- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Tumors of genitourinary organs презентация
Содержание
- 1. Tumors of genitourinary organs
- 2. Tumors of the kidney
- 3. Tumors of the kidney The most common
- 4. Tumors of the kidney The tumors of
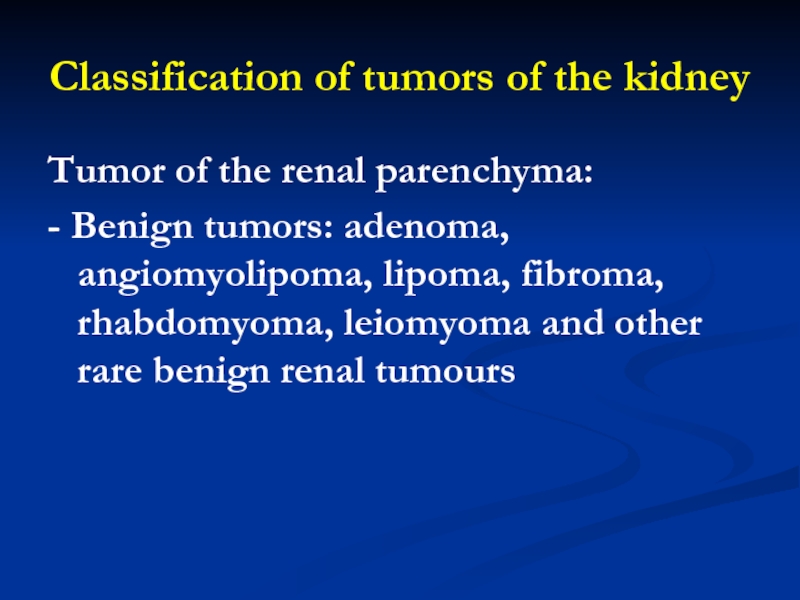
- 5. Classification of tumors of the kidney Tumor
- 6. Classification of malignant tumors of the kidney
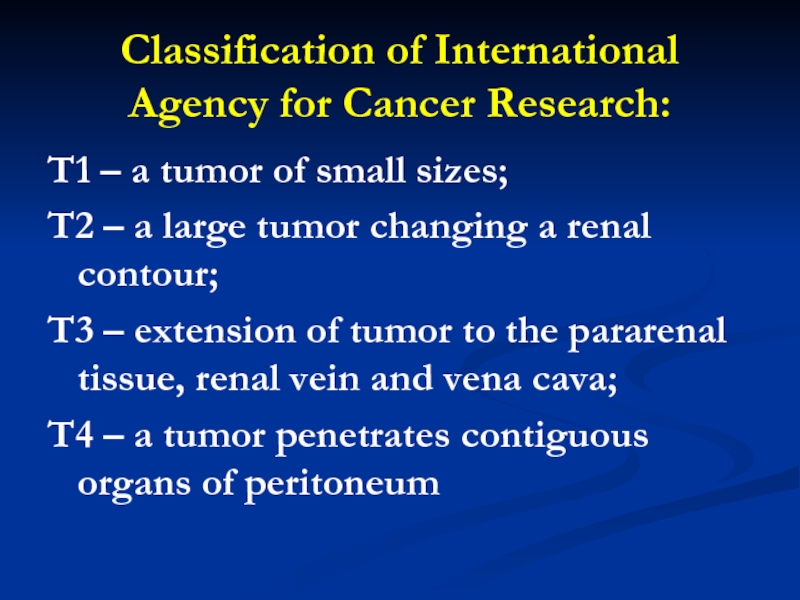
- 7. Classification of International Agency for Cancer Research:
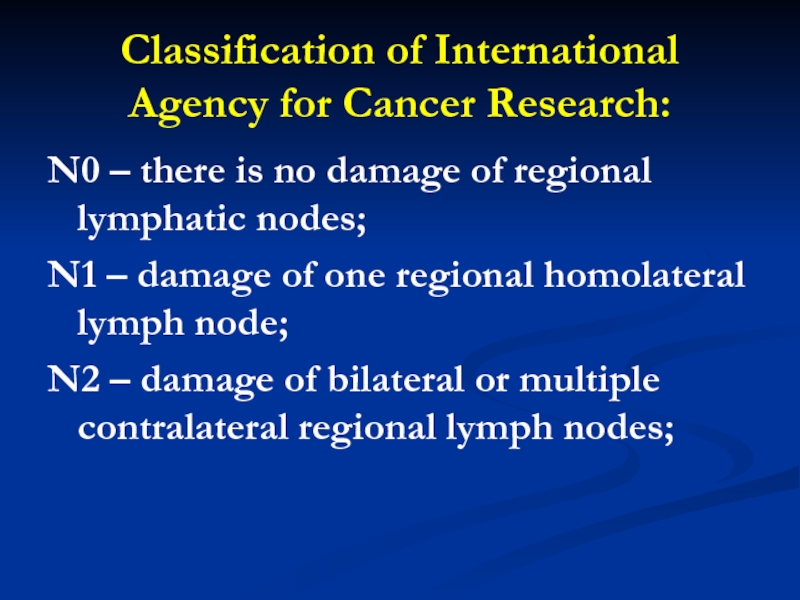
- 8. Classification of International Agency for Cancer Research:
- 9. Classification of International Agency for Cancer Research:
- 10. Classification of International Agency for Cancer Research:
- 11. Benign Tumors of the kidney Adenoma of
- 12. Benign Tumors of the kidney Oncocytomas
- 13. Benign Tumors of the kidney Angiomyolipomas.
- 14. Malignant Tumors Renal Cell Carcinoma (Hypernephroma, Renal Adenocarcinoma)
- 15. Wilms’ Tumor Wilms’ Tumor is nephroblastoma of
- 16. Tumors of the Urinary Bladder Tumors of
- 17. Tumors of the Urinary Bladder According to
- 18. Classification is valid only while observing the
- 19. Bening Prostatic Hyperplasia Until recently benign prostatic
- 20. Bening Prostatic Hyperplasia The prostate gland is
- 21. Bening Prostatic Hyperplasia The posterior surface of
- 22. Bening Prostatic Hyperplasia The normal prostate measures
- 23. Bening Prostatic Hyperplasia Incidence & Epidemiology
- 24. Bening Prostatic Hyperplasia BPH is the most
- 25. Bening Prostatic Hyperplasia At age 55, approximately 25% of men report obstructive voiding symptoms.
- 26. Bening Prostatic Hyperplasia Risk factors for the development of BPH are poorly understood.
- 27. Bening Prostatic Hyperplasia Etiology
- 28. Bening Prostatic Hyperplasia The etiology of BPH
- 29. Bening Prostatic Hyperplasia Observations and clinical studies
- 30. Bening Prostatic Hyperplasia The latter may suggest
- 31. Bening Prostatic Hyperplasia Symptoms
- 32. Bening Prostatic Hyperplasia As discussed above, the
- 33. Bening Prostatic Hyperplasia A detailed history focusing
- 34. Bening Prostatic Hyperplasia Signs
- 35. Bening Prostatic Hyperplasia A physical examination, DRE,
- 36. Bening Prostatic Hyperplasia Laboratory Findings
- 37. Bening Prostatic Hyperplasia A urinalysis to exclude
- 38. Bening Prostatic Hyperplasia Serum PSA is considered
- 39. Bening Prostatic Hyperplasia Imaging
- 40. Bening Prostatic Hyperplasia Upper-tract imaging (intravenous pyelogram
- 41. Bening Prostatic Hyperplasia Cystoscopy is not recommended
- 42. Bening Prostatic Hyperplasia Cystometrograms and urodynamic profiles
- 43. Bening Prostatic Hyperplasia Differential Diagnosis
- 44. Bening Prostatic Hyperplasia Other obstructive conditions of
- 45. Bening Prostatic Hyperplasia A urinary tract infection,
- 46. Bening Prostatic Hyperplasia Likewise, patients with neurogenic
- 47. Bening Prostatic Hyperplasia Treatment
- 48. Bening Prostatic Hyperplasia After patients have been
- 49. Bening Prostatic Hyperplasia Specific treatment recommendations can
- 50. Bening Prostatic Hyperplasia Watchful Waiting
- 51. Bening Prostatic Hyperplasia Very few studies on
- 52. Bening Prostatic Hyperplasia Retrospective studies on the
- 53. Bening Prostatic Hyperplasia As mentioned above, watchful
- 54. Bening Prostatic Hyperplasia Medical Therapy Alpha Blockers
- 55. Bening Prostatic Hyperplasia The human prostate and
- 56. Bening Prostatic Hyperplasia 5 α -Reductase Inhibitors
- 57. Bening Prostatic Hyperplasia Finasteride is a 5
- 58. Bening Prostatic Hyperplasia Several randomized, double-blind, placebo-controlled trials have compared finasteride with placebo.
- 59. Bening Prostatic Hyperplasia However, optimal identification of
- 60. Bening Prostatic Hyperplasia Phytotherapy refers to the
- 61. Bening Prostatic Hyperplasia Conventional Surgical Therapy Transurethral Resection of the Prostate (TURP)
- 62. Bening Prostatic Hyperplasia Ninety-five percent of simple prostatectomies can be done endoscopically.
- 63. Bening Prostatic Hyperplasia Much controversy revolves around
- 64. Bening Prostatic Hyperplasia Several other studies could
- 65. Bening Prostatic Hyperplasia Clinical manifestations of the
- 66. Bening Prostatic Hyperplasia Men with moderate to
- 67. Bening Prostatic Hyperplasia Outcomes in well-selected patients
- 68. Bening Prostatic Hyperplasia Open Simple Prostatectomy When
- 69. Bening Prostatic Hyperplasia Open prostatectomy may also
- 70. Bening Prostatic Hyperplasia Open prostatectomies can be done with either a suprapubic or retropubic approach.
- 71. Bening Prostatic Hyperplasia The dissection plane is
- 72. Bening Prostatic Hyperplasia In a simple retropubic prostatectomy, the bladder is not entered.
- 73. Bening Prostatic Hyperplasia Minimally Invasive Therapy Laser
- 74. Bening Prostatic Hyperplasia Several different coagulation necrosis techniques have been described.
- 75. Bening Prostatic Hyperplasia Transurethral Electrovaporization of the
- 76. Bening Prostatic Hyperplasia Hyperthermia Microwave hyperthermia is most commonly delivered with a transurethral catheter.
- 77. Bening Prostatic Hyperplasia Transurethral Needle Ablation of
- 78. Bening Prostatic Hyperplasia This technique is not
- 79. Bening Prostatic Hyperplasia High-Intensity Focused Ultrasound
- 80. Bening Prostatic Hyperplasia This probe allows transrectal
- 81. Bening Prostatic Hyperplasia Intraurethral Stents
- 82. Bening Prostatic Hyperplasia These devices are typically
- 83. Bening Prostatic Hyperplasia Transurethral Balloon Dilation of
- 84. Carcinoma of the Prostate (CaP) Incidence & Epidemiology
- 85. Carcinoma of the Prostate (CaP) Prostate cancer
- 86. Carcinoma of the Prostate (CaP) The lifetime
- 87. Carcinoma of the Prostate (CaP) Thus,
- 88. Carcinoma of the Prostate (CaP) Several risk
- 89. Carcinoma of the Prostate (CaP) African Americans
- 90. Carcinoma of the Prostate (CaP) The age
- 91. Carcinoma of the Prostate (CaP) High dietary
- 92. Carcinoma of the Prostate (CaP) Etiology The
- 93. Carcinoma of the Prostate (CaP) Pathology Over
- 94. Carcinoma of the Prostate (CaP) Symptoms Most
- 95. Carcinoma of the Prostate (CaP) Metastatic disease to the bones may cause bone pain.
- 96. Carcinoma of the Prostate (CaP) Signs A physical examination, including a DRE, is needed.
- 97. Carcinoma of the Prostate (CaP) Locally advanced
- 98. Carcinoma of the Prostate (CaP) Laboratory Findings
- 99. Carcinoma of the Prostate (CaP) Tumor Markers—Prostate-Specific
- 100. Carcinoma of the Prostate (CaP) Prostate Biopsy
- 101. Carcinoma of the Prostate (CaP) Information from
- 102. Carcinoma of the Prostate (CaP) TRUS TRUS
- 103. Carcinoma of the Prostate (CaP) TRUS provides
- 104. Carcinoma of the Prostate (CaP) Endorectal Magnetic
- 105. Carcinoma of the Prostate (CaP) Differential Diagnosis
- 106. Carcinoma of the Prostate (CaP) Sclerotic lesions
- 107. Carcinoma of the Prostate (CaP) Treatment Localized
- 108. Carcinoma of the Prostate (CaP) Treatment dilemmas
- 109. Carcinoma of the Prostate (CaP) Watchful Waiting
- 110. Carcinoma of the Prostate (CaP) In addition,
- 111. Carcinoma of the Prostate (CaP) Radical Prostatectomy
- 112. Carcinoma of the Prostate (CaP) Description of
Слайд 3Tumors of the kidney
The most common kind of tumor of the
kidney is cancer of the renal parenchyma.
Слайд 4Tumors of the kidney
The tumors of the kidney in adults make
up 2-3% of the number of all neoplasm. Men suffer more often than woman.
Слайд 5Classification of tumors of the kidney
Tumor of the renal parenchyma:
- Benign
tumors: adenoma, angiomyolipoma, lipoma, fibroma, rhabdomyoma, leiomyoma and other rare benign renal tumours
Слайд 6Classification of malignant tumors of the kidney in stages:
Tumor within the
limits of renal capsule
Слайд 7Classification of International Agency for Cancer Research:
T1 – a tumor of
small sizes;
T2 – a large tumor changing a renal contour;
T3 – extension of tumor to the pararenal tissue, renal vein and vena cava;
T4 – a tumor penetrates contiguous organs of peritoneum
T2 – a large tumor changing a renal contour;
T3 – extension of tumor to the pararenal tissue, renal vein and vena cava;
T4 – a tumor penetrates contiguous organs of peritoneum
Слайд 8Classification of International Agency for Cancer Research:
N0 – there is no
damage of regional lymphatic nodes;
N1 – damage of one regional homolateral lymph node;
N2 – damage of bilateral or multiple contralateral regional lymph nodes;
N1 – damage of one regional homolateral lymph node;
N2 – damage of bilateral or multiple contralateral regional lymph nodes;
Слайд 9Classification of International Agency for Cancer Research:
N3 – not dislodged metastatic
regional lymph nodes;
N4 – damage of juxtaregional lymph nodes;
Nx – minimum requirements for recognition of a state estimation of regional lymph nodes are not fullfilled;
N4 – damage of juxtaregional lymph nodes;
Nx – minimum requirements for recognition of a state estimation of regional lymph nodes are not fullfilled;
Слайд 10Classification of International Agency for Cancer Research:
M0 – absence
of the distant metastates;
M1 – presence of the distant metastases;
M x – minimum requirements for recognition of the distant metastases are not fulfilled
M1 – presence of the distant metastases;
M x – minimum requirements for recognition of the distant metastases are not fulfilled
Слайд 11Benign Tumors of the kidney
Adenoma of the cortex of the kidney
is a small dense tumor. Adenomas almost always proceed asymptomatically, they are found out accidentally, frequently they are multiple.
Слайд 12Benign Tumors of the kidney
Oncocytomas
are spherical, distinctly limited formations that
may contain radial cicatrix posed in the center.
Слайд 13Benign Tumors of the kidney
Angiomyolipomas.
These tumors consist of blood vessels,
muscular elements and fatty tissues. They arise more often and develop almost exclusively in adult women.
Слайд 15Wilms’ Tumor
Wilms’ Tumor is nephroblastoma of the kidney. The tumor is
named in honour of Max Wilms, who gave its description in 1899.
Слайд 16Tumors of the Urinary Bladder
Tumors of the urinary bladder make up
about 4% of all neoplasms or 70% of all tumors of the urinary tract, yielding in frequency only to tumors of the stomach, esophagus, lungs and larynx.
Слайд 17Tumors of the Urinary Bladder
According to the world statistics, frequency of
this disease increases. 80% of cases occur in patients at the age over 50.
Слайд 18Classification is valid only while observing the following conditions: It is applied
only to cancer and not used in case of papilloma.
Слайд 19Bening Prostatic Hyperplasia
Until recently benign prostatic hyperpasia was considered as rather
age and hormone dependent surgical disease. It was known, that for its development, as a minimum, two conditions are necessary.
Слайд 20Bening Prostatic Hyperplasia
The prostate gland is the male organ most commonly
afflicted with either benign or malignant neoplasms.
Слайд 21Bening Prostatic Hyperplasia
The posterior surface of the prostate is separated from
the rectal ampulla by Denonvilliers' fascia.
Слайд 22Bening Prostatic Hyperplasia
The normal prostate measures 3–4 cm at the base,
4–6 cm in cephalocaudad, and 2–3 cm in anteroposterior dimensions.
Слайд 24Bening Prostatic Hyperplasia
BPH is the most common benign tumor in men,
and its incidence is age-related.
Слайд 25Bening Prostatic Hyperplasia
At age 55, approximately 25% of men report obstructive
voiding symptoms.
Слайд 28Bening Prostatic Hyperplasia
The etiology of BPH is not completely understood, but
it seems to be multifactorial and endocrine controlled.
Слайд 29Bening Prostatic Hyperplasia
Observations and clinical studies in men have clearly demonstrated
that BPH is under endocrine control.
Слайд 30Bening Prostatic Hyperplasia
The latter may suggest that the association between aging
and BPH might result from the increased estrogen levels of aging causing induction of the androgen receptor, which thereby sensitizes the prostate to free testosterone.
Слайд 32Bening Prostatic Hyperplasia
As discussed above, the symptoms of BPH can be
divided into obstructive and irritative complaints.
Слайд 33Bening Prostatic Hyperplasia
A detailed history focusing on the urinary tract excludes
other possible causes of symptoms that may not result from the prostate, such as urinary tract infection, neurogenic bladder, urethral stricture, or prostate cancer.
Слайд 35Bening Prostatic Hyperplasia
A physical examination, DRE, and focused neurologic examination are
performed on all patients.
Слайд 37Bening Prostatic Hyperplasia
A urinalysis to exclude infection or hematuria and serum
creatinine measurement to assess renal function are required.
Слайд 38Bening Prostatic Hyperplasia
Serum PSA is considered optional, but most physicians will
include it in the initial evaluation.
Слайд 40Bening Prostatic Hyperplasia
Upper-tract imaging (intravenous pyelogram or renal ultrasound) is recommended
only in the presence of concomitant urinary tract disease or complications from BPH (e.g., hematuria, urinary tract infection, renal insufficiency, history of stone disease).
Слайд 41Bening Prostatic Hyperplasia
Cystoscopy is not recommended to determine the need for
treatment but may assist in choosing the surgical approach in patients opting for invasive therapy.
Слайд 42Bening Prostatic Hyperplasia
Cystometrograms and urodynamic profiles are reserved for patients with
suspected neurologic disease or those who have failed prostate surgery.
Слайд 44Bening Prostatic Hyperplasia
Other obstructive conditions of the lower urinary tract, such
as urethral stricture, bladder neck contracture, bladder stone, or CaP, must be entertained when evaluating men with presumptive BPH.
Слайд 45Bening Prostatic Hyperplasia
A urinary tract infection, which can mimic the irritative
symptoms of BPH, can be readily identified by urinalysis and culture; however, a urinary tract infection can also be a complication of BPH.
Слайд 46Bening Prostatic Hyperplasia
Likewise, patients with neurogenic bladder disorders may have many
of the signs and symptoms of BPH, but a history of neurologic disease, stroke, diabetes mellitus, or back injury may be present as well.
Слайд 48Bening Prostatic Hyperplasia
After patients have been evaluated, they should be informed
of the various therapeutic options for BPH. It is advisable for patients to consult with their physicians to make an educated decision on the basis of the relative efficacy and side effects of the treatment options.
Слайд 49Bening Prostatic Hyperplasia
Specific treatment recommendations can be offered for certain groups
of patients. For those with mild symptoms (symptom score 0–7), watchful waiting only is advised.
Слайд 51Bening Prostatic Hyperplasia
Very few studies on the natural history of BPH
have been reported.
Слайд 52Bening Prostatic Hyperplasia
Retrospective studies on the natural history of BPH are
inherently subject to bias, related to patient selection and the type and extent of follow-up.
Слайд 53Bening Prostatic Hyperplasia
As mentioned above, watchful waiting is the appropriate management
of men with mild symptom scores (0–7).
Men with moderate or severe symptoms can also be managed in this fashion if they so choose.
Neither the optimal interval for follow-up nor specific endpoints for intervention have been defined.
Men with moderate or severe symptoms can also be managed in this fashion if they so choose.
Neither the optimal interval for follow-up nor specific endpoints for intervention have been defined.
Слайд 55Bening Prostatic Hyperplasia
The human prostate and bladder base contains alpha-1-adrenoreceptors, and
the prostate shows a contractile response to corresponding agonists.
Слайд 57Bening Prostatic Hyperplasia
Finasteride is a 5 α -reductase inhibitor that blocks
the conversion of testosterone to dihydrotestosterone.
Слайд 58Bening Prostatic Hyperplasia
Several randomized, double-blind, placebo-controlled trials have compared finasteride with
placebo.
Слайд 59Bening Prostatic Hyperplasia
However, optimal identification of appropriate patients for prophylactic therapy
remains to be determined.
Слайд 60Bening Prostatic Hyperplasia
Phytotherapy refers to the use of plants or plant
extracts for medicinal purposes.
Слайд 61Bening Prostatic Hyperplasia
Conventional Surgical Therapy
Transurethral Resection of the Prostate (TURP)
Слайд 62Bening Prostatic Hyperplasia
Ninety-five percent of simple prostatectomies can be done endoscopically.
Слайд 63Bening Prostatic Hyperplasia
Much controversy revolves around possible higher rates of morbidity
and mortality associated with TURP in comparison with those of open surgery, but the higher rates observed in one study were probably related to more significant comorbidities in the TURP patients than in the patients undergoing open surgery.
Слайд 64Bening Prostatic Hyperplasia
Several other studies could not confirm the difference in
mortality when results were controlled for age and comorbidities.
Слайд 65Bening Prostatic Hyperplasia
Clinical manifestations of the TUR syndrome include nausea, vomiting,
confusion, hypertension, bradycardia, and visual disturbances.
Слайд 66Bening Prostatic Hyperplasia
Men with moderate to severe symptoms and a small
prostate often have posterior commissure hyperplasia (elevated bladder neck).
Слайд 67Bening Prostatic Hyperplasia
Outcomes in well-selected patients are comparable, although a lower
rate of retrograde ejaculation with transurethral incision has been reported (25%).
Слайд 68Bening Prostatic Hyperplasia
Open Simple Prostatectomy
When the prostate is too large to
be removed endoscopically, an open enucleation is necessary.
Слайд 69Bening Prostatic Hyperplasia
Open prostatectomy may also be initiated when concomitant bladder
diverticulum or a bladder stone is present or if dorsal lithotomy positioning is not possible.
Слайд 70Bening Prostatic Hyperplasia
Open prostatectomies can be done with either a suprapubic
or retropubic approach.
Слайд 71Bening Prostatic Hyperplasia
The dissection plane is initiated sharply, and then blunt
dissection with the finger is performed to remove the adenoma.
Слайд 72Bening Prostatic Hyperplasia
In a simple retropubic prostatectomy, the bladder is not
entered.
Слайд 73Bening Prostatic Hyperplasia
Minimally Invasive Therapy
Laser Therapy
Many different techniques of laser surgery
for the prostate have been described.
Two main energy sources of lasers have been utilized—Nd:YAG and holmium:YAG.
Two main energy sources of lasers have been utilized—Nd:YAG and holmium:YAG.
Слайд 74Bening Prostatic Hyperplasia
Several different coagulation necrosis techniques have been described.
Слайд 75Bening Prostatic Hyperplasia
Transurethral Electrovaporization of the Prostate
Transurethral electrovaporization uses the standard
resectoscope but replaces a conventional loop with a variation of a grooved rollerball.
Слайд 76Bening Prostatic Hyperplasia
Hyperthermia
Microwave hyperthermia is most commonly delivered with a transurethral
catheter.
Слайд 77Bening Prostatic Hyperplasia
Transurethral Needle Ablation of the Prostate
Transurethral needle ablation uses
a specially designed urethral catheter that is passed into the urethra.
Слайд 78Bening Prostatic Hyperplasia
This technique is not adequate treatment for bladder neck
and median lobe enlargement.
Слайд 79Bening Prostatic Hyperplasia
High-Intensity Focused Ultrasound
High-intensity focused ultrasound is another means of
performing thermal tissue ablation. A specially designed, dual-function ultrasound probe is placed in the rectum.
Слайд 80Bening Prostatic Hyperplasia
This probe allows transrectal imaging of the prostate and
also delivers short bursts of high-intensity focused ultrasound energy, which heats the prostate tissue and results in coagulative necrosis.
Слайд 81Bening Prostatic Hyperplasia
Intraurethral Stents
They are usually covered by urothelium within
4–6 months after insertion.
Слайд 82Bening Prostatic Hyperplasia
These devices are typically used for patients with limited
life expectancy who are not deemed to be appropriate candidates for surgery or anesthesia.
Слайд 83Bening Prostatic Hyperplasia
Transurethral Balloon Dilation of the Prostate
Balloon dilation of the
prostate is performed with specially designed catheters that enable dilation of the prostatic fossa alone or the prostatic fossa and bladder neck.
Слайд 85Carcinoma of the Prostate (CaP)
Prostate cancer is the most common cancer
diagnosed and is the second leading cause of cancer death in American men.
Слайд 86Carcinoma of the Prostate (CaP)
The lifetime risk of a 50-year-old man
for latent CaP (detected as an incidental finding at autopsy, not related to the cause of death) is 40%; for clinically apparent CaP, 9.5%; and for death from CaP, 2.9%.
Слайд 87Carcinoma of the Prostate (CaP)
Thus, many prostate cancers are indolent
and inconsequential to the patient while others are virulent, and if detected too late or left untreated, they result in a patient's death.
Слайд 88Carcinoma of the Prostate (CaP)
Several risk factors for prostate cancer have
been identified. As discussed above, increasing age heightens the risk for CaP.
Слайд 89Carcinoma of the Prostate (CaP)
African Americans are at a higher risk
for CaP than whites. In addition, African American men tend to present at a later stage of disease than whites.
Слайд 90Carcinoma of the Prostate (CaP)
The age of disease onset in the
family member with the diagnosis of CaP affects a patient's relative risk.
Слайд 91Carcinoma of the Prostate (CaP)
High dietary fat intake increases the relative
risk for CaP by almost a factor of 2.
Слайд 92Carcinoma of the Prostate (CaP)
Etiology
The specific molecular mechanisms involved in the
development and progression of CaP are an area of intense interest in the laboratory.
Слайд 93Carcinoma of the Prostate (CaP)
Pathology
Over 95% of the cancers of the
prostate are adenocarcinomas.
Слайд 94Carcinoma of the Prostate (CaP)
Symptoms
Most patients with early-stage CaP are asymptomatic.
The presence of symptoms often suggests locally advanced or metastatic disease.
Слайд 97Carcinoma of the Prostate (CaP)
Locally advanced disease with bulky regional lymphadenopathy
may lead to lymphedema of the lower extremities.
Слайд 98Carcinoma of the Prostate (CaP)
Laboratory Findings
Azotemia can result from bilateral ureteral
obstruction either from direct extension into the trigone or from retroperitoneal adenopathy.
Слайд 99Carcinoma of the Prostate (CaP)
Tumor Markers—Prostate-Specific Antigen (PSA)
Serum PSA has revolutionized
our ability to detect CaP. Current detection strategies include the efficient use of the combination of DRE, serum PSA, and TRUS with systematic biopsy. Unfortunately, PSA is not specific for CaP, as other factors such as BPH, urethral instrumentation, and infection can cause elevations of serum PSA.
Although the last two factors can usually be clinically ascertained, distinguishing between elevations of serum PSA resulting from BPH and those related to CaP remains the most problematic.
Although the last two factors can usually be clinically ascertained, distinguishing between elevations of serum PSA resulting from BPH and those related to CaP remains the most problematic.
Слайд 100Carcinoma of the Prostate (CaP)
Prostate Biopsy
Systematic sextant prostate biopsy was the
most commonly employed technique used in detecting CaP.
Слайд 101Carcinoma of the Prostate (CaP)
Information from sextant biopsies has mainly focused
on cancer detection and has been underutilized for cancer staging.
Слайд 102Carcinoma of the Prostate (CaP)
TRUS
TRUS is useful in performing prostatic biopsies
and in providing some useful local staging information if cancer is detected.
Слайд 104Carcinoma of the Prostate (CaP)
Endorectal Magnetic Resonance Imaging
The reported staging accuracy
of endorectal coil magnetic resonance imaging (MRI) varies from 51% to 92%.
Слайд 105Carcinoma of the Prostate (CaP)
Differential Diagnosis
Not all patients with an elevated
PSA concentration have CaP.
Слайд 106Carcinoma of the Prostate (CaP)
Sclerotic lesions on plain x-ray films and
elevated levels of alkaline phosphatase can be seen in Paget disease and can often be difficult to distinguish from metastatic CaP.
Слайд 107Carcinoma of the Prostate (CaP)
Treatment
Localized Disease
General Considerations
The optimal form of therapy
for all stages of CaP remains a subject of great debate.
Слайд 108Carcinoma of the Prostate (CaP)
Treatment dilemmas persist in the management of
localized disease (T1 and T2) because of the uncertainty surrounding the relative efficacy of various modalities, including radical prostatectomy, radiation therapy, and surveillance.
Слайд 109Carcinoma of the Prostate (CaP)
Watchful Waiting
No randomized trial has demonstrated the
therapeutic benefit of radical treatment for early-stage prostate cancer.
Слайд 110Carcinoma of the Prostate (CaP)
In addition, the small, well-differentiated prostate cancers
commonly found in this population are often associated with very slow growth rates.
Слайд 111Carcinoma of the Prostate (CaP)
Radical Prostatectomy
The first radical perineal prostatectomy was
performed by Hugh Hampton Young in 1904, and Millin first described the radical retropubic approach in 1945.
Слайд 112Carcinoma of the Prostate (CaP)
Description of the anatomy of the dorsal
vein complex resulted in modifications in the surgical technique leading to reduced operative blood loss.