CCC-SLP
- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Oral motor skills and feeding презентация
Содержание
- 1. Oral motor skills and feeding
- 2. AGENDA Anatomy and physiology of
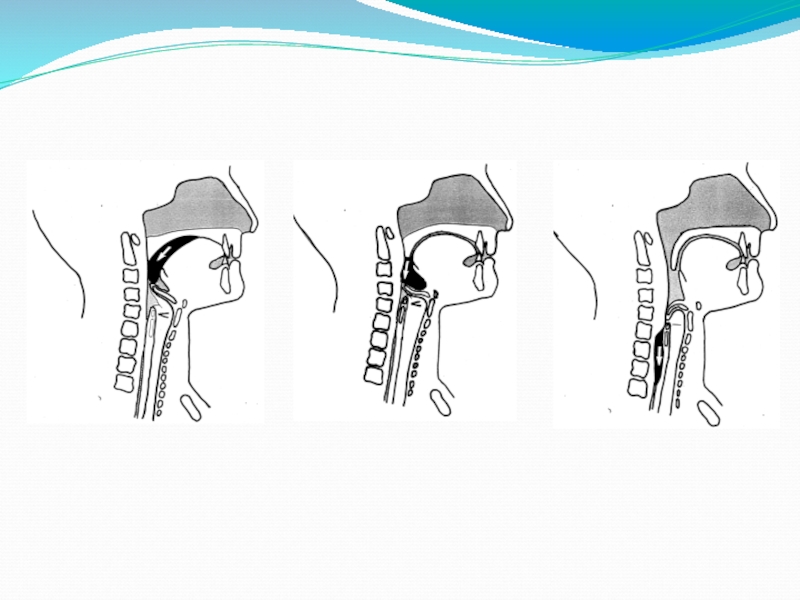
- 3. Anatomy Lips Teeth Tongue Palate/Velum Epiglottis Trachea Esophagus
- 5. Normal Development and Feeding Skills Please refer to handout
- 6. Initial Observations Look at motor patterns and
- 7. Medical Issues To Consider Reflux: The backward
- 9. Positioning: What happens in your hips passes
- 11. For Safety Sake Children should always be
- 12. Sensory Needs How comfortable is the child
- 13. Techniques For Dysfunctional Oral Structures (Lips, jaw
- 14. Chewing Techniques The goal is to teach
- 15. Tongue Retraction In tongue retraction the tongue
- 16. Tongue Protrusion Low tone tongue moves forward
- 17. Lip retraction Lip retraction occurs with increase
- 18. Low tone cheeks/lips Hypotonia in the
- 19. Straw drinking/Cup use Use a squeeze box
- 20. Incorporate solid foods in therapy Cheetos and
- 21. Prevent Food Jags Food jags are when
Слайд 2AGENDA
Anatomy and physiology of the oral/pharyngeal structures for feeding skills
A
sequential look at development related to feeding skills
Oral motor treatment and feeding
Oral motor treatment and feeding
Слайд 6Initial Observations
Look at motor patterns and body stability; positioning options
Determine sensory
needs: gravitational security, tactile/auditory/olfactory/gustatory defensiveness
Assess problems with function of individual oral structures (jaw, kips, tongue, cheeks, palate)
Type of food child is eating
Behavioral issues: rule out medical, then determine if it’s a sensory vs. behavioral issue
Assess problems with function of individual oral structures (jaw, kips, tongue, cheeks, palate)
Type of food child is eating
Behavioral issues: rule out medical, then determine if it’s a sensory vs. behavioral issue
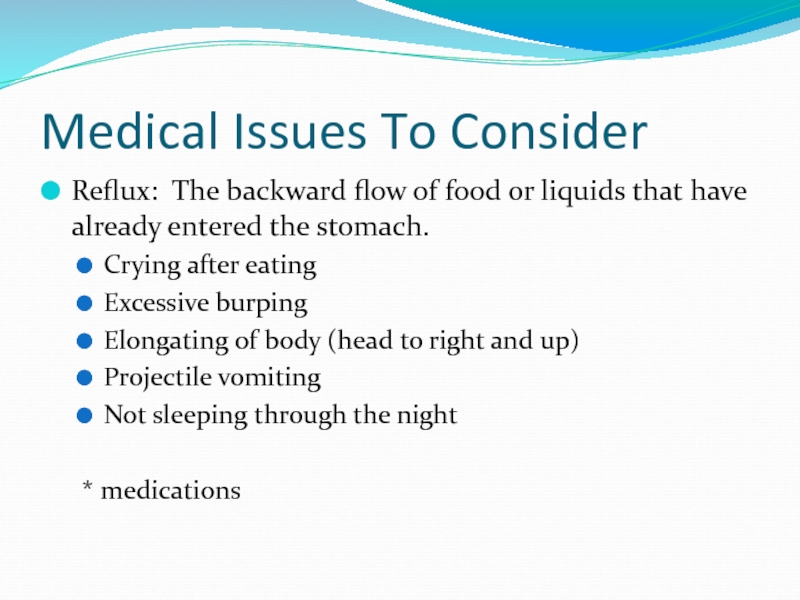
Слайд 7Medical Issues To Consider
Reflux: The backward flow of food or liquids
that have already entered the stomach.
Crying after eating
Excessive burping
Elongating of body (head to right and up)
Projectile vomiting
Not sleeping through the night
* medications
Crying after eating
Excessive burping
Elongating of body (head to right and up)
Projectile vomiting
Not sleeping through the night
* medications
Слайд 9Positioning: What happens in your hips passes to your lips!
Mobility develops
from proximal to distal; precise interchange between stability and mobility that influences oral motor skills.
Oral stability is dependent upon the development of neck and shoulder stability that is in turn dependent on trunk and pelvic stability.
Lips, cheeks, and tongue are dependent on jaw stability.
Position the child to support the head and trunk so that the hands and mouth are free to work.
Oral stability is dependent upon the development of neck and shoulder stability that is in turn dependent on trunk and pelvic stability.
Lips, cheeks, and tongue are dependent on jaw stability.
Position the child to support the head and trunk so that the hands and mouth are free to work.
Слайд 11For Safety Sake
Children should always be fed in a highchair or
the lap of their parent
No cracked or sticky/gummy nipples (replace them)
Children under the age of 3 should not be given hard candy
No chocolate of any kind before 1 year
No honey before age 1
Hot dogs, peanuts, peanut butter, whole grapes, and candy are choking hazards.
Begin open cup drinking at 6 months
Never lay a baby down with a propped bottle
Never give a baby a bottle or sippy cup to keep in their bed to pacify them. If you must, only fill it with water
No bottles after 15 months
No cereal in bottle!!!!!
No cracked or sticky/gummy nipples (replace them)
Children under the age of 3 should not be given hard candy
No chocolate of any kind before 1 year
No honey before age 1
Hot dogs, peanuts, peanut butter, whole grapes, and candy are choking hazards.
Begin open cup drinking at 6 months
Never lay a baby down with a propped bottle
Never give a baby a bottle or sippy cup to keep in their bed to pacify them. If you must, only fill it with water
No bottles after 15 months
No cereal in bottle!!!!!
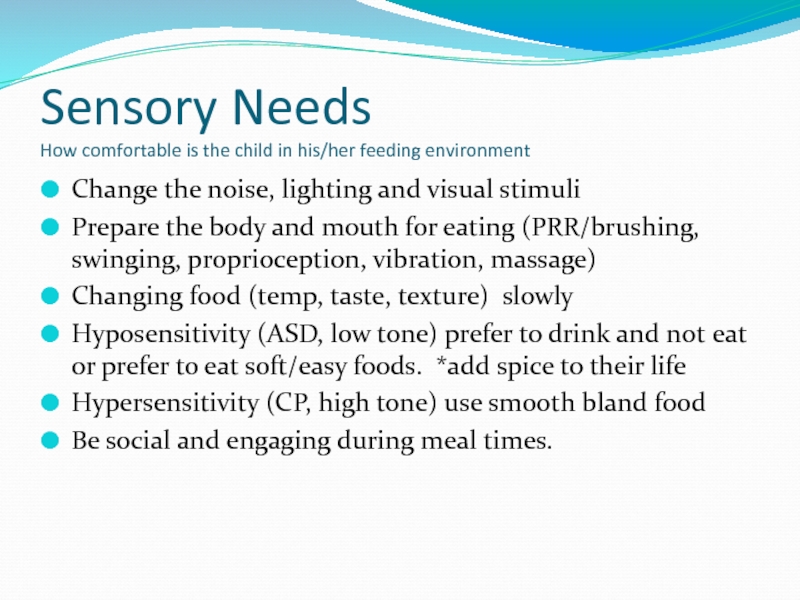
Слайд 12Sensory Needs
How comfortable is the child in his/her feeding environment
Change the
noise, lighting and visual stimuli
Prepare the body and mouth for eating (PRR/brushing, swinging, proprioception, vibration, massage)
Changing food (temp, taste, texture) slowly
Hyposensitivity (ASD, low tone) prefer to drink and not eat or prefer to eat soft/easy foods. *add spice to their life
Hypersensitivity (CP, high tone) use smooth bland food
Be social and engaging during meal times.
Prepare the body and mouth for eating (PRR/brushing, swinging, proprioception, vibration, massage)
Changing food (temp, taste, texture) slowly
Hyposensitivity (ASD, low tone) prefer to drink and not eat or prefer to eat soft/easy foods. *add spice to their life
Hypersensitivity (CP, high tone) use smooth bland food
Be social and engaging during meal times.
Слайд 13Techniques For Dysfunctional Oral Structures
(Lips, jaw tongue and cheeks)
Jaw: slack/low muscle
tone or jaw thrust open/increased muscle tone and teeth grinding
Check positioning of the hips/shoulders/chin (reduce hip extension or posterior tilt and shoulder retraction, and position the chin down)
Give jaw control/support as needed
Calm/organize the mouth with vibration
Ice/cold increases swallow reflex (ie ice straw)
Chew tubes
Bite tip on Z-Vibe (front to back on left and right)
Check positioning of the hips/shoulders/chin (reduce hip extension or posterior tilt and shoulder retraction, and position the chin down)
Give jaw control/support as needed
Calm/organize the mouth with vibration
Ice/cold increases swallow reflex (ie ice straw)
Chew tubes
Bite tip on Z-Vibe (front to back on left and right)
Слайд 14Chewing Techniques
The goal is to teach a graded, lateral chew with
tongue-tip dissociation and movement across midline.
Graded lateral chew with tongue tip pointing: chew tube or Z-Vibe perpendicular to the lateral molar ridge as you support jaw as needed, encourage 2-3 bites. Alternate sides 4-5 times. Intro. Veggie stix or ice straw
Tongue tip Pointing and movement of bolus to lateral incisor and molar ridge: place tube/stick food from molar ridge to lateral incisor and alternate sides
Tongue-tip pointing and tongue lateralization across midline: present stick-shaped food or tube on lateral incisor and bit quickly present bolus to opposite lateral incisor.
5 point bite: present the stick shaped bolus perpendicular to the lateral molar ridge, to the incisor, to the front, and move bolus around midline to opposite molar ridge.
Graded lateral chew with tongue tip pointing: chew tube or Z-Vibe perpendicular to the lateral molar ridge as you support jaw as needed, encourage 2-3 bites. Alternate sides 4-5 times. Intro. Veggie stix or ice straw
Tongue tip Pointing and movement of bolus to lateral incisor and molar ridge: place tube/stick food from molar ridge to lateral incisor and alternate sides
Tongue-tip pointing and tongue lateralization across midline: present stick-shaped food or tube on lateral incisor and bit quickly present bolus to opposite lateral incisor.
5 point bite: present the stick shaped bolus perpendicular to the lateral molar ridge, to the incisor, to the front, and move bolus around midline to opposite molar ridge.
Слайд 15Tongue Retraction
In tongue retraction the tongue pulls back into the posterior
¾ of the mouth or in the pharyngeal airway. Can be related to low or high muscle tone with neck hyper extension or cleft palate
Work on building tone by bouncing on a ball or lap before positioning for eating
Child is prone over lap then stroke tongue from middle to tip toward lips
When seated, keep child’s chin tucked down, gently tap/hold under chin to increase tongue tone/stability, vibrate from middle to tip and lateral to tip (Z-vibe)
Work on building tone by bouncing on a ball or lap before positioning for eating
Child is prone over lap then stroke tongue from middle to tip toward lips
When seated, keep child’s chin tucked down, gently tap/hold under chin to increase tongue tone/stability, vibrate from middle to tip and lateral to tip (Z-vibe)
Слайд 16Tongue Protrusion
Low tone tongue moves forward beyond the border of the
gums and may stick out between the lips and may cause food to be pushed out of the mouth
Build tone in the trunk and provide proximal stability by compression of spine through shoulders, bounce on lap or ball
Position in feeding chair with increased support of the trunk and feet
Feed to the sides of the mouth to improve tongue lateralization
Thicken liquids
Present flat bowl spoon in horizontal position midway and vibrate to tip (Z-Vibe)
Offer vibration with battery operated toothbrush or Z-Vibe
Build tone in the trunk and provide proximal stability by compression of spine through shoulders, bounce on lap or ball
Position in feeding chair with increased support of the trunk and feet
Feed to the sides of the mouth to improve tongue lateralization
Thicken liquids
Present flat bowl spoon in horizontal position midway and vibrate to tip (Z-Vibe)
Offer vibration with battery operated toothbrush or Z-Vibe
Слайд 17Lip retraction
Lip retraction occurs with increase muscle tone pulling/drawing the lips
and cheeks backward to form a tight horizontal mouth, making it difficult to suck from a bottle or remove food from a spoon. Lip pursing occurs when the child attempts to counteract the effects of retraction. Before each meal:
Check sitting position for too much hip extension/shoulder retraction/head extension
check for overstimulating environment and sensory properties of the food given (spicy/bland)
Midline orientation/3 point massage (cheeks, facial folds, upper lip)
Reduce hypertonicity in cheeks with vibrating hands on each cheek forward or vibrating bug/Z-vibe
Lip massage: rub infadent finger or roll cut down toothette from the R corner to midline, the L corner to midline *DO NOT CROSS MIDLINE
Facial molding with towel or flat palms move the cheeks forward and chin/lower lip upward
Straw drinking or cup drinking (with cut out cup)
Check sitting position for too much hip extension/shoulder retraction/head extension
check for overstimulating environment and sensory properties of the food given (spicy/bland)
Midline orientation/3 point massage (cheeks, facial folds, upper lip)
Reduce hypertonicity in cheeks with vibrating hands on each cheek forward or vibrating bug/Z-vibe
Lip massage: rub infadent finger or roll cut down toothette from the R corner to midline, the L corner to midline *DO NOT CROSS MIDLINE
Facial molding with towel or flat palms move the cheeks forward and chin/lower lip upward
Straw drinking or cup drinking (with cut out cup)
Слайд 18Low tone cheeks/lips
Hypotonia in the cheeks reduces the strength/skill of the
lips causing inefficient sucking and bolus collection, excessive drooling and open mouth, decreased awareness and overstuffing/food pocketing. Before each meal:
Increase tone in body with bouncing and compressions
Engage midline orientation with 3 point massage
Play patty-cake and other games to the cheeks that provide firm input to sides of the face
Lip massage: rub lips from midline out ward to sides (stretch)
Explore mouth with ice, spicy, tart/sour foods to increase pucker
“Hide” soft food/banana or cheese in cheek pockets and have child squeeze side of cheek to push food to center
Vibrate to increase awareness
Straw drinking
Three Point massage…
Increase tone in body with bouncing and compressions
Engage midline orientation with 3 point massage
Play patty-cake and other games to the cheeks that provide firm input to sides of the face
Lip massage: rub lips from midline out ward to sides (stretch)
Explore mouth with ice, spicy, tart/sour foods to increase pucker
“Hide” soft food/banana or cheese in cheek pockets and have child squeeze side of cheek to push food to center
Vibrate to increase awareness
Straw drinking
Three Point massage…
Слайд 19Straw drinking/Cup use
Use a squeeze box with short, thick straw *place
straw at corner of mouth and quickly move to midline (repeat on each side).
Use aquarium tubing in squeeze bottle
Use cork or medium bead to adjust the length of straw in the mouth. The portion that enters the mouth should be very short at first.
Use thick liquids (honey consistency) with straw or cup (ie. milkshake, applesauce, baby food)
Use cut out cup and push corner to corner to improve lip closure and decrease tone *use jaw control as needed.
*Try club soda and juice to increase awareness of liquid
Use aquarium tubing in squeeze bottle
Use cork or medium bead to adjust the length of straw in the mouth. The portion that enters the mouth should be very short at first.
Use thick liquids (honey consistency) with straw or cup (ie. milkshake, applesauce, baby food)
Use cut out cup and push corner to corner to improve lip closure and decrease tone *use jaw control as needed.
*Try club soda and juice to increase awareness of liquid
Слайд 20Incorporate solid foods in therapy
Cheetos and other junk food are good
starter foods (they melt)
Shave a carrot or potato for teething, texture, and proprioception/biting
Use veggie stix for chewing
Shave a carrot or potato for teething, texture, and proprioception/biting
Use veggie stix for chewing
Слайд 21Prevent Food Jags
Food jags are when a child will only eat
certain foods and may demand that they are presented the same way (ie.certain label food, on a stick, wrapped in paper towel)
The brain does not produce pathways to accept other foods
Steps to prevent food jags
The brain does not produce pathways to accept other foods
Steps to prevent food jags
Слайд 22
Works Cited
(2010). Retrieved September 20, 2010, from Mealtime notions llc: http://www.mealtimenotions.com
C
Drobek, C. M. (2005). Building Blocks of Pediatric Therapy. Detroit: Children's Hospital of Michigan Detroit Medical Center/Wayne State University.
Harrison, T. (1996). Feeding your 1 to 5 year old building good eating habits. Okemos, Michigan: United Dairy Council of Michigan.
K. Toomey, E. R. (2007). When Children Won't Eat The SOS Approach to Feeding. Farmington Hills, MI: Abilities Center.
Klein, S. M. (1987). Pre-Feeding Skills. Tucson: Therapy Skill Builders.
Logemann, J., (1993). Manual for the videofluorographic study of swallowing (2nd ed.) Austin, TX: Pro-Ed
Overland, L. (1996). Feeding Therapy: A Sensory Motor Approach. Talk Tools Inoovative Therapists International.
Winstock, A. (2005). Eating & Drinking Difficulties in Children. Oxen: Speechmark Publishing Ltd.
Harrison, T. (1996). Feeding your 1 to 5 year old building good eating habits. Okemos, Michigan: United Dairy Council of Michigan.
K. Toomey, E. R. (2007). When Children Won't Eat The SOS Approach to Feeding. Farmington Hills, MI: Abilities Center.
Klein, S. M. (1987). Pre-Feeding Skills. Tucson: Therapy Skill Builders.
Logemann, J., (1993). Manual for the videofluorographic study of swallowing (2nd ed.) Austin, TX: Pro-Ed
Overland, L. (1996). Feeding Therapy: A Sensory Motor Approach. Talk Tools Inoovative Therapists International.
Winstock, A. (2005). Eating & Drinking Difficulties in Children. Oxen: Speechmark Publishing Ltd.