practice – family medicine
- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Chest pain презентация
Содержание
- 2. CHEST PAIN 5% of all ED visits per year Differential diagnosis is difficult
- 3. CHEST PAIN ANATOMY DIFFERENTIAL DIAGNOSIS BRIEF OVERVIEW
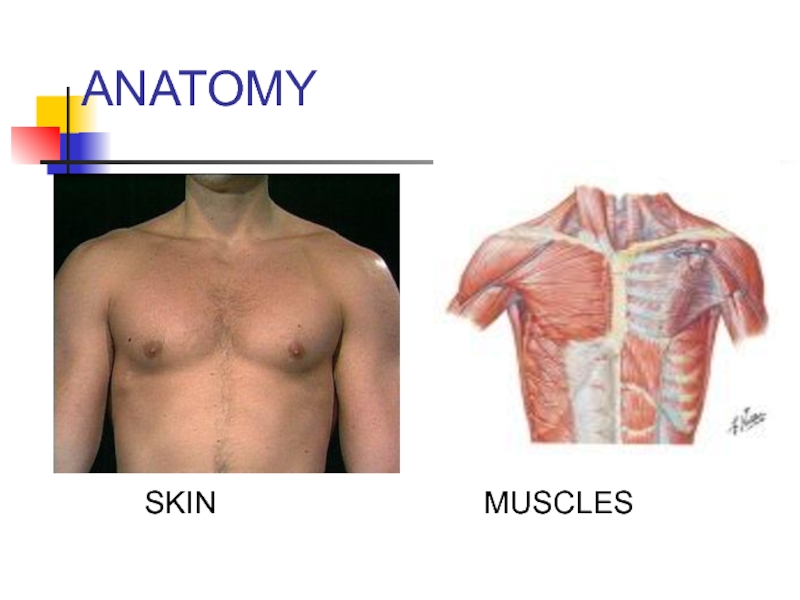
- 4. ANATOMY In devising a differential diagnosis for
- 5. ANATOMY
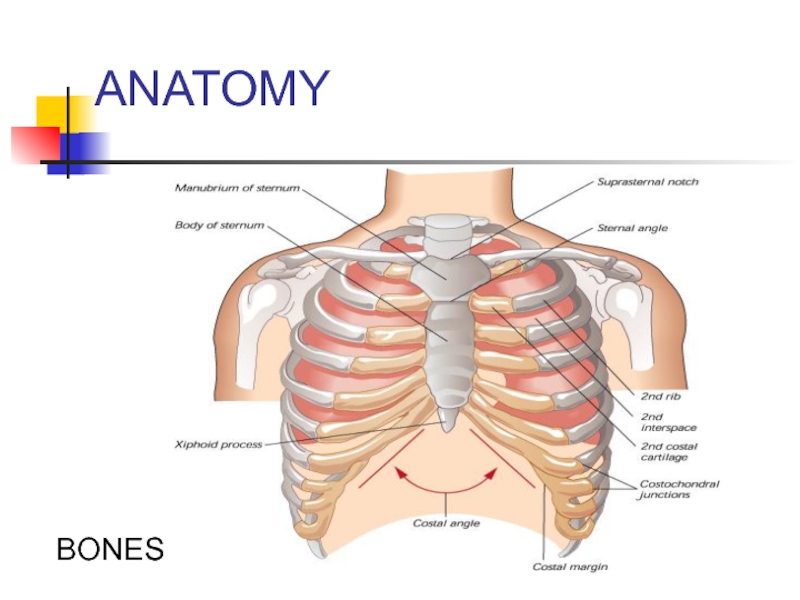
- 6. ANATOMY BONES
- 7. ANATOMY PULMONARY SYSTEM
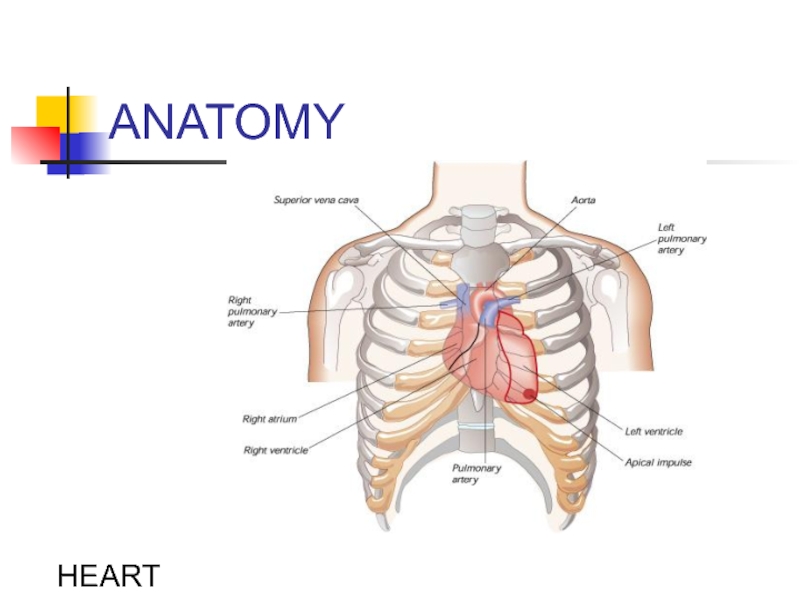
- 8. ANATOMY HEART
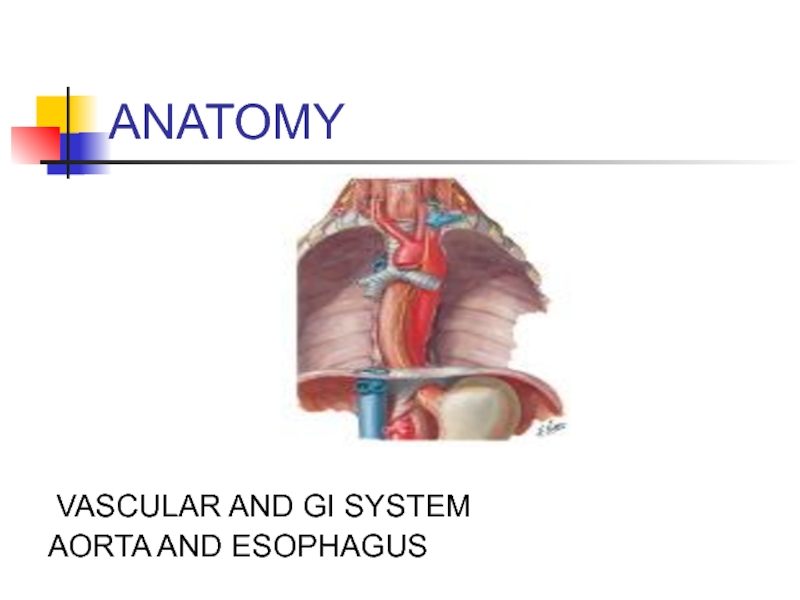
- 9. ANATOMY VASCULAR AND GI SYSTEM AORTA AND ESOPHAGUS
- 10. DIFFERENTIAL DIAGNOSIS OF CHEST PAIN CHEST WALL
- 11. DD: CHEST PAIN CHEST WALL PAIN
- 12. DD: CHEST PAIN PULMONARY CAUSES 1 -
- 13. DD: CHEST PAIN CARDIAC CAUSES
- 14. DD: CHEST PAIN Vascular Causes: -Aortic Dissection
- 15. DD: CHEST PAIN GI CAUSES
- 16. DD: CHEST PAIN PSYCHIATRIC -
- 17. CHEST PAIN BRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAIN
- 18. CHEST WALL PAIN .
- 19. CHEST WALL PAIN HERPES ZOSTER
- 20. HERPES ZOSTER Clusters of vesicles (with clear
- 21. HERPES ZOSTER TREATMENT: * Antivirals:
- 22. CHEST WALL PAIN Musculoskeletal Pain -
- 23. MUSCULOSKELETAL PAIN DIAGNOSIS COSTOCHONDRITIS TIETZE SYNDROME
- 24. MUSCULOSKELETAL PAIN Treatment: Analgesia (NSAIDs)
- 25. PULMONARY CAUSES OF CHEST PAIN .
- 26. PULMONARY EMBOLISM RISK FACTORS: VIRCHOW’S TRIAD
- 27. PULMONARY EMBOLISM (PE) CLINICAL FEATURES
- 28. PE: DIAGNOSTIC TESTS ECG:
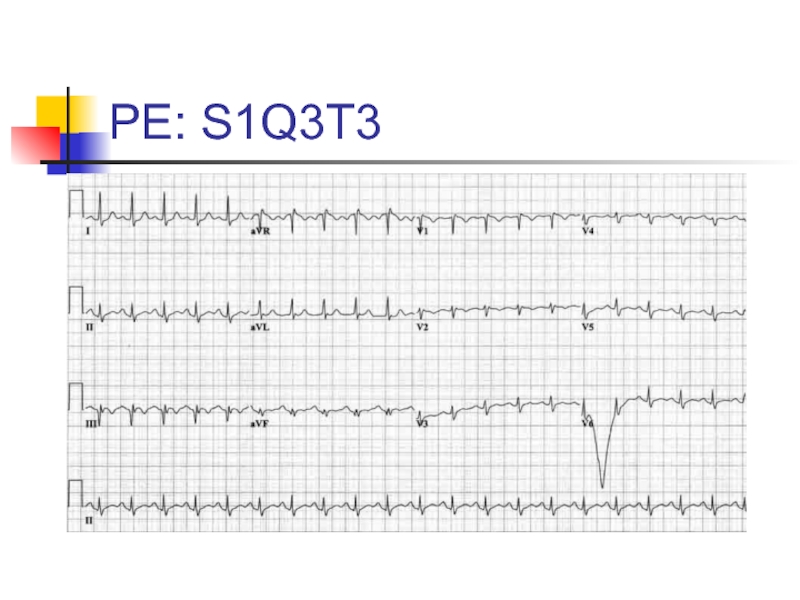
- 29. PE: S1Q3T3
- 30. PE: DIAGNOSTIC TESTS CHEST X-RAY
- 31. CXR: Hampton’s Hump and Westermark’s Sign
- 32. PE: DIAGNOSTIC TESTS ABG:
- 34. PE: DIAGNOSTIC TESTS VQ SCAN (Ventilation-Perfusion scan)-
- 35. PE: TREATMENT Initiate Heparin *
- 36. PNEUMONIA CLINICAL FEATURES - Cough
- 37. PNEUMONIA: DIAGNOSIS X-Ray If patient is to
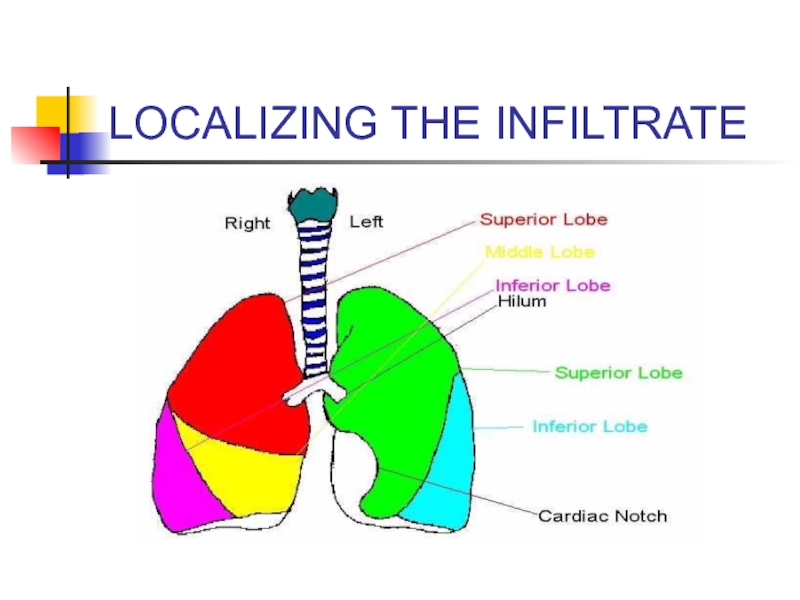
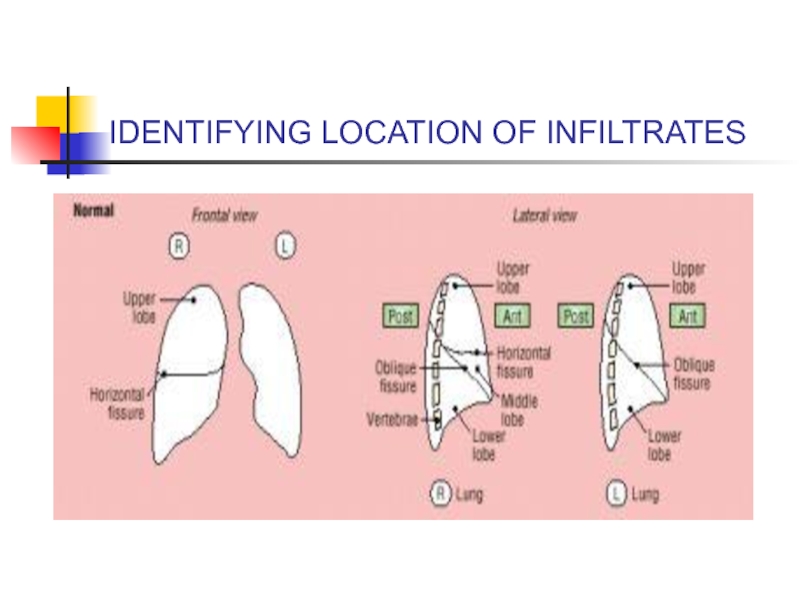
- 38. LOCALIZING THE INFILTRATE
- 39. IDENTIFYING LOCATION OF INFILTRATES
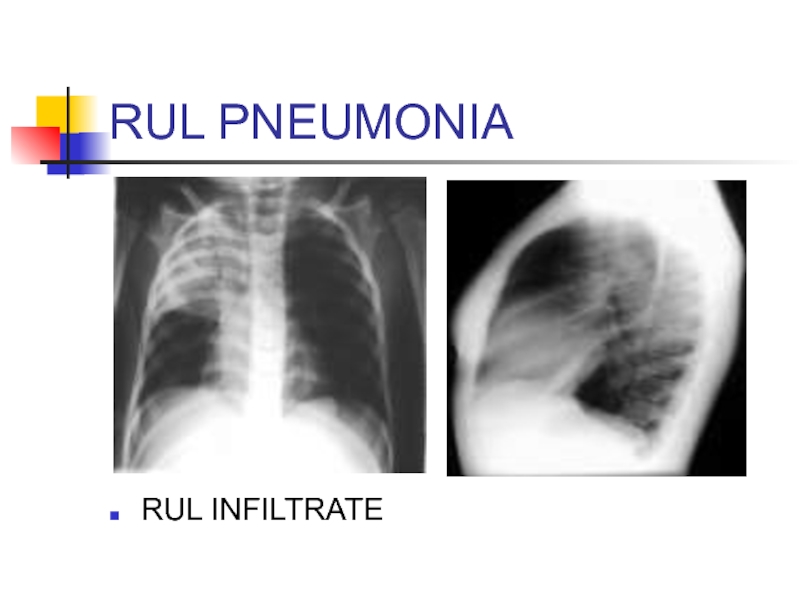
- 40. RUL PNEUMONIA RUL INFILTRATE
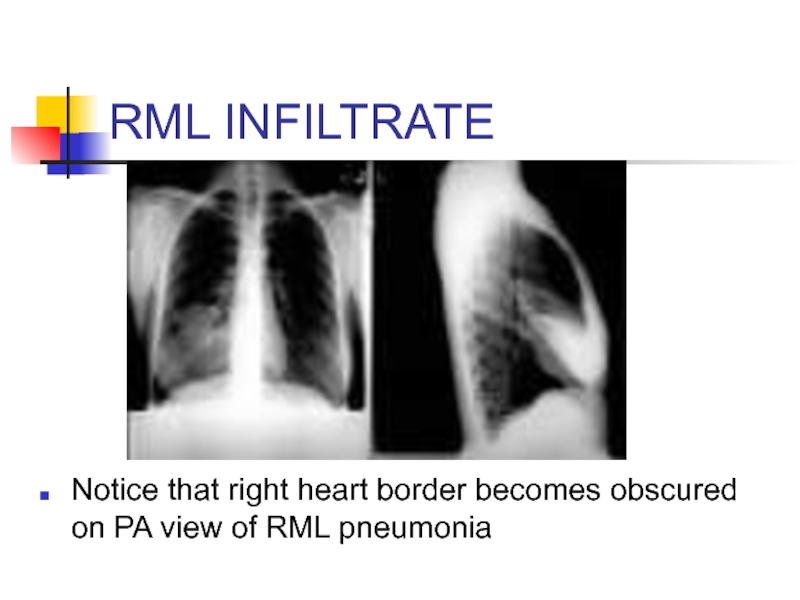
- 41. RML INFILTRATE Notice that right heart border becomes obscured on PA view of RML pneumonia
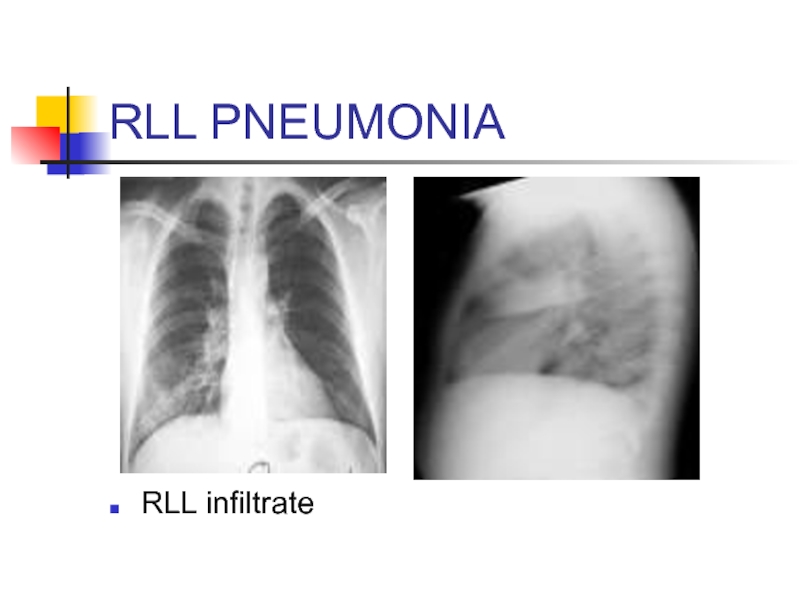
- 42. RLL PNEUMONIA RLL infiltrate
- 43. PNEUMONIA: TREATMENT Community- Acquired: -
- 44. SPONTANEOUS PNEUMOTHORAX RISK FACTORS: -
- 45. PNEUMOTHORAX CLINICAL FEATURES - Acute
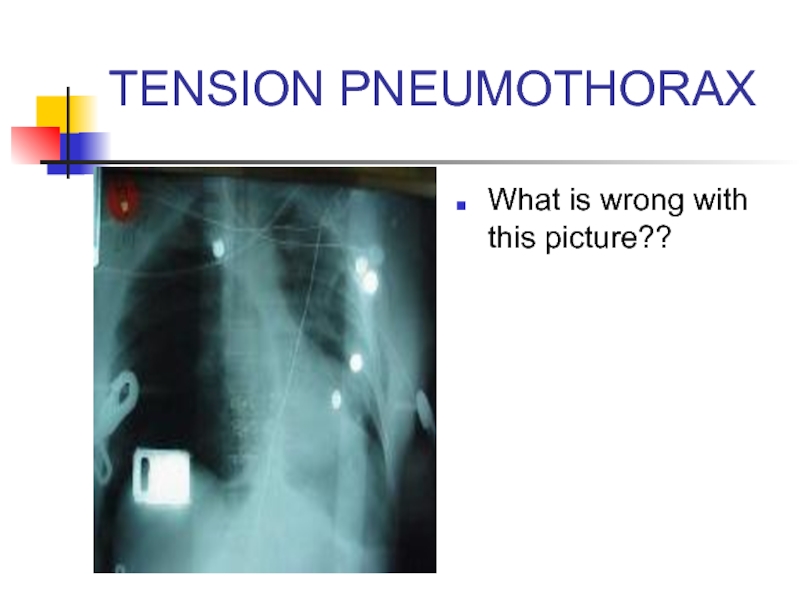
- 46. TENSION PNEUMOTHORAX What is wrong with this picture??
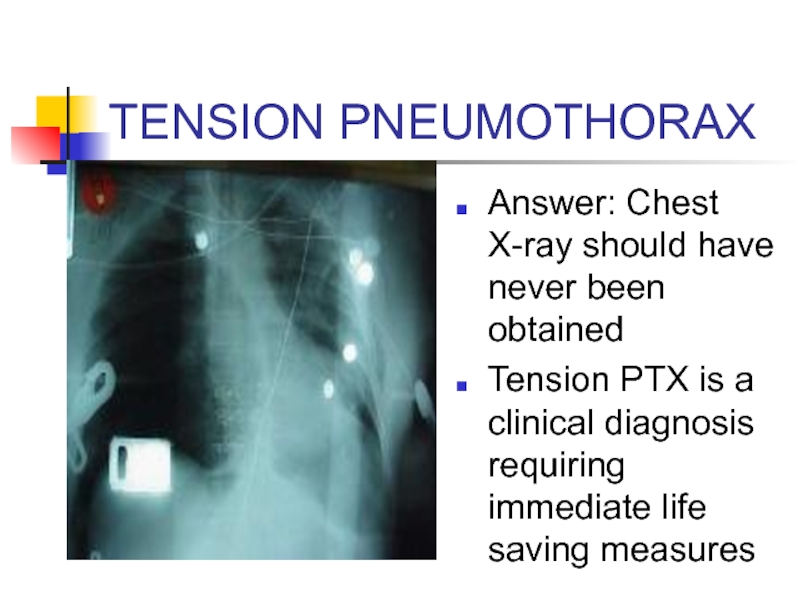
- 47. TENSION PNEUMOTHORAX Answer: Chest X-ray should have
- 48. Tension Pneumothorax Trachea deviates to contralateral side
- 49. NEEDLE DECOMPRESSION Insert large bore needle (14
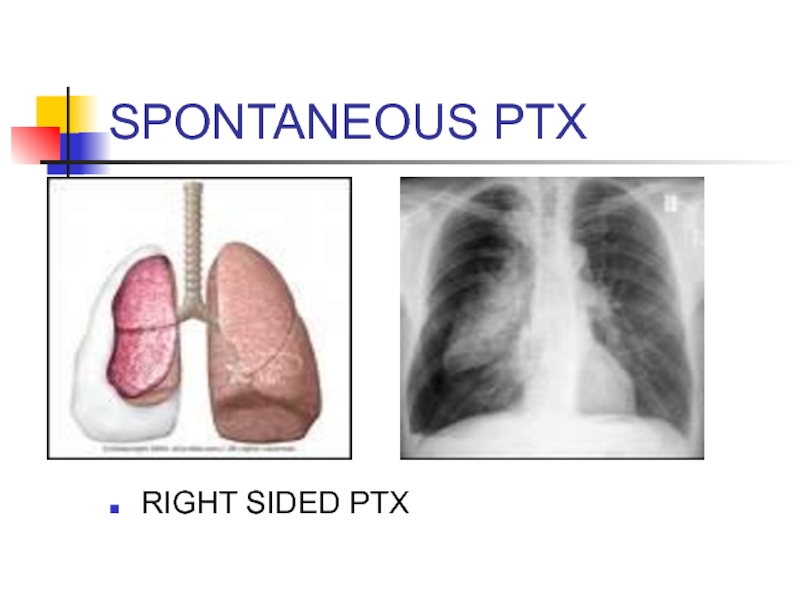
- 50. SPONTANEOUS PTX RIGHT SIDED PTX
- 51. SPONTANEOUS PTX TREATMENT: - If small (
- 52. PLEURITIS/SEROSITIS Inflammation of pleura that covers lung
- 53. COPD/ASTHMA EXACERBATIONS CLINICAL FEATURES: -
- 54. COPD EXACERBATION: TREATMENT Oxygen: Must prevent hypoxemia.
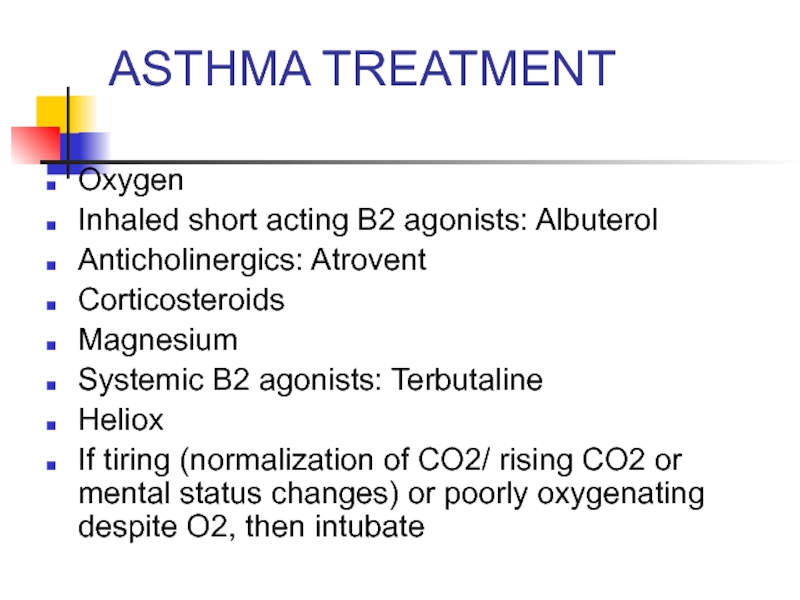
- 55. ASTHMA TREATMENT Oxygen Inhaled short acting B2
- 56. CARDIAC CAUSES OF CHEST PAIN .
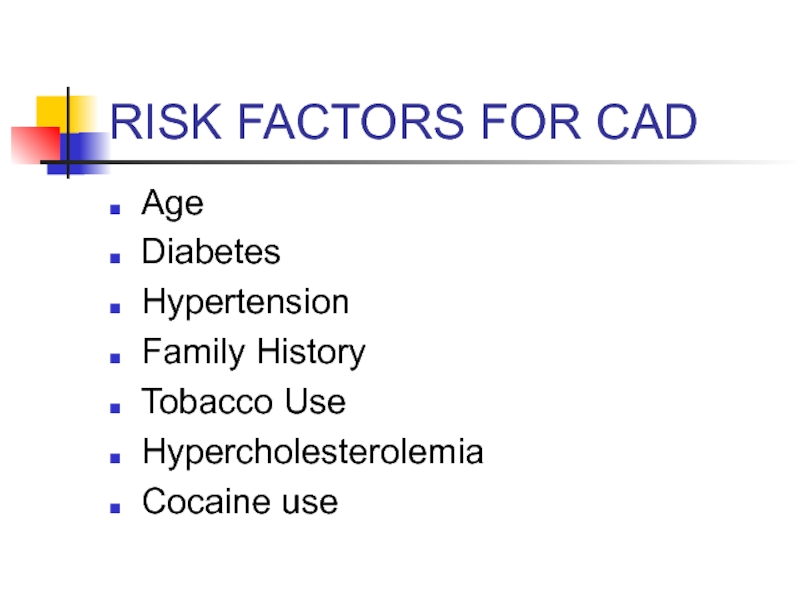
- 57. RISK FACTORS FOR CAD Age Diabetes Hypertension Family History Tobacco Use Hypercholesterolemia Cocaine use
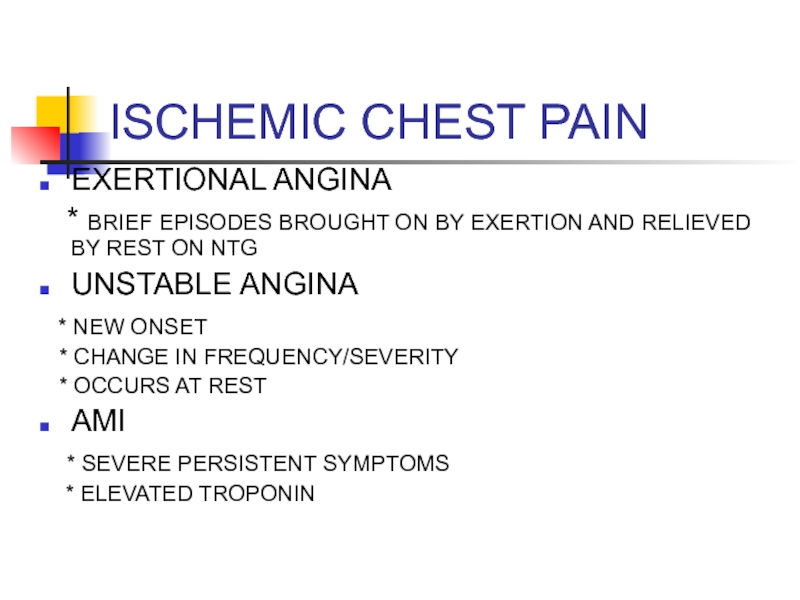
- 58. ISCHEMIC CHEST PAIN EXERTIONAL ANGINA
- 59. Angina pectoris Stable angina pectoris is a
- 60. Angina pectoris The chest discomfort may be
- 61. The chest discomfort usually lasts up
- 62. ISCHEMIC CHEST PAIN: DIAGNOSIS 12 LEAD EСG
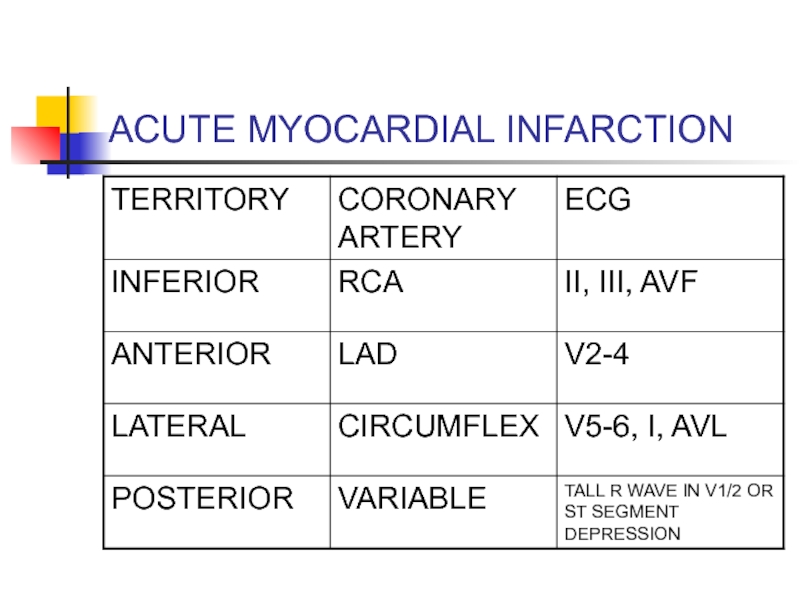
- 63. ACUTE MYOCARDIAL INFARCTION
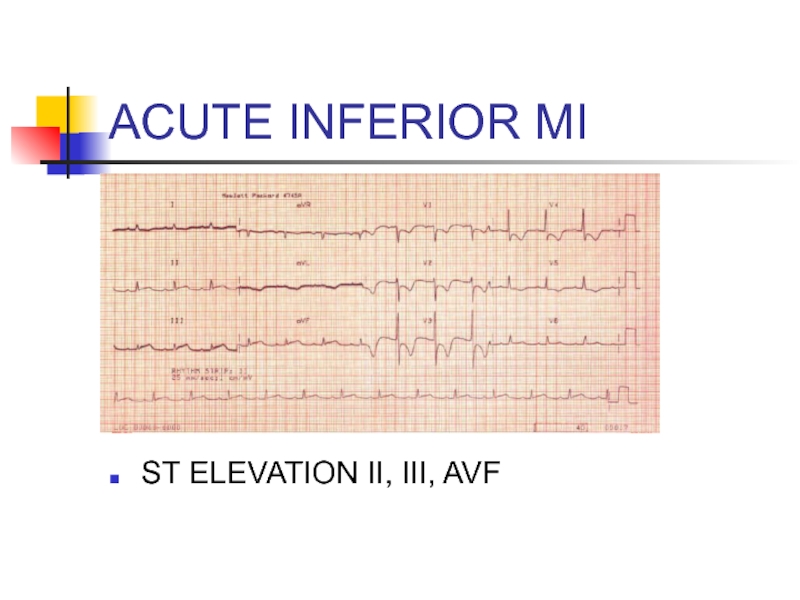
- 64. ACUTE INFERIOR MI ST ELEVATION II, III, AVF
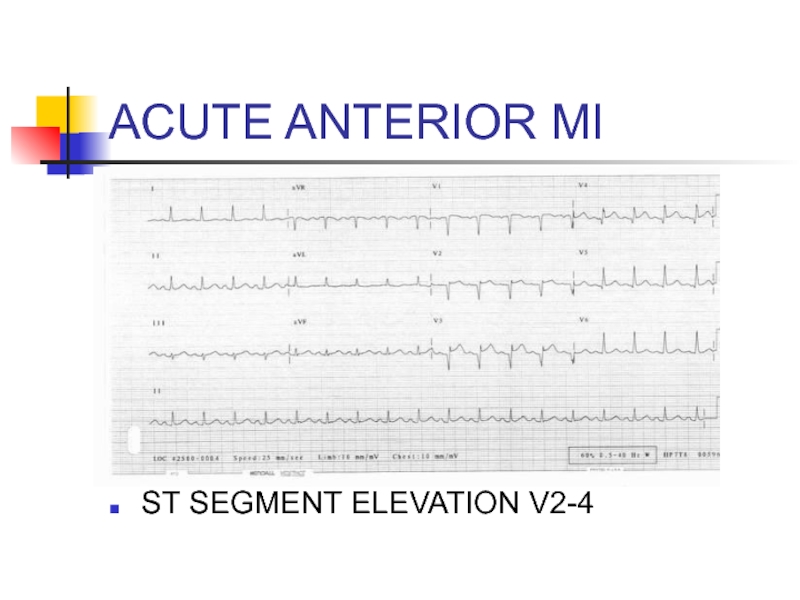
- 65. ACUTE ANTERIOR MI ST SEGMENT ELEVATION V2-4
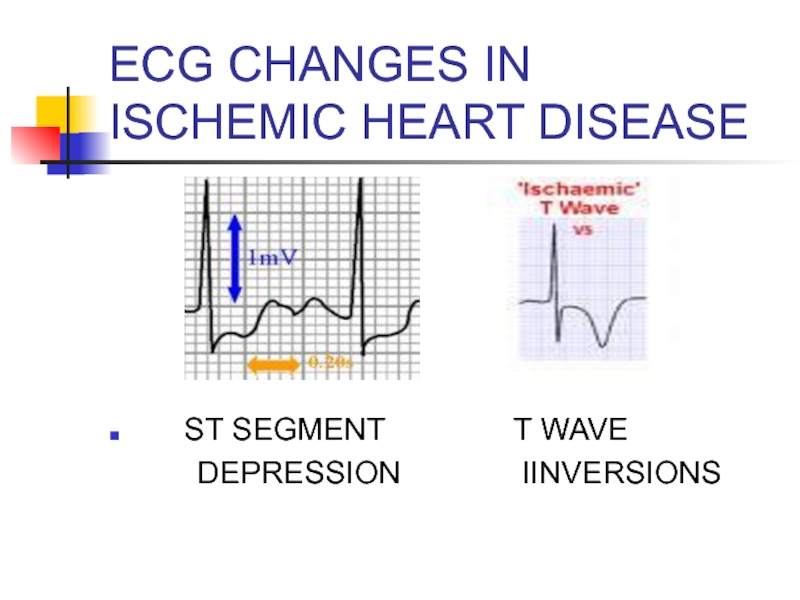
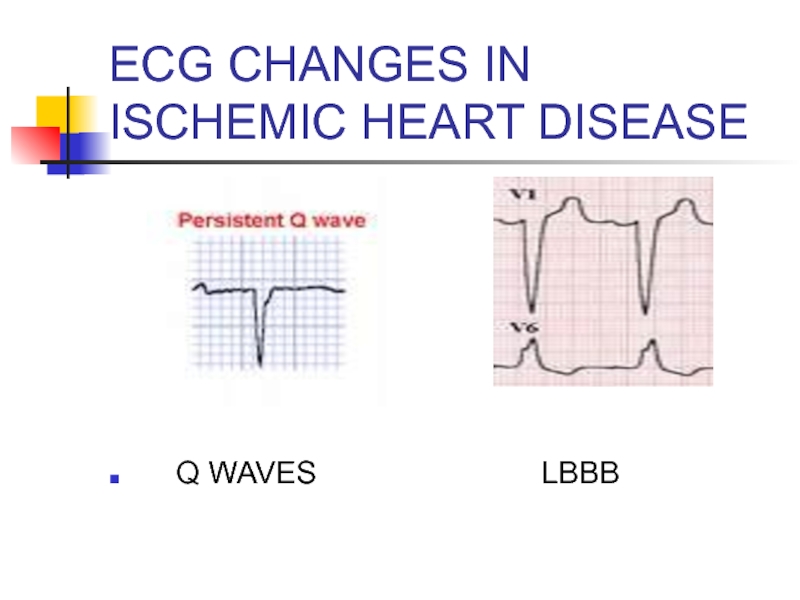
- 66. EСG CHANGES IN ISCHEMIC HEART DISEASE
- 67. EСG CHANGES IN ISCHEMIC HEART DISEASE
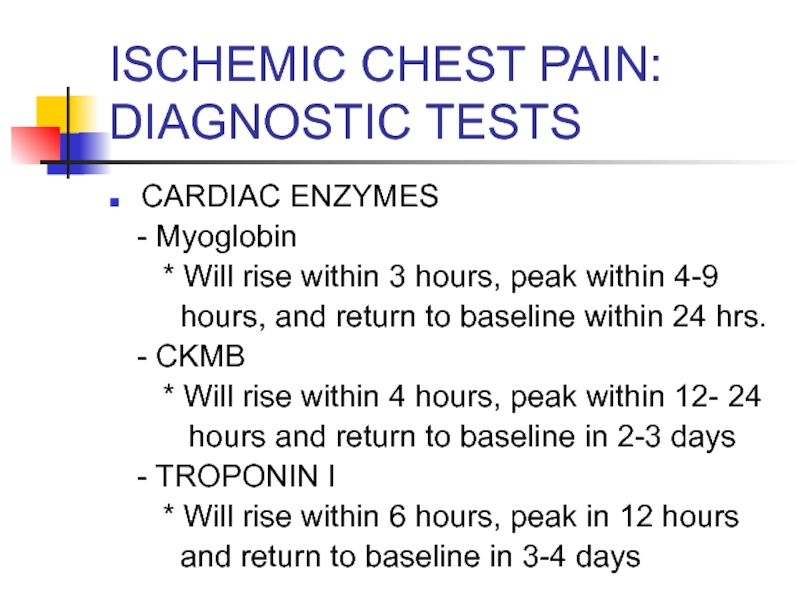
- 68. ISCHEMIC CHEST PAIN: DIAGNOSTIC TESTS CARDIAC ENZYMES
- 69. ISCHEMIC HEART DISEASE TREATMENT: ACUTE ST SEGMENT
- 70. ISCHEMIC HEART DISEASE TREATMENT: NONSTEMI AND UNSTABLE
- 71. LOW RISK CARDIAC CHEST PAIN If low
- 72. VALVULAR HEART DISEASE AORTIC STENOSIS
- 73. ACUTE PERICARDITIS CLINICAL FEATURES - Acute,
- 74. ACUTE PERICARDITIS COMMON CAUSES *
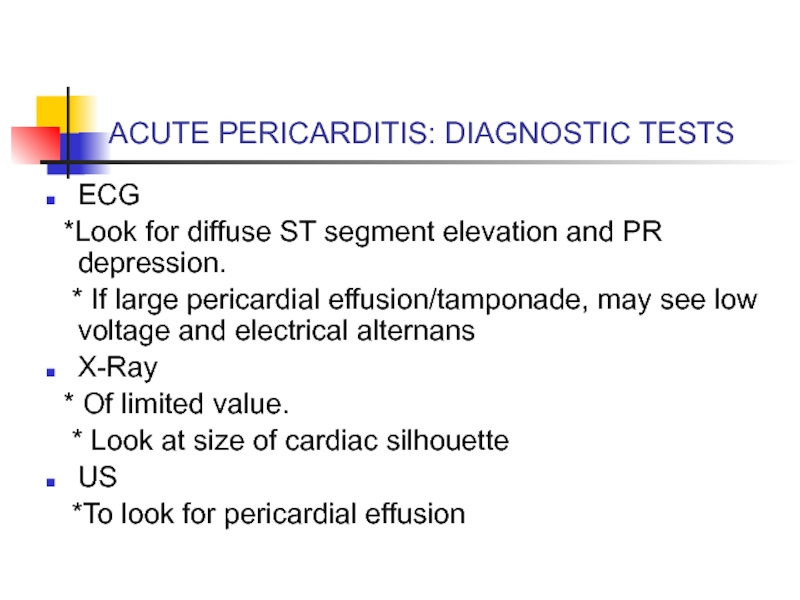
- 75. ACUTE PERICARDITIS: DIAGNOSTIC TESTS ECG *Look
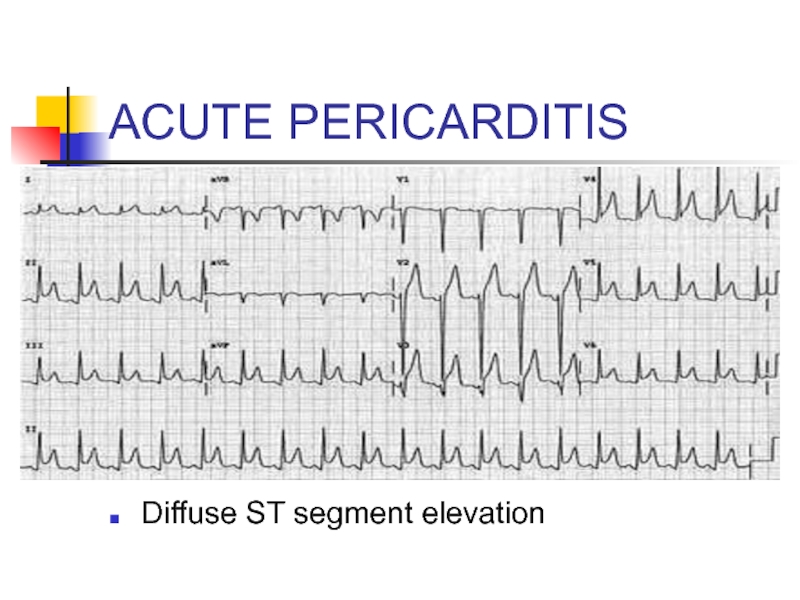
- 76. ACUTE PERICARDITIS Diffuse ST segment elevation
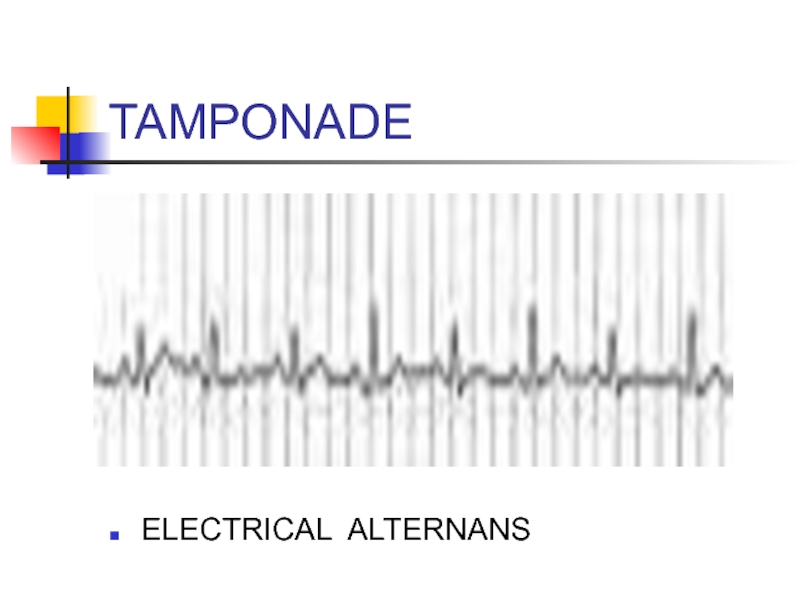
- 77. TAMPONADE ELECTRICAL ALTERNANS
- 78. ACUTE PERICARDITIS TREATMENT: - If
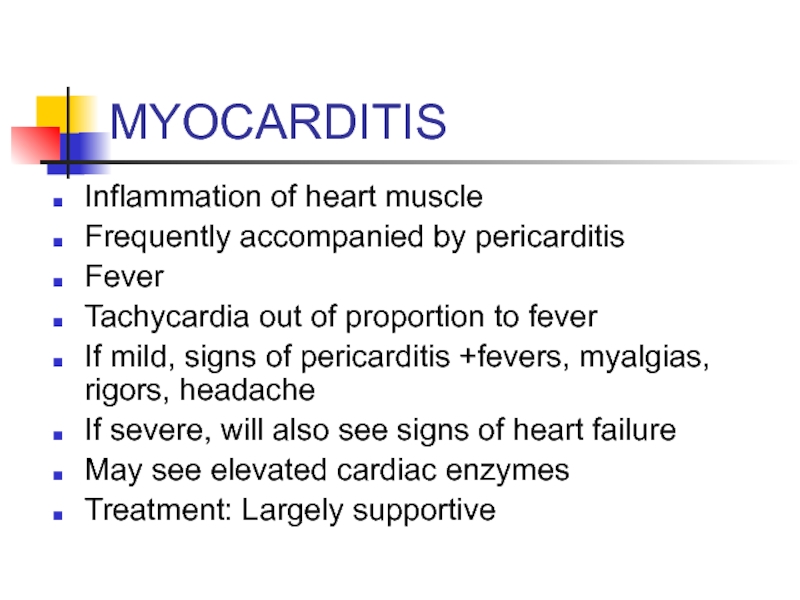
- 79. MYOCARDITIS Inflammation of heart muscle Frequently accompanied
- 80. VASCULAR CAUSES OF CHEST PAIN .
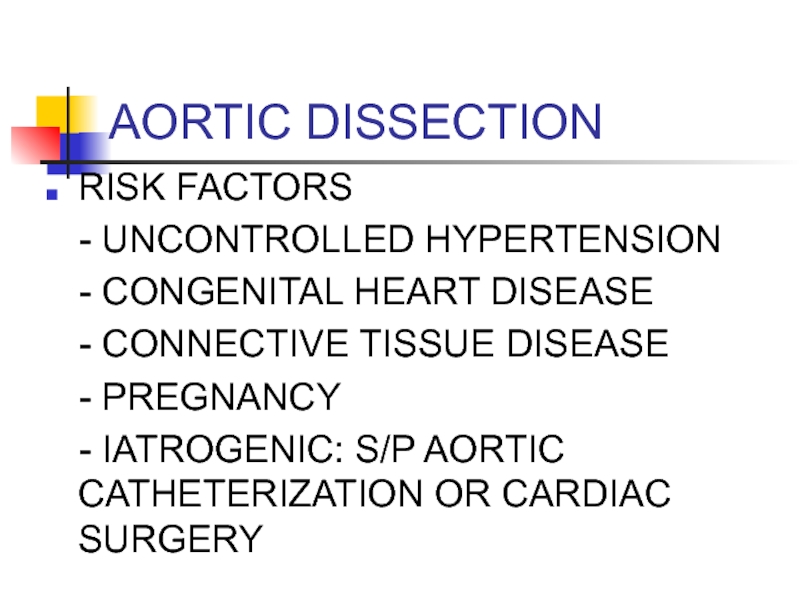
- 81. AORTIC DISSECTION RISK FACTORS -
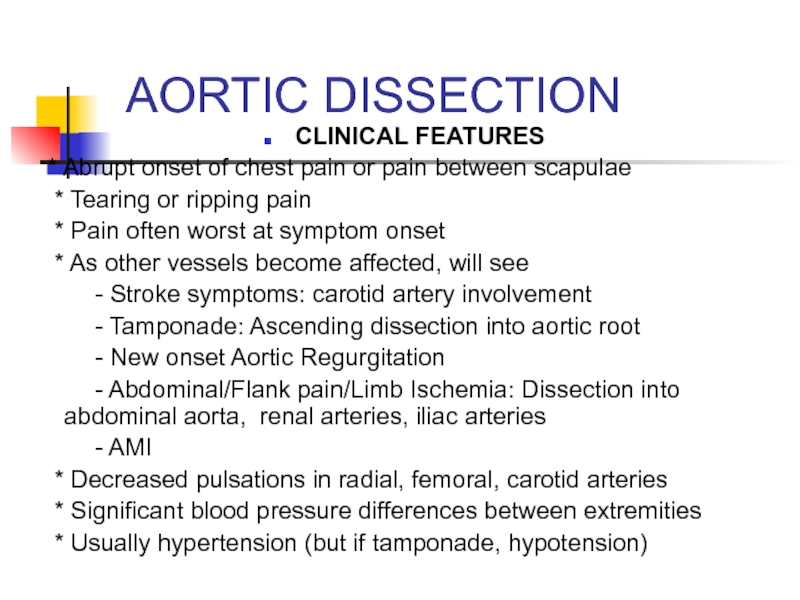
- 82. AORTIC DISSECTION CLINICAL FEATURES * Abrupt
- 83. DIAGNOSIS: AORTIC DISSECTION CXR: Look for widened
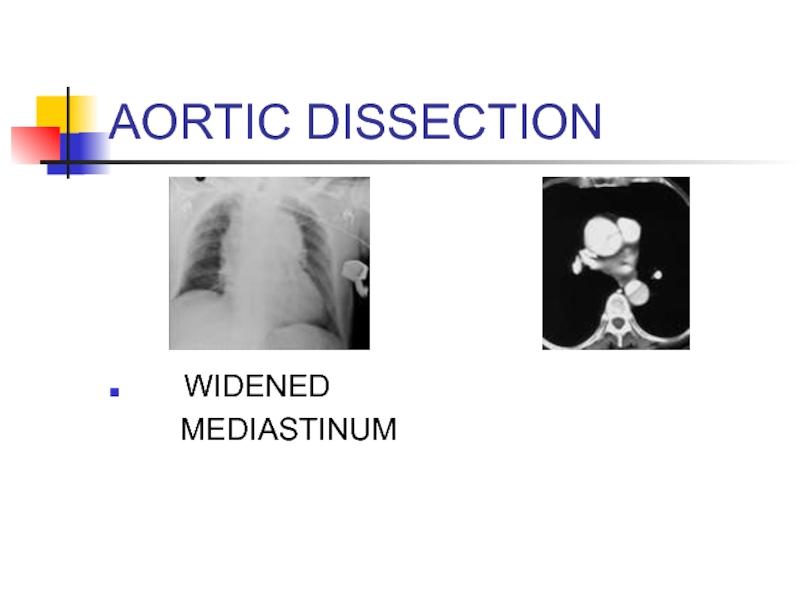
- 84. AORTIC DISSECTION WIDENED MEDIASTINUM
- 85. AORTIC DISSECTION TREATMENT: - ANTIHYPERTENSIVE
- 86. GI CAUSES OF CHEST PAIN .
- 87. ESOPHAGEAL CAUSES REFLUX ESOPHAGITIS ESOPHAGEAL PERFORATION SPASM/MOTILITY DISORDER/
- 88. GERD RISK FACTORS * High
- 89. GERD CLINICAL FEATURES * Burning pain
- 90. ESOPHAGITIS CLINICAL FEATURES *Chest pain
- 91. ESOPHAGEAL PERFORATION CAUSES *Iatrogenic: Endoscopy
- 92. ESOPHAGEAL PERFORATION CLINICAL FEATURES *Acute persistent
- 93. ESOPHAGEAL PERFORATION DIAGNOSIS *x-Ray: May see
- 94. ESOPHAGEAL MOTILITY DISORDERS CLINICAL FEATURES:
- 95. OTHER GI CAUSES In appropriate setting, consider
- 96. PSYCHOLOGIC CAUSES Diagnosis of exclusion
- 97. APPROACH TO THE PATIENT WITH CHEST PAIN PUTTING IT ALL TOGETHER
- 98. INITIAL APPROACH Like everything else: ABCs
- 99. CHEST PAIN: HISTORY Time and character of
- 100. CHEST PAIN: HISTORY TIME AND CHARACTER OF
- 101. CHEST PAIN: HISTORY Quality: *Pleuritic
- 102. CHEST PAIN: HISTORY RADIATION: *
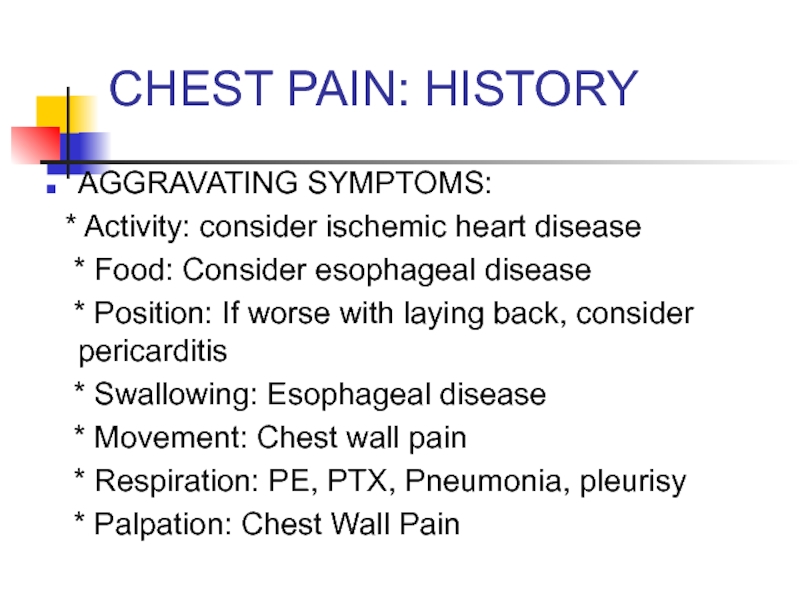
- 103. CHEST PAIN: HISTORY AGGRAVATING SYMPTOMS: *
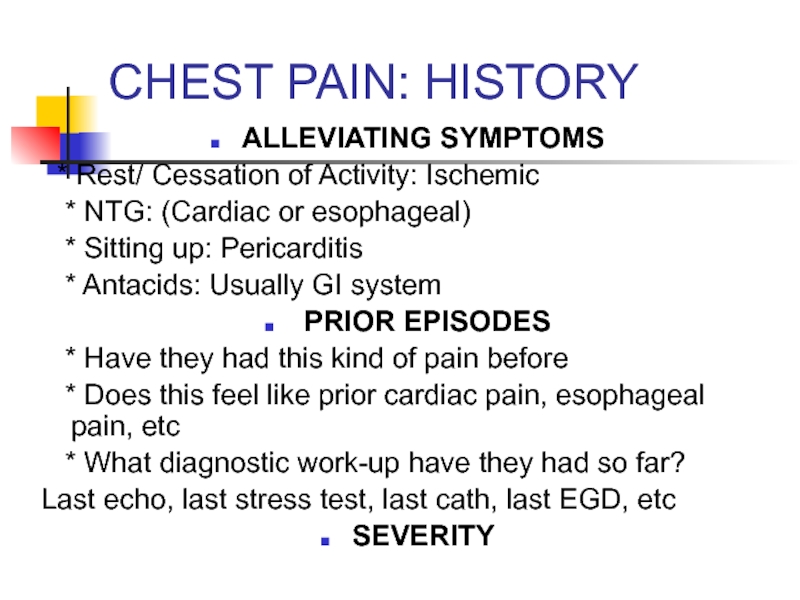
- 104. CHEST PAIN: HISTORY ALLEVIATING SYMPTOMS *
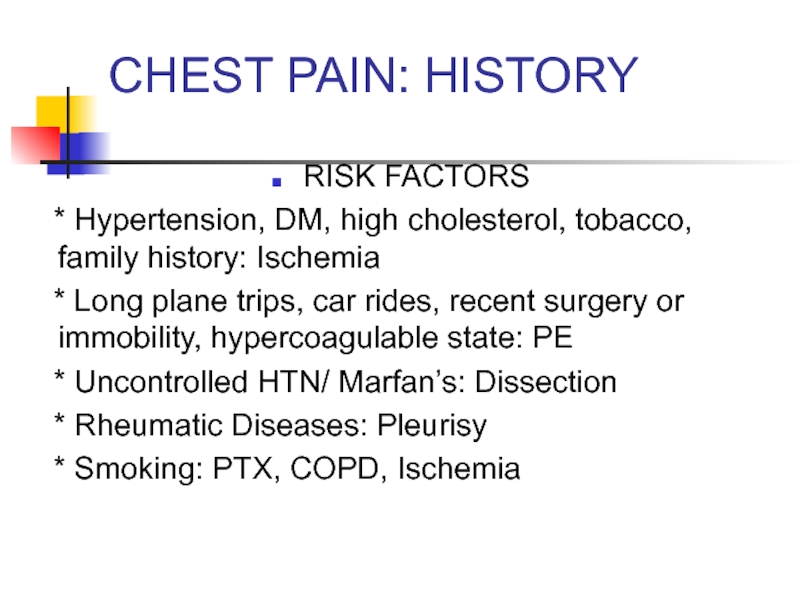
- 105. CHEST PAIN: HISTORY RISK FACTORS
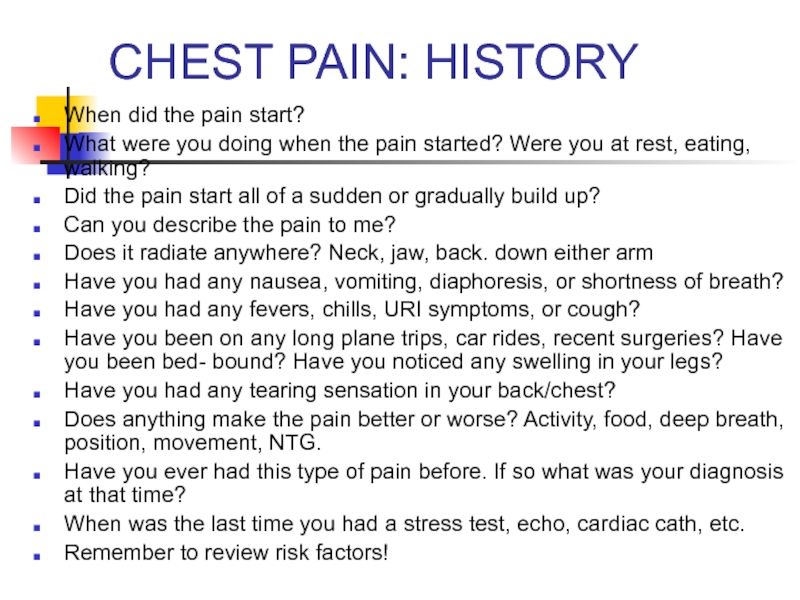
- 106. CHEST PAIN: HISTORY When did the pain
- 107. CHEST PAIN: PHYSICAL EXAM Review vital signs
- 108. CHEST PAIN: PHYSICAL EXAM CV EXAM
- 109. CHEST PAIN: ANCILLARY TESTING LABS: Consider…….
- 110. CHEST PAIN: ANCILLARY TESTS IMAGING: CONSIDER……
- 111. CHEST PAIN Remember, many symptoms overlap. Goal
Слайд 3CHEST PAIN
ANATOMY
DIFFERENTIAL DIAGNOSIS
BRIEF OVERVIEW OF DISEASE PROCESSES CAUSING CHEST PAIN
APPROACH TO
CHEST PAIN
Слайд 4ANATOMY
In devising a differential diagnosis for chest pain, it becomes essential
to review the anatomy of the thorax.
The various components of the thorax can all be responsible for chest pain
The various components of the thorax can all be responsible for chest pain
Слайд 10DIFFERENTIAL DIAGNOSIS OF CHEST PAIN
CHEST WALL PAIN
PULMONARY CAUSES
CARDIAC CAUSES
VASCULAR CAUSES
GI CAUSES
OTHER
(PSYCHOGENIC CAUSES)
Слайд 11DD: CHEST PAIN
CHEST WALL PAIN
1 - Skin and
sensory nerves
-Herpes Zoster
2 - Musculoskeletal system
- Isolated Musculoskeletal Chest Pain Syndrome
*Costochondritis
*Xiphoidalgia
*Precordial Catch Syndrome
*Rib Fractures
- Rheumatic and Systemic Diseases causing
chest wall pain
-Herpes Zoster
2 - Musculoskeletal system
- Isolated Musculoskeletal Chest Pain Syndrome
*Costochondritis
*Xiphoidalgia
*Precordial Catch Syndrome
*Rib Fractures
- Rheumatic and Systemic Diseases causing
chest wall pain
Слайд 12DD: CHEST PAIN
PULMONARY CAUSES
1 - Pulmonary Embolism
2 – Pneumonia
3
- Pneumothorax/ Tension PTX
4 - Pleuritis/Serositis
5 - Sarcoidosis
6 - Asthma/COPD
7 - Lung cancer (rare cases)
4 - Pleuritis/Serositis
5 - Sarcoidosis
6 - Asthma/COPD
7 - Lung cancer (rare cases)
Слайд 13DD: CHEST PAIN
CARDIAC CAUSES
- Coronary Heart Disease
*Myocardial Ischemia
*Unstable Angina
*Angina
- Valvular Heart Disease
*Mitral Valve Prolapse
*Aortic Stenosis
- Pericarditis/Myocarditis
*Unstable Angina
*Angina
- Valvular Heart Disease
*Mitral Valve Prolapse
*Aortic Stenosis
- Pericarditis/Myocarditis
Слайд 15DD: CHEST PAIN
GI CAUSES
-ESOPHAGEAL
*Reflux
* Esophagitis
* Rupture (Boerhaave Syndrome)
* Spasm/Motility Disorder/Foreign Body Secondary to Stricture/Web/Etc
-OTHER
*Consider Pain referred from PUD, Biliary Disease, or Pancreatitis
* Rupture (Boerhaave Syndrome)
* Spasm/Motility Disorder/Foreign Body Secondary to Stricture/Web/Etc
-OTHER
*Consider Pain referred from PUD, Biliary Disease, or Pancreatitis
Слайд 19CHEST WALL PAIN
HERPES ZOSTER
-Reactivation of Herpes Varicellae
-
Immunocompromised patients often
at risk for reactivation.
- 60% of zoster infections involve the trunk
- Pain may precede rash
at risk for reactivation.
- 60% of zoster infections involve the trunk
- Pain may precede rash
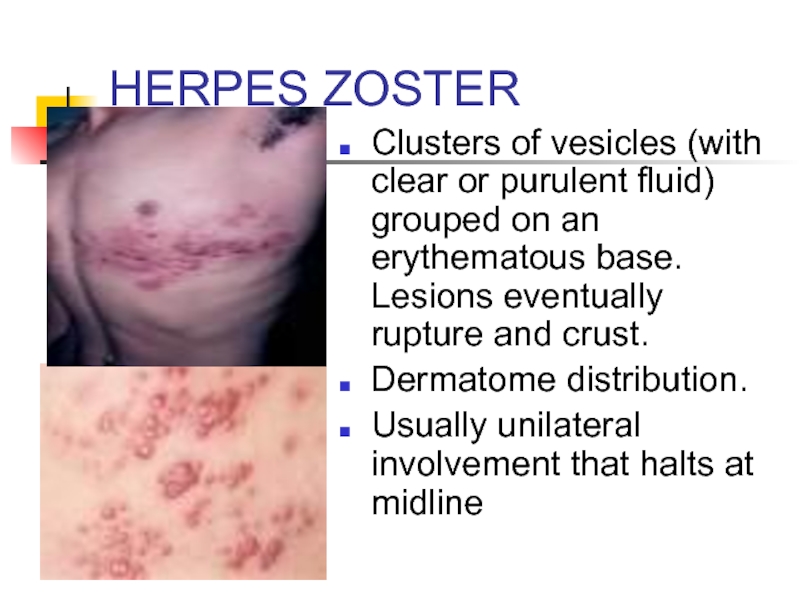
Слайд 20HERPES ZOSTER
Clusters of vesicles (with clear or purulent fluid) grouped on
an erythematous base. Lesions eventually rupture and crust.
Dermatome distribution.
Usually unilateral involvement that halts at midline
Dermatome distribution.
Usually unilateral involvement that halts at midline
Слайд 21HERPES ZOSTER
TREATMENT:
* Antivirals: reduce duration of symptoms; incidence of
postherpatic neuralgia.
* +/- corticosteroids: may reduce inflammation
* Analgesia
POSTHERPETIC NEURALGIA:
* May follow course of acute zoster
* Shooting, acute pain.
* Hyperesthesia in involved dermatome
* Treatment: analgesics, antidepressants, gabapentin
* +/- corticosteroids: may reduce inflammation
* Analgesia
POSTHERPETIC NEURALGIA:
* May follow course of acute zoster
* Shooting, acute pain.
* Hyperesthesia in involved dermatome
* Treatment: analgesics, antidepressants, gabapentin
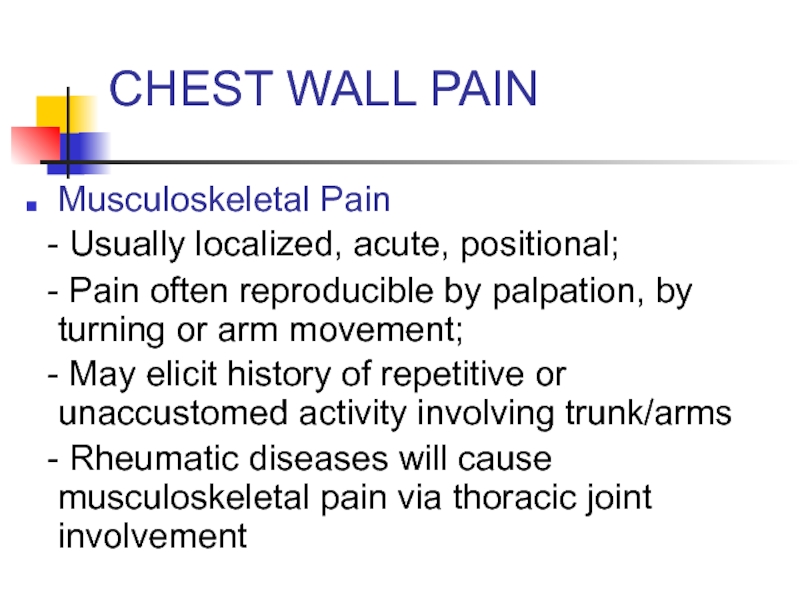
Слайд 22CHEST WALL PAIN
Musculoskeletal Pain
- Usually localized, acute, positional;
- Pain
often reproducible by palpation, by turning or arm movement;
- May elicit history of repetitive or unaccustomed activity involving trunk/arms
- Rheumatic diseases will cause musculoskeletal pain via thoracic joint involvement
- May elicit history of repetitive or unaccustomed activity involving trunk/arms
- Rheumatic diseases will cause musculoskeletal pain via thoracic joint involvement
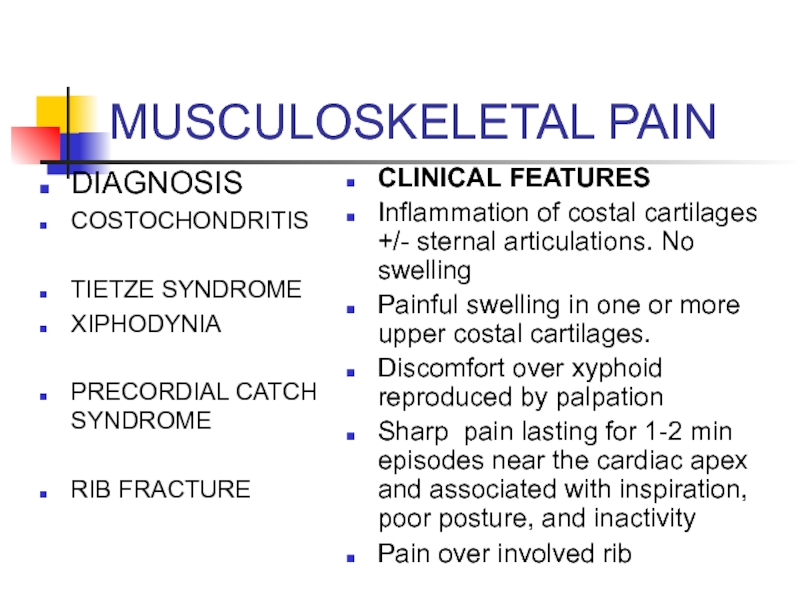
Слайд 23MUSCULOSKELETAL PAIN
DIAGNOSIS
COSTOCHONDRITIS
TIETZE SYNDROME
XIPHODYNIA
PRECORDIAL CATCH SYNDROME
RIB FRACTURE
CLINICAL FEATURES
Inflammation of costal cartilages +/-
sternal articulations. No swelling
Painful swelling in one or more upper costal cartilages.
Discomfort over xyphoid reproduced by palpation
Sharp pain lasting for 1-2 min episodes near the cardiac apex and associated with inspiration, poor posture, and inactivity
Pain over involved rib
Painful swelling in one or more upper costal cartilages.
Discomfort over xyphoid reproduced by palpation
Sharp pain lasting for 1-2 min episodes near the cardiac apex and associated with inspiration, poor posture, and inactivity
Pain over involved rib
Слайд 26PULMONARY EMBOLISM
RISK FACTORS: VIRCHOW’S TRIAD
- Hypercoagulability
*Malignancy
*Pregnancy, Early Postpartum, OCPs, HRT
*Genetic Mutations: Factor V Leiden, Prothrombin, Protein C or S deficiencies, antiphospholipid Ab, etc
- Venous Stasis
* Long distance travel
* Prolonged bed rest or recent hospitalization
* Cast
- Venous Injury:
* Recent surgery or Trauma
*Genetic Mutations: Factor V Leiden, Prothrombin, Protein C or S deficiencies, antiphospholipid Ab, etc
- Venous Stasis
* Long distance travel
* Prolonged bed rest or recent hospitalization
* Cast
- Venous Injury:
* Recent surgery or Trauma
Слайд 27PULMONARY EMBOLISM (PE)
CLINICAL FEATURES
- Shortness of breath
-
Chest pain: often pleuritic
- Tachycardia, tachypnea, hypoxemia
- Hemoptysis, Cough
- Consider diagnosis in new onset A fib
- Look for asymmetric leg swelling (signs of
DVT) which places patients at risk for PE
- If massive PE, may present with hypotension, unstable vital signs, and acute cor pulmonale. Also may present with cardiac arrest (PEA >>asystole).
- Tachycardia, tachypnea, hypoxemia
- Hemoptysis, Cough
- Consider diagnosis in new onset A fib
- Look for asymmetric leg swelling (signs of
DVT) which places patients at risk for PE
- If massive PE, may present with hypotension, unstable vital signs, and acute cor pulmonale. Also may present with cardiac arrest (PEA >>asystole).
Слайд 28PE: DIAGNOSTIC TESTS
ECG:
-Sinus tachycardia most common
- Often see nonspecific abnormalities
- Look for S1 Q3 T3 (S wave in lead I, Q wave in lead III, inverted T wave in lead III)
- Look for S1 Q3 T3 (S wave in lead I, Q wave in lead III, inverted T wave in lead III)
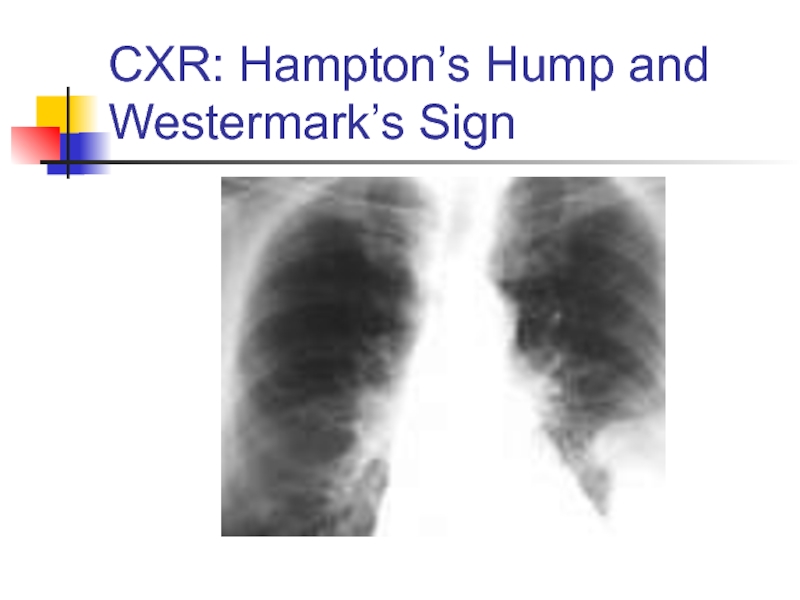
Слайд 30PE: DIAGNOSTIC TESTS
CHEST X-RAY
- Normal in 25% of cases
- Often nonspecific findings
- Look for Hampton’s Hump (triangular pleural based density with apex pointed towards hilum): sign of pulmonary infarction
-Look for Westermark’s sign: Dilation of pulmonary vessels proximal to embolism and collapse distal
- Look for Hampton’s Hump (triangular pleural based density with apex pointed towards hilum): sign of pulmonary infarction
-Look for Westermark’s sign: Dilation of pulmonary vessels proximal to embolism and collapse distal
Слайд 32PE: DIAGNOSTIC TESTS
ABG:
*Look for abnormal PaO2 or
A-a gradient
D-Dimer:
*Often elevated in PE.
* Useful test in low probability patients.
*May be abnormally high in various conditions:
(Malignancy, Pregnancy, sepsis, recent surgery)
D-Dimer:
*Often elevated in PE.
* Useful test in low probability patients.
*May be abnormally high in various conditions:
(Malignancy, Pregnancy, sepsis, recent surgery)
Слайд 34PE: DIAGNOSTIC TESTS
VQ SCAN (Ventilation-Perfusion scan)- use in setting of renal
insufficiency
Helical CT scan with IV contrast
Pulmonary angiography - Gold Standard
Helical CT scan with IV contrast
Pulmonary angiography - Gold Standard
Слайд 35PE: TREATMENT
Initiate Heparin
* Unfractionated Heparin: 80 Units/Kg bolus IV,
then
18units/kg/hr
* Fractionated Heparin (Lovenox): 1mg/kg SubQ BID
* If high pre-test probability for PE, initiate empiric heparin
while waiting for imaging
* Make sure no intraparenchymal brain hemorrhage or GI
hemorrhage prior to initiating heparin.
Consider Fibrinolytic Therapy:
* Especially if PE + hypotension
18units/kg/hr
* Fractionated Heparin (Lovenox): 1mg/kg SubQ BID
* If high pre-test probability for PE, initiate empiric heparin
while waiting for imaging
* Make sure no intraparenchymal brain hemorrhage or GI
hemorrhage prior to initiating heparin.
Consider Fibrinolytic Therapy:
* Especially if PE + hypotension
Слайд 36PNEUMONIA
CLINICAL FEATURES
- Cough +/- sputum production
- Fevers/chills
- Pleuritic chest pain
- Shortness of breath
- May be preceded by viral URI symptoms
- Weakness/malaise/ myalgias
- If severe: tachycardia, tachypnea, hypotension
- Decreased sats
-Abnormal findings on pulmonary auscultation: (rales, decreased breath sounds, wheezing, rhonchi)
- Shortness of breath
- May be preceded by viral URI symptoms
- Weakness/malaise/ myalgias
- If severe: tachycardia, tachypnea, hypotension
- Decreased sats
-Abnormal findings on pulmonary auscultation: (rales, decreased breath sounds, wheezing, rhonchi)
Слайд 37PNEUMONIA: DIAGNOSIS
X-Ray
If patient is to be hospitalized:
Consider GBC (to look for
leukocytosis)
Consider sputum cultures
Consider blood cultures
Consider ABG if in respiratory distress
Consider sputum cultures
Consider blood cultures
Consider ABG if in respiratory distress
Слайд 43PNEUMONIA: TREATMENT
Community- Acquired:
- OUT-PATIENT
*Doxycycline: Low cost
option
* Macrolide
*Newer fluoroquinolone: Moxifloxacin, Levofloxacin, Gatifloxacin
- IN-PATIENT:
* Second or third generation cephalosporin +macrolide
* Fluoroquinolone: Avelox
Nursing Home: * Zosyn + Erythromcyin
* Clindamycin + Cipro
* Macrolide
*Newer fluoroquinolone: Moxifloxacin, Levofloxacin, Gatifloxacin
- IN-PATIENT:
* Second or third generation cephalosporin +macrolide
* Fluoroquinolone: Avelox
Nursing Home: * Zosyn + Erythromcyin
* Clindamycin + Cipro
Слайд 44SPONTANEOUS PNEUMOTHORAX
RISK FACTORS:
- Primary
* No underlying
lung disease
* Young male with greater height to weight ratio
* Smoking: 20:1 relative risk compared to nonsmokers.
-Secondary
* COPD
* Cystic Fibrosis
* AIDS/PCP
* Neoplasms
* Young male with greater height to weight ratio
* Smoking: 20:1 relative risk compared to nonsmokers.
-Secondary
* COPD
* Cystic Fibrosis
* AIDS/PCP
* Neoplasms
Слайд 45PNEUMOTHORAX
CLINICAL FEATURES
- Acute pleuritic chest pain: 95%
-
Usually pain localized to side of PTX
- Dyspnea
- May see tachycardia or tachypnea
- Decreased breath sounds on side of PTX
- Hyperresonance on side of PTX
- If tension PTX, will have above findings + tracheal deviation + unstable vital signs. This is rare complication with spontaneous PTX
- Dyspnea
- May see tachycardia or tachypnea
- Decreased breath sounds on side of PTX
- Hyperresonance on side of PTX
- If tension PTX, will have above findings + tracheal deviation + unstable vital signs. This is rare complication with spontaneous PTX
Слайд 47TENSION PNEUMOTHORAX
Answer: Chest X-ray should have never been obtained
Tension PTX is
a clinical diagnosis requiring immediate life saving measures
Слайд 48Tension Pneumothorax
Trachea deviates to contralateral side
Mediastinum shifts to contralateral side
Decreased breath
sounds and hyperresonance on affected side
JVD
Treatment: Emergent needle decompression followed by chest tube insertion
JVD
Treatment: Emergent needle decompression followed by chest tube insertion
Слайд 49NEEDLE DECOMPRESSION
Insert large bore needle (14 or 16 Gauge) with catheter
in the 2nd intercostal space mid-clavicular line. Remove needle and leave catheter in place. Should hear air.
Слайд 51SPONTANEOUS PTX
TREATMENT:
- If small (
Give oxygen: Increases pleural air absorption
- If large, place chest tube
- If large, place chest tube
Слайд 52PLEURITIS/SEROSITIS
Inflammation of pleura that covers lung
Pleuritic chest pain
Causes:
- Viral
etiology
- SLE
- Rheumatoid Arthritis
- Drugs causing lupus like reaction:
Procainamide, Hydralazine, Isoniazid
- SLE
- Rheumatoid Arthritis
- Drugs causing lupus like reaction:
Procainamide, Hydralazine, Isoniazid
Слайд 53COPD/ASTHMA EXACERBATIONS
CLINICAL FEATURES:
- Decrease in O2 saturations
-
Shortness of Breath
- May see chest pain
- Decreased breath sounds, wheezing, or prolonged expiratory phase on exam
- Look for accessory muscle use (nasal flaring, tracheal tugging, retractions).
Order CXR to r/o associated complications: PTX, pneumonia that may have led to exacerbation
- May see chest pain
- Decreased breath sounds, wheezing, or prolonged expiratory phase on exam
- Look for accessory muscle use (nasal flaring, tracheal tugging, retractions).
Order CXR to r/o associated complications: PTX, pneumonia that may have led to exacerbation
Слайд 54COPD EXACERBATION: TREATMENT
Oxygen: Must prevent hypoxemia. Watch for hypercapnia with O2
therapy
B2 agonist (albuterol)
Anticholinergic (atrovent)
Corticosteroids
Consider Abx if: change in sputum or fever)
If patient is tiring out, not oxygenating well despite O2, developing worsening respiratory acidosis or mental status changes, then intubate.
B2 agonist (albuterol)
Anticholinergic (atrovent)
Corticosteroids
Consider Abx if: change in sputum or fever)
If patient is tiring out, not oxygenating well despite O2, developing worsening respiratory acidosis or mental status changes, then intubate.
Слайд 55ASTHMA TREATMENT
Oxygen
Inhaled short acting B2 agonists: Albuterol
Anticholinergics: Atrovent
Corticosteroids
Magnesium
Systemic B2 agonists: Terbutaline
Heliox
If
tiring (normalization of CO2/ rising CO2 or mental status changes) or poorly oxygenating despite O2, then intubate
Слайд 57RISK FACTORS FOR CAD
Age
Diabetes
Hypertension
Family History
Tobacco Use
Hypercholesterolemia
Cocaine use
Слайд 58ISCHEMIC CHEST PAIN
EXERTIONAL ANGINA
* BRIEF EPISODES BROUGHT ON BY
EXERTION AND RELIEVED BY REST ON NTG
UNSTABLE ANGINA
* NEW ONSET
* CHANGE IN FREQUENCY/SEVERITY
* OCCURS AT REST
AMI
* SEVERE PERSISTENT SYMPTOMS
* ELEVATED TROPONIN
UNSTABLE ANGINA
* NEW ONSET
* CHANGE IN FREQUENCY/SEVERITY
* OCCURS AT REST
AMI
* SEVERE PERSISTENT SYMPTOMS
* ELEVATED TROPONIN
Слайд 59Angina pectoris
Stable angina pectoris is a clinical syndrome characterized by precordial
or anterior chest discomfort, often with radiation to the left shoulder or arm.
The pain typically accompanies physical activity or emotional stress, although many patients with chronic stable angina pectoris have intermittent rest pain.
The pain may radiate to the left side of the neck or jaw.
The pain typically accompanies physical activity or emotional stress, although many patients with chronic stable angina pectoris have intermittent rest pain.
The pain may radiate to the left side of the neck or jaw.
Слайд 60Angina pectoris
The chest discomfort may be described by the patient either
as a true pain or as a variety of symptoms, such as heaviness, squeezing, tightness, pressure, or aching.
True angina is accompanied by some sternal or substernal localization.
Some individuals may experience an associated sensation of dyspnea, which can be the dominant symptom (angina equivalent) in a small number of patients.
True angina is accompanied by some sternal or substernal localization.
Some individuals may experience an associated sensation of dyspnea, which can be the dominant symptom (angina equivalent) in a small number of patients.
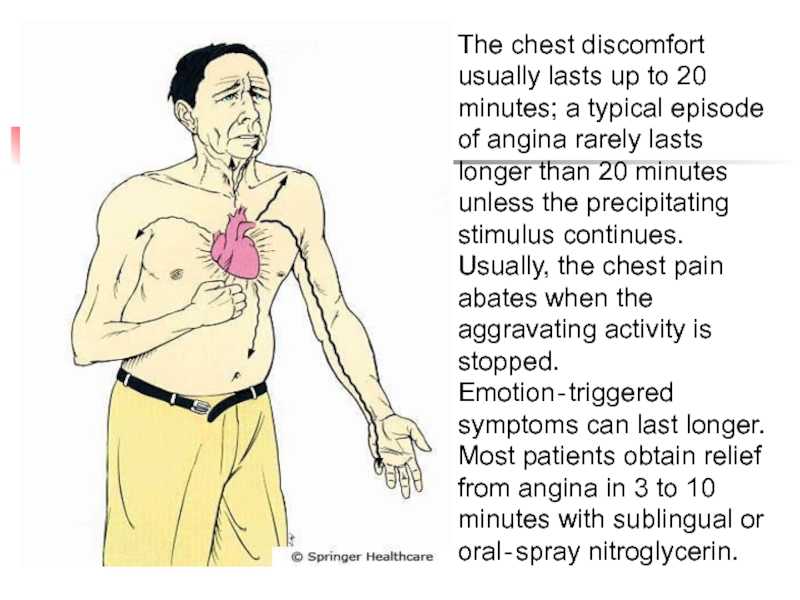
Слайд 61
The chest discomfort usually lasts up to 20 minutes; a typical
episode of angina rarely lasts longer than 20 minutes unless the precipitating stimulus continues. Usually, the chest pain abates when the aggravating activity is stopped. Emotion‐triggered symptoms can last longer. Most patients obtain relief from angina in 3 to 10 minutes with sublingual or oral‐spray nitroglycerin.
Слайд 62ISCHEMIC CHEST PAIN: DIAGNOSIS
12 LEAD EСG
- Look for ST
segment elevation (at least
1mm in two contiguous leads)
- Look for ST segment depression
- Look for T wave inversions
- Look for Q waves
- Look for new LBBB
- Always compare to old EСGs
1mm in two contiguous leads)
- Look for ST segment depression
- Look for T wave inversions
- Look for Q waves
- Look for new LBBB
- Always compare to old EСGs
Слайд 68ISCHEMIC CHEST PAIN: DIAGNOSTIC TESTS
CARDIAC ENZYMES
- Myoglobin
* Will rise within 3 hours, peak within 4-9
hours, and return to baseline within 24 hrs.
- CKMB
* Will rise within 4 hours, peak within 12- 24
hours and return to baseline in 2-3 days
- TROPONIN I
* Will rise within 6 hours, peak in 12 hours
and return to baseline in 3-4 days
hours, and return to baseline within 24 hrs.
- CKMB
* Will rise within 4 hours, peak within 12- 24
hours and return to baseline in 2-3 days
- TROPONIN I
* Will rise within 6 hours, peak in 12 hours
and return to baseline in 3-4 days
Слайд 69ISCHEMIC HEART DISEASE TREATMENT:
ACUTE ST SEGMENT ELEVATION MI
- OXYGEN
-
ASPIRIN (4 BABY ASPIRIN)
- IV NITROGLYCERIN
* Hold for SBP <100
* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting,
*Check rectal exam.
*Check CXR: to r/o dissection
- CATH LAB VS TPA
- IV NITROGLYCERIN
* Hold for SBP <100
* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting,
*Check rectal exam.
*Check CXR: to r/o dissection
- CATH LAB VS TPA
Слайд 70ISCHEMIC HEART DISEASE TREATMENT: NONSTEMI AND UNSTABLE ANGINA
- OXYGEN
-
ASPIRIN (4 BABY ASPIRIN)
- NITROGLYCERIN
* Hold for SBP <100
* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- PLAVIX
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting, *Check rectal exam.
*Check CXR: to r/o dissection
- NITROGLYCERIN
* Hold for SBP <100
* Use cautiously in inferior wall MI. Some of these patients have Right
ventricular involvement which is volume/preload dependent.
- PLAVIX
- BETA BLOCKERS
* Hold for SBP <100 or HR <60
* Hold if wheezing
* Hold if cocaine use (unopposed alpha)
- MORPHINE
- HEPARIN: Before starting, *Check rectal exam.
*Check CXR: to r/o dissection
Слайд 71LOW RISK CARDIAC CHEST PAIN
If low risk chest pain, can consider
serial EСGs and enzymes. If normal, can order stress test in ED if available.
Слайд 72VALVULAR HEART DISEASE
AORTIC STENOSIS
*Classic triad: dyspnea, chest pain, and
syncope
* Harsh systolic ejection murmur at right 2nd intercostal space radiating towards carotids
* Carotid pulse: slow rate of increase
* Brachioradial delay: Delay in pulses between right brachial and right radial arteries
* Try to avoid nitrates: Theses patients are preload dependent
MITRAL VALVE PROLAPSE
* Symptoms include atypical chest pain, palpitations, fatigue, dyspnea
* Often hear mid-systolic click
* Patients with chest pain or palpitations often respond to β-blockers.
* Harsh systolic ejection murmur at right 2nd intercostal space radiating towards carotids
* Carotid pulse: slow rate of increase
* Brachioradial delay: Delay in pulses between right brachial and right radial arteries
* Try to avoid nitrates: Theses patients are preload dependent
MITRAL VALVE PROLAPSE
* Symptoms include atypical chest pain, palpitations, fatigue, dyspnea
* Often hear mid-systolic click
* Patients with chest pain or palpitations often respond to β-blockers.
Слайд 73ACUTE PERICARDITIS
CLINICAL FEATURES
- Acute, stabbing chest pain
- Pleuritic
chest pain
- Pain often referred to left trapezial ridge
- Pain more severe when supine.
- Pain often relieved when sitting up and leaning forward
- Listen for pericardial friction rub
- Pain often referred to left trapezial ridge
- Pain more severe when supine.
- Pain often relieved when sitting up and leaning forward
- Listen for pericardial friction rub
Слайд 74ACUTE PERICARDITIS
COMMON CAUSES
* IDIOPATHIC
* INFECTIOUS
*
MALIGNANCY
* UREMIA
* RADIATION INDUCED
* POST MI (DRESSLER SYNDROME)
* MYXEDEMA
* DRUG INDUCED
* SYSTEMIC RHEUMATIC DISEASES
* UREMIA
* RADIATION INDUCED
* POST MI (DRESSLER SYNDROME)
* MYXEDEMA
* DRUG INDUCED
* SYSTEMIC RHEUMATIC DISEASES
Слайд 75ACUTE PERICARDITIS: DIAGNOSTIC TESTS
ECG
*Look for diffuse ST segment elevation and
PR depression.
* If large pericardial effusion/tamponade, may see low voltage and electrical alternans
X-Ray
* Of limited value.
* Look at size of cardiac silhouette
US
*To look for pericardial effusion
* If large pericardial effusion/tamponade, may see low voltage and electrical alternans
X-Ray
* Of limited value.
* Look at size of cardiac silhouette
US
*To look for pericardial effusion
Слайд 78ACUTE PERICARDITIS
TREATMENT:
- If idiopathic or viral: NSAIDs
-
Otherwise treat underlying pathology
Слайд 79MYOCARDITIS
Inflammation of heart muscle
Frequently accompanied by pericarditis
Fever
Tachycardia out of proportion to
fever
If mild, signs of pericarditis +fevers, myalgias, rigors, headache
If severe, will also see signs of heart failure
May see elevated cardiac enzymes
Treatment: Largely supportive
If mild, signs of pericarditis +fevers, myalgias, rigors, headache
If severe, will also see signs of heart failure
May see elevated cardiac enzymes
Treatment: Largely supportive
Слайд 81AORTIC DISSECTION
RISK FACTORS
- UNCONTROLLED HYPERTENSION
- CONGENITAL HEART
DISEASE
- CONNECTIVE TISSUE DISEASE
- PREGNANCY
- IATROGENIC: S/P AORTIC CATHETERIZATION OR CARDIAC SURGERY
- CONNECTIVE TISSUE DISEASE
- PREGNANCY
- IATROGENIC: S/P AORTIC CATHETERIZATION OR CARDIAC SURGERY
Слайд 82AORTIC DISSECTION
CLINICAL FEATURES
* Abrupt onset of chest pain or pain
between scapulae
* Tearing or ripping pain
* Pain often worst at symptom onset
* As other vessels become affected, will see
- Stroke symptoms: carotid artery involvement
- Tamponade: Ascending dissection into aortic root
- New onset Aortic Regurgitation
- Abdominal/Flank pain/Limb Ischemia: Dissection into abdominal aorta, renal arteries, iliac arteries
- AMI
* Decreased pulsations in radial, femoral, carotid arteries
* Significant blood pressure differences between extremities
* Usually hypertension (but if tamponade, hypotension)
* Tearing or ripping pain
* Pain often worst at symptom onset
* As other vessels become affected, will see
- Stroke symptoms: carotid artery involvement
- Tamponade: Ascending dissection into aortic root
- New onset Aortic Regurgitation
- Abdominal/Flank pain/Limb Ischemia: Dissection into abdominal aorta, renal arteries, iliac arteries
- AMI
* Decreased pulsations in radial, femoral, carotid arteries
* Significant blood pressure differences between extremities
* Usually hypertension (but if tamponade, hypotension)
Слайд 83DIAGNOSIS: AORTIC DISSECTION
CXR: Look for widened mediastinum
CT SCAN:
ANGIOGRAPHY
TEE
** suspected dissectons
must be confirmed radiologically prior to operative repair.
Слайд 85AORTIC DISSECTION
TREATMENT:
- ANTIHYPERTENSIVE THERAPY
*Start with beta
blockers (smell, labetalol)
* Can add vasodilators (nitroprusside) if further BP control is needed ONLY after have achieved HR control with beta-blockers
- If ascending dissection: OR
- If descending: May be able to medically manage
* Can add vasodilators (nitroprusside) if further BP control is needed ONLY after have achieved HR control with beta-blockers
- If ascending dissection: OR
- If descending: May be able to medically manage
Слайд 88GERD
RISK FACTORS
* High food fat
* Caffeine
* Nicotine, alcohol
* Medicines: CCB, nitrates, Anticholinergics
* Pregnancy
* DM
* Scleroderma
* Medicines: CCB, nitrates, Anticholinergics
* Pregnancy
* DM
* Scleroderma
Слайд 89GERD
CLINICAL FEATURES
* Burning pain
* Association with sour taste
in mouth, nausea/vomiting
* May be relieved by antacids
* May find association with food
* May mimic ischemic disease and visa versa
TREATMENT
* Can try GI coctail in ED (30cc Mylanta, 10 cc viscous lidocaine)
* H2 blockers and PPI
* Behavior modification:
- Avoid alcohol, nicotine, caffeine, fatty foods
- Avoiding eating prior to sleep.
- Sleep with Head of Bed elevated.
* May be relieved by antacids
* May find association with food
* May mimic ischemic disease and visa versa
TREATMENT
* Can try GI coctail in ED (30cc Mylanta, 10 cc viscous lidocaine)
* H2 blockers and PPI
* Behavior modification:
- Avoid alcohol, nicotine, caffeine, fatty foods
- Avoiding eating prior to sleep.
- Sleep with Head of Bed elevated.
Слайд 90ESOPHAGITIS
CLINICAL FEATURES
*Chest pain +Odynophagia (pain with swallowing)
Causes
*Inflammatory process:
GERD or med related
*Infectious process: Candida or HSV (often seen in immunocompromised patients)
DIAGNOSIS: Endoscopy with biopsy and culture
TREATMENT: Address underlying pathology
*Infectious process: Candida or HSV (often seen in immunocompromised patients)
DIAGNOSIS: Endoscopy with biopsy and culture
TREATMENT: Address underlying pathology
Слайд 91ESOPHAGEAL PERFORATION
CAUSES
*Iatrogenic: Endoscopy
* Boerhaave Syndrome: Spontaneous rupture secondary
to increased intraesophageal pressure.
- Often presents as sudden onset of chest pain immediately following episode of forceful vomiting
*Trauma
*Foreign Body
- Often presents as sudden onset of chest pain immediately following episode of forceful vomiting
*Trauma
*Foreign Body
Слайд 92ESOPHAGEAL PERFORATION
CLINICAL FEATURES
*Acute persistent chest pain that may radiate to
back, shoulders, neck
* Pain often worse with swallowing
* Shortness of breath
* Tachypnea and abdominal rigidity
* If severe, will see fever, tachycardia, hypotension, subQ emphysema, necrotizing mediastinitis
* Listen for Hammon crunch (pneumomediastinum)
* Pain often worse with swallowing
* Shortness of breath
* Tachypnea and abdominal rigidity
* If severe, will see fever, tachycardia, hypotension, subQ emphysema, necrotizing mediastinitis
* Listen for Hammon crunch (pneumomediastinum)
Слайд 93ESOPHAGEAL PERFORATION
DIAGNOSIS
*x-Ray: May see pleural effusion (usually on left). Also
may see subQ emphysema, pneumomediastinum,pneumothorax
*CT chest
* Esophagram
TREATMENT
*Broad spectrum Antibiotics
*Immediate surgical consultation
*CT chest
* Esophagram
TREATMENT
*Broad spectrum Antibiotics
*Immediate surgical consultation
Слайд 94ESOPHAGEAL MOTILITY DISORDERS
CLINICAL FEATURES:
* Chest pain often induced by
ingestion of liquids at extremes of temperature
* Often will experience dysphagia
DIAGNOSIS:
Esophageal manometry
* Often will experience dysphagia
DIAGNOSIS:
Esophageal manometry
Слайд 95OTHER GI CAUSES
In appropriate setting, consider PUD, Biliary Disease, and Pancreatitis
in differential of chest pain.
Слайд 98INITIAL APPROACH
Like everything else: ABCs
A: Airway
B: Breathing
C: Circulation
IV, O2, cardiac monitor
Vital signs
IV, O2, cardiac monitor
Vital signs
Слайд 99CHEST PAIN: HISTORY
Time and character of onset
Quality
Location
Radiation
Associated symptoms
Aggravating symptoms
Alleviating symptoms
Prior episodes
Severity
Review
risk factors
Слайд 100CHEST PAIN: HISTORY
TIME AND CHARACTER OF ONSET:
* Abrupt onset
with greatest intensity at start:
-Aortic dissection
-PTX
-Occasionally PE will present in this manner
* Chest pain lasting seconds or constant over weeks is not likely to be due to ischemia
-Aortic dissection
-PTX
-Occasionally PE will present in this manner
* Chest pain lasting seconds or constant over weeks is not likely to be due to ischemia
Слайд 101CHEST PAIN: HISTORY
Quality:
*Pleuritic Pain: PE, Pleurisy, Pneumonia, Pericarditis, PTX
*Esophageal: Burning, etc
*MI: squeezing, tightness, pressure, heavy weight on chest. Can also be burning
* acute, tearing, ripping pain: Aortic Dissection
Location:
* If very localized, consider chest wall pain or pain of pleural origin
*MI: squeezing, tightness, pressure, heavy weight on chest. Can also be burning
* acute, tearing, ripping pain: Aortic Dissection
Location:
* If very localized, consider chest wall pain or pain of pleural origin
Слайд 102CHEST PAIN: HISTORY
RADIATION:
* To neck, jaw, down either arm:
consider Ischemia
ASSOCIATED SYMPTOMS:
* Fevers, chills, URI symptoms, productive cough: Pneumonia
* Nausea, vomiting, diaphoresis, shortness of breath: MI
* Shortness of breath: PE, PTX, MI, Pneumonia, COPD / Asthma
* Asymmetric leg swelling: DVT
* With new onset neurologic findings or limb ischemia: consider dissection
* Pain with swallowing, acid taste in mouth: Esophageal disease
ASSOCIATED SYMPTOMS:
* Fevers, chills, URI symptoms, productive cough: Pneumonia
* Nausea, vomiting, diaphoresis, shortness of breath: MI
* Shortness of breath: PE, PTX, MI, Pneumonia, COPD / Asthma
* Asymmetric leg swelling: DVT
* With new onset neurologic findings or limb ischemia: consider dissection
* Pain with swallowing, acid taste in mouth: Esophageal disease
Слайд 103CHEST PAIN: HISTORY
AGGRAVATING SYMPTOMS:
* Activity: consider ischemic heart disease
* Food: Consider esophageal disease
* Position: If worse with laying back, consider pericarditis
* Swallowing: Esophageal disease
* Movement: Chest wall pain
* Respiration: PE, PTX, Pneumonia, pleurisy
* Palpation: Chest Wall Pain
* Position: If worse with laying back, consider pericarditis
* Swallowing: Esophageal disease
* Movement: Chest wall pain
* Respiration: PE, PTX, Pneumonia, pleurisy
* Palpation: Chest Wall Pain
Слайд 104CHEST PAIN: HISTORY
ALLEVIATING SYMPTOMS
* Rest/ Cessation of Activity: Ischemic
* NTG: (Cardiac or esophageal)
* Sitting up: Pericarditis
* Antacids: Usually GI system
PRIOR EPISODES
* Have they had this kind of pain before
* Does this feel like prior cardiac pain, esophageal pain, etc
* What diagnostic work-up have they had so far?
Last echo, last stress test, last cath, last EGD, etc
SEVERITY
* Sitting up: Pericarditis
* Antacids: Usually GI system
PRIOR EPISODES
* Have they had this kind of pain before
* Does this feel like prior cardiac pain, esophageal pain, etc
* What diagnostic work-up have they had so far?
Last echo, last stress test, last cath, last EGD, etc
SEVERITY
Слайд 105CHEST PAIN: HISTORY
RISK FACTORS
* Hypertension, DM, high cholesterol, tobacco,
family history: Ischemia
* Long plane trips, car rides, recent surgery or immobility, hypercoagulable state: PE
* Uncontrolled HTN/ Marfan’s: Dissection
* Rheumatic Diseases: Pleurisy
* Smoking: PTX, COPD, Ischemia
* Long plane trips, car rides, recent surgery or immobility, hypercoagulable state: PE
* Uncontrolled HTN/ Marfan’s: Dissection
* Rheumatic Diseases: Pleurisy
* Smoking: PTX, COPD, Ischemia
Слайд 106CHEST PAIN: HISTORY
When did the pain start?
What were you doing when
the pain started? Were you at rest, eating, walking?
Did the pain start all of a sudden or gradually build up?
Can you describe the pain to me?
Does it radiate anywhere? Neck, jaw, back. down either arm
Have you had any nausea, vomiting, diaphoresis, or shortness of breath?
Have you had any fevers, chills, URI symptoms, or cough?
Have you been on any long plane trips, car rides, recent surgeries? Have you been bed- bound? Have you noticed any swelling in your legs?
Have you had any tearing sensation in your back/chest?
Does anything make the pain better or worse? Activity, food, deep breath, position, movement, NTG.
Have you ever had this type of pain before. If so what was your diagnosis at that time?
When was the last time you had a stress test, echo, cardiac cath, etc.
Remember to review risk factors!
Did the pain start all of a sudden or gradually build up?
Can you describe the pain to me?
Does it radiate anywhere? Neck, jaw, back. down either arm
Have you had any nausea, vomiting, diaphoresis, or shortness of breath?
Have you had any fevers, chills, URI symptoms, or cough?
Have you been on any long plane trips, car rides, recent surgeries? Have you been bed- bound? Have you noticed any swelling in your legs?
Have you had any tearing sensation in your back/chest?
Does anything make the pain better or worse? Activity, food, deep breath, position, movement, NTG.
Have you ever had this type of pain before. If so what was your diagnosis at that time?
When was the last time you had a stress test, echo, cardiac cath, etc.
Remember to review risk factors!
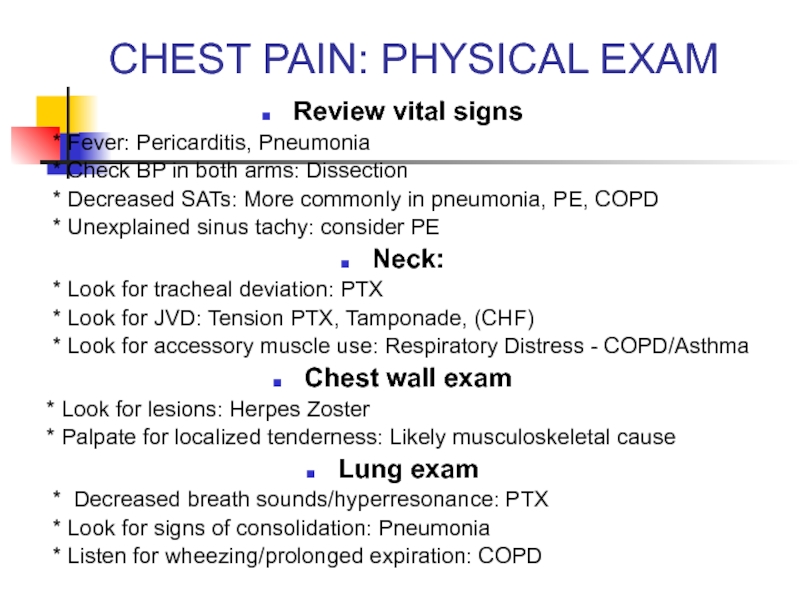
Слайд 107CHEST PAIN: PHYSICAL EXAM
Review vital signs
* Fever: Pericarditis,
Pneumonia
* Check BP in both arms: Dissection
* Decreased SATs: More commonly in pneumonia, PE, COPD
* Unexplained sinus tachy: consider PE
Neck:
* Look for tracheal deviation: PTX
* Look for JVD: Tension PTX, Tamponade, (CHF)
* Look for accessory muscle use: Respiratory Distress - COPD/Asthma
Chest wall exam
* Look for lesions: Herpes Zoster
* Palpate for localized tenderness: Likely musculoskeletal cause
Lung exam
* Decreased breath sounds/hyperresonance: PTX
* Look for signs of consolidation: Pneumonia
* Listen for wheezing/prolonged expiration: COPD
* Check BP in both arms: Dissection
* Decreased SATs: More commonly in pneumonia, PE, COPD
* Unexplained sinus tachy: consider PE
Neck:
* Look for tracheal deviation: PTX
* Look for JVD: Tension PTX, Tamponade, (CHF)
* Look for accessory muscle use: Respiratory Distress - COPD/Asthma
Chest wall exam
* Look for lesions: Herpes Zoster
* Palpate for localized tenderness: Likely musculoskeletal cause
Lung exam
* Decreased breath sounds/hyperresonance: PTX
* Look for signs of consolidation: Pneumonia
* Listen for wheezing/prolonged expiration: COPD
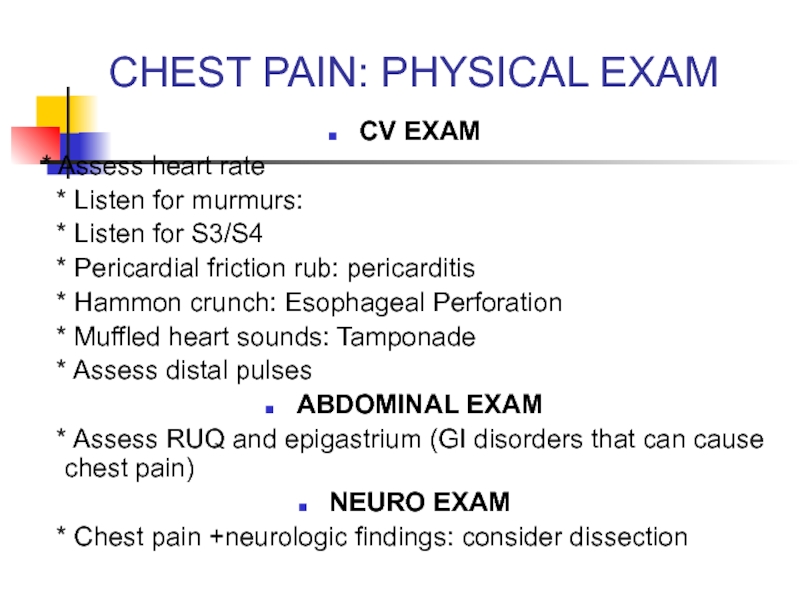
Слайд 108CHEST PAIN: PHYSICAL EXAM
CV EXAM
* Assess heart rate
*
Listen for murmurs:
* Listen for S3/S4
* Pericardial friction rub: pericarditis
* Hammon crunch: Esophageal Perforation
* Muffled heart sounds: Tamponade
* Assess distal pulses
ABDOMINAL EXAM
* Assess RUQ and epigastrium (GI disorders that can cause chest pain)
NEURO EXAM
* Chest pain +neurologic findings: consider dissection
* Listen for S3/S4
* Pericardial friction rub: pericarditis
* Hammon crunch: Esophageal Perforation
* Muffled heart sounds: Tamponade
* Assess distal pulses
ABDOMINAL EXAM
* Assess RUQ and epigastrium (GI disorders that can cause chest pain)
NEURO EXAM
* Chest pain +neurologic findings: consider dissection
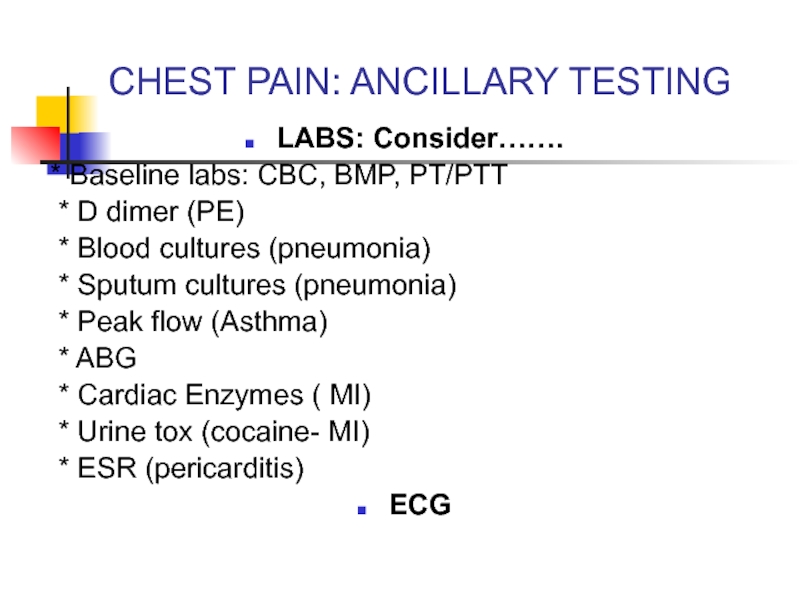
Слайд 109CHEST PAIN: ANCILLARY TESTING
LABS: Consider…….
* Baseline labs: CBC, BMP, PT/PTT
* D dimer (PE)
* Blood cultures (pneumonia)
* Sputum cultures (pneumonia)
* Peak flow (Asthma)
* ABG
* Cardiac Enzymes ( MI)
* Urine tox (cocaine- MI)
* ESR (pericarditis)
ECG
* Blood cultures (pneumonia)
* Sputum cultures (pneumonia)
* Peak flow (Asthma)
* ABG
* Cardiac Enzymes ( MI)
* Urine tox (cocaine- MI)
* ESR (pericarditis)
ECG
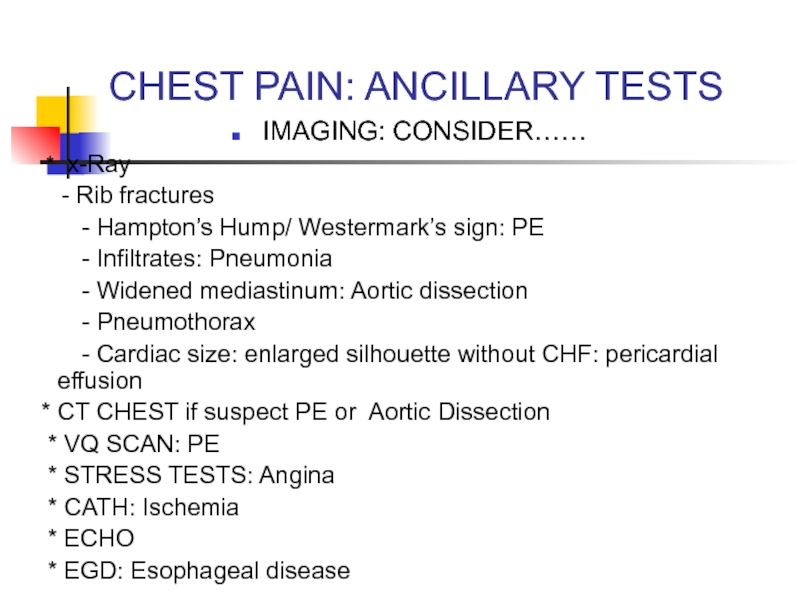
Слайд 110CHEST PAIN: ANCILLARY TESTS
IMAGING: CONSIDER……
* x-Ray
-
Rib fractures
- Hampton’s Hump/ Westermark’s sign: PE
- Infiltrates: Pneumonia
- Widened mediastinum: Aortic dissection
- Pneumothorax
- Cardiac size: enlarged silhouette without CHF: pericardial effusion
* CT CHEST if suspect PE or Aortic Dissection
* VQ SCAN: PE
* STRESS TESTS: Angina
* CATH: Ischemia
* ECHO
* EGD: Esophageal disease
- Hampton’s Hump/ Westermark’s sign: PE
- Infiltrates: Pneumonia
- Widened mediastinum: Aortic dissection
- Pneumothorax
- Cardiac size: enlarged silhouette without CHF: pericardial effusion
* CT CHEST if suspect PE or Aortic Dissection
* VQ SCAN: PE
* STRESS TESTS: Angina
* CATH: Ischemia
* ECHO
* EGD: Esophageal disease
Слайд 111CHEST PAIN
Remember, many symptoms overlap.
Goal in ED is to r/o life
threatening causes of chest pain
With appropriate history, physical exam, and ancillary tests, rule out
* Pneumothorax
* Aortic Dissection
* PE
* Unstable Angina
* MI
* Esophageal Perforation
With appropriate history, physical exam, and ancillary tests, rule out
* Pneumothorax
* Aortic Dissection
* PE
* Unstable Angina
* MI
* Esophageal Perforation