- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Gastric and duodenal ulcers презентация
Содержание
- 1. Gastric and duodenal ulcers
- 2. PLAN: I.Introduction What is an ulcer? II.Main
- 3. WHAT IS AN ULCER?
- 4. DIAGNOSIS Endoscopy (>55yrs, first time). Capture all
- 5. WHY ARE THEY IMPORTANT? HPA – “infectious
- 6. EMERGENCY ADMISSION FOR PERFORATION RATES
- 7. CAUSES? Ulcers are only found in white
- 8. CAUSES & RISK FACTORS Helicobacter pylori
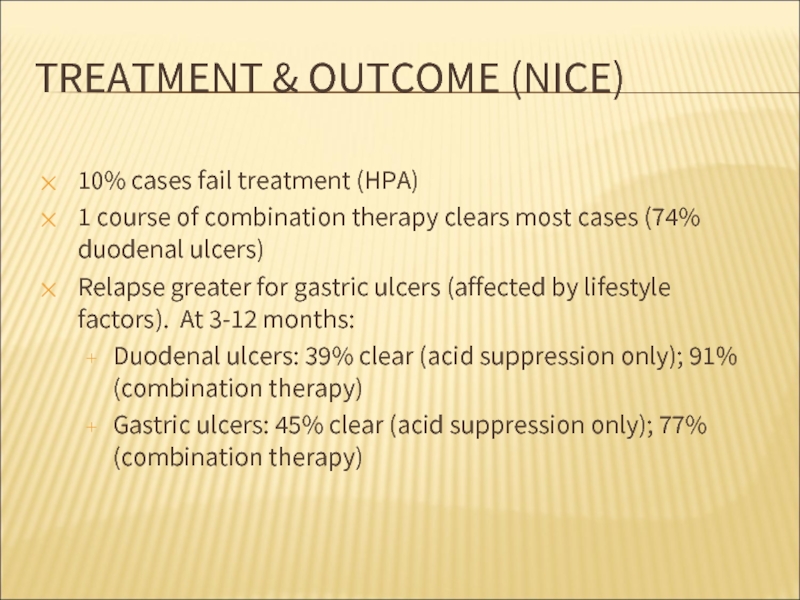
- 9. TREATMENT & OUTCOME (NICE) 10% cases fail
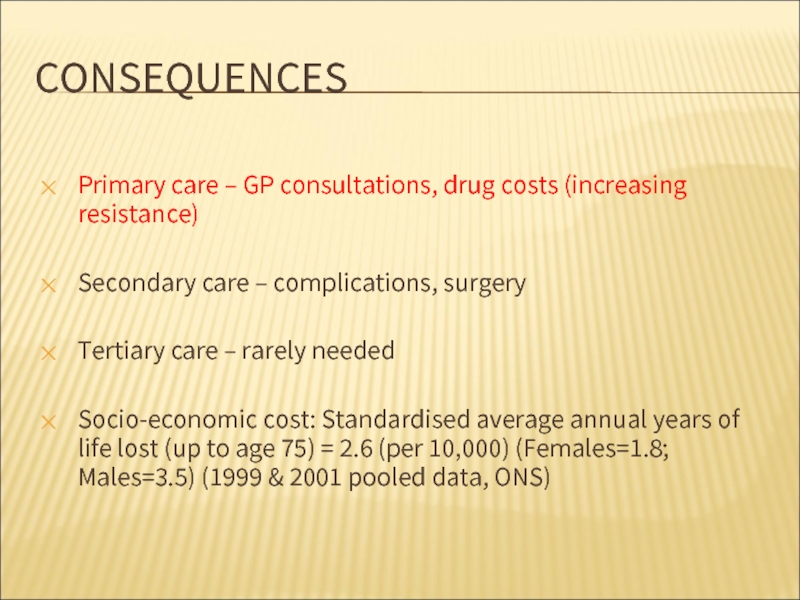
- 10. CONSEQUENCES Primary care – GP consultations, drug
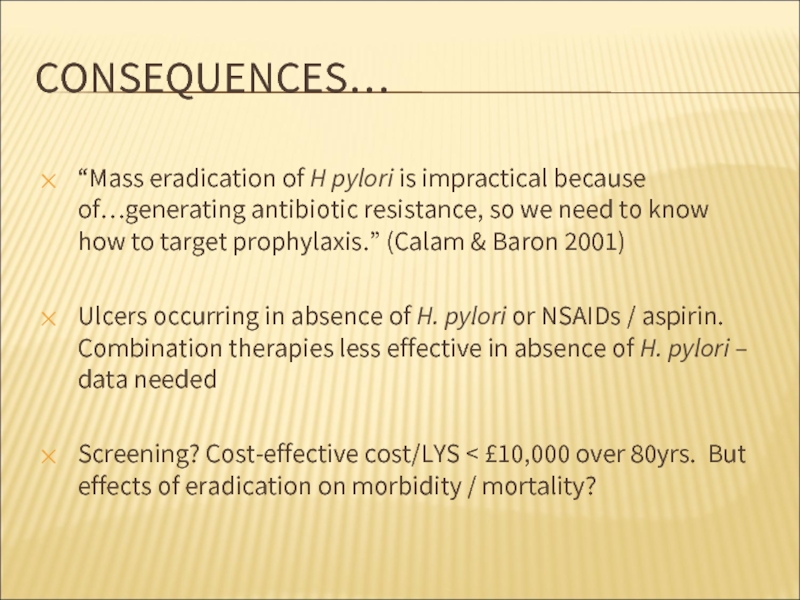
- 11. CONSEQUENCES… “Mass eradication of H pylori is impractical
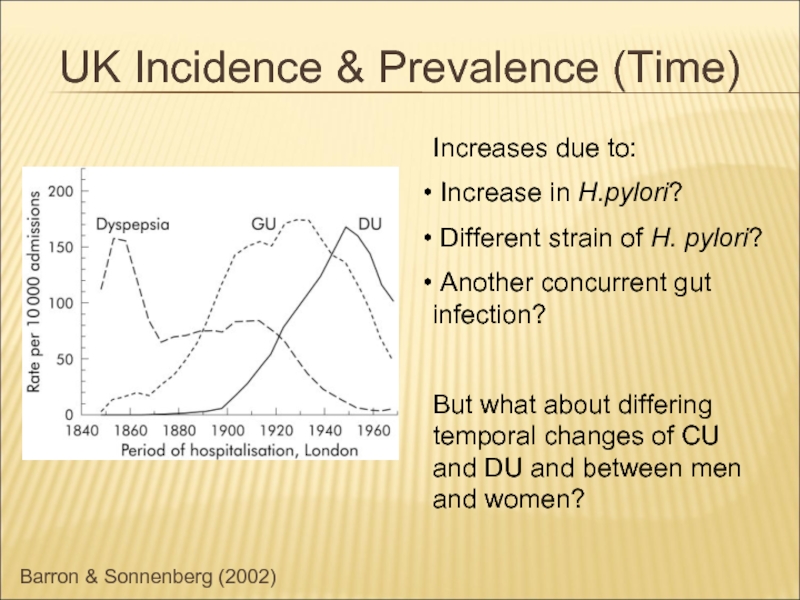
- 12. Barron & Sonnenberg (2002) UK Incidence &
- 13. UK INCIDENCE & PREVALENCE (TIME) Evidence of
- 14. UK INCIDENCE & PREVALENCE (PERSON) H. pylori
- 15. UK INCIDENCE & PREVALENCE (PERSON) Current trends:
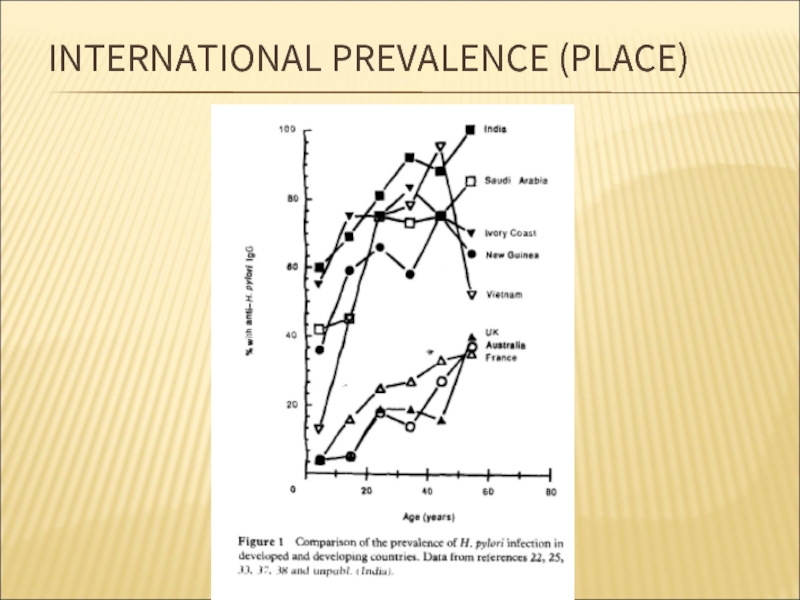
- 16. INTERNATIONAL PREVALENCE (PLACE)
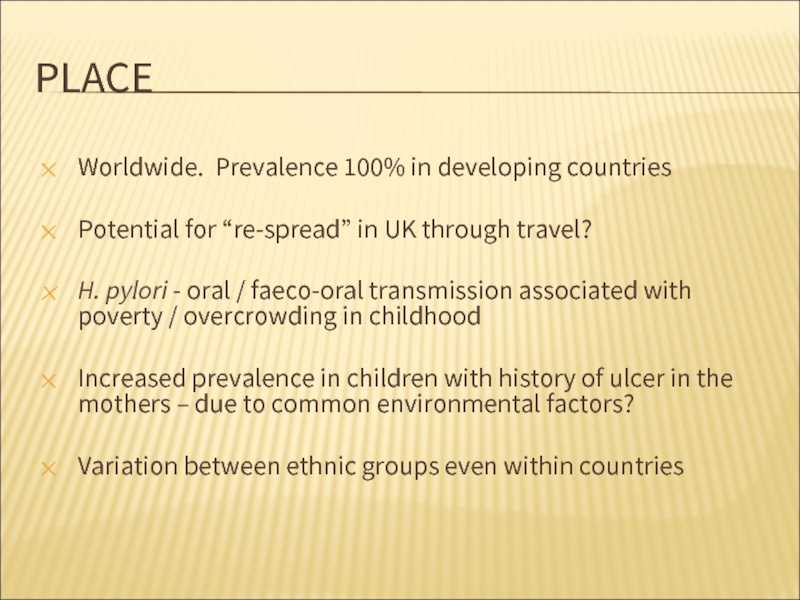
- 17. PLACE Worldwide. Prevalence 100% in developing countries
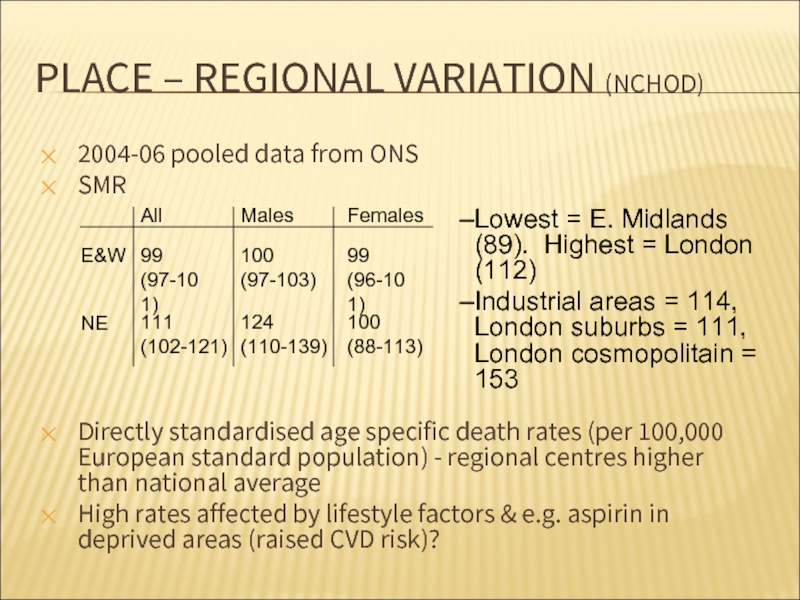
- 18. PLACE – REGIONAL VARIATION (NCHOD) 2004-06 pooled
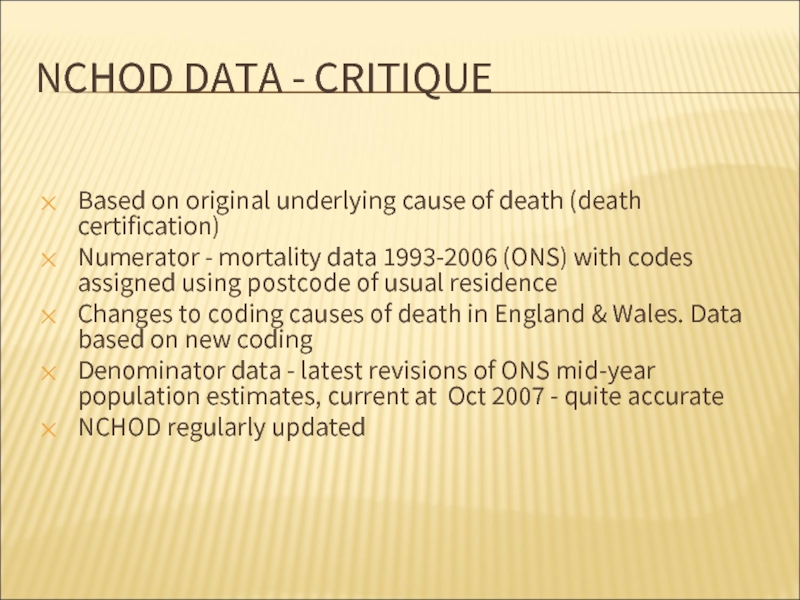
- 19. NCHOD DATA - CRITIQUE Based on original
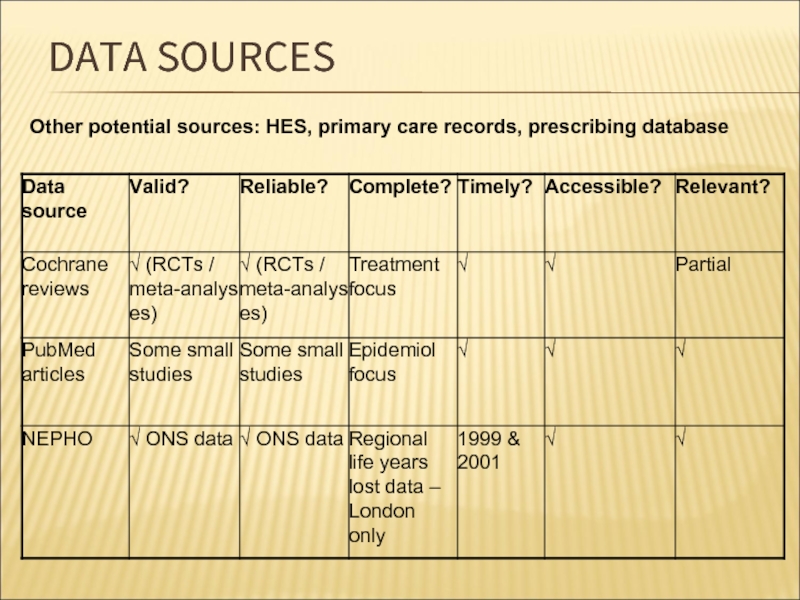
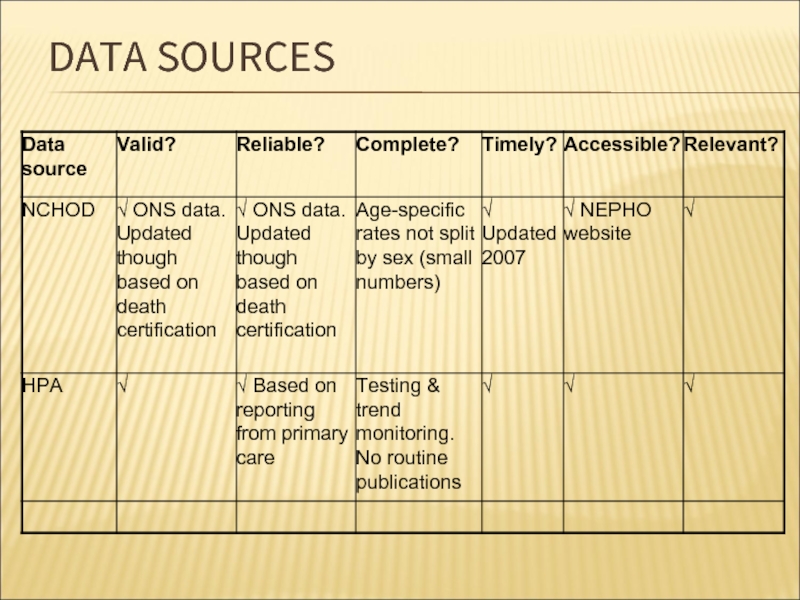
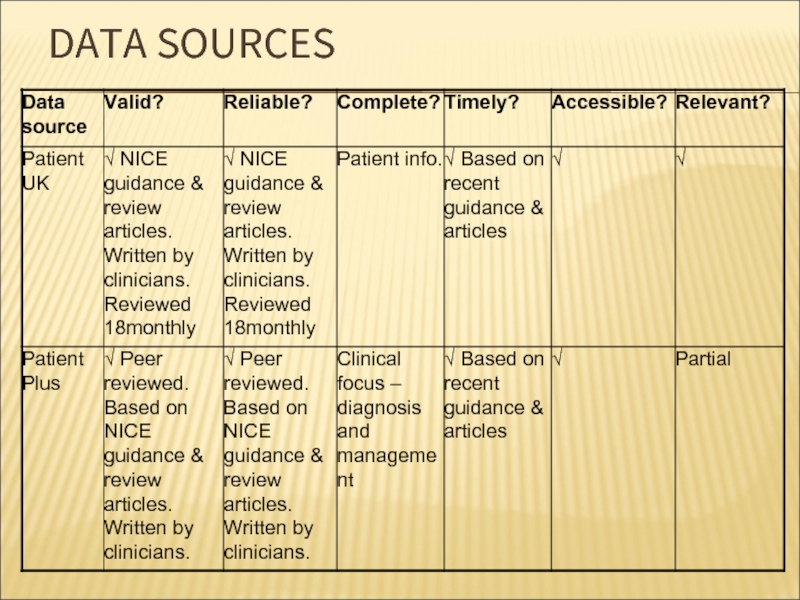
- 20. DATA SOURCES Other potential sources: HES, primary care records, prescribing database
- 21. DATA SOURCES
- 22. DATA SOURCES
- 23. CONCLUSION Disease mechanism / transmission poorly understood
- 24. Used books Tuberculosis Fact sheet N°104".
Слайд 1GASTRIC AND DUODENAL ULCERS
Prepared by:Beken O.SH
Faculty:GM
Course:2
Group:027-2
Almaty,2017
Слайд 2PLAN:
I.Introduction
What is an ulcer?
II.Main section
Diagnosis
Causes & Risk Factors
Why are they important?
Consequences
III.Conclusion
IV.Used
Слайд 3WHAT IS AN ULCER?
Acid breaks through protective substances on gut
Duodenum (1st part small intestine) – most common site
“Gastric” ulcers – in stomach
Pain, bloating, nausea, “fullness”, weight loss, tiredness
Complications: bleeding, perforation, obstruction
Слайд 4DIAGNOSIS
Endoscopy (>55yrs, first time). Capture all cases?
Faecal / breath tests for
GI series (rare)
False positive tests
Missed cases? – risk of transmission / disease progression
Слайд 5WHY ARE THEY IMPORTANT?
HPA – “infectious disease” but main effects are
Potential “medical emergency”
Chronic symptoms – health and economic costs
H. pylori also linked to:
Functional dypepsia
Cancer (2-6x more likely, though still rare)
Differential clinical outcome - interaction between bacterial properties (phenotypic variation), genetics and environmental / behavioural factors
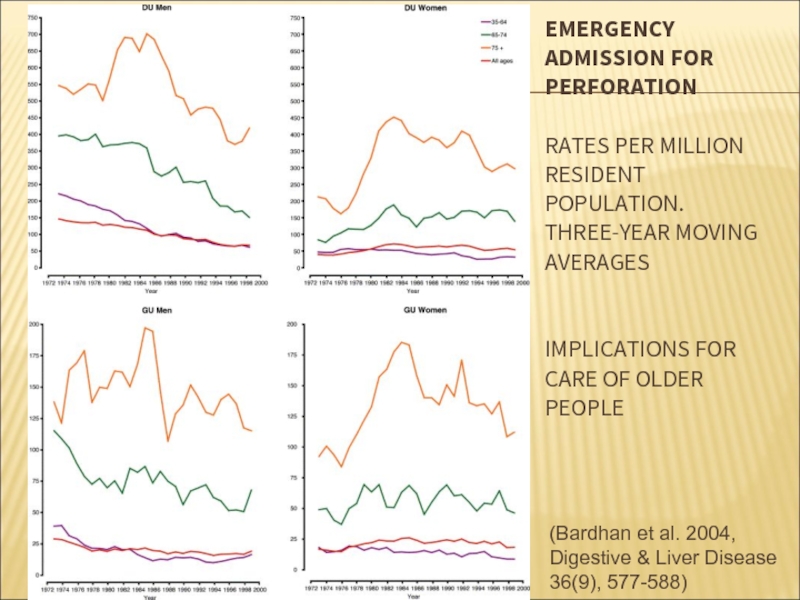
Слайд 6EMERGENCY ADMISSION FOR PERFORATION RATES PER MILLION RESIDENT POPULATION. THREE-YEAR MOVING
(Bardhan et al. 2004, Digestive & Liver Disease 36(9), 577-588)
Слайд 7CAUSES?
Ulcers are only found in white people, usually in long thin
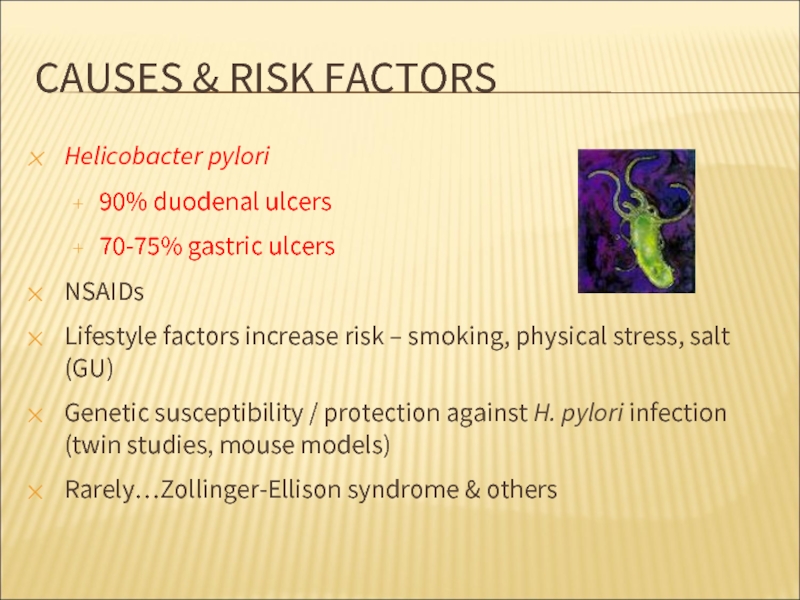
Слайд 8CAUSES & RISK FACTORS
Helicobacter pylori
90% duodenal ulcers
70-75% gastric ulcers
NSAIDs
Lifestyle factors
Genetic susceptibility / protection against H. pylori infection (twin studies, mouse models)
Rarely…Zollinger-Ellison syndrome & others
Слайд 9TREATMENT & OUTCOME (NICE)
10% cases fail treatment (HPA)
1 course of combination
Relapse greater for gastric ulcers (affected by lifestyle factors). At 3-12 months:
Duodenal ulcers: 39% clear (acid suppression only); 91% (combination therapy)
Gastric ulcers: 45% clear (acid suppression only); 77% (combination therapy)
Слайд 10CONSEQUENCES
Primary care – GP consultations, drug costs (increasing resistance)
Secondary care –
Tertiary care – rarely needed
Socio-economic cost: Standardised average annual years of life lost (up to age 75) = 2.6 (per 10,000) (Females=1.8; Males=3.5) (1999 & 2001 pooled data, ONS)
Слайд 11CONSEQUENCES…
“Mass eradication of H pylori is impractical because of…generating antibiotic resistance, so
Ulcers occurring in absence of H. pylori or NSAIDs / aspirin. Combination therapies less effective in absence of H. pylori – data needed
Screening? Cost-effective cost/LYS < £10,000 over 80yrs. But effects of eradication on morbidity / mortality?
Слайд 12Barron & Sonnenberg (2002)
UK Incidence & Prevalence (Time)
Increases due to:
Different strain of H. pylori?
Another concurrent gut infection?
But what about differing temporal changes of CU and DU and between men and women?
Слайд 13UK INCIDENCE & PREVALENCE (TIME)
Evidence of cohort effect 1970-1986: (Primatesta et
Decreased hospitalized morbidity and mortality
Related more to changes in risk factors (e.g. smoking) in different cohorts than new pharmacological treatments? - implications for public health!
OR: Genetic factors may be more important (Malaty et al. 1994)
Слайд 14UK INCIDENCE & PREVALENCE (PERSON)
H. pylori infection
Incidence: 1-3% of adults p.a.
Prevalence infection: 40% population (HPA: >50% of 50+yr olds)
Ulceration
Incidence:
DU in 30-50yrs old; higher incidence in men
GU in >60yr olds; higher incidence in women
Low prevalence in younger age groups
Duodenal ulcer: up to 10% of population
Слайд 15UK INCIDENCE & PREVALENCE (PERSON)
Current trends:
Annual age-standardized period prevalence decreased 1994-1998,
Sex incidence evening out – decreasing incidence in young men; increasing in older women
But emergency admission rates for complications unchanged in last 30yrs
Kang et al. (2006) – increase in case fatality for DU. Due to concomitant comorbidity / increasing ulceration (NSAIDs) / H.pylori (i.e. changing natural history)?
Future decrease in prevalence?
Слайд 17PLACE
Worldwide. Prevalence 100% in developing countries
Potential for “re-spread” in UK through
H. pylori - oral / faeco-oral transmission associated with poverty / overcrowding in childhood
Increased prevalence in children with history of ulcer in the mothers – due to common environmental factors?
Variation between ethnic groups even within countries
Слайд 18PLACE – REGIONAL VARIATION (NCHOD)
2004-06 pooled data from ONS
SMR
Directly standardised age
High rates affected by lifestyle factors & e.g. aspirin in deprived areas (raised CVD risk)?
Lowest = E. Midlands (89). Highest = London (112)
Industrial areas = 114, London suburbs = 111, London cosmopolitain = 153
Слайд 19NCHOD DATA - CRITIQUE
Based on original underlying cause of death (death
Numerator - mortality data 1993-2006 (ONS) with codes assigned using postcode of usual residence
Changes to coding causes of death in England & Wales. Data based on new coding
Denominator data - latest revisions of ONS mid-year population estimates, current at Oct 2007 - quite accurate
NCHOD regularly updated
Слайд 23CONCLUSION
Disease mechanism / transmission poorly understood
Risk factors multiple & interacting
H. pylori
“Each generation has carried its own particular risk of bearing ulcers throughout adult life” (Susser & Stein 1962)
Current pattern = exposure to H. pylori + genetics + exposure to drugs + environmental / behavioural factors
DU / GU likely to continue causing significant chronic disease burden and personal / societal cost. Predicting future pattern difficult
Слайд 24Used books
Tuberculosis Fact sheet N°104". WHO. October 2015. Retrieved 11 February
"Basic TB Facts". CDC. March 13, 2012. Retrieved 11 February 2016
Medical Laboratory Science: Theory and Practice. New Delhi: Tata McGraw-Hill. 2000. p. 473
"Acid-Fast Stain Protocols". 21 August 2013. Retrieved 26 March 2016.
Wkipedia.org