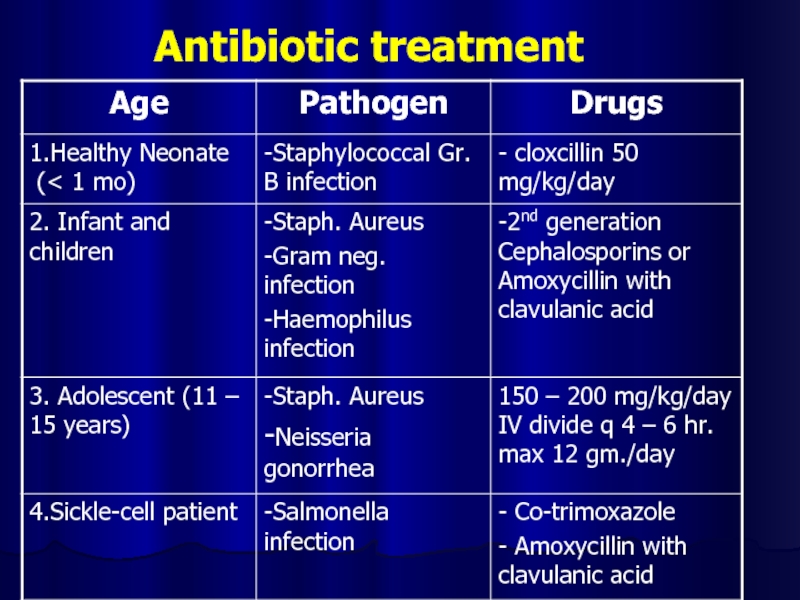
- 30. Antibiotic treatment
- 31. TREATMENT Indication for Surgery Diagnostic Hip joint involvement Neurologic complication Poor Sequestration
- 32. PROGNOSIS Is related to: Causative organisms
- 33. COMPLICATION Bone abscess Bacteremia Fracture Loosing
- 34. Post Osteomyelitis Treatment
- 35. Septic Osteomyelitis Post Osteomyelitis Scar
- 36. Post Osteomyelitis Deformity of the Forearm
- 37. Necrotizing pneumonia Necrotizing pneumonia is characterized
- 38. Pathophysiology The alveoli fill with proteinaceous fluid,
- 39. Physical examination Newborns: rarely cough they more
- 40. Toddlers and preschoolers: most often present with
- 41. Generalized symptoms Intoxication sundrome Nasal flaring Auscultation:
- 42. Extrapulmonary symptoms Abdominal pain or an
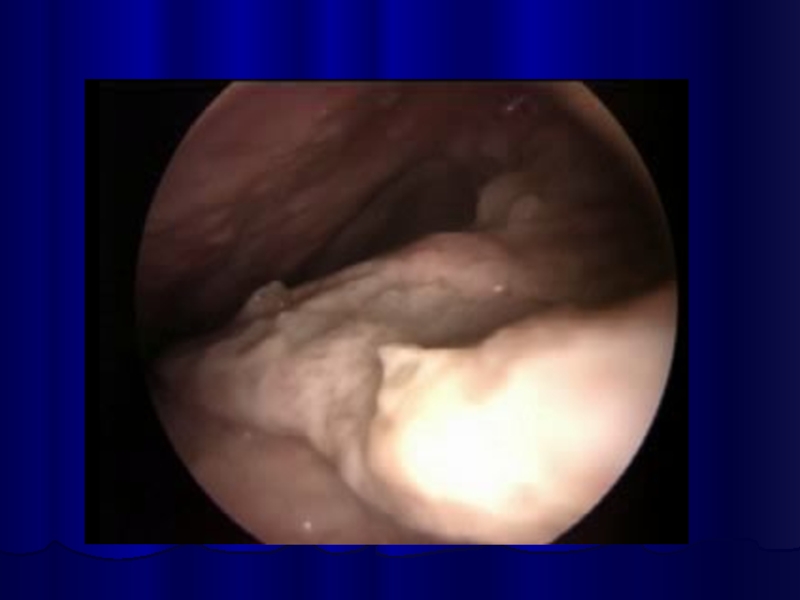
- 43. Diagnosis Laboratory tests (inflammation signs). Radiography Lung
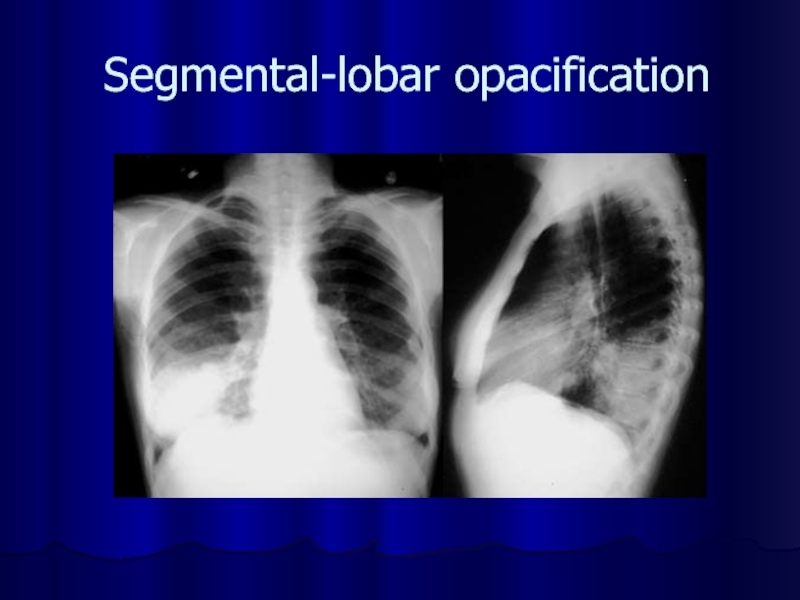
- 45. Segmental-lobar opacification
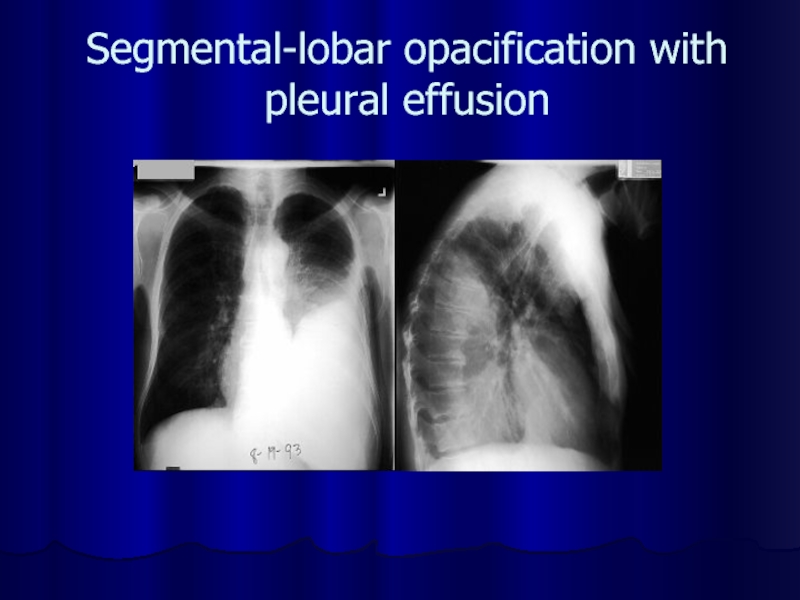
- 46. Segmental-lobar opacification with pleural effusion
- 48. Differential diagnosis Afebrile Pneumonia Syndrome Airway Foreign
- 49. Antibacterial therapy Cephalosporins (III-IV gen.): Ceftriaxone (Rocephin),
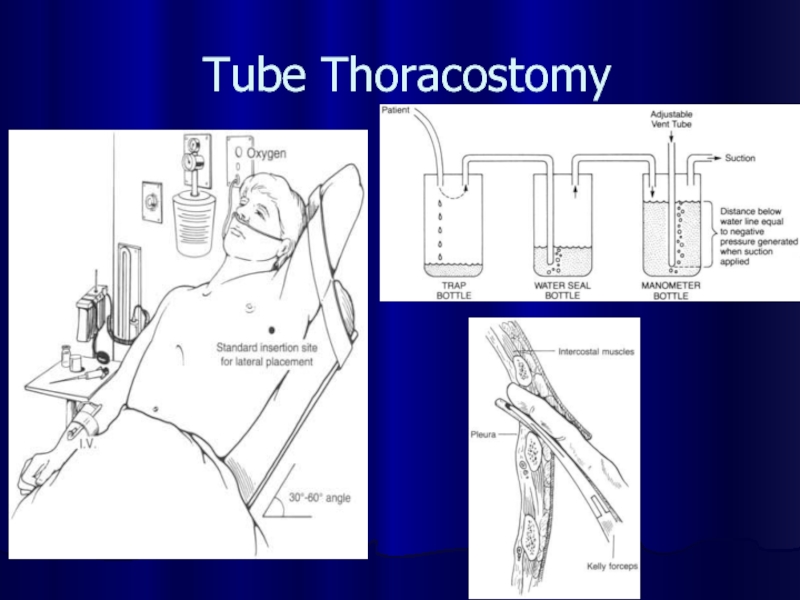
- 50. Tube Thoracostomy
- 53. Necrotic phlegmon Purulent lesions in the
- 55. Causes Vulnerability epidermis A lot of intrecellular liquid Progress vasculature Congenital hypoplasia subjacent tissues
- 56. Clinical stages Intoxication syndrome Hyperaemia Compression soft tissues Edema Fluctuation Exfolation skin
- 57. Differential diagnosis Aseptic necrosis Erythematous erysipelas Idiopathic erysipelas Phlegmonous erysipelas
- 58. Treatment Fluid therapy Antibacterial therapy (cephalosporinis III-
- 61. Omphalitis Omphalitis is an infection
- 62. Associated risk factors include the following: Low birth weight (
- 63. Clinic Purulent or malodorous discharge from the
- 64. Differential diagnosis Umbilical fistula Soaking umbilical Enterocystoma
- 65. Complications Necrotizing fasciitis Myonecrosis Sepsis
- 66. Treatment Fluid therapy Antibacterial therapy (cephalosporinis III-
- 67. Neonatal Sepsis Clinical syndrome of systemic illness
- 68. Early Onset First 5-7 days of life
- 69. Late Onset May occur as early as
- 70. Causative organisms Primary sepsis Group B streptococcus
- 71. Risk factors Prematurity and low birth weight
- 72. Clinical presentation Clinical signs and symptoms are
- 73. Temperature irregularity (high or low) Change in
- 74. Diagnosis Cultures Blood Confirms sepsis 94% grow
- 75. Treatment Antibiotics Primary sepsis: ampicillin and gentamicin
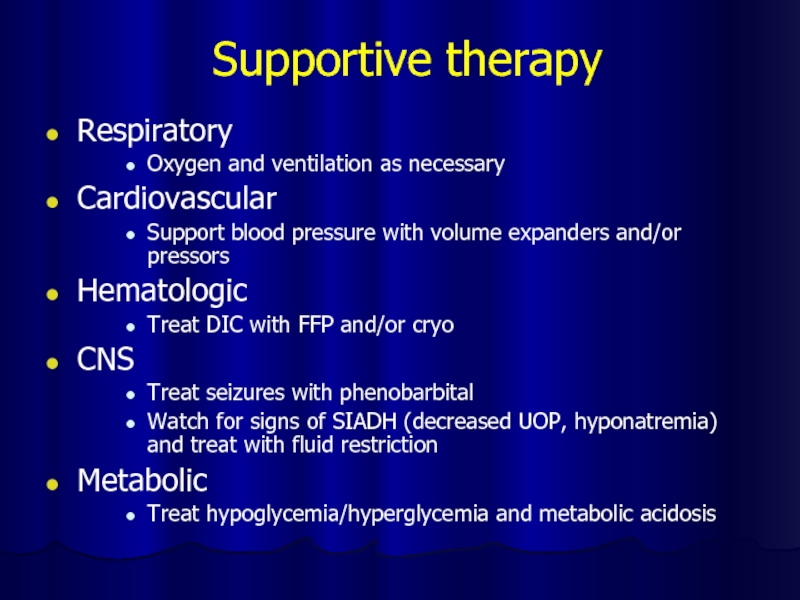
- 76. Supportive therapy Respiratory Oxygen and ventilation as
- 77. Thank you for attention!
Слайд 2Overall manifestations
Signs of sepsis or other systemic disease
are nonspecific and include disturbances of thermoregulation or evidence of dysfunction of multiple organ systems.
1.Disturbances of thermoregulation - fever (temperature >38°C), hypothermia (temperature <36°C), or temperature instability.
2. Cardiovascular disturbances - tachycardia (pulse >180 beats per minute ), hypotension (systolic blood pressure <60 mm Hg in full-term infants), or delayed capillary refill (<2-3 s).
1.Disturbances of thermoregulation - fever (temperature >38°C), hypothermia (temperature <36°C), or temperature instability.
2. Cardiovascular disturbances - tachycardia (pulse >180 beats per minute ), hypotension (systolic blood pressure <60 mm Hg in full-term infants), or delayed capillary refill (<2-3 s).
Слайд 33. Respiratory disturbances - apnea, tachypnea (respirations >60/min), grunting, flaring of
the alae nasi, intercostal or subcostal retractions, or hypoxemia.
4. Gastrointestinal tract disturbances - rigid or distended abdomen or absent bowel sounds.
5. Cutaneous abnormalities - jaundice, petechiae, or cyanosis.
6. Neurologic abnormalities - irritability, lethargy, hypotonia, or hypertonia.
4. Gastrointestinal tract disturbances - rigid or distended abdomen or absent bowel sounds.
5. Cutaneous abnormalities - jaundice, petechiae, or cyanosis.
6. Neurologic abnormalities - irritability, lethargy, hypotonia, or hypertonia.
Слайд 4Hematogenous Osteomyelitis
Hematogenous infection begins in the medullary cavity of
bones, is encased in a rigid structure, which does not allow for the expansion of the inflammatory process. . Progression of the infection restricts medullary blood supply. Passage of pus through the cortex elevates the periosteum and the resulting sub-periosteal abscess causes bony infarction as the cortical bone is supplied by end-arteries from the periosteum.
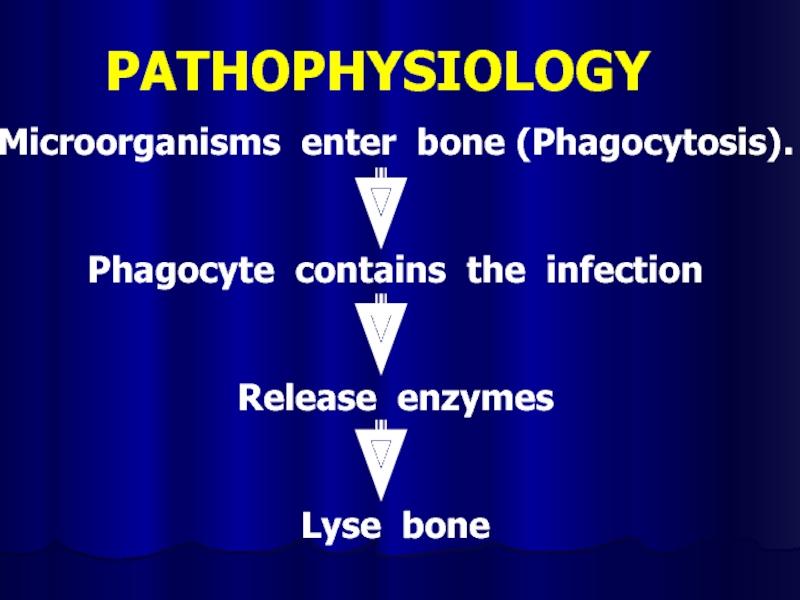
Слайд 5
PATHOPHYSIOLOGY
Microorganisms enter bone (Phagocytosis).
Phagocyte contains the infection
Release enzymes
Lyse bone
Слайд 6
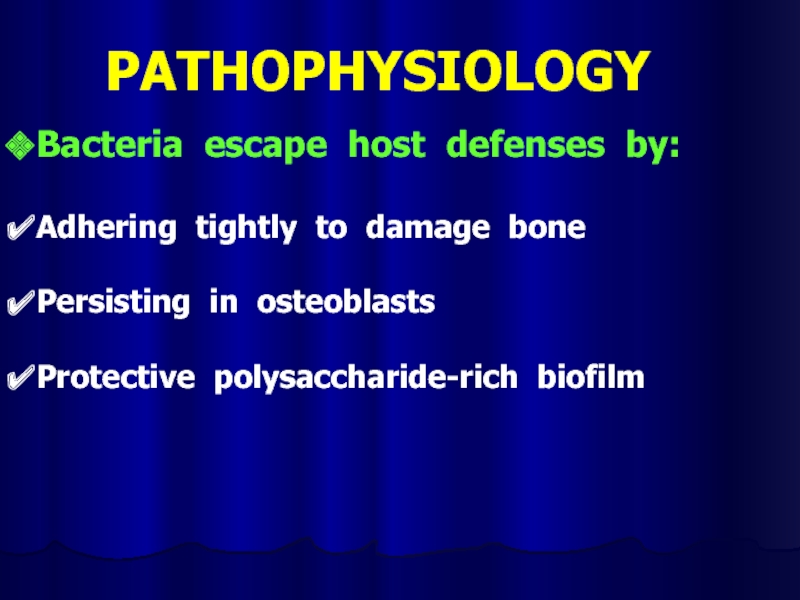
PATHOPHYSIOLOGY
Bacteria escape host defenses by:
Adhering tightly to damage bone
Persisting in osteoblasts
Protective
polysaccharide-rich biofilm
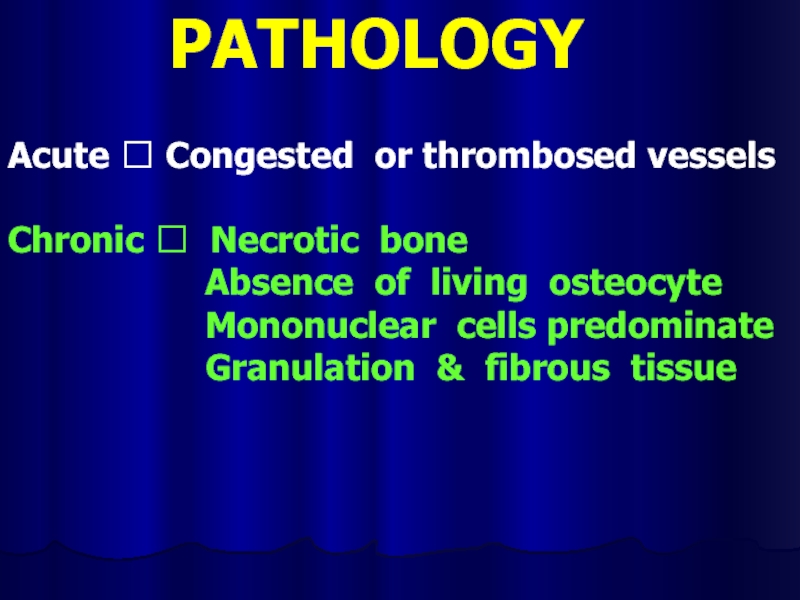
Слайд 7PATHOLOGY
Acute ? Congested or thrombosed vessels
Chronic ? Necrotic bone
Absence of living osteocyte
Mononuclear cells predominate
Granulation & fibrous tissue
Mononuclear cells predominate
Granulation & fibrous tissue
Слайд 10Symptoms in newborn
Clinical of septicemia : fever (36 - 74 %)
irritable, refuses to feed, rapid pulse
Joint swelling
Tenderness and resistance to movement of the joint
Look for umbilical infection
Joint swelling
Tenderness and resistance to movement of the joint
Look for umbilical infection
Слайд 11Symptoms in infant
Drowsy
Irritable
History of birth difficulties
History of umbilical artery catheterization
Metaphyseal tenderness
and resistance to joint movement
Слайд 12Symptoms in child
Severe pain
Malaise
Fever
Toxemia
History of recent infection
Local inflammation
pus escape from bone
Lymphadenopathy
Lymphadenopathy
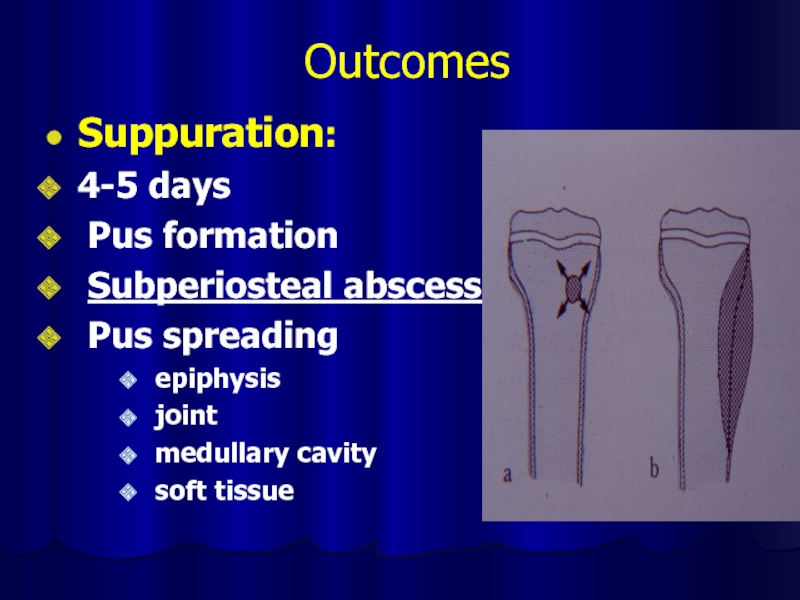
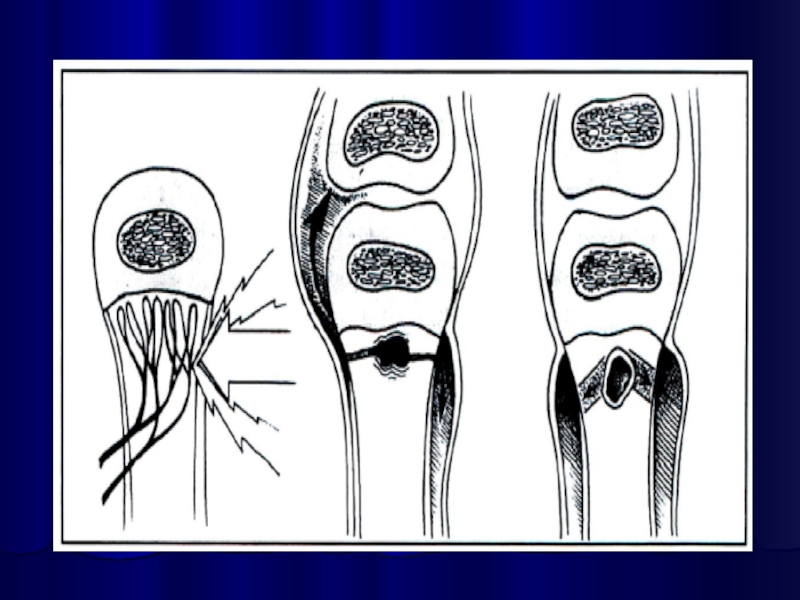
Слайд 13Outcomes
Suppuration:
4-5 days
Pus formation
Subperiosteal abscess
Pus spreading
epiphysis
joint
medullary
cavity
soft tissue
soft tissue
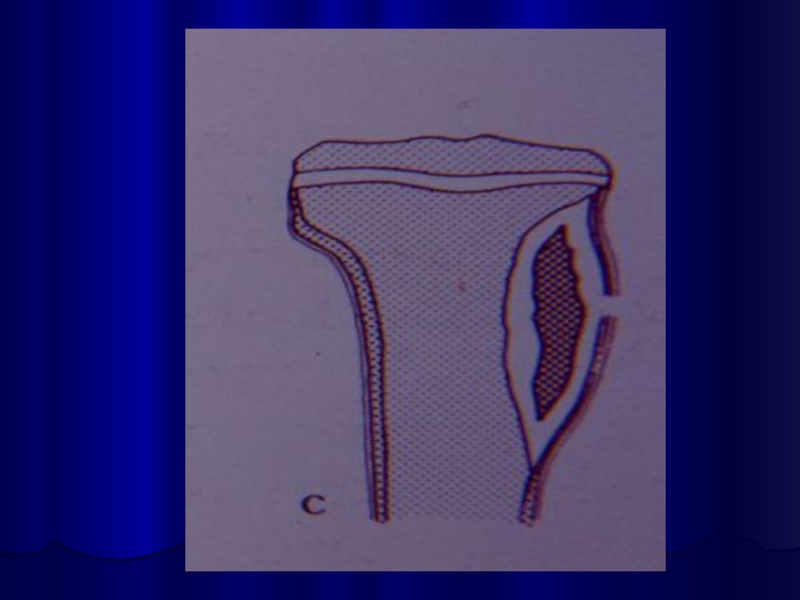
Слайд 14Necrosis
Bone death by the end of a week
Bone destruction ← toxin
← ischemia
Epiphyseal plate injury
Sequestrum formation
small ⭢ removed by macrophage,osteoclast.
large ⭢ remained
Epiphyseal plate injury
Sequestrum formation
small ⭢ removed by macrophage,osteoclast.
large ⭢ remained
Слайд 16New bone formation
By the end of 2nd week
(10 – 14
days)
New bone formation from deep layer of periosteum.
If infection persist- pus discharge through sinus to skin surface ⭢Chronic osteomyelitis
New bone formation from deep layer of periosteum.
If infection persist- pus discharge through sinus to skin surface ⭢Chronic osteomyelitis
Слайд 18Joint capsule of 4 metaphysis cause of osteomyelitis
Femoral head and
neck ( hip )
Humeral head ( shoulder )
lateral side of distal tibia ( ankle joint )
radial head and neck ( elbow joint )
Humeral head ( shoulder )
lateral side of distal tibia ( ankle joint )
radial head and neck ( elbow joint )
Слайд 21Differential diagnosis
Toxic synovitis
Juvenile rheumatoid arthritis
Cellulitis
Pyomyositis
Psoas abscess
Слайд 27Investigation : Aspiration
confirm diagnosis
smear for cell and organism
culture and sensitivity
test
Слайд 28HEMATOGENOUS OSTEOMYELITIS
Microbiologic features
Staphylococci ? Aureus, Epidermidis
Streptococci ? Group A
& B
Haemophilus influenzae
Gram-negative enteric bacilli
Anaerobes
Polymicrobial
Mycobacterial
Fungi
Haemophilus influenzae
Gram-negative enteric bacilli
Anaerobes
Polymicrobial
Mycobacterial
Fungi
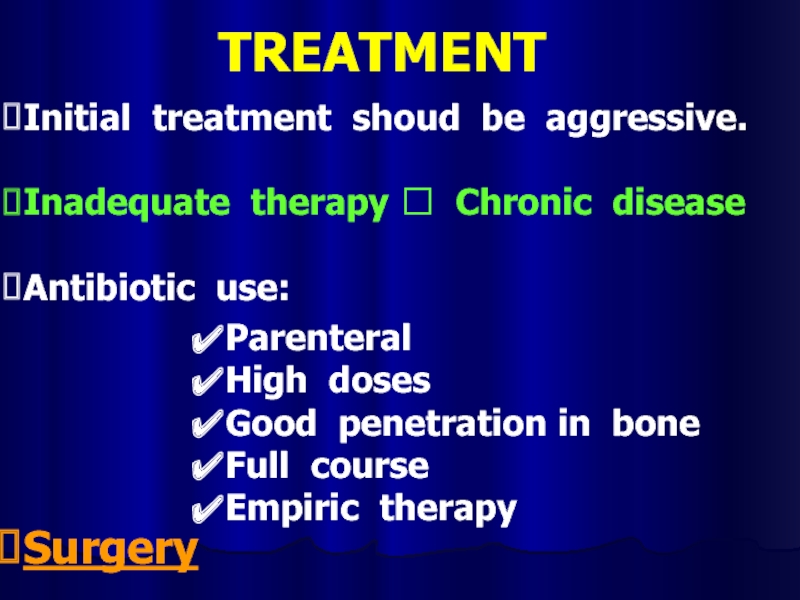
Слайд 29TREATMENT
Initial treatment shoud be aggressive.
Inadequate therapy ? Chronic disease
Antibiotic use:
Surgery
Parenteral
High doses
Good penetration in bone
Full course
Empiric therapy
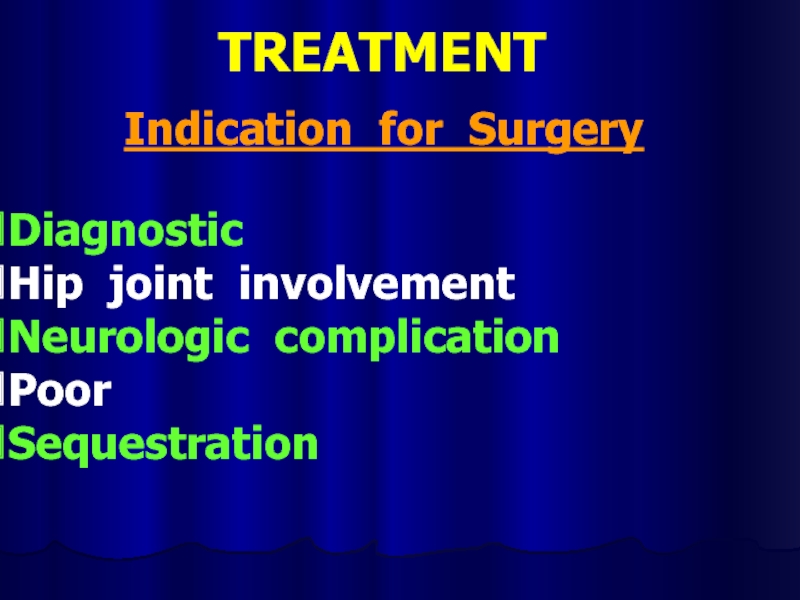
Слайд 31TREATMENT
Indication for Surgery
Diagnostic
Hip joint involvement
Neurologic complication
Poor
Sequestration
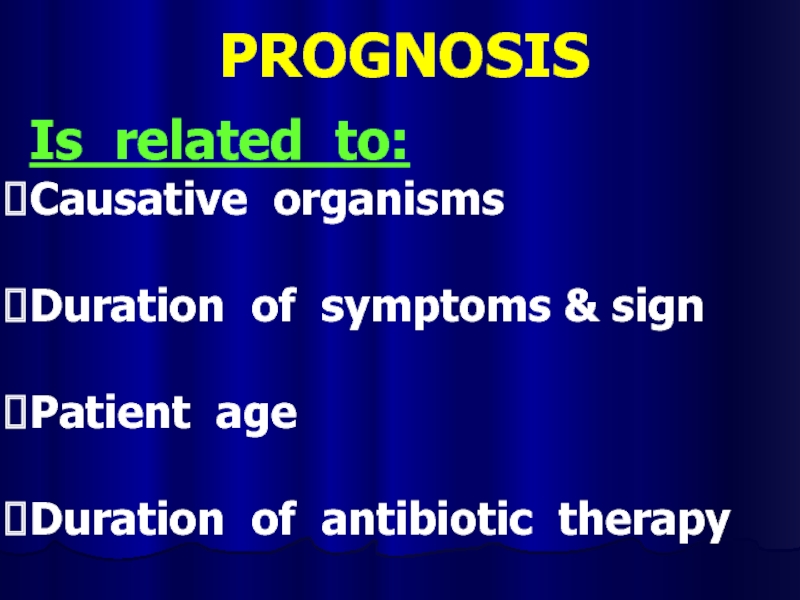
Слайд 32PROGNOSIS
Is related to:
Causative organisms
Duration of symptoms & sign
Patient age
Duration of antibiotic
therapy
Слайд 33COMPLICATION
Bone abscess
Bacteremia
Fracture
Loosing of the prosthetic implant
Overlying soft-tissue cellulitis
Draining soft-tissue tract
Слайд 37Necrotizing pneumonia
Necrotizing pneumonia is characterized by inflammation of the alveoli
and terminal airspaces in response to invasion by an infectious agent introduced into the lungs through hematogenous spread or inhalation.
Слайд 38Pathophysiology
The alveoli fill with proteinaceous fluid, which triggers a brisk influx
and polymorphonuclear cells followed by the deposition of fibrin and the degradation of inflammatory cells.
Intra-alveolar debris is ingested and removed by the alveolar macrophages.
This consolidation leads to decreased air entry and dullness to percussion.
Inflammation in the small airways leads to crackles.
The patient must increase his or her respiratory rate to maintain adequate ventilation.
Intra-alveolar debris is ingested and removed by the alveolar macrophages.
This consolidation leads to decreased air entry and dullness to percussion.
Inflammation in the small airways leads to crackles.
The patient must increase his or her respiratory rate to maintain adequate ventilation.
Слайд 39Physical examination
Newborns:
rarely cough
they more commonly present with tachypnea, retractions, grunting, and
hypoxemia
grunting suggests a lower respiratory tract disease
Older infants:
grunting may be less common
tachypnea, retractions, and hypoxemia are common
may be accompanied by a persistent cough, congestion, fever, irritability, and decreased feeding
grunting suggests a lower respiratory tract disease
Older infants:
grunting may be less common
tachypnea, retractions, and hypoxemia are common
may be accompanied by a persistent cough, congestion, fever, irritability, and decreased feeding
Слайд 40Toddlers and preschoolers:
most often present with fever, cough (productive or nonproductive),
tachypnea, and congestion
sometimes emesis
Older children and adolescents:
1. This group may also present with fever, cough (productive or nonproductive), congestion, chest pain, dehydration, and lethargy.
sometimes emesis
Older children and adolescents:
1. This group may also present with fever, cough (productive or nonproductive), congestion, chest pain, dehydration, and lethargy.
Слайд 41Generalized symptoms
Intoxication sundrome
Nasal flaring
Auscultation: dry or bubbling rales, wheezing, diminished breath
sounds, tubular breath sounds, pleural friction rub.
The affected lung field may be dull to percussion.
Decreased tactile and vocal fremitus.
The affected lung field may be dull to percussion.
Decreased tactile and vocal fremitus.
Слайд 42Extrapulmonary symptoms
Abdominal pain or an ileus accompanied by emesis in
patients with lower lobe pneumonia.
Nuchal rigidity in patients with right upper lobe pneumonia.
Rub caused by pericardial effusion in patients with lower lobe pneumonia due to Haemophilus influenzae infection.
Nuchal rigidity in patients with right upper lobe pneumonia.
Rub caused by pericardial effusion in patients with lower lobe pneumonia due to Haemophilus influenzae infection.
Слайд 43Diagnosis
Laboratory tests (inflammation signs).
Radiography
Lung aspirate
Sputum culture
Blood culture
Polymerase chain reaction
Skin tests (TB
pneumonia BCG)
Bronchoscopy
CT - scan
Bronchoscopy
CT - scan
Слайд 48Differential diagnosis
Afebrile Pneumonia Syndrome
Airway Foreign Body
Aspiration Syndromes
Bronchiectasis
Bronchiolitis
Bronchitis, Acute and Chronic
Chronic
Granulomatous Disease
Congenital Pneumonia
Cystic Adenomatoid Malformation
Cystic Fibrosis
Empyema
Gastroesophageal Reflux
Pulmonary Sequestration
Congenital Pneumonia
Cystic Adenomatoid Malformation
Cystic Fibrosis
Empyema
Gastroesophageal Reflux
Pulmonary Sequestration
Слайд 49Antibacterial therapy
Cephalosporins (III-IV gen.): Ceftriaxone (Rocephin), Cefotaxime (Claforan), Cefuroxime (Zinacef, Ceftin,
Kefurox).
Macrolide antibiotics: Azithromycin (Zithromax), Clarithromycin (Biaxin), Erythromycin (E.E.S., E-Mycin, Ery-Tab),
Macrolide antibiotics: Azithromycin (Zithromax), Clarithromycin (Biaxin), Erythromycin (E.E.S., E-Mycin, Ery-Tab),
Слайд 53Necrotic phlegmon
Purulent lesions in the skin and hypodermic
tissue,
usually this process localisations in the scapular and sacrcococcygeal regions.
Necrotic phlegmon is predominantly a disease of the neonate.
Necrotic phlegmon is predominantly a disease of the neonate.
Слайд 55Causes
Vulnerability epidermis
A lot of intrecellular liquid
Progress vasculature
Congenital hypoplasia subjacent tissues
Слайд 56Clinical stages
Intoxication syndrome
Hyperaemia
Compression soft tissues
Edema
Fluctuation
Exfolation skin
Слайд 57Differential diagnosis
Aseptic necrosis
Erythematous erysipelas
Idiopathic erysipelas
Phlegmonous erysipelas
Слайд 58Treatment
Fluid therapy
Antibacterial therapy (cephalosporinis III- IV gen.)
General health-improving therapy
Surgical treatment –
chess incisions in the lesion region, irrigation aspiration.
Слайд 61Omphalitis
Omphalitis is an infection of the umbilical stump. Omphalitis
typically presents as a superficial cellulitis that may spread to involve the entire abdominal wall and may progress to necrotizing fasciitis, myonecrosis, or systemic disease. Aerobic bacteria are present in approximately 85% of infections, predominated by Staphylococcus aureus, group A Streptococcus, Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis
Слайд 62 Associated risk factors include the following:
Low birth weight (
Prior umbilical catheterization
Septic delivery
Prolonged rupture of membranes
Immunologic disorder
Слайд 63Clinic
Purulent or malodorous discharge from the umbilical stump
Periumbilical erythema
Edema
Tenderness
Ecchymoses
Progression of cellulitis despite antimicrobial therapy
Слайд 65Complications
Necrotizing fasciitis
Myonecrosis
Sepsis
Septic embolization
Particularly endocarditis and liver abscess formation
Abdominal
complications
Слайд 66Treatment
Fluid therapy
Antibacterial therapy (cephalosporinis III- IV gen.)
Surgical care: management of necrotizing
fasciitis and myonecrosis involves early and complete surgical debridement of the affected tissue and muscle
Слайд 67Neonatal Sepsis
Clinical syndrome of systemic illness accompanied by bacteremia occurring in
the first month of life
Incidence
1-8/1000 live births
13-27/1000 live births for infants < 1500g
Mortality rate is 13-25%
Higher rates in premature infants and those with early fulminant disease
Incidence
1-8/1000 live births
13-27/1000 live births for infants < 1500g
Mortality rate is 13-25%
Higher rates in premature infants and those with early fulminant disease
Слайд 68Early Onset
First 5-7 days of life
Usually multisystem fulminant illness with
prominent respiratory symptoms (probably due to aspiration of infected amniotic fluid)
High mortality rate
5-20%
Typically acquired during intrapartum period from maternal genital tract
Associated with maternal chorioamnionitis
High mortality rate
5-20%
Typically acquired during intrapartum period from maternal genital tract
Associated with maternal chorioamnionitis
Слайд 69Late Onset
May occur as early as 5 days but is most
common after the first week of life
Less association with obstetric complications
Usually have an identifiable focus
Most often meningitis or sepsis
Acquired from maternal genital tract or human contact
Less association with obstetric complications
Usually have an identifiable focus
Most often meningitis or sepsis
Acquired from maternal genital tract or human contact
Слайд 70Causative organisms
Primary sepsis
Group B streptococcus
Gram-negative enterics (esp. E. coli)
Listeria monocytogenes, Staphylococcus,
other streptococci (entercocci), anaerobes, H. flu
Nosocomial sepsis
Varies by nursery
Staphylococcus epidermidis, Pseudomonas, Klebsiella, Serratia, Proteus, and yeast are most common
Nosocomial sepsis
Varies by nursery
Staphylococcus epidermidis, Pseudomonas, Klebsiella, Serratia, Proteus, and yeast are most common
Слайд 71Risk factors
Prematurity and low birth weight
Premature and prolonged rupture of membranes
Maternal
peripartum fever
Amniotic fluid problems (i.e. mec, chorio)
Resuscitation at birth, fetal distress
Multiple gestation
Invasive procedures
Galactosemia
Other factors: sex, race, variations in immune function, hand washing in the NICU
Amniotic fluid problems (i.e. mec, chorio)
Resuscitation at birth, fetal distress
Multiple gestation
Invasive procedures
Galactosemia
Other factors: sex, race, variations in immune function, hand washing in the NICU
Слайд 72Clinical presentation
Clinical signs and symptoms are nonspecific
Differential diagnosis
RDS
Metabolic disease
Hematologic disease
CNS disease
Cardiac
disease
Other infectious processes (i.e. TORCH)
Other infectious processes (i.e. TORCH)
Слайд 73Temperature irregularity (high or low)
Change in behavior
Lethargy, irritability, changes in tone
Skin
changes
Poor perfusion, mottling, cyanosis, pallor, petechiae, rashes, jaundice
Feeding problems
Intolerance, vomiting, diarrhea, abdominal distension
Cardiopulmonary
Tachypnea, grunting, flaring, retractions, apnea, tachycardia, hypotension
Metabolic
Hypo or hyperglycemia, metabolic acidosis
Poor perfusion, mottling, cyanosis, pallor, petechiae, rashes, jaundice
Feeding problems
Intolerance, vomiting, diarrhea, abdominal distension
Cardiopulmonary
Tachypnea, grunting, flaring, retractions, apnea, tachycardia, hypotension
Metabolic
Hypo or hyperglycemia, metabolic acidosis
Слайд 74Diagnosis
Cultures
Blood
Confirms sepsis
94% grow by 48 hours of age
Urine
Don’t need in infants
<24 hours old because UTIs are exceedingly rare in this age group
CSF
Controversial
May be useful in clinically ill newborns or those with positive blood cultures
CSF
Controversial
May be useful in clinically ill newborns or those with positive blood cultures
Слайд 75Treatment
Antibiotics
Primary sepsis: ampicillin and gentamicin
Nosocomial sepsis: vancomycin and gentamicin or cefotaxime
Change
based on culture sensitivities
Don’t forget to check levels
Don’t forget to check levels
Слайд 76Supportive therapy
Respiratory
Oxygen and ventilation as necessary
Cardiovascular
Support blood pressure with volume expanders
and/or pressors
Hematologic
Treat DIC with FFP and/or cryo
CNS
Treat seizures with phenobarbital
Watch for signs of SIADH (decreased UOP, hyponatremia) and treat with fluid restriction
Metabolic
Treat hypoglycemia/hyperglycemia and metabolic acidosis
Hematologic
Treat DIC with FFP and/or cryo
CNS
Treat seizures with phenobarbital
Watch for signs of SIADH (decreased UOP, hyponatremia) and treat with fluid restriction
Metabolic
Treat hypoglycemia/hyperglycemia and metabolic acidosis