- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
GIT disorders. (Subject 16) презентация
Содержание
- 1. GIT disorders. (Subject 16)
- 2. Gastric mucosal barrier tight cellular junctions presence
- 3. Acute gastritis Causes Diet and personal
- 4. Gastritis pathogenesis Reduced blood flow →mucosal hypo-perfusion→
- 5. Types of chronic gastritis Type A Gastritis
- 6. Types of chronic gastritis Type AB Gastritis
- 7. Peptic ulcer disease Ethiology: H pylori infection
- 8. Stress ulceration High level of glucocorticoids and
- 9. Clinical manifestations affection of one or all
- 10. Complications Hemorrhage bleeding from granulation tissue
- 11. Complications Obstruction edema, spasm or contraction
- 12. Therapy principles Eradication of Helicobacter pylori with
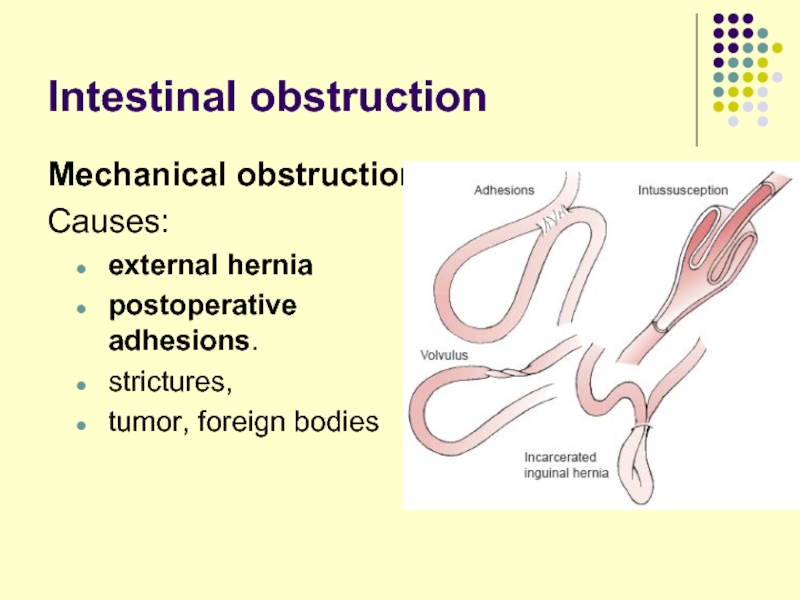
- 13. Intestinal obstruction Mechanical obstruction Causes:
- 14. Intestinal obstruction Paralytic, or adynamic, obstruction
- 15. Intestinal obstruction pathogenesis
- 16. Intestinal autointoxication poisoning of the organism
- 17. Intestinal autointoxication General symptoms ↓ ABP and
- 18. Liver pathology
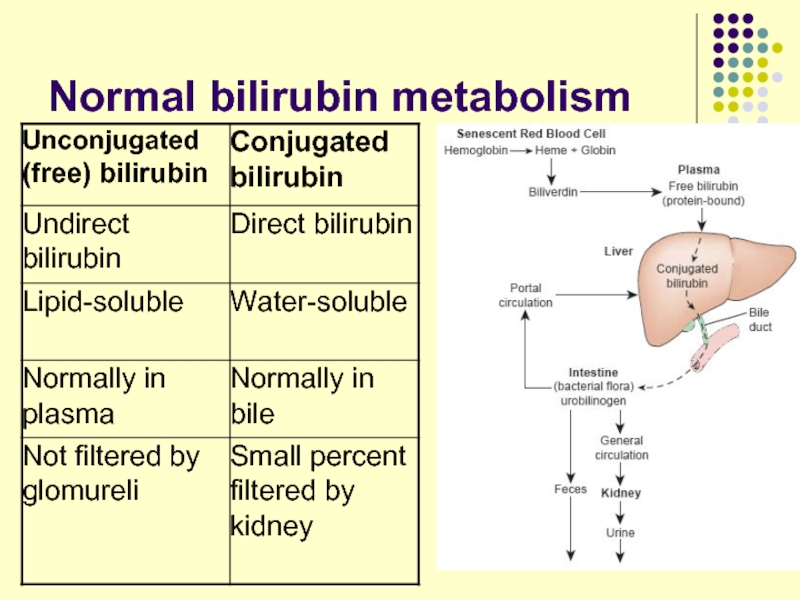
- 19. Normal bilirubin metabolism
- 20. Jaundice Yellowish discoloration of the
- 21. Prehepatic jaundice Reason - ↑ hemolysis of
- 22. Hepatic jaundice Synonym – intrahepatic or
- 23. Hepatic jaundice Hereditary disorders: ↓ bilirubin uptake
- 24. Posthepatic jaundice Synonym – mechanical, obstructive, cholestatic
- 25. Cholemia - bile in blood ↑ levels
- 26. Acholia ↓ or absence of bile
- 27. Hepatic failure severe impairment of the
- 28. Hepatic failure Hematologic Disorders. anemia due
- 29. Hepatic failure Endocrine Disorders –impaired steroid hormones
- 30. Hepatic failure Hepatic Encephalopathy Stages I -
- 31. Hepatic failure Hepatorenal Syndrome Acute liver failure→
- 32. Portal hypertension ↑ resistance to flow
- 33. Portal hypertension Intrahepatic portal hypertension: liver cirrhosis.
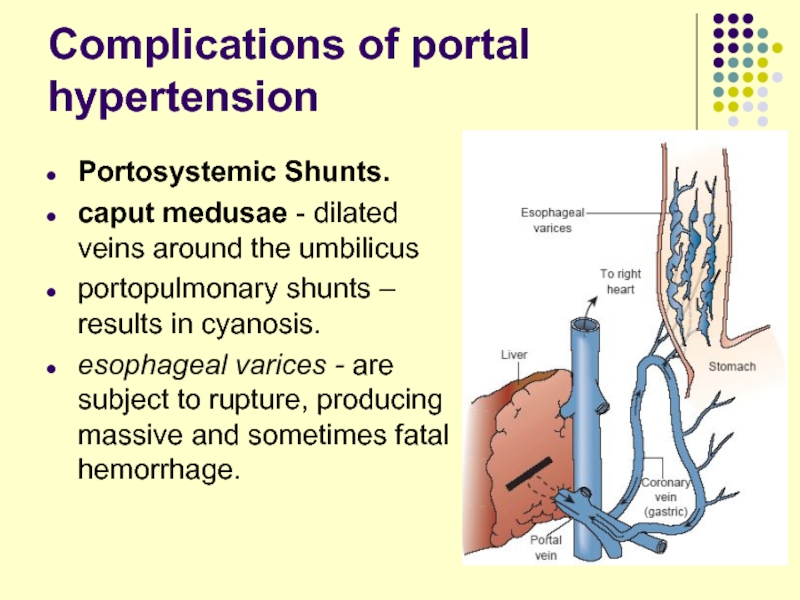
- 34. Complications of portal hypertension
- 35. Complications of portal hypertension Portosystemic Shunts.
- 36. Hepatolienal syndrome Enlargement of liver is usually
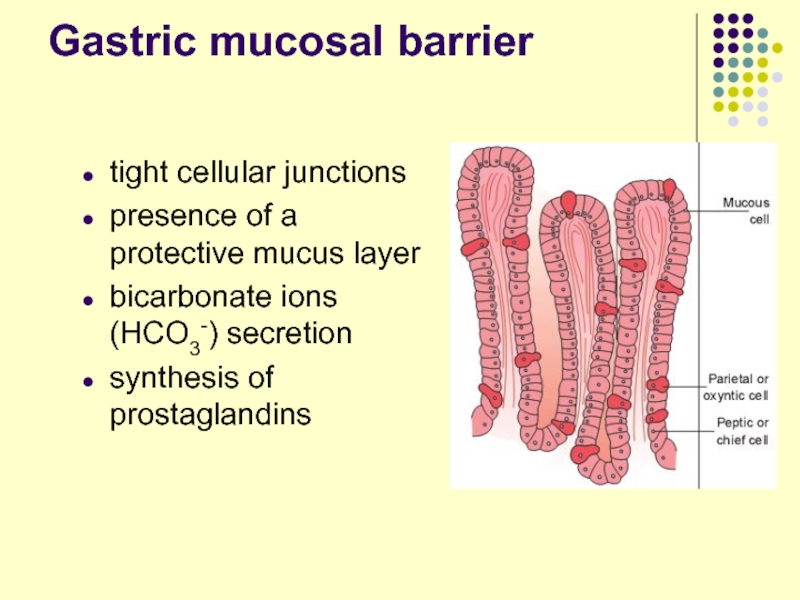
Слайд 2Gastric mucosal barrier
tight cellular junctions
presence of a protective mucus layer
bicarbonate ions
(HCO3-) secretion
synthesis of prostaglandins
synthesis of prostaglandins
Слайд 3Acute gastritis
Causes
Diet and personal habits (excessive alcohol, smoking, malnutrition).
Infections:
bacterial
- Helicobacter pylori, diphtheria, salmonellosis, staphylococcal food poisoning;
viral - viral hepatitis, influenza.
Drugs (NSAIDs, cortisone).
Chemical and physical agents.
Severe stress.
viral - viral hepatitis, influenza.
Drugs (NSAIDs, cortisone).
Chemical and physical agents.
Severe stress.
Слайд 4Gastritis pathogenesis
Reduced blood flow →mucosal hypo-perfusion→ ischemia.
Increased acid secretion (in H.pylori
infection)→ damage to epithelial barrier.
Decreased production of bicarbonates.
Decreased production of bicarbonates.
Слайд 5Types of chronic gastritis
Type A Gastritis (Autoimmune gastritis).
antibodies against parietal
cells and intrinsic factor.
other autoimmune diseases .
gastric atrophy
hypo- or achlorhydria.
Type B Gastritis (Helicobacter pylori-related).
excessive secretion of acid (hypersecretory gastritis)
associated peptic ulcer
other autoimmune diseases .
gastric atrophy
hypo- or achlorhydria.
Type B Gastritis (Helicobacter pylori-related).
excessive secretion of acid (hypersecretory gastritis)
associated peptic ulcer
Слайд 6Types of chronic gastritis
Type AB Gastritis (environmental)
gastric atrophy
caused by environmental factors.
Type
C Gastritis (Chemical)
due to reflux of alkaline duodenal contents, pancreatic secretions, and bile into the stomach.
in persons after GIT surgery, with gastric ulcer, gallbladder diseases.
due to reflux of alkaline duodenal contents, pancreatic secretions, and bile into the stomach.
in persons after GIT surgery, with gastric ulcer, gallbladder diseases.
Слайд 7Peptic ulcer disease
Ethiology:
H pylori infection
NSAIDs (aspirin - the most ulcerogenic)
Lifestyle factors
Severe
physiologic stress
Genetic factors (hereditary predisposition)
Genetic factors (hereditary predisposition)
Слайд 8Stress ulceration
High level of glucocorticoids and adrenaline (stress hormones) causes:
↓ mucus
secretion (glucocorticoids)
↓ regeneration of gastric epithelial cells (glucocorticoids)
↓ microcirculation and ischemia of mucosal tunic (glucocorticoids, adrenaline)
other reasons of ischemia (collapse, shock, acute blood loss, spasm of blood vessels)
↑ tonus of the vagal nerve → ↑ HCl and pepsin secretion.
↓ regeneration of gastric epithelial cells (glucocorticoids)
↓ microcirculation and ischemia of mucosal tunic (glucocorticoids, adrenaline)
other reasons of ischemia (collapse, shock, acute blood loss, spasm of blood vessels)
↑ tonus of the vagal nerve → ↑ HCl and pepsin secretion.
Слайд 9Clinical manifestations
affection of one or all layers of stomach
remissions and exacerbation
healing with scar formation
stomach discomfort and pain.
periodicity of pain (on empty stomach).
recurrence of pain.
pain is relieved by food or antacids.
Слайд 10Complications
Hemorrhage
bleeding from granulation tissue
erosion of an ulcer into an
artery or vein
Hematemesis or melena.
Acute hemorrhage – signs of circulatory shock depending on the amount of blood loss.
Hematemesis or melena.
Acute hemorrhage – signs of circulatory shock depending on the amount of blood loss.
Слайд 11Complications
Obstruction
edema, spasm or contraction of scar.
epigastric fullness, vomiting of
undigested food.
Perforation
GI contents enter the peritoneum (peritonitis),
ulcer penetrate adjacent structures (pancreas),
severe pain radiating into the back.
Perforation
GI contents enter the peritoneum (peritonitis),
ulcer penetrate adjacent structures (pancreas),
severe pain radiating into the back.
Слайд 12Therapy principles
Eradication of Helicobacter pylori with antibiotics
Inhibition of gastric secretion
H2
histamine receptor antagonists (cimetidine, ranitidine)
Prostaglandin E1 analogues (misoprostol)
Surgical management
highly selective vagotomy in order to inhibit gastric secretion
Prostaglandin E1 analogues (misoprostol)
Surgical management
highly selective vagotomy in order to inhibit gastric secretion
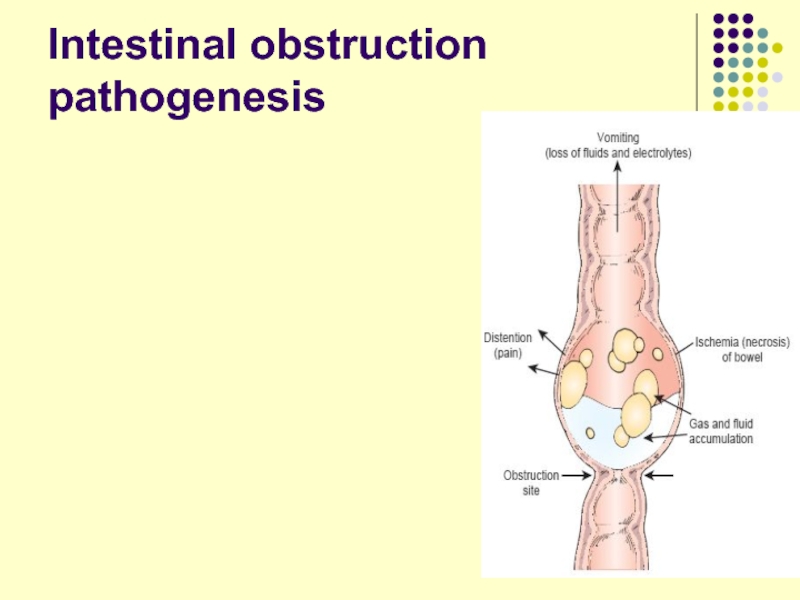
Слайд 13Intestinal obstruction
Mechanical obstruction
Causes:
external hernia
postoperative adhesions.
strictures,
tumor, foreign bodies
Слайд 14Intestinal obstruction
Paralytic, or adynamic, obstruction
after abdominal surgery
inflammatory conditions of
the abdomen,
pelvic and back injuries.
chemical irritation (bile, bacterial toxins, electrolyte imbalances).
pelvic and back injuries.
chemical irritation (bile, bacterial toxins, electrolyte imbalances).
Слайд 16Intestinal autointoxication
poisoning of the organism by toxic substances from the
bowels.
The causes and mechanisms:
↑ formation of the toxic substances - skatole, cresol, indole, phenol.
↑ permeability of the intestinal wall - inflammation and distension of bowels.
Hepatic failure due to the decrease of the liver detoxication activity.
The causes and mechanisms:
↑ formation of the toxic substances - skatole, cresol, indole, phenol.
↑ permeability of the intestinal wall - inflammation and distension of bowels.
Hepatic failure due to the decrease of the liver detoxication activity.
Слайд 17Intestinal autointoxication
General symptoms
↓ ABP and pain sensitivity,
↓ glycogen amount in the
liver, hyperglycaemia,
myocardial dystrophy
respiratory depression,
headaches, brain activity inhibition up to coma
↓ appetite, violation of digestion, anemia.
myocardial dystrophy
respiratory depression,
headaches, brain activity inhibition up to coma
↓ appetite, violation of digestion, anemia.
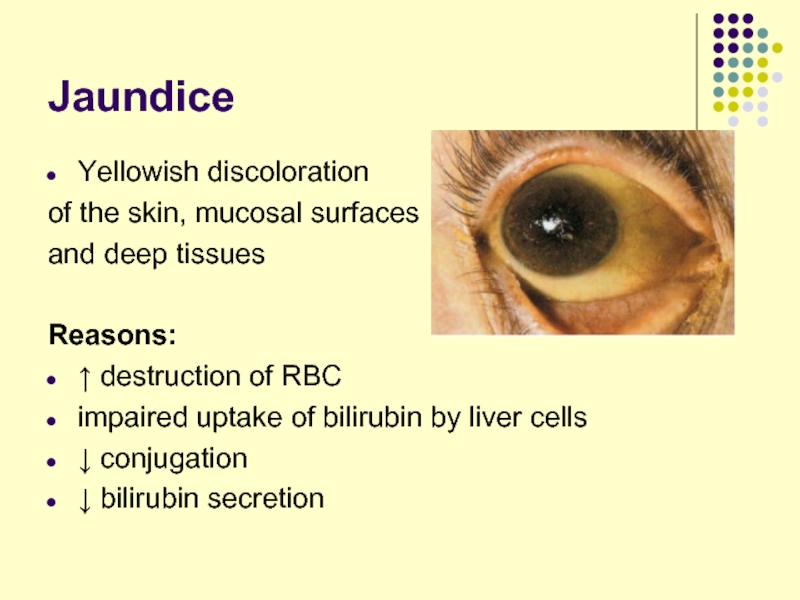
Слайд 20Jaundice
Yellowish discoloration
of the skin, mucosal surfaces
and deep tissues
Reasons:
↑ destruction of RBC
impaired uptake of bilirubin by liver cells
↓ conjugation
↓ bilirubin secretion
Слайд 21Prehepatic jaundice
Reason - ↑ hemolysis of red blood cells:
Hemolytic blood
transfusion reaction
Hereditary and acquired hemolytic anemias
Neonatal jaundice (physiologic jaundice)
Blood - unconjugated bilirubin ↑
Urine – urobiline normal or ↑
Faeces – stercobiline ↑
Hereditary and acquired hemolytic anemias
Neonatal jaundice (physiologic jaundice)
Blood - unconjugated bilirubin ↑
Urine – urobiline normal or ↑
Faeces – stercobiline ↑
Слайд 22Hepatic jaundice
Synonym – intrahepatic or hepatocellular jaundice
Hepatitis, cirrhosis, cancer of
the liver.
↓ bilirubin uptake, conjugation, excretion
Blood - unconjugated bilirubin ↑, conjugated bilirubin ↑
Urine – urobilin normal or ↓, bilirubin ↑
Faeces – stercobiline normal or ↓
↓ bilirubin uptake, conjugation, excretion
Blood - unconjugated bilirubin ↑, conjugated bilirubin ↑
Urine – urobilin normal or ↓, bilirubin ↑
Faeces – stercobiline normal or ↓
Слайд 23Hepatic jaundice
Hereditary disorders:
↓ bilirubin uptake (Gilbert’s syndrome);
↓ of enzymes supporting conjugation
(Crigler-Najjar syndrome);
↓ bilirubin excretion (Dubin-Johnson syndrome).
↓ bilirubin excretion (Dubin-Johnson syndrome).
Слайд 24Posthepatic jaundice
Synonym – mechanical, obstructive, cholestatic jaundice
Reasons – obstruction of bile
flow between the liver and the intestine
Structural disorders of the bile duct
Cholelithiasis
Tumors in the bile duct
Blood - conjugated bilirubin ↑ , bile salts, cholesterol
Urine – urobilin absent, bilirubin ↑
Faeces – stercobiline absent
Structural disorders of the bile duct
Cholelithiasis
Tumors in the bile duct
Blood - conjugated bilirubin ↑ , bile salts, cholesterol
Urine – urobilin absent, bilirubin ↑
Faeces – stercobiline absent
Слайд 25Cholemia - bile in blood
↑ levels of cholesterol, bile acids and
bilirubin
Clinical signs of cholemia:
Urine dark color.
Xanthomas formation (due to excess of cholesterol)
Skin itching (pruritis)
Arterial hypotension
Bradycardia
↑ irritability and excitability of the patient
Depression, insomnia, increased fatigueability
Multiply subcutaneous hemorrhages
Clinical signs of cholemia:
Urine dark color.
Xanthomas formation (due to excess of cholesterol)
Skin itching (pruritis)
Arterial hypotension
Bradycardia
↑ irritability and excitability of the patient
Depression, insomnia, increased fatigueability
Multiply subcutaneous hemorrhages
Слайд 26Acholia
↓ or absence of bile secretion into the intestines
Clinical
signs of acholia:
steatorrhea - fat, clay colored stools
intestinal autointoxication and disbacteriosis development
deficiency of fat soluble vitamins (A,D,E,K)
steatorrhea - fat, clay colored stools
intestinal autointoxication and disbacteriosis development
deficiency of fat soluble vitamins (A,D,E,K)
Слайд 27Hepatic failure
severe impairment of the liver functions
Acute failure (fulminant hepatitis)
Chronic
failure (alcoholic liver cirrhosis)
Clinical signs
Fetor hepaticus - musty, sweetish odor of the breath in the patient with liver failure.
Clinical signs
Fetor hepaticus - musty, sweetish odor of the breath in the patient with liver failure.
Слайд 28Hepatic failure
Hematologic Disorders.
anemia due to
blood loss,
excessive destruction or
impaired formation of RBC,
folic acid deficiency
leukopenia, thrombocytopenia due to excessive destruction as the result of splenomegaly,
coagulation defects due to ↓ protein synthesis by the liver, vitamin K deficiency
folic acid deficiency
leukopenia, thrombocytopenia due to excessive destruction as the result of splenomegaly,
coagulation defects due to ↓ protein synthesis by the liver, vitamin K deficiency
Слайд 29Hepatic failure
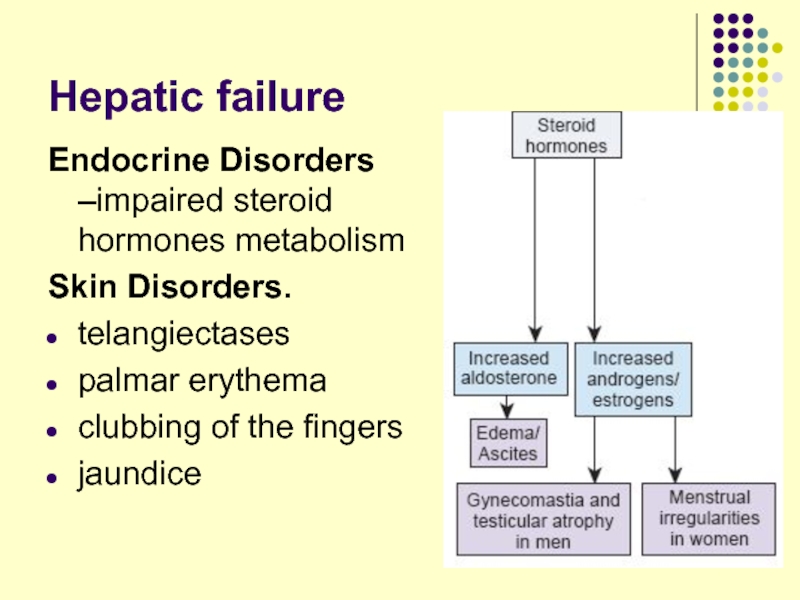
Endocrine Disorders –impaired steroid hormones metabolism
Skin Disorders.
telangiectases
palmar erythema
clubbing
of the fingers
jaundice
jaundice
Слайд 30Hepatic failure
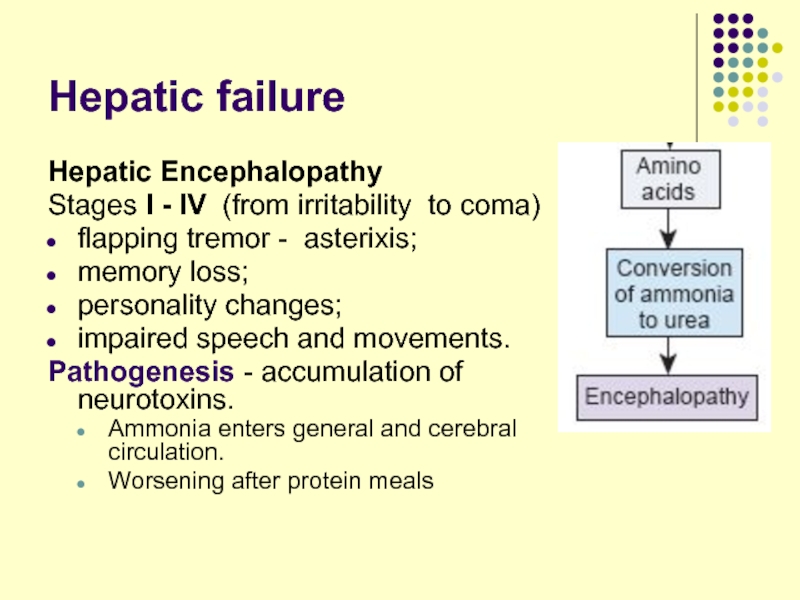
Hepatic Encephalopathy
Stages I - IV (from irritability to coma)
flapping
tremor - asterixis;
memory loss;
personality changes;
impaired speech and movements.
Pathogenesis - accumulation of neurotoxins.
Ammonia enters general and cerebral circulation.
Worsening after protein meals
memory loss;
personality changes;
impaired speech and movements.
Pathogenesis - accumulation of neurotoxins.
Ammonia enters general and cerebral circulation.
Worsening after protein meals
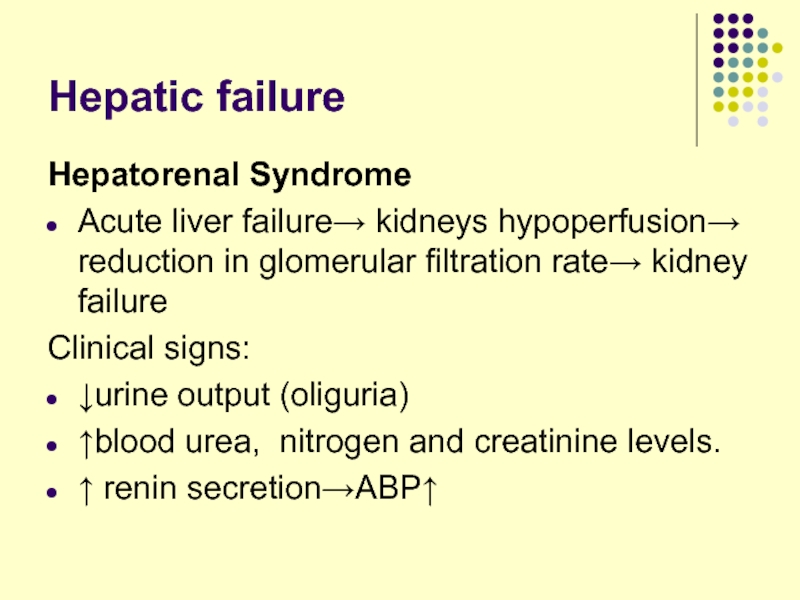
Слайд 31Hepatic failure
Hepatorenal Syndrome
Acute liver failure→ kidneys hypoperfusion→ reduction in glomerular filtration
rate→ kidney failure
Clinical signs:
↓urine output (oliguria)
↑blood urea, nitrogen and creatinine levels.
↑ renin secretion→ABP↑
Clinical signs:
↓urine output (oliguria)
↑blood urea, nitrogen and creatinine levels.
↑ renin secretion→ABP↑
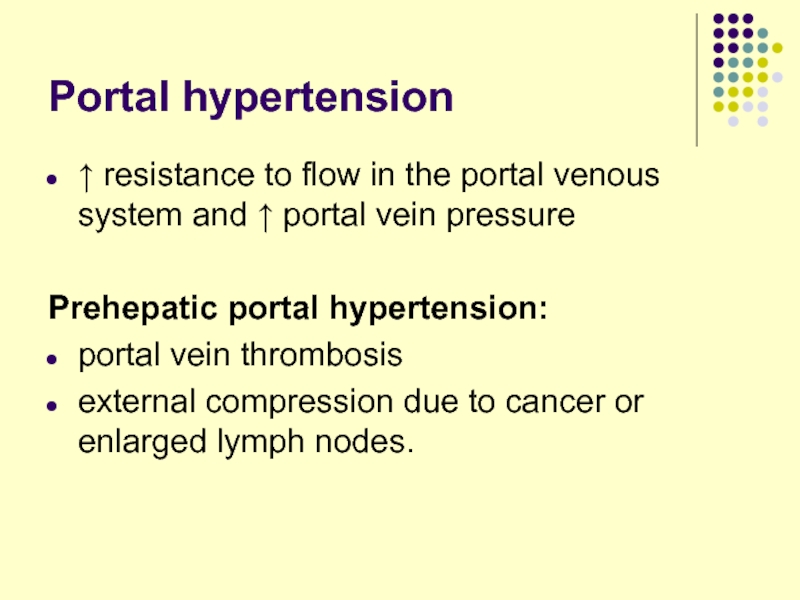
Слайд 32Portal hypertension
↑ resistance to flow in the portal venous system
and ↑ portal vein pressure
Prehepatic portal hypertension:
portal vein thrombosis
external compression due to cancer or enlarged lymph nodes.
Prehepatic portal hypertension:
portal vein thrombosis
external compression due to cancer or enlarged lymph nodes.
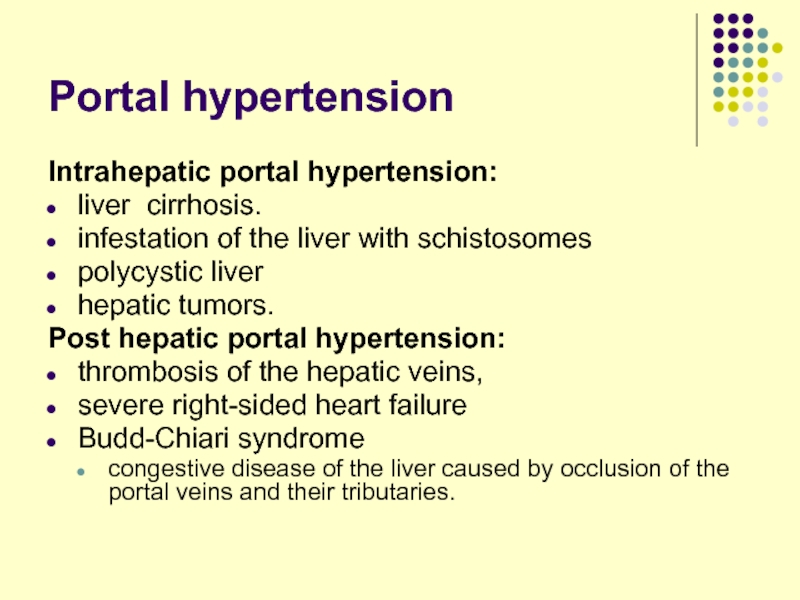
Слайд 33Portal hypertension
Intrahepatic portal hypertension:
liver cirrhosis.
infestation of the liver with schistosomes
polycystic
liver
hepatic tumors.
Post hepatic portal hypertension:
thrombosis of the hepatic veins,
severe right-sided heart failure
Budd-Chiari syndrome
congestive disease of the liver caused by occlusion of the portal veins and their tributaries.
hepatic tumors.
Post hepatic portal hypertension:
thrombosis of the hepatic veins,
severe right-sided heart failure
Budd-Chiari syndrome
congestive disease of the liver caused by occlusion of the portal veins and their tributaries.
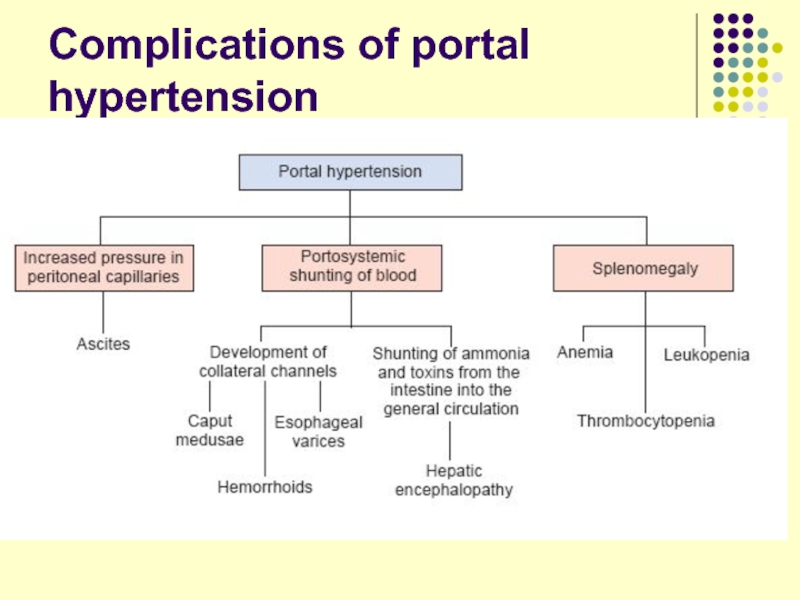
Слайд 35Complications of portal hypertension
Portosystemic Shunts.
caput medusae - dilated veins around
the umbilicus
portopulmonary shunts – results in cyanosis.
esophageal varices - are subject to rupture, producing massive and sometimes fatal hemorrhage.
portopulmonary shunts – results in cyanosis.
esophageal varices - are subject to rupture, producing massive and sometimes fatal hemorrhage.
Слайд 36Hepatolienal syndrome
Enlargement of liver is usually combined with the enlargement of
spleen due to:
common vein system
common innnervation
common lymphatic
common vein system
common innnervation
common lymphatic