- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Osgood-schlatter disease презентация
Содержание
- 1. Osgood-schlatter disease
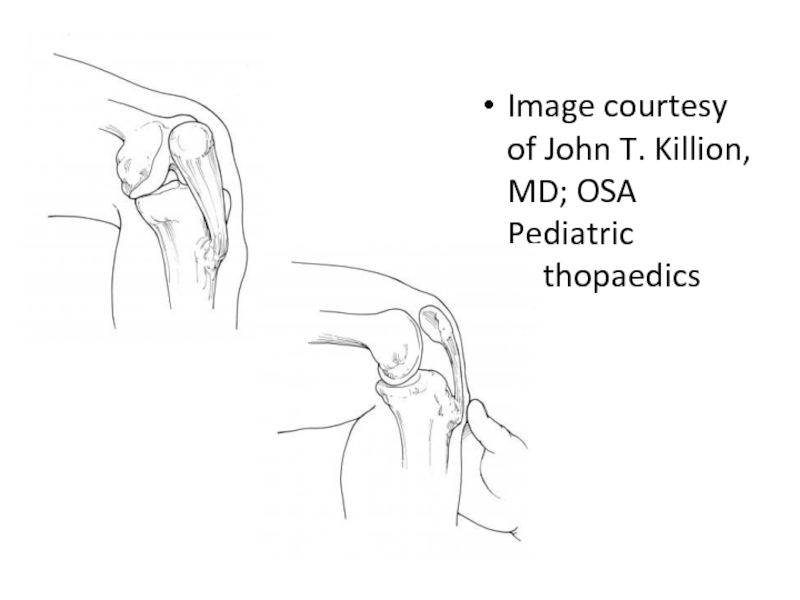
- 3. Image courtesy of John T. Killion, MD; OSA Pediatric Orthopaedics
- 4. OSD is a very common cause of
- 5. The onset of OSD is usually gradual,
- 6. OSD is a self-limiting condition. In a
- 7. Development of Osgood-Schlatter disease The insertion of
- 8. The most commonly accepted theory regarding the
- 9. Etiology The cause of Osgood-Schlatter disease (OSD)
- 10. During running, jumping, gymnastics, and other sports
- 11. Epidemiology Incidence One study found
- 12. Prognosis The prognosis in Osgood-Schlatter disease
- 13. Physical Examination The physical examination is
- 14. Diagnostic Considerations The most significant pitfall
- 15. Radiographs Not all patients with Osgood-Schlatter
- 16. The acute phase of OSD may reveal
- 17. Approach Considerations While there are no
- 18. Medical Care Treatment for Osgood-Schlatter disease
- 19. Physical Therapy The goal of rehabilitation
- 20. Straight leg raises can be performed as
- 21. Surgical Care Surgery to treat Osgood-Schlatter
- 22. In a review of a series of
- 23. Indications for surgery Occasionally, adults have
- 24. Complications While the typical conservative management
- 25. List of references http://emedicine.medscape.com/article/1993268-treatment#d3
- 26. Thank you for Attention!
Слайд 2
Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
Слайд 4OSD is a very common cause of knee pain in children
aged 8-15 years. This condition can have a prolonged course and cause loss of time from athletics. However, it is rarely a cause of permanent impairment or disability. (See Etiology and Prognosis.)
Because of a lack of a precise etiology and therefore definition, some practitioners may find differentiating OSD from avulsion fractures of the tibial tubercle to be difficult. In general if the patient is unable to ambulate, an acute avulsion fracture of the tibial tubercle is more likely. OSD patients typically can ambulate, albeit with pain. (See Physical Examination and Differentials.)
Because of a lack of a precise etiology and therefore definition, some practitioners may find differentiating OSD from avulsion fractures of the tibial tubercle to be difficult. In general if the patient is unable to ambulate, an acute avulsion fracture of the tibial tubercle is more likely. OSD patients typically can ambulate, albeit with pain. (See Physical Examination and Differentials.)
Слайд 5The onset of OSD is usually gradual, with patients commonly complaining
of pain in the tibial tubercle and/or patellar tendon region after repetitive activities. Typically, running or jumping activities that significantly stress the patellar tendon insertion upon the tibial tubercle aggravate the patient's symptoms. They may even have waxing and waning of symptoms that correspond to variations in their athletic seasons. A sudden onset of pain with no antecedent symptoms in the region of the tibial tubercle should alert the clinician to assess for a possible acute tibial tubercle avulsion rather than OSD. (See History.)
Слайд 6OSD is a self-limiting condition. In a study by Krause et
al, 90% of patients treated with conservative care were relieved of all of their symptoms approximately 1 year after onset of symptoms. [2] After skeletal maturity, patients may continue to have problems kneeling. This typically is due to tenderness over an unfused tibial tubercle ossicle or a bursa that may require resection. [3] Minimal association seems to exist between residual anterior knee pain after OSD and patellar stability, as was noted in the Krause study. The authors also noted no cases of recurvatum from premature closure of the proximal tibial physis. (See Prognosis.)
Слайд 7Development of Osgood-Schlatter disease
The insertion of the patellar tendon at the
tibial tubercle consists of cartilaginous tissue in girls younger than age 11 years and in boys younger than age 13 years. The secondary ossification center, or apophysis, of the tibial tubercle develops when girls are aged 10-12 years and when boys are aged 12-14 years. (During this stage of skeletal development, the Osgood-Schlatter lesion may occur.) (See Etiology.)
By the end of the ensuing 2 stages of bony development (eg, epiphyseal and bony stages), the primary growth plate of the proximal tibia and the secondary ossification center of the tibial tubercle fuse in males and females (usually when aged 14-18 y), and the OSD usually subsides.
By the end of the ensuing 2 stages of bony development (eg, epiphyseal and bony stages), the primary growth plate of the proximal tibia and the secondary ossification center of the tibial tubercle fuse in males and females (usually when aged 14-18 y), and the OSD usually subsides.
Слайд 8The most commonly accepted theory regarding the development of OSD is
that repeated traction (traction apophysitis) on the anterior portion of the developing ossification center leads to multiple subacute microavulsion fractures and/or tendinous inflammation, resulting in a benign, self-limited disturbance manifested as pain, swelling, and tenderness.
The most common long-term ramifications of OSD are pain on kneeling as an adult and the cosmesis of a bony prominence on the anterior knee. Less common complications are the persistence of a painful ossicle requiring surgical excision and a displaced avulsion of a tibial tubercle.
The most common long-term ramifications of OSD are pain on kneeling as an adult and the cosmesis of a bony prominence on the anterior knee. Less common complications are the persistence of a painful ossicle requiring surgical excision and a displaced avulsion of a tibial tubercle.
Слайд 9Etiology
The cause of Osgood-Schlatter disease (OSD) is unknown; however, theories suggest
that this condition is a result of repeated knee extensor mechanism contraction that causes partial microavulsions of the chondrofibro-osseous tibial tubercle. This proposed pathophysiology is supported by the repetitive runner, jumper athletic patient population OSD occurs most commonly.
Слайд 10During running, jumping, gymnastics, and other sports requiring repeated contractions of
the quadriceps, an extra-articular osteochondral stress fracture or microavulsion occurs. The proximal area of the patellar tendon insertion separates, resulting in elevation of the tibial tubercle. During the reparative phase of this stress fracture, new bone is laid down in the avulsion space, which may result in a deviated and prominent tibial tubercle. When an individual with an injured tibial tubercle continues to participate in sports, more and more microavulsions develop, and the reparative process may result in a markedly pronounced prominence of the tubercle, with longer-term cosmetic and functional implications. A separated fragment may develop at the patellar tendon insertion and may lead to chronic, nonunion-type pain.
In a magnetic resonance imaging (MRI) study of 20 patients with OSD, the patellar tendon was noted to attach more proximally and in a broader area to the tibia in patients with OSD. [4] Approximately 50% of patients with OSD relate a history of precipitating trauma.
Histologic studies support a traumatic etiology.
Risk factors
Risk factors for OSD include the following:
Age: female 8-12 years & male between 12-15 years
Male sex (3:1)
Rapid skeletal growth
Repetitive sprinting and jumping sports
A study by Nakase et al found that quadriceps femoris muscle tightness and strength during knee extension and flexibility of the hamstring muscles were risk factors for incidence of Osgood-Schlatter disease
In a magnetic resonance imaging (MRI) study of 20 patients with OSD, the patellar tendon was noted to attach more proximally and in a broader area to the tibia in patients with OSD. [4] Approximately 50% of patients with OSD relate a history of precipitating trauma.
Histologic studies support a traumatic etiology.
Risk factors
Risk factors for OSD include the following:
Age: female 8-12 years & male between 12-15 years
Male sex (3:1)
Rapid skeletal growth
Repetitive sprinting and jumping sports
A study by Nakase et al found that quadriceps femoris muscle tightness and strength during knee extension and flexibility of the hamstring muscles were risk factors for incidence of Osgood-Schlatter disease
Слайд 11Epidemiology
Incidence
One study found that Osgood-Schlatter disease (OSD) affected approximately 21% of
athletic adolescents surveyed, as compared with a frequency of 4.5% in age-matched nonathletic controls. [6]
One Finnish study found that OSD affected 13% of athletes.
Sex predilection
OSD occurs more frequently in boys, with a male-to-female ratio of 3:1.
Age predilection
OSD usually is seen in the adolescent years, after a patient has undergone a rapid growth spurt the previous year.
Girls who are affected are typically aged 10-11 years but can range from age 8-12 years.
Boys who are affected are typically aged 13-14 years but can range from age 12-15 years.
One Finnish study found that OSD affected 13% of athletes.
Sex predilection
OSD occurs more frequently in boys, with a male-to-female ratio of 3:1.
Age predilection
OSD usually is seen in the adolescent years, after a patient has undergone a rapid growth spurt the previous year.
Girls who are affected are typically aged 10-11 years but can range from age 8-12 years.
Boys who are affected are typically aged 13-14 years but can range from age 12-15 years.
Слайд 12Prognosis
The prognosis in Osgood-Schlatter disease (OSD) is excellent. OSD is usually
self-limiting and resolves by the time the patient is aged 18 years, when the tibial tubercle apophysis ossifies. In approximately 10% of patients, however, the symptoms continue unabated into adulthood despite all conservative measures. [7] This may be from residual enlargement of the tuberosity or from ossicle formation in the patellar tendon.
The likelihood for long-term sequelae increases in severe cases, in cases in which treatment is not sought, or in cases in which the patient demonstrates poor compliance with the physician's recommendations.
In the study by Krause et al, 90% of patients treated with conservative care were relieved of all of their symptoms approximately 1 year following symptom onset. [2]
In some cases, however, discomfort may persist for 2-3 years until the tibial growth plate closes.
The likelihood for long-term sequelae increases in severe cases, in cases in which treatment is not sought, or in cases in which the patient demonstrates poor compliance with the physician's recommendations.
In the study by Krause et al, 90% of patients treated with conservative care were relieved of all of their symptoms approximately 1 year following symptom onset. [2]
In some cases, however, discomfort may persist for 2-3 years until the tibial growth plate closes.
Слайд 13Physical Examination
The physical examination is very specific, with point tenderness over
the tibial tubercle. A firm mass may be palpable.
Other physical examination findings may include the following:
Proximal tibial swelling and tenderness
Enlargement or prominence of the tibial tubercle
Reproducible and aggravated pain by direct pressure and jumping (quadriceps contraction)
Pain with resisted knee extension (quadriceps contraction)
Hamstring tightness
Quadriceps atrophy
Erythema of the tibial tuberosity
The following exam findings must be tested and confirmed to verify no concomitant or more severe injury:
Full range of motion of the knee
No effusion or meniscal signs
Negative Lachman test (no knee instability)
Normal neurovascular examination
No abnormal findings in the hip and ankle joints
Other physical examination findings may include the following:
Proximal tibial swelling and tenderness
Enlargement or prominence of the tibial tubercle
Reproducible and aggravated pain by direct pressure and jumping (quadriceps contraction)
Pain with resisted knee extension (quadriceps contraction)
Hamstring tightness
Quadriceps atrophy
Erythema of the tibial tuberosity
The following exam findings must be tested and confirmed to verify no concomitant or more severe injury:
Full range of motion of the knee
No effusion or meniscal signs
Negative Lachman test (no knee instability)
Normal neurovascular examination
No abnormal findings in the hip and ankle joints
Слайд 14Diagnostic Considerations
The most significant pitfall is failing to diagnose another condition
that could result in long-term permanent damage (eg, tumor, osteochondritis dissecans). Most other conditions have a more concerning clinical examination or history. Therefore, always obtain radiographs and consider the possibility of a referred pain syndrome from the hip.
Conditions to be considered in the differential diagnosis of Osgood-Schlatter disease (OSD), in addition to those in the next section, include the following:
Sinding-Larson-Johansson syndrome
Tumor (bone or soft tissue)
Perthes disease (often presents with knee pain instead of hip complaints)
Patellar tendon avulsion/rupture
Chondromalacia patellae (Patellofemoral syndrome)
Patellar tendonitis
Infectious apophysitis
Accessory ossification centers
Osteomyelitis of the proximal tibia
Hoffa's syndrome
Synovial plica injury
Tibial tubercle fracture
Differential Diagnoses
Femur Injuries and Fractures
Knee Osteochondritis Dissecans
Legg-Calve-Perthes Disease
Osteomyelitis
Patellar Tendon Rupture
Patellofemoral Joint Syndromes
Pes Anserine Bursitis
Prepatellar Bursitis
Tibia and Fibula Fracture in the ED
Tibial Tubercle Avulsion
Conditions to be considered in the differential diagnosis of Osgood-Schlatter disease (OSD), in addition to those in the next section, include the following:
Sinding-Larson-Johansson syndrome
Tumor (bone or soft tissue)
Perthes disease (often presents with knee pain instead of hip complaints)
Patellar tendon avulsion/rupture
Chondromalacia patellae (Patellofemoral syndrome)
Patellar tendonitis
Infectious apophysitis
Accessory ossification centers
Osteomyelitis of the proximal tibia
Hoffa's syndrome
Synovial plica injury
Tibial tubercle fracture
Differential Diagnoses
Femur Injuries and Fractures
Knee Osteochondritis Dissecans
Legg-Calve-Perthes Disease
Osteomyelitis
Patellar Tendon Rupture
Patellofemoral Joint Syndromes
Pes Anserine Bursitis
Prepatellar Bursitis
Tibia and Fibula Fracture in the ED
Tibial Tubercle Avulsion
Слайд 15Radiographs
Not all patients with Osgood-Schlatter disease (OSD) need radiography, since the
diagnosis is clinical. However, plain films are should be obtained at least once in the evaluation and treatment to rule out other etiologies, such as neoplasm, acute tibial apophyseal fracture, and infection.
Radiographs may indicate:
Superficial ossicle in the patellar tendon
Irregular ossification of the proximal tibial tuberosity
Calcification within the patellar tendon
Thickening of the patellar tendon
Soft-tissue edema proximal to the tibial tuberosity
The Osgood-Schlatter lesion is best seen on the lateral view, with the knee in slight internal rotation of 10-20°.
The most common finding is that the knee films are normal, especially if the child is in the preossification phase.
Radiographs may indicate:
Superficial ossicle in the patellar tendon
Irregular ossification of the proximal tibial tuberosity
Calcification within the patellar tendon
Thickening of the patellar tendon
Soft-tissue edema proximal to the tibial tuberosity
The Osgood-Schlatter lesion is best seen on the lateral view, with the knee in slight internal rotation of 10-20°.
The most common finding is that the knee films are normal, especially if the child is in the preossification phase.
Слайд 16The acute phase of OSD may reveal a prominent and elevated
tibial tubercle with anterior soft-tissue swelling.
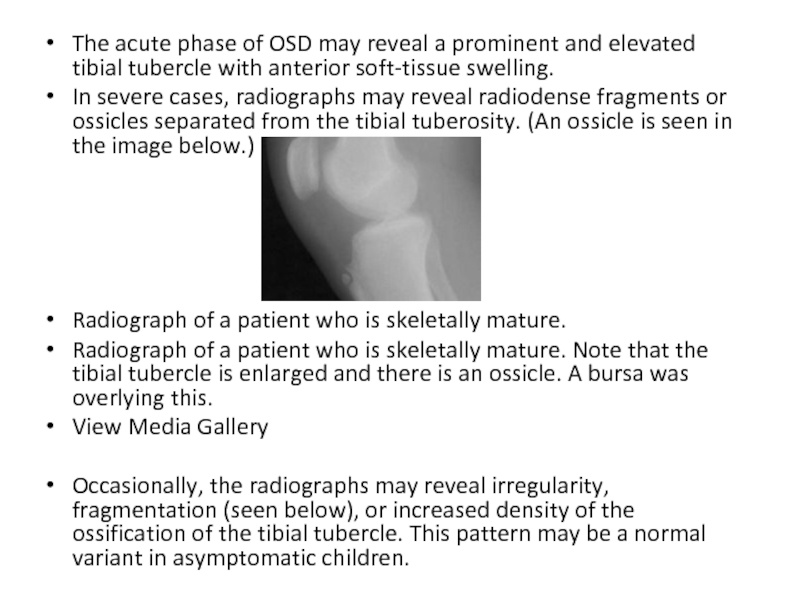
In severe cases, radiographs may reveal radiodense fragments or ossicles separated from the tibial tuberosity. (An ossicle is seen in the image below.)
Radiograph of a patient who is skeletally mature.
Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
View Media Gallery
Occasionally, the radiographs may reveal irregularity, fragmentation (seen below), or increased density of the ossification of the tibial tubercle. This pattern may be a normal variant in asymptomatic children.
In severe cases, radiographs may reveal radiodense fragments or ossicles separated from the tibial tuberosity. (An ossicle is seen in the image below.)
Radiograph of a patient who is skeletally mature.
Radiograph of a patient who is skeletally mature. Note that the tibial tubercle is enlarged and there is an ossicle. A bursa was overlying this.
View Media Gallery
Occasionally, the radiographs may reveal irregularity, fragmentation (seen below), or increased density of the ossification of the tibial tubercle. This pattern may be a normal variant in asymptomatic children.
Слайд 17Approach Considerations
While there are no prospective studies evaluating the treatment of
OSD, including the recommended conservative treatments, The American Academy of Orthopaedic Surgeons and the American Academy of Family Practice recommend the following for the management of Osgood-Schlatter disease (OSD).
Activity limitation
Ice
Anti-inflammatories
Protective padding
Quadriceps/hamstring strengthening
Time
Activity limitation
Ice
Anti-inflammatories
Protective padding
Quadriceps/hamstring strengthening
Time
Слайд 18Medical Care
Treatment for Osgood-Schlatter disease (OSD) is conservative. Initial treatment includes
the application of ice for 20 minutes every 2-4 hours.
Analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) may be given for pain relief and reduction of local inflammation. However, NSAIDs have not been shown to shorten the course of OSD.
Patellar tendon insertion injections have historically not been recommended. This is due in large part to the possibility of subcutaneous tissue atrophy after corticosteroid injections. A recent study out of Japan looked at lidocaine/dextrose injection vs. just lidocaine. No difference was seen between the two injection groups however both groups reported symptom relief with no adverse outcomes. [13]
Long-term immobilization is typically contraindicated, because it may result in increased knee stiffness in mild cases, thus predisposing the athlete to additional sports-related injuries. However, if a patient is noncompliant, the clinician may recommend immobilization in a knee brace for a minimum of 6 weeks. The brace should be removed daily, but only for stretching and strengthening exercises.
Inform the patient to avoid pain-producing activities (eg, sports that involve excess amounts of jumping).
Infrapatellar strap, pads, or braces may also be used for support, but none have any proven efficacy.
Once the acute symptoms have abated, quadriceps-stretching exercises, including hip extension for a complete stretch of the extensor mechanism, may be performed to reduce tension on the tibial tubercle. Stretching exercises for the hamstrings, which are commonly tight, may also be performed.
Other than the presence of an ossicle that causes pain with kneeling, there are no long-term disabilities or problems associated with this condition.
Analgesics and nonsteroidal anti-inflammatory drugs (NSAIDs) may be given for pain relief and reduction of local inflammation. However, NSAIDs have not been shown to shorten the course of OSD.
Patellar tendon insertion injections have historically not been recommended. This is due in large part to the possibility of subcutaneous tissue atrophy after corticosteroid injections. A recent study out of Japan looked at lidocaine/dextrose injection vs. just lidocaine. No difference was seen between the two injection groups however both groups reported symptom relief with no adverse outcomes. [13]
Long-term immobilization is typically contraindicated, because it may result in increased knee stiffness in mild cases, thus predisposing the athlete to additional sports-related injuries. However, if a patient is noncompliant, the clinician may recommend immobilization in a knee brace for a minimum of 6 weeks. The brace should be removed daily, but only for stretching and strengthening exercises.
Inform the patient to avoid pain-producing activities (eg, sports that involve excess amounts of jumping).
Infrapatellar strap, pads, or braces may also be used for support, but none have any proven efficacy.
Once the acute symptoms have abated, quadriceps-stretching exercises, including hip extension for a complete stretch of the extensor mechanism, may be performed to reduce tension on the tibial tubercle. Stretching exercises for the hamstrings, which are commonly tight, may also be performed.
Other than the presence of an ossicle that causes pain with kneeling, there are no long-term disabilities or problems associated with this condition.
Слайд 19Physical Therapy
The goal of rehabilitation is for the athlete to be
able to return to his or her sport as quickly and safely as possible. Since the main treatment is rest, ice, and NSAIDs, the role of physical therapy is limited, if used at all. The pain may take up to 6-24 months to resolve. If an individual returns to activity too soon, he or she may worsen the condition. Athletes need to work on improving the flexibility and strength of the quadriceps and hamstring muscles throughout the course of rehabilitation to ensure that they are ready to return to sports.
Acute phase
Several techniques may be recommended by the physical therapist to alleviate discomfort and avert recurrence of the disease. Treatment recommendations are dependent upon the severity of the condition.
An infrapatellar strap may be recommended during sports activity but has no proven efficacy.
Resting is recommended when pain arises.
Ice should be applied to the area for 20 minutes following activity.
Short-term rest and knee immobilization may be required.
On rare occasions, this author has casted a patient who has severe pain and is noncompliant with conservative care. This is usually with a parent who is intent on relieving the pain. While a brace can be recommended, it is doubtful that it will be used in a noncompliant patient.
Recovery phase
The following regimen recommendations for patients with OSD are taken from Meisterling, Wall, and Meisterling.
Acute phase
Several techniques may be recommended by the physical therapist to alleviate discomfort and avert recurrence of the disease. Treatment recommendations are dependent upon the severity of the condition.
An infrapatellar strap may be recommended during sports activity but has no proven efficacy.
Resting is recommended when pain arises.
Ice should be applied to the area for 20 minutes following activity.
Short-term rest and knee immobilization may be required.
On rare occasions, this author has casted a patient who has severe pain and is noncompliant with conservative care. This is usually with a parent who is intent on relieving the pain. While a brace can be recommended, it is doubtful that it will be used in a noncompliant patient.
Recovery phase
The following regimen recommendations for patients with OSD are taken from Meisterling, Wall, and Meisterling.
Слайд 20Straight leg raises can be performed as follows:
Lie on the floor
with the back propped up a few inches with the elbows
Bend the unaffected knee to a comfortable position; using adjustable ankle weights with half-pound increments, determine the weight at which 10 raises can be performed on the affected leg
Tighten the thigh muscles and lift the affected leg 12 inches, keeping the leg straight
Hold for 5 seconds
Slowly lower the leg and relax
Start with 10 repetitions for each leg
When 15 repetitions have been performed comfortably, increase the weight by half a pound and drop back to 10 repetitions
Once 15 repetitions again can be performed comfortably, increase the weight again, to a maximum of 7-12 lb
Short-arc quadriceps exercises can be performed as follows:
Lie back with the unaffected knee bent (same as for straight leg raises)
Place a few rolled up towels under the affected knee to raise it 6 inches from the floor
Tighten the thigh muscles and straighten the leg until it is 12 inches from the floor
Hold for 5 seconds
Slowly lower the leg and relax
Start with 10 repetitions for each leg and increase to 15, using the same ankle weight and repetition progression as for straight leg raises
Wall slides can be performed as follows:
To do wall slides or quarter seats, stand about 12 inches from a smooth wall and lean back against it with the feet shoulder width apart
Holding a light dumbbell in each hand with the arms straight down, bend the knees and slowly lower the body 4-6 inches
If pain is felt, the body has squatted too far
Hold for 5 seconds and then rise up quickly
Start with 10 repetitions and increase to 15, gradually increasing the dumbbell weight in the same type of progression as for straight leg raises
A good rule of thumb with regard to squats and wall slides for patients with patellar pain of any kind is a relative restriction of not flexing the knee beyond 90°.
Bend the unaffected knee to a comfortable position; using adjustable ankle weights with half-pound increments, determine the weight at which 10 raises can be performed on the affected leg
Tighten the thigh muscles and lift the affected leg 12 inches, keeping the leg straight
Hold for 5 seconds
Slowly lower the leg and relax
Start with 10 repetitions for each leg
When 15 repetitions have been performed comfortably, increase the weight by half a pound and drop back to 10 repetitions
Once 15 repetitions again can be performed comfortably, increase the weight again, to a maximum of 7-12 lb
Short-arc quadriceps exercises can be performed as follows:
Lie back with the unaffected knee bent (same as for straight leg raises)
Place a few rolled up towels under the affected knee to raise it 6 inches from the floor
Tighten the thigh muscles and straighten the leg until it is 12 inches from the floor
Hold for 5 seconds
Slowly lower the leg and relax
Start with 10 repetitions for each leg and increase to 15, using the same ankle weight and repetition progression as for straight leg raises
Wall slides can be performed as follows:
To do wall slides or quarter seats, stand about 12 inches from a smooth wall and lean back against it with the feet shoulder width apart
Holding a light dumbbell in each hand with the arms straight down, bend the knees and slowly lower the body 4-6 inches
If pain is felt, the body has squatted too far
Hold for 5 seconds and then rise up quickly
Start with 10 repetitions and increase to 15, gradually increasing the dumbbell weight in the same type of progression as for straight leg raises
A good rule of thumb with regard to squats and wall slides for patients with patellar pain of any kind is a relative restriction of not flexing the knee beyond 90°.
Слайд 21Surgical Care
Surgery to treat Osgood-Schlatter disease (OSD) is rarely indicated.
Surgery in
a skeletally immature patient is almost never indicated. Removal of ossicle fragmentation in immature patients with an unfused apophysis can lead to premature fusion of the tibial tubercle. [3]
In a study of the surgical treatment of unresolved Osgood-Schlatter disease (OSD), Pihlajamäki et al concluded that in most young adults, good to excellent functional outcomes can be achieved with surgical treatment of unresolved OSD. [14] The investigators examined postsurgical clinical courses, radiographic characteristics, and long-term outcomes of 107 military recruits (117 knees) who were operated on for the condition. Functional outcome data were gathered from medical records, interviews, questionnaires, and physical and radiographic examinations. By the end of a (median) 10-year follow-up period, 93 patients (87%) reported that they could participate without restriction in daily and work activities, and 80 patients (75%) had regained their preoperative sports activity level. In addition, 41 patients (38%) reported the ability to kneel without pain. Minor postoperative complications occurred in 6 patients, and 2 patients required reoperation for OSD.
In a study of the surgical treatment of unresolved Osgood-Schlatter disease (OSD), Pihlajamäki et al concluded that in most young adults, good to excellent functional outcomes can be achieved with surgical treatment of unresolved OSD. [14] The investigators examined postsurgical clinical courses, radiographic characteristics, and long-term outcomes of 107 military recruits (117 knees) who were operated on for the condition. Functional outcome data were gathered from medical records, interviews, questionnaires, and physical and radiographic examinations. By the end of a (median) 10-year follow-up period, 93 patients (87%) reported that they could participate without restriction in daily and work activities, and 80 patients (75%) had regained their preoperative sports activity level. In addition, 41 patients (38%) reported the ability to kneel without pain. Minor postoperative complications occurred in 6 patients, and 2 patients required reoperation for OSD.
Слайд 22In a review of a series of patients who were treated
operatively, Binazzi et al found that the most widely used procedure was excision of all intratendinous ossicles, with or without removal of a portion of the prominent tibial tubercle. [15] A comparison of 2 groups of individuals, 1 with 15 individuals treated with excision of ossicles and 1 with 11 individuals treated with various methods before 1975, clearly showed that results of simple excision of the ossicles were better.
A study looked to determine the outcomes of bursoscopic ossicle excision in young, skeletally-mature, active patients with unresolved symptoms from an ossicle related to prior Osgood-Schlatter disease. The study concluded that bursoscopic ossicle excision showed satisfactory outcomes in selective young, skeletally-mature, and active patients with persistent symptoms and the presence of an ossicle. However, the authors added that bursoscopic surgery showed limitation in reducing the prominence of the tibial tuberosity. [16]
In another study, patients treated operatively were found to be no more likely than conservatively treated patients to be relieved of pain or to have improvement of cosmetic appearance.
If a true tibial tubercle avulsion occurs due to the contracture of the extensor mechanism. Open reduction and internal fixation (ORIF) usually is recommended, depending on the size and displacement of the fragment as well as the phase of apophyseal closure.
A study looked to determine the outcomes of bursoscopic ossicle excision in young, skeletally-mature, active patients with unresolved symptoms from an ossicle related to prior Osgood-Schlatter disease. The study concluded that bursoscopic ossicle excision showed satisfactory outcomes in selective young, skeletally-mature, and active patients with persistent symptoms and the presence of an ossicle. However, the authors added that bursoscopic surgery showed limitation in reducing the prominence of the tibial tuberosity. [16]
In another study, patients treated operatively were found to be no more likely than conservatively treated patients to be relieved of pain or to have improvement of cosmetic appearance.
If a true tibial tubercle avulsion occurs due to the contracture of the extensor mechanism. Open reduction and internal fixation (ORIF) usually is recommended, depending on the size and displacement of the fragment as well as the phase of apophyseal closure.
Слайд 23Indications for surgery
Occasionally, adults have a large ossicle and an
overlying bursa, which may cause pain with kneeling. If so, treatment consists of excision of the bursa, ossicle, and any prominence.
Contraindications for surgery
The real question is whether or not surgery is ever indicated in the growing child, as OSD is self-limiting. Trail reviewed 2 groups of symptomatic patients with this condition with 4-5 years of follow-up. [18] One group was treated surgically with tibial sequestrectomy, and the other was managed conservatively. Surgery was found to offer no significant benefit over conservative care. In addition, a significant complication rate was identified with tibial sequestrectomy.
Contraindications for surgery
The real question is whether or not surgery is ever indicated in the growing child, as OSD is self-limiting. Trail reviewed 2 groups of symptomatic patients with this condition with 4-5 years of follow-up. [18] One group was treated surgically with tibial sequestrectomy, and the other was managed conservatively. Surgery was found to offer no significant benefit over conservative care. In addition, a significant complication rate was identified with tibial sequestrectomy.
Слайд 24Complications
While the typical conservative management will relieve the pain associated once
skeletal maturity is reached, continued tibial tubercle prominence and pain upon kneeling can be a problem into adulthood.
Complications following resection of an ossicle can include:
surgical wound infection/dehiscence
poor cosmesis
unsightly scar
peri-incisional numbness
growth disturbance (skeletally immature)
Trail et al showed 55% of patients had an obvious bony prominence postoperatively. One third of these were quite apparent and troublesome and 3 required repeat procedures to deal with associated discomfort.
Complications following resection of an ossicle can include:
surgical wound infection/dehiscence
poor cosmesis
unsightly scar
peri-incisional numbness
growth disturbance (skeletally immature)
Trail et al showed 55% of patients had an obvious bony prominence postoperatively. One third of these were quite apparent and troublesome and 3 required repeat procedures to deal with associated discomfort.