- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
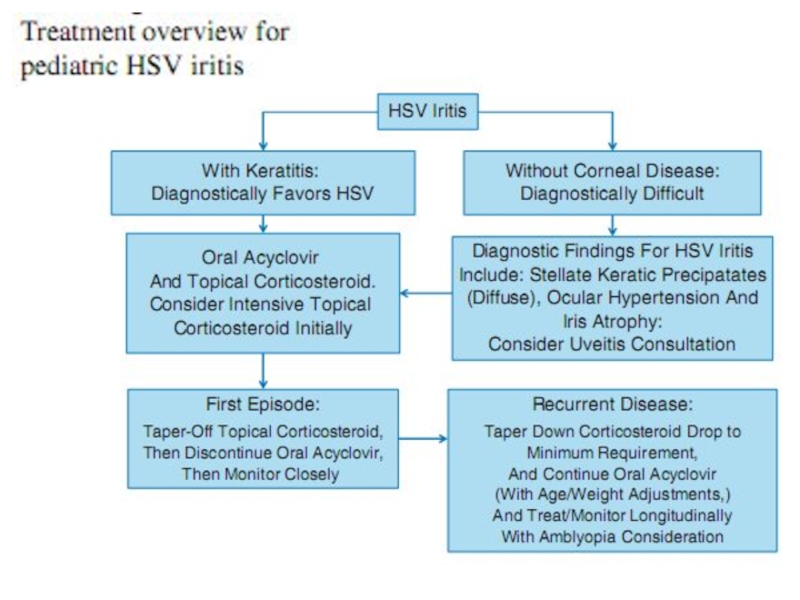
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Pediatric HSV Epithelial Keratitis презентация
Содержание
- 1. Pediatric HSV Epithelial Keratitis
- 3. Herpes simplex virus (HSV) keratitis is an
- 4. HSV keratitis occurs when the infection reaches
- 5. Recurrent ocular HSV-1 infection and inflammation eventually
- 6. HSV keratitis in children may differ from
- 8. HERPES SIMPLEX VIRUS PRIMARY HSV
- 10. RECURRENT HSV INFECTIONS Multiple factors are thought
- 11. Sunlight, local physical trauma, hormonal changes, and
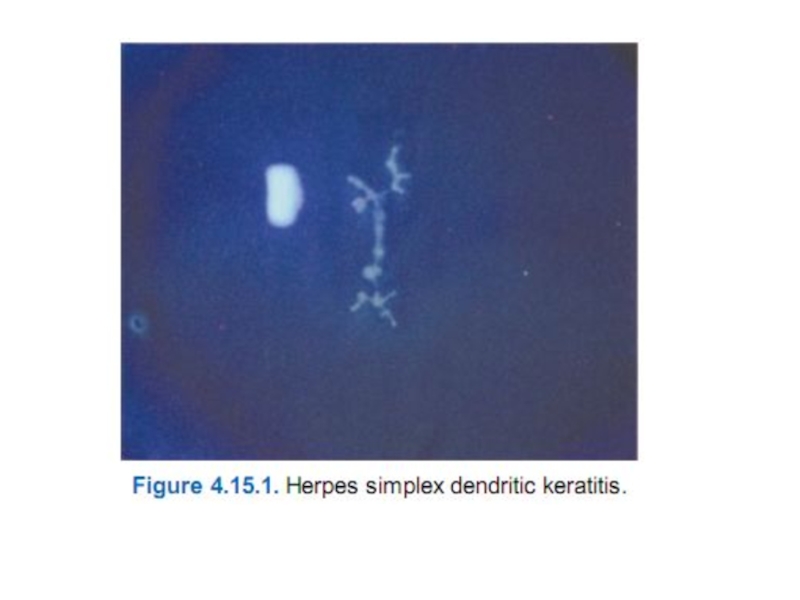
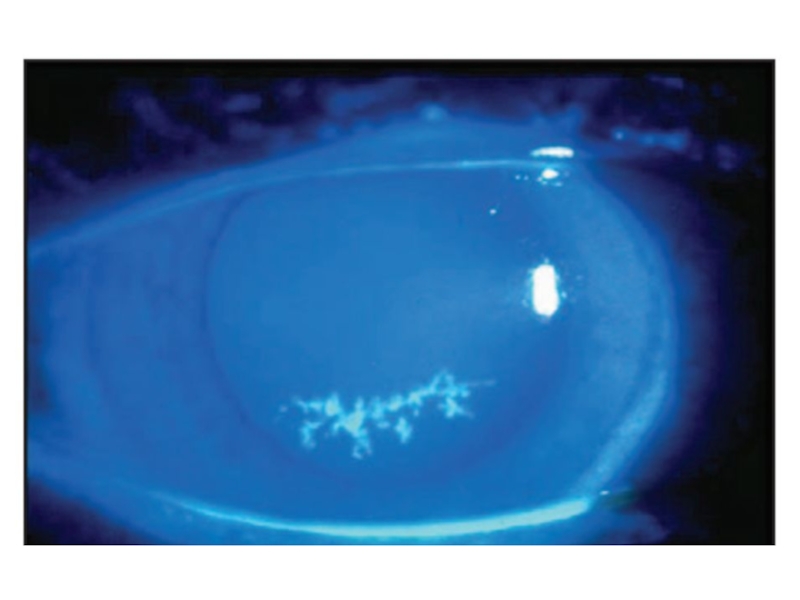
- 12. Epithelial ulcers may cause sensitivity to
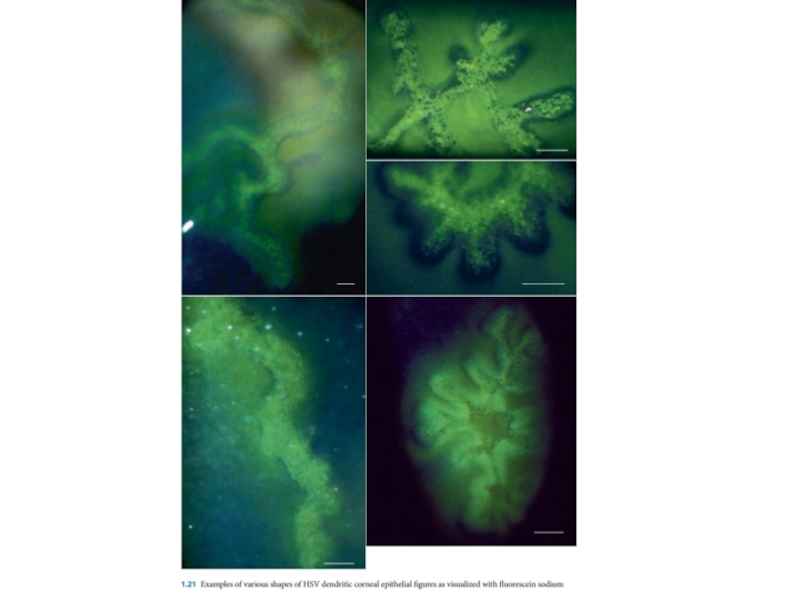
- 18. Fig. 1.17 (c) Afer a blink, the
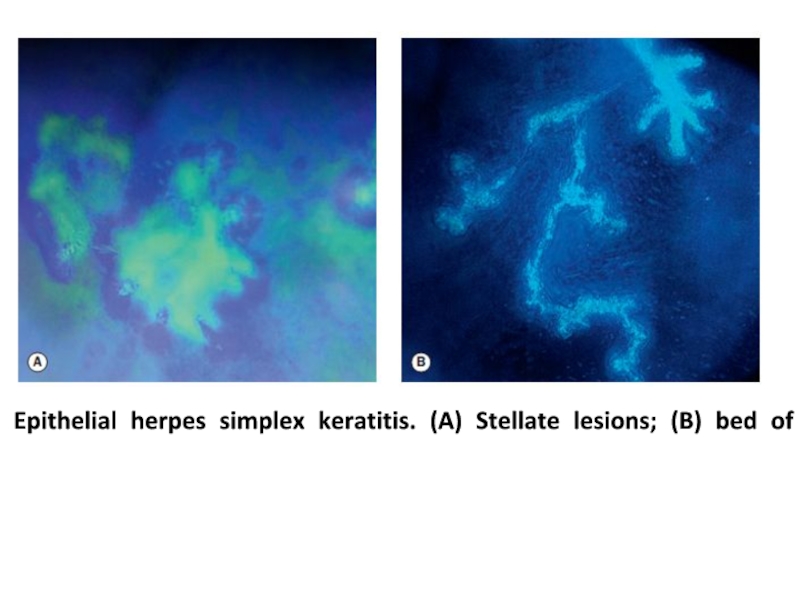
- 20. Epithelial herpes simplex keratitis. (A) Stellate lesions; (B) bed of a dendritic ulcer stained with fuorescein;
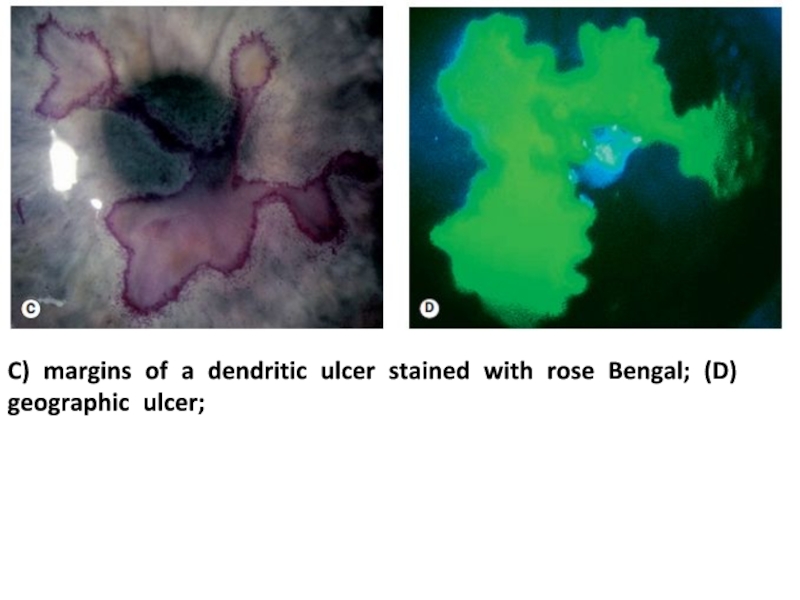
- 21. C) margins of a dendritic ulcer stained with rose Bengal; (D) geographic ulcer;
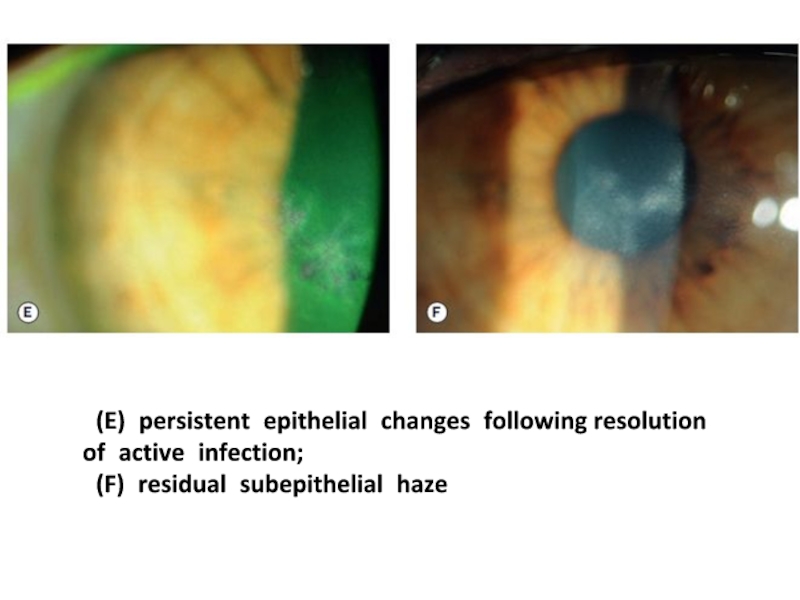
- 22. (E) persistent epithelial changes following resolution of active infection; (F) residual subepithelial haze
- 28. In particular, HSV culture and
- 29. A 5-year-old patient with a history of
- 30. She returned 12 months later with worsening
- 31. Although HSV epithelial disease may resolve
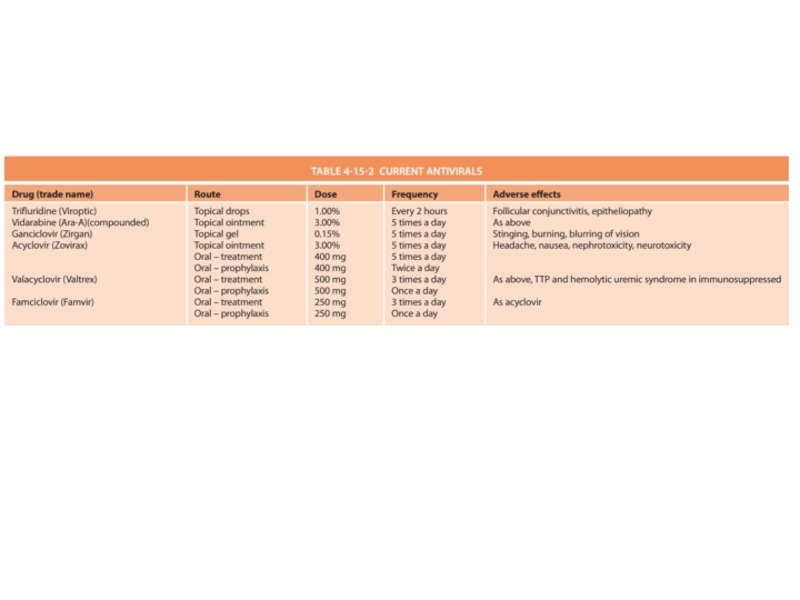
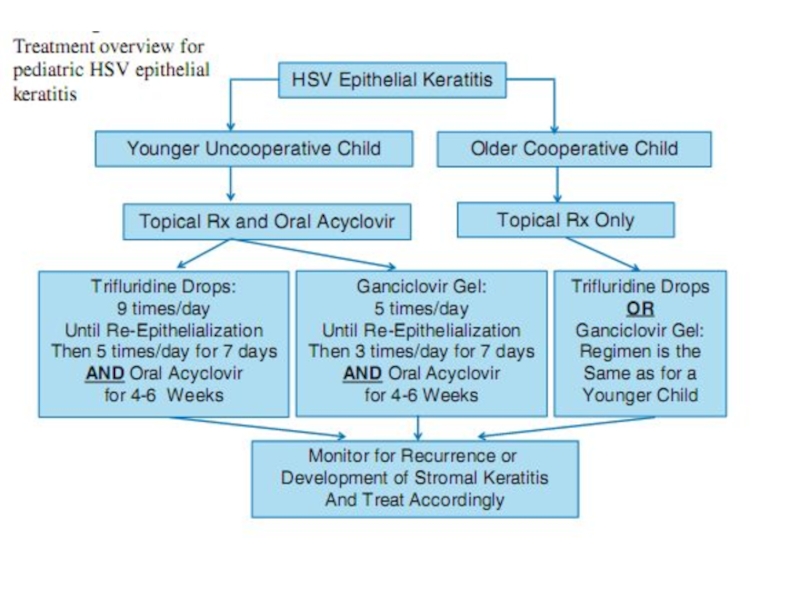
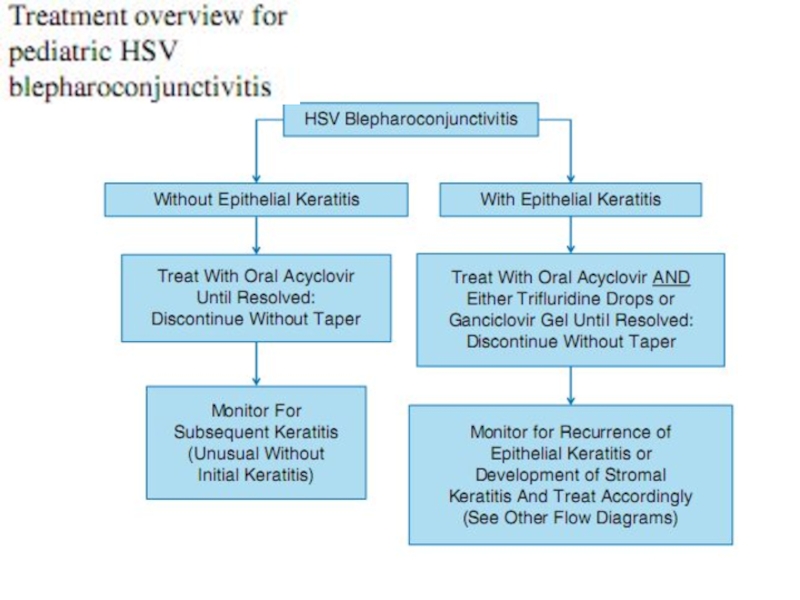
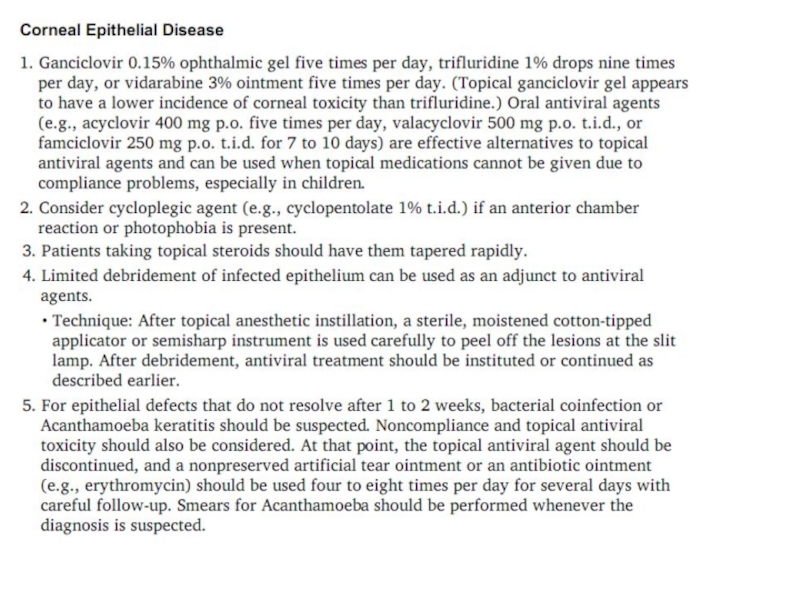
- 33. For infectious HSV epithelial keratitis, topical or
- 35. Oral acyclovir did not hasten healing
- 36. Topical corticosteroids are not indicated for
- 37. Unfortunately, as described in the introduction,
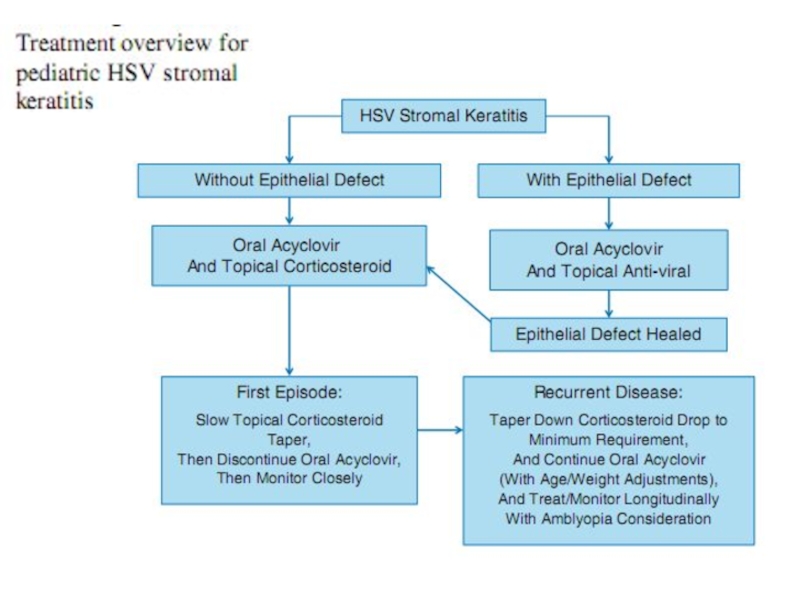
- 41. HSV stromal keratitis classically involves an
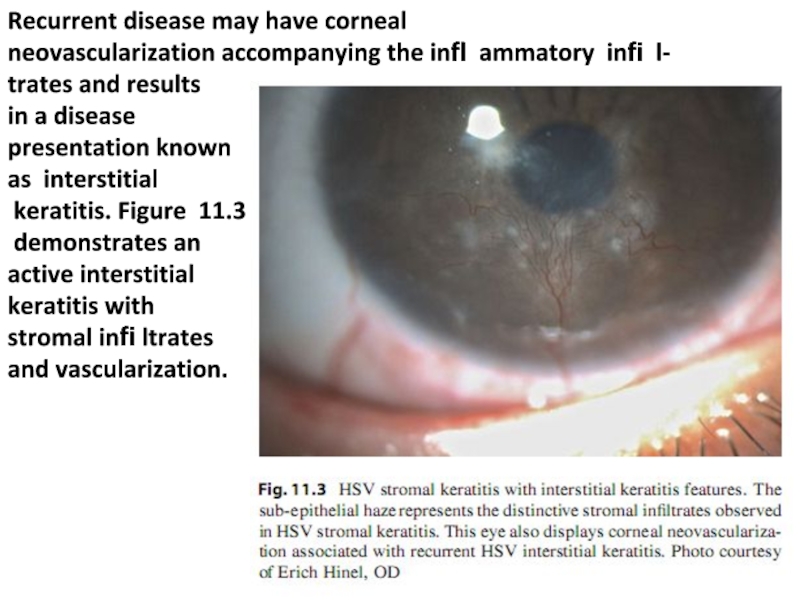
- 42. Recurrent disease may have corneal neovascularization
- 43. Treatment of stromal keratitis in children
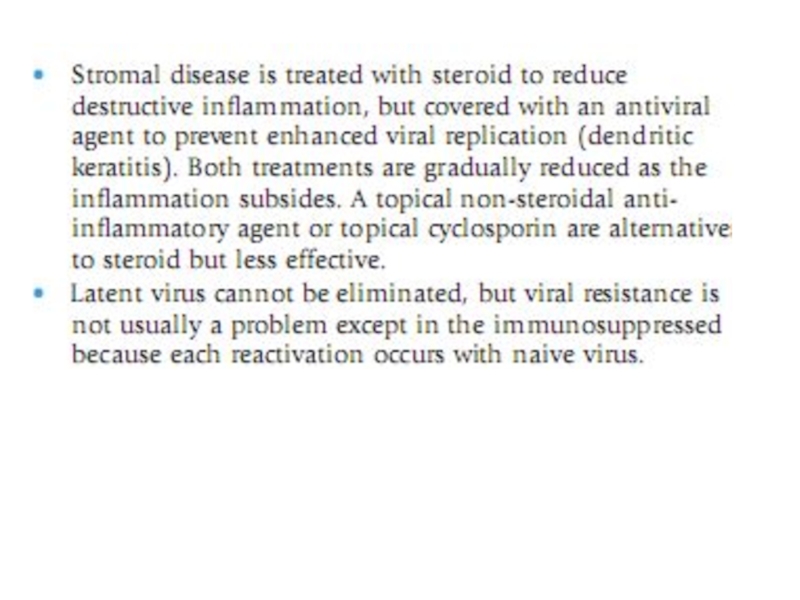
- 44. The topical corticosteroid may be tapered and
- 45. Valacyclovir may be considered for older
- 46. Epithelial keratitis later followed by stromal keratitis
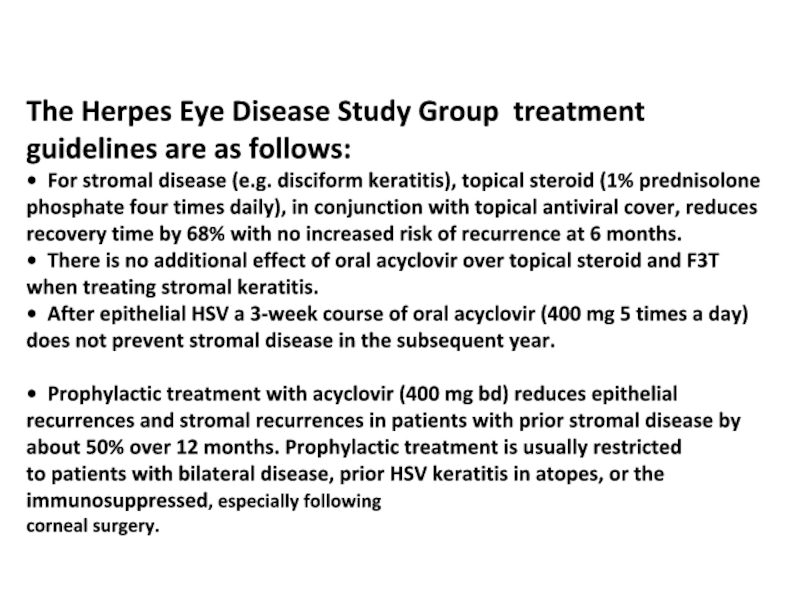
- 49. The Herpes Eye Disease Study Group treatment
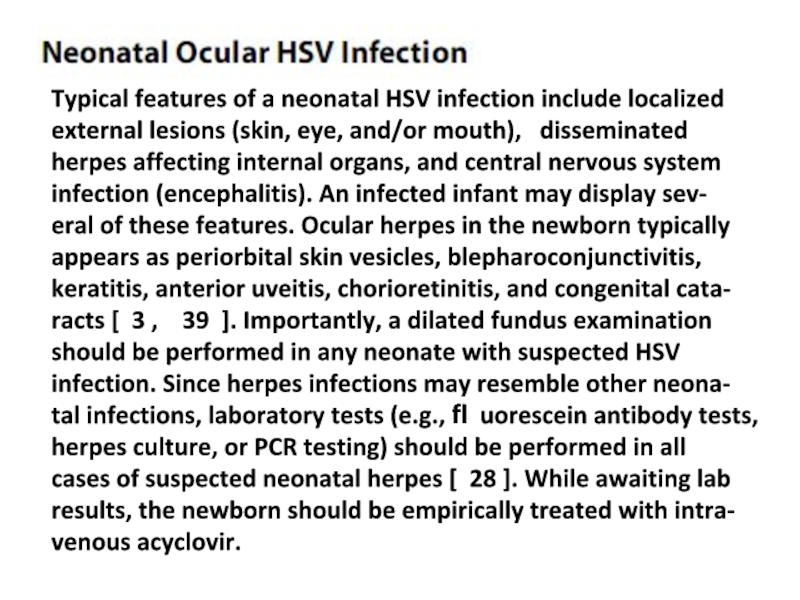
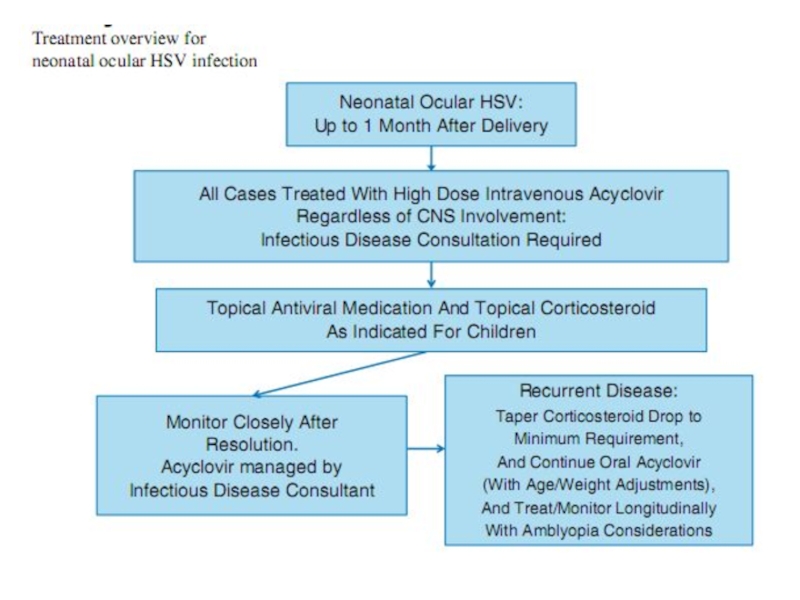
- 51. Typical features of a neonatal HSV infection
- 52. Overall prognosis of neonatal ocular HSV
Слайд 3Herpes simplex virus (HSV) keratitis is an important cause of ocular
Слайд 4HSV keratitis occurs when the infection reaches the corneal epithelium and
Слайд 5Recurrent ocular HSV-1 infection and inflammation eventually cause corneal scarring, thinning,
Слайд 6HSV keratitis in children may differ from that in adults. The
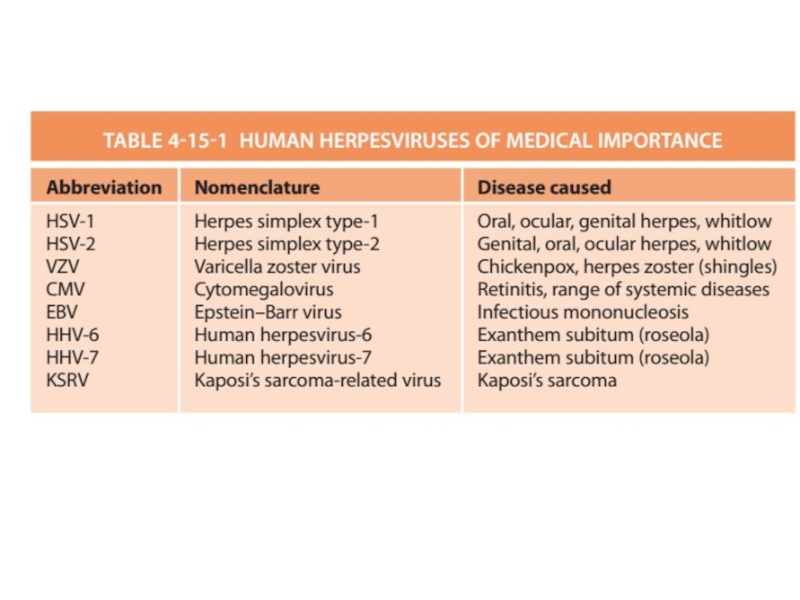
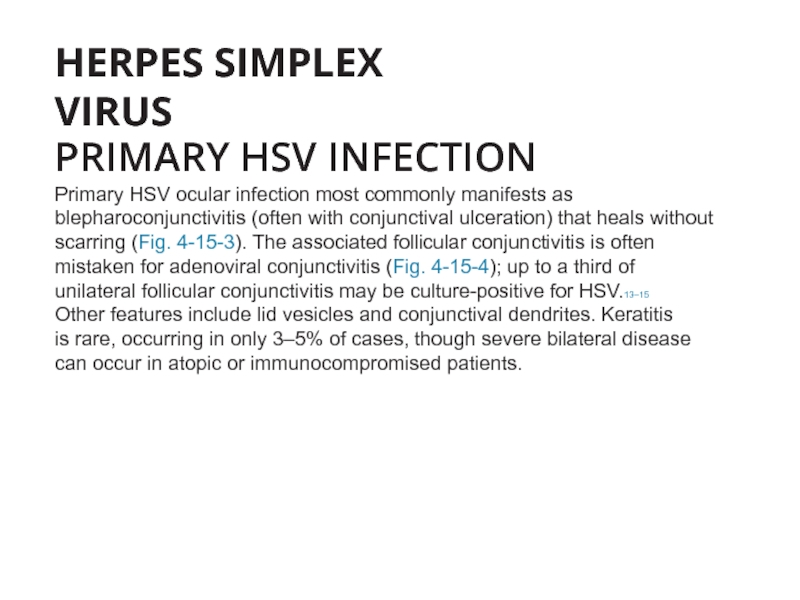
Слайд 8HERPES SIMPLEX VIRUS
PRIMARY HSV INFECTION
Primary HSV ocular infection most commonly
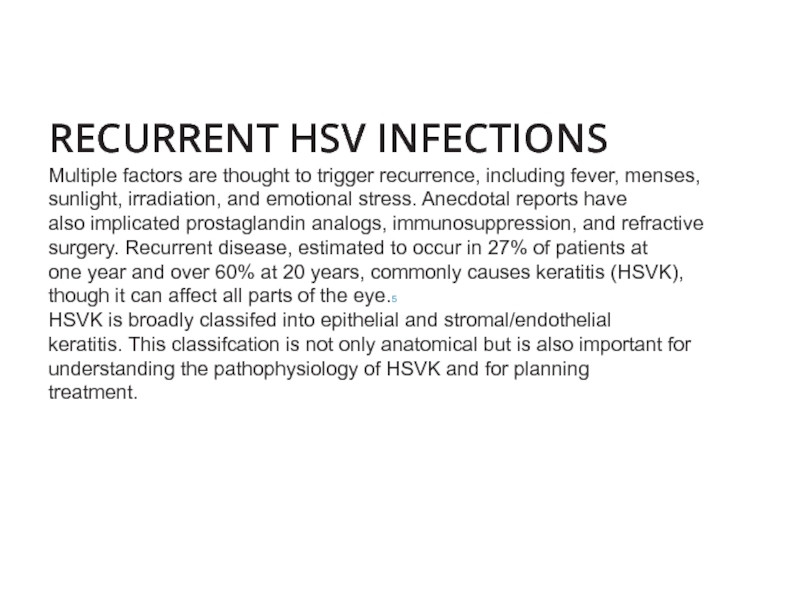
Слайд 10RECURRENT HSV INFECTIONS Multiple factors are thought to trigger recurrence, including fever,
Слайд 11Sunlight, local physical trauma, hormonal changes, and
immunological stress (as by
to risk of recurrence of non-ocular herpetic disease [ 9 ].
However, with correction for recall bias, the Herpetic Eye
Disease Study (HEDS) Group found that none of these fac-
tors were a signifi cant cause of recurrent ocular herpes [ 10 ].
However, a history of atopic disease has been associated
with recurrent herpetic eye disease, possibly secondary to
immunologic dysfunction [ 11 – 13 ]. Therefore, the practitio-
ner should inquire about personal and family history of con-
ditions such as asthma, eczema, and seasonal allergies.
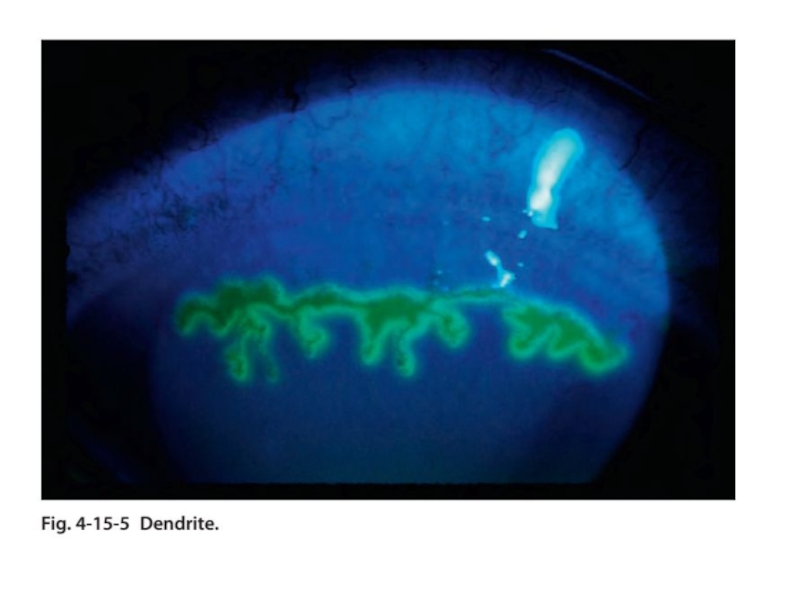
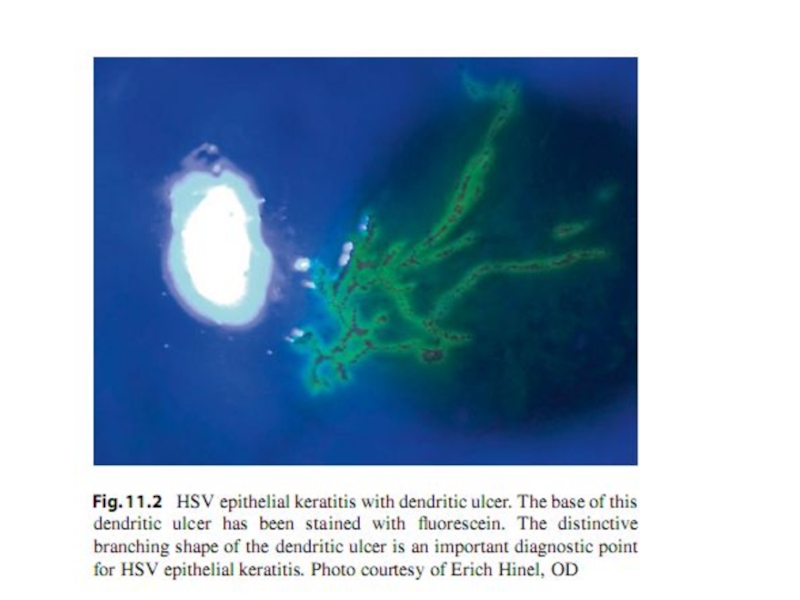
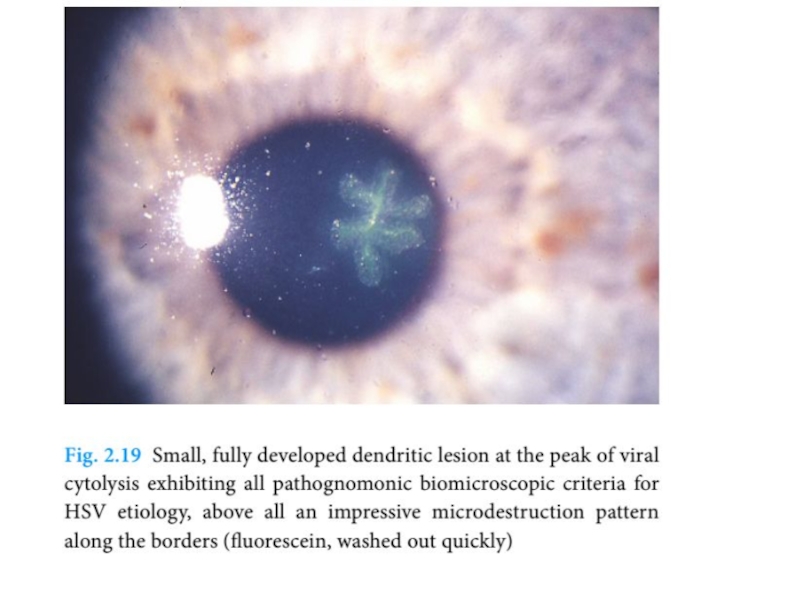
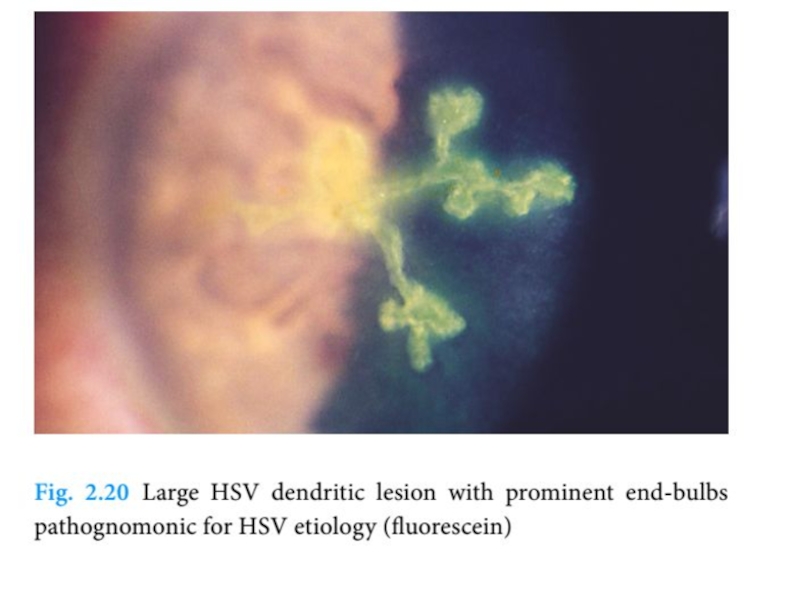
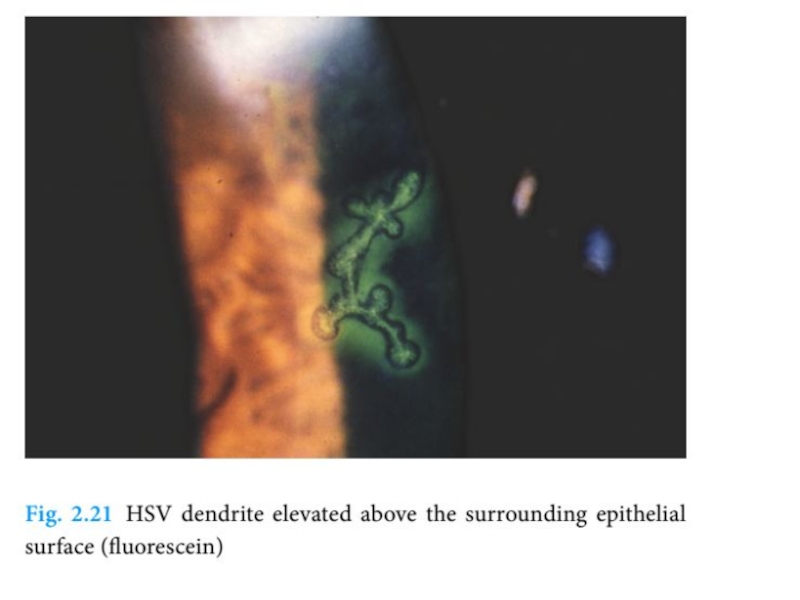
Слайд 12 Epithelial ulcers may cause sensitivity to light,
blurriness, or a
Diagnosis of HSV epithelial keratitis is typically based on
clinical fi ndings. Figure 11.2 shows a typical HSV dendrite.
The distinctive appearance and staining pattern of these
ulcers are important diagnostic points.
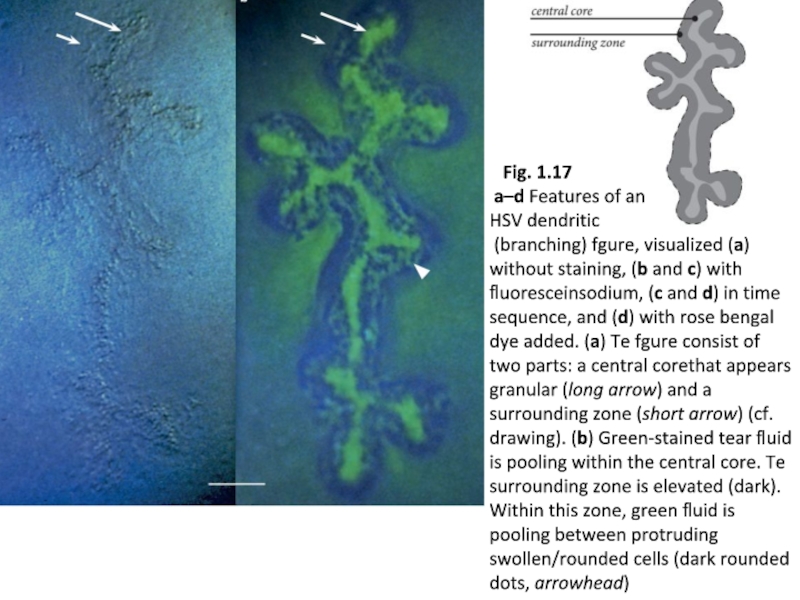
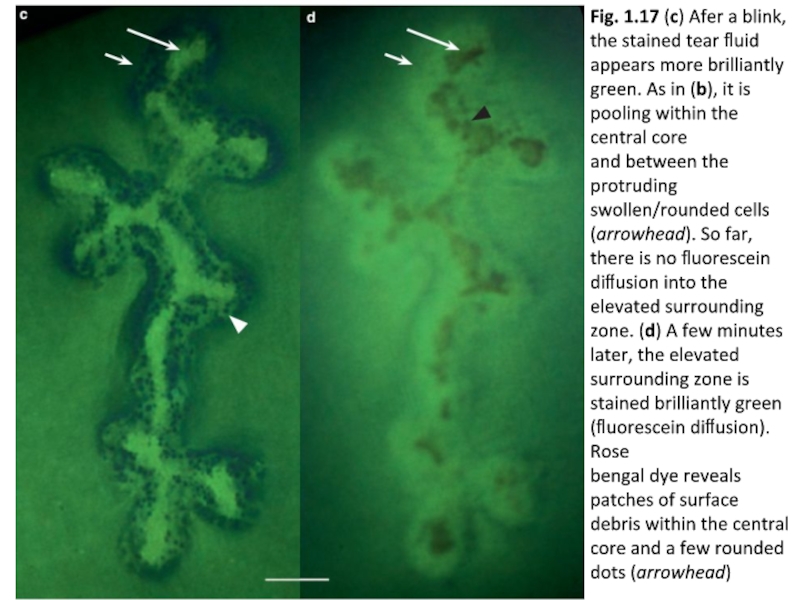
Слайд 17
Слайд 18Fig. 1.17 (c) Afer a blink, the stained tear fluid appears
Слайд 20 Epithelial herpes simplex keratitis. (A) Stellate lesions; (B) bed of a dendritic ulcer stained with fuorescein;
Слайд 22 (E) persistent epithelial changes following resolution
of active infection;
(F) residual subepithelial haze
Слайд 28In particular, HSV
culture and PCR are commonly available testing
that can be utilized to aid in the diagnosis of HSV epithelial
keratitis. Serum antibody testing can identify previous HSV
infection. It is important to note that viral samples for lab
testing should be collected prior to epithelial staining since rose bengal is toxic to HSV [ 29 ]. Collecting samples prior to staining will thus reduce false negative test results.
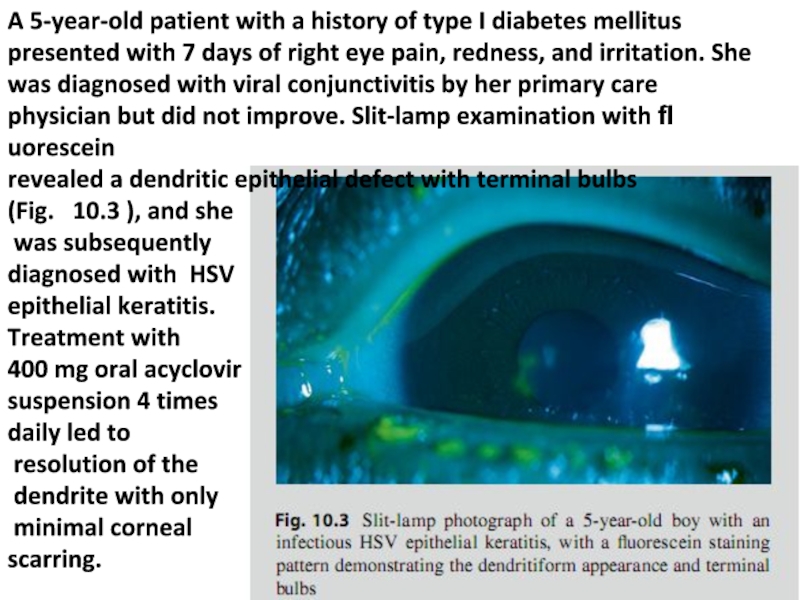
Слайд 29A 5-year-old patient with a history of type I diabetes mellitus
revealed a dendritic epithelial defect with terminal bulbs (Fig. 10.3 ), and she was subsequently diagnosed with HSV epithelial keratitis. Treatment with 400 mg oral acyclovir suspension 4 times daily led to resolution of the dendrite with only minimal corneal scarring.
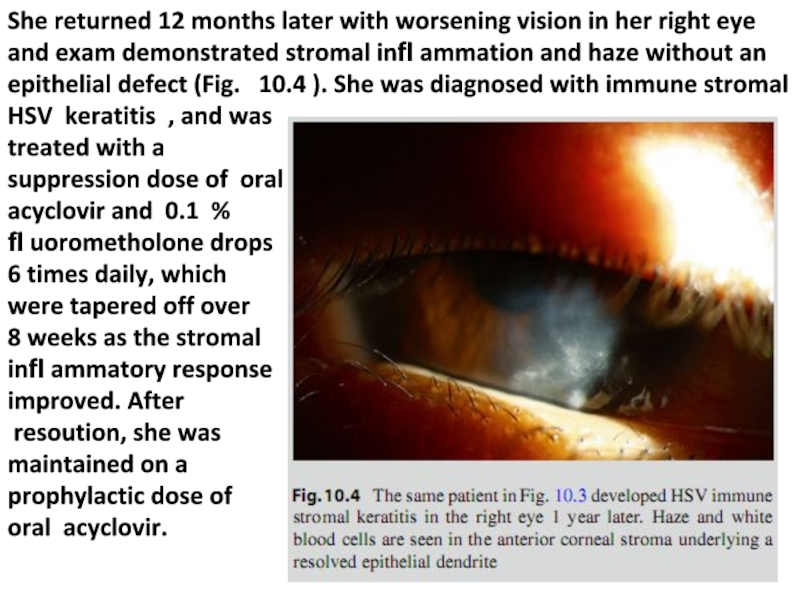
Слайд 30She returned 12 months later with worsening vision in her right
oral acyclovir.
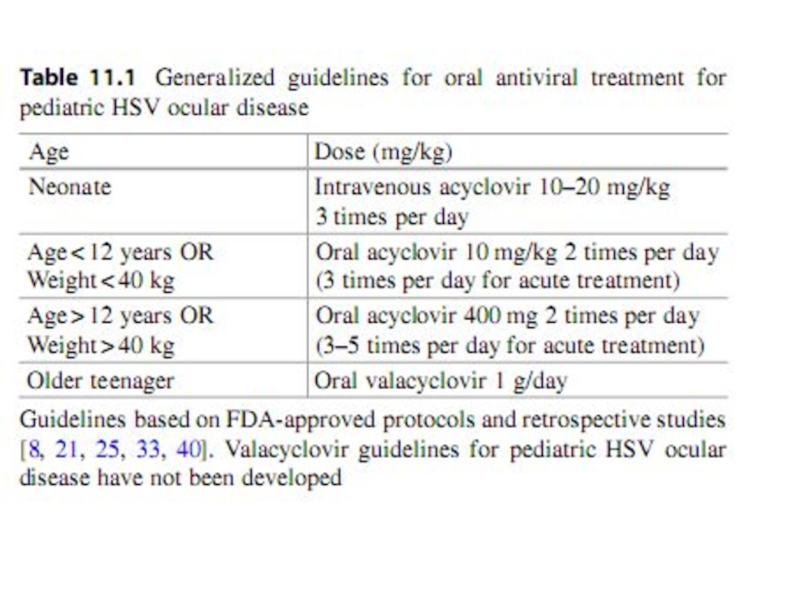
Слайд 31 Although HSV epithelial disease may resolve in some
cases without
resolution, reduce corneal scarring, and diminish stromal
infl ammation. Since the epithelial ulcers are caused by actively
replicating virus, treatment targets the virus itself. Topical
antiviral drugs (trifluridine drops, vidarabine ointment [not
currently commercially available], or ganciclovir gel) have
been shown to be effective in resolving HSV epithelial kerati-
tis. However, instillation of eye drops in small
children may be difficult, and tear dilution from crying could
prevent an effective dose. Oral acyclovir thus provides an
important adjunctive treatment for pediatric HSV epithelial
keratitis, and may provide effective treatment without the use
of a topical antiviral [ 21 ]. See Table 11.1 for acyclovir dosage
considerations.
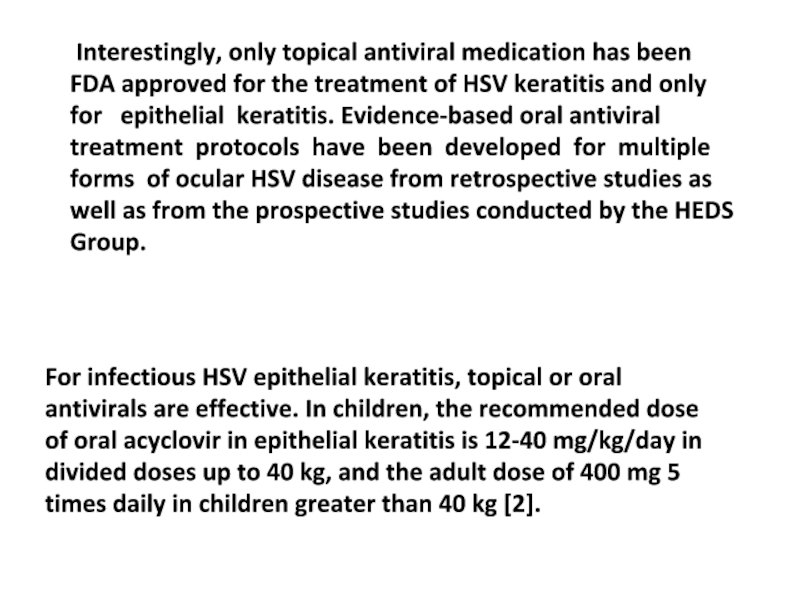
Слайд 33For infectious HSV epithelial keratitis, topical or oral
antivirals are effective.
of oral acyclovir in epithelial keratitis is 12-40 mg/kg/day in
divided doses up to 40 kg, and the adult dose of 400 mg 5
times daily in children greater than 40 kg [2].
Interestingly, only topical antiviral medication has been
FDA approved for the treatment of HSV keratitis and only
for epithelial keratitis. Evidence-based oral antiviral treatment protocols have been developed for multiple forms of ocular HSV disease from retrospective studies as well as from the prospective studies conducted by the HEDS Group.
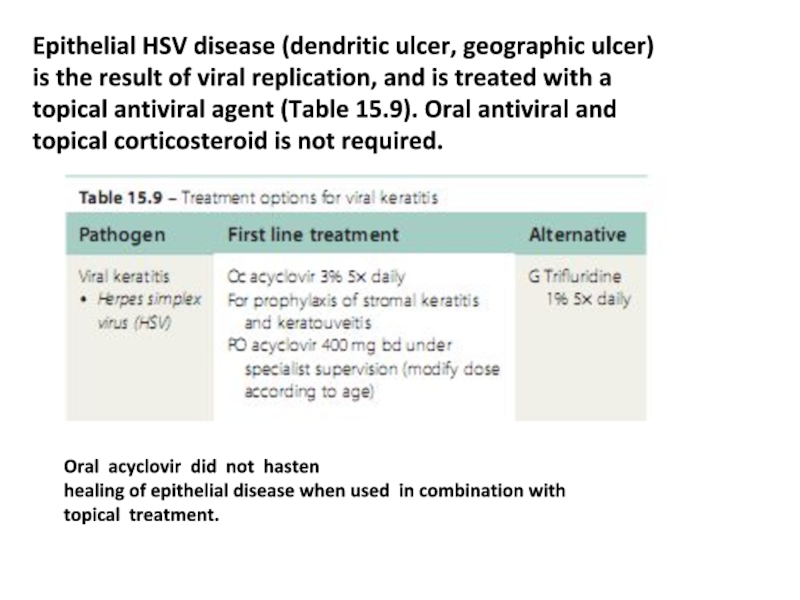
Слайд 35Oral acyclovir did not hasten
healing of epithelial disease when used
topical treatment.
Epithelial HSV disease (dendritic ulcer, geographic ulcer)
is the result of viral replication, and is treated with a
topical antiviral agent (Table 15.9). Oral antiviral and
topical corticosteroid is not required.
Слайд 36Topical corticosteroids are not indicated for
HSV epithelial keratitis and may
[ 24 ]. However, topical corticosteroids play a role in the treat-
ment of HSV stromal keratitis. Stromal keratitis is discussed
in the next section. Some clinicians recommend debridement
of infected epithelial cells to enhance resolution. Historically,
corneal debridement has been described as a method to reduce
the amount of active virus in the epithelium. However, debride-
ment may be less effective than antiviral therapy and may not
signifi cantly improve outcome of antiviral therapy [ 32 ].
Additionally, corneal debridement is diffi cult in children, and
may increase discomfort.
Слайд 37Unfortunately, as described in the introduction, HSV epi-
thelial
faint stromal scar may remain. Recurrent HSV dendritic
ulcers may recur near the scar. Epithelial recurrences increase
the risk of HSV stromal keratitis, an immune-mediated dis-
ease process. Recurrence of HSV keratitis is higher in chil-
dren and is a major management concern [ 21 ]. Thus,
monitoring of children with periodic follow-up examinations
and educating the parents for signs of recurrence are essen-
tial.
Слайд 41 HSV stromal keratitis classically involves an immune-
mediated response to
stroma [ 6 ]. However, complex presentations with mixed pat-
terns of anterior corneal disease and corneal scarring from
multiple recurrences are possible [ 24 ]. Simple HSV stromal
keratitis may present with single or multifocal sub-epithelial
infl ammatory infi ltrates.
Слайд 42Recurrent disease may have corneal
neovascularization accompanying the infl ammatory infi
trates and results in a disease presentation known as interstitial keratitis. Figure 11.3 demonstrates an active interstitial keratitis with stromal infi ltrates and vascularization.
Слайд 43Treatment of
stromal keratitis in children typically involves the use of
cal corticosteroids and oral antivirals. The topical corticoste-
roid is necessary to treat the stromal infl ammation, and the
oral antiviral treats any active viral disease in addition to a
putative contribution in preventing recurrence
Слайд 44The topical corticosteroid may be tapered and the oral antiviral discontinued
minimum amount necessary to control infl ammation.
Слайд 45Valacyclovir may be considered for
older teenage patients with HSV stromal
been FDA approved for long-term treatment (at the 1 g/day
suppressive therapy dose for genital herpes) [ 33 ]. Valacyclovir
is a pro-drug of acyclovir that has an ester moiety that is
removed by esterases to result in the active acyclovir. As a
pro-drug of acyclovir, valacyclovir has greater bioavailability
and would theoretically be expected to have a similar side
effect profi le. Famciclovir has also been approved for long-
term suppressive therapy of genital herpes (at 250 mg twice a
day), so it may also be considered for HSV stromal keratitis
in older teenage patients [ 34 ]. However, famciclovir is not
FDA approved for children.
Слайд 46Epithelial keratitis later followed by stromal keratitis or concomitant epithelial
In cases with concomitant epithelial disease, topical treatment is generally added for the fi rst 2 weeks.
Слайд 49The Herpes Eye Disease Study Group treatment guidelines are as follows:
•
• There is no additional effect of oral acyclovir over topical steroid and F3T when treating stromal keratitis.
• After epithelial HSV a 3-week course of oral acyclovir (400 mg 5 times a day) does not prevent stromal disease in the subsequent year.
• Prophylactic treatment with acyclovir (400 mg bd) reduces epithelial recurrences and stromal recurrences in patients with prior stromal disease by about 50% over 12 months. Prophylactic treatment is usually restricted
to patients with bilateral disease, prior HSV keratitis in atopes, or the immunosuppressed, especially following
corneal surgery.
Слайд 51Typical features of a neonatal HSV infection include localized external lesions
herpes affecting internal organs, and central nervous system
infection (encephalitis). An infected infant may display sev-
eral of these features. Ocular herpes in the newborn typically
appears as periorbital skin vesicles, blepharoconjunctivitis,
keratitis, anterior uveitis, chorioretinitis, and congenital cata-
racts [ 3 , 39 ]. Importantly, a dilated fundus examination
should be performed in any neonate with suspected HSV infection. Since herpes infections may resemble other neona-
tal infections, laboratory tests (e.g., fl uorescein antibody tests,
herpes culture, or PCR testing) should be performed in all
cases of suspected neonatal herpes [ 28 ]. While awaiting lab
results, the newborn should be empirically treated with intra-
venous acyclovir.
Слайд 52 Overall prognosis of neonatal ocular HSV infection
treated with intravenous
However, mortality is higher in newborns with disseminated
infection or CNS disease [ 28 ]. Visual outcome is poorer
when corneal herpetic disease causes scarring. Infants must
also be monitored closely for evidence of recurrent disease.
Infants with recurrent HSV keratitis are typically followed
longitudinally by an infectious disease specialist.
Additionally, longitudinal follow-up by a pediatric ophthal-
mologist is important due to the risk of amblyopia develop-
ment associated with recurrent HSV keratitis. If there is
recurrent neonatal ocular HSV infection, higher oral doses of
acyclovir may be necessary.
![Although HSV epithelial disease may resolve in some cases without intervention [ 30 ],](/img/tmb/5/449630/b66e1855d5d9782b80db429ea9ca139a-800x.jpg)