- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
The Science of Patient Safety презентация
Содержание
- 1. The Science of Patient Safety
- 2. Objectives Outline major principles for systems
- 3. CASE #1 35 year old male Seeking
- 4. CASE #2 • 52 year old patient
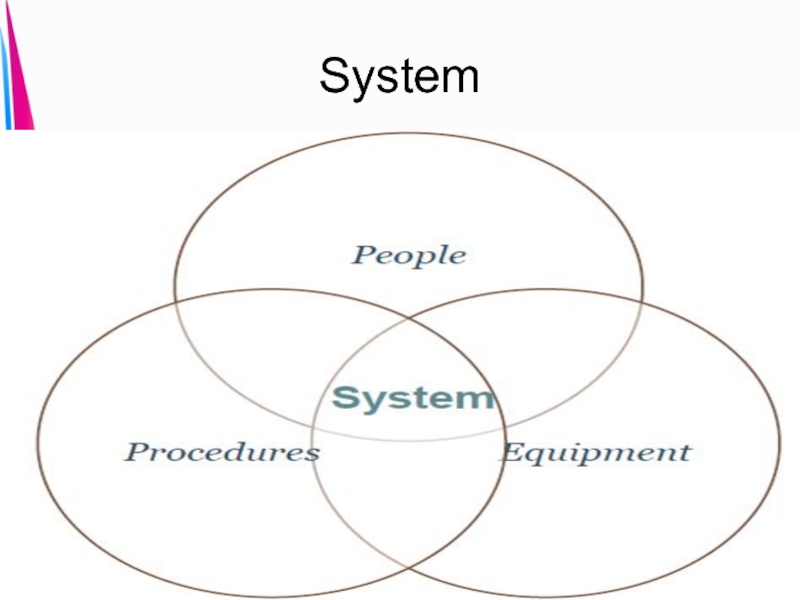
- 5. System
- 6. Hazards • Hazard activities (i.e., behaviors)
- 7. 44,000- 98,0000
- 8. Healthcare World before 1999-2000 • Quality/safety assumed
- 9. Healthcare World Now • Growing business case
- 10. Why Is This So Hard? • Medicine
- 11. Definition of Insanity Insanity: doing the
- 12. Error Causation and Prevention Most preventable harm
- 13. Human Error – James Reason
- 15. Systems Thinking Refers to thinking in terms of: Interdependencies Interactions Sequences
- 16. Systems Thinking Provides a conceptual framework to
- 17. Reliability Science Definition of Reliability: “the
- 18. High Reliability Organization (HRO) Organizations despite functioning
- 19. PRINCIPLES OF RELIABILITY SCIENCE Anticipation: used
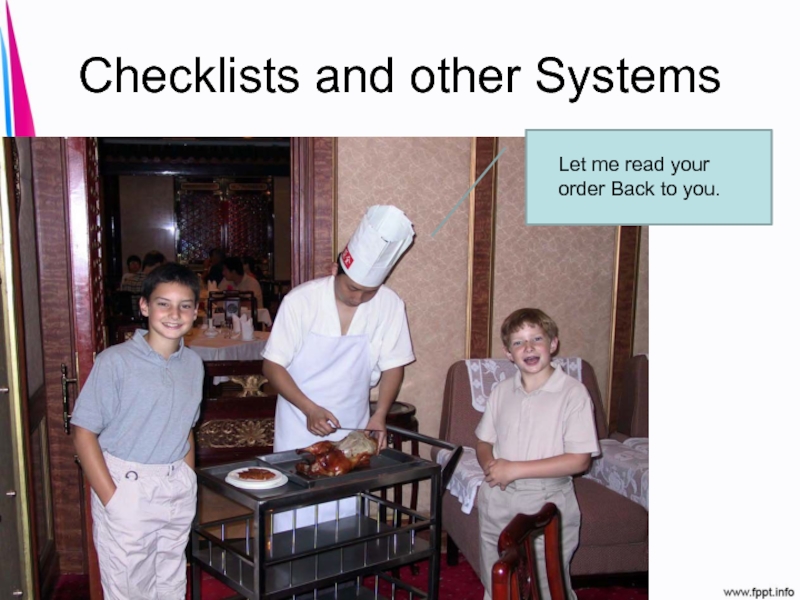
- 20. Checklists and other Systems Let me read your order Back to you.
- 21. The Culture of Low Expectations “We suspect
- 22. Human Factors • Human factors engineering
- 23. Sleep Deprivation
- 24. Interruptions
- 25. Memory Issues
- 26. Forcing Functions Be more careful, or…. Redesign the breaks
- 27. Error Proofing 1. Simplification 2. Standardization 3.
- 28. Error Proofing 6. Use visual controls
- 29. PI approaches Common Characters Planned Systematic Collaborative Organization-wide
- 30. Planned ORGANIZED DOCUMENTED
- 31. Systematic PLANNING PRIORITIZATION ASSESSMENT IMPLEMENTING MAINTENANCE
- 32. ORGANIZATION WIDE ALL LEADERS ENTIRE ORGANIZATION IMPORTANT FUNCTIONS
- 33. COLLABORATIVE DEPARTMENTS SETTINGS DISCIPLINES
- 34. Model for Improvement Three Questions 1)
- 35. SHEWHART (PDCA) AND DEMING MODEL (PDSA) P
- 36. Shewhart Cycle Plan Do Check Act
- 38. FOCUS – PDCA MODEL F = FIND
- 39. F.O.C.U.S. Find an improvement project (initiative):
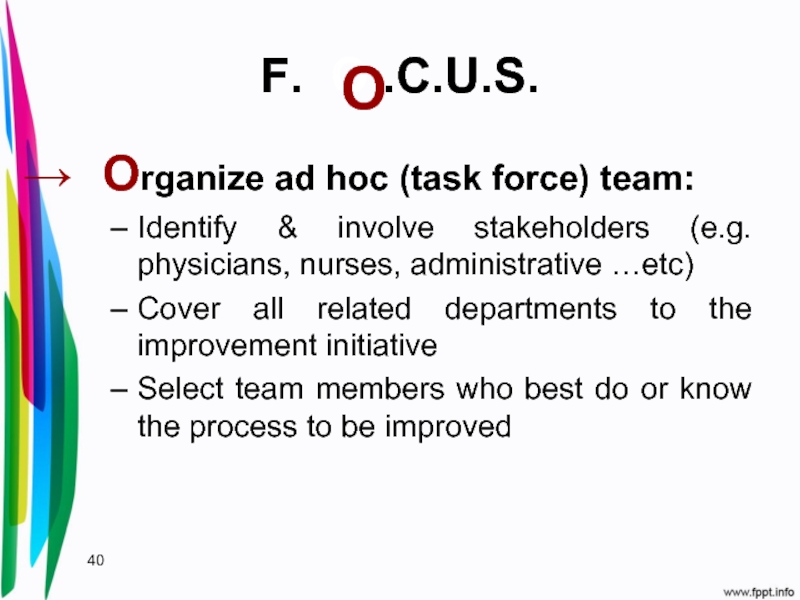
- 40. F. O .C.U.S. Organize ad hoc (task
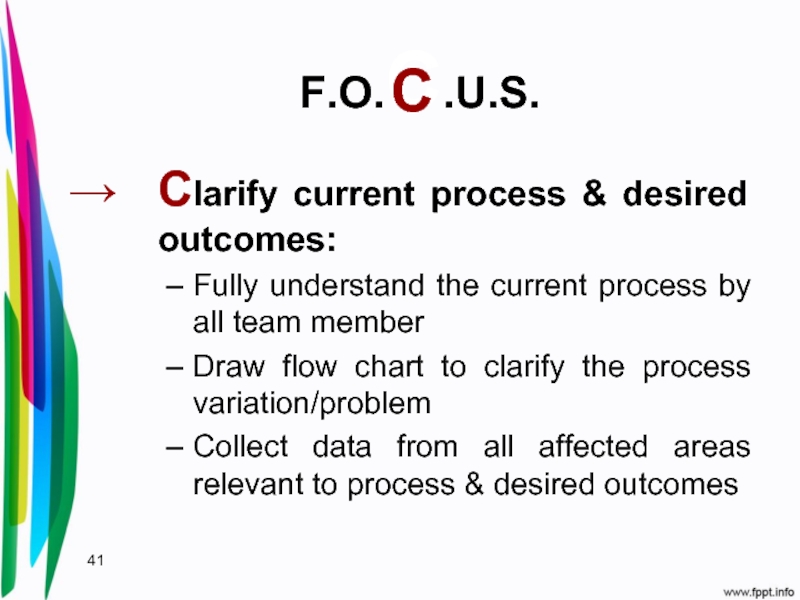
- 41. F.O.C.U.S. Clarify current process & desired outcomes:
- 42. F.O.C.U.S. Understand Process Variation, Root Causes & Desired Outcomes
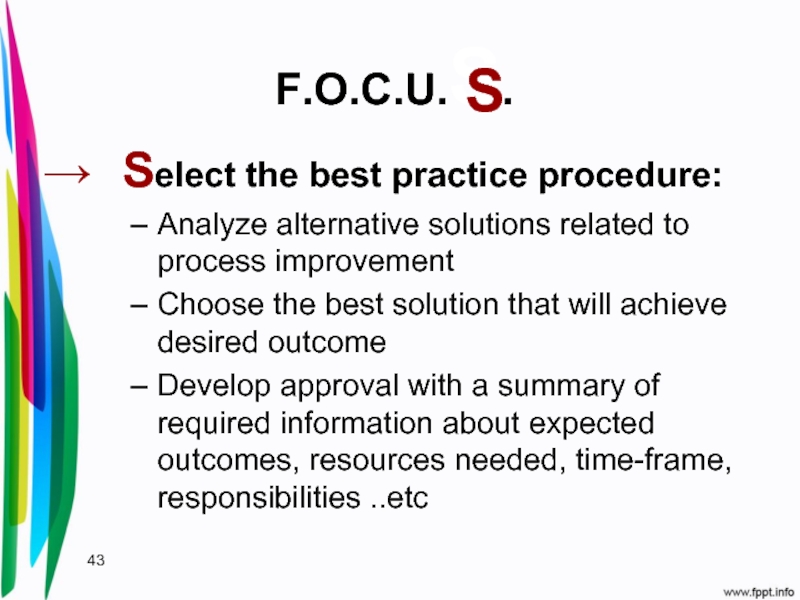
- 43. F.O.C.U.S. Select the best practice procedure: Analyze
- 44. P.D.C.A. Plan the improvement project:
- 45. P.D.C.A. Do the improvement project:
- 46. P.D.C.A. Check the results:
- 47. P.D.C.A. Act to hold gains or re-adjust FOCUS_PDCA
- 48. Lean Methodology LEAN: An effective approach for
- 49. Focus Area of Lean Lean: Lean pioneered
- 50. Six Sigma
- 51. Core Attributes for Safe, Reliable Systems •
- 52. The Science of Patient Safety • New
- 53. “We think that the anxiety, demoralization,
Слайд 2Objectives
Outline major principles for systems thinking and reliable design
Describe human
Differentiate improvement models that have been utilized outside and inside of the healthcare industry
Слайд 3CASE #1
35 year old male
Seeking opthamology referral
Lab results for a different
Слайд 6Hazards
• Hazard activities (i.e., behaviors) or conditions that pose threat of
• Sometimes hazards lie hidden in the system, and sometimes they are quite obvious
Слайд 8Healthcare World before 1999-2000
• Quality/safety assumed to be excellent.
• No business
• No local expertise, research or best practices.
• Little concerted effort by board, C-suite or physicians to improve quality/safety
• Combination of wrong mental model and no incentive leads to predictable results
Слайд 9Healthcare World Now
• Growing business case for safety/quality
• Steady progression from
transparency), eventually settling on “all of the above”
plus payment changes
• Capacity building: people, tools, measures and IT
• Transition from quality/safety to value
• Recognition of need to remake delivery system to
survive/succeed in new healthcare world
Слайд 10Why Is This So Hard?
• Medicine is complex
• High degree of
• Care across the continuum is challenging
• Diversity of workforce and
complexity of patients
Слайд 11Definition of Insanity
Insanity: doing the same thing over and over
Albert Einstein
Слайд 12Error Causation and Prevention
Most preventable harm to patients receiving healthcare today
Слайд 16Systems Thinking
Provides a conceptual framework to help see and understand relationships
Helps
Focus on interdependencies
Слайд 17Reliability Science
Definition of Reliability:
“the extent to which an experiment, test,
By Institute for Healthcare Improvement
“Failure free operation over time”
Relation to IOM’s aims: effectiveness, timeliness, and patient-centeredness.
Слайд 18High Reliability Organization (HRO)
Organizations despite functioning in complex, hazardous environments, have
Examples: airline industry, nuclear power, chemical plants, aircraft carriers.
One small error can lead to catastrophic consequences for not only the employees but also for the general public.
Слайд 19PRINCIPLES OF RELIABILITY SCIENCE
Anticipation: used to detect an error before it
Containment: control the consequences of errors
Слайд 21The Culture of Low Expectations
“We suspect that these physicians and nurses
Drs. Mark Chassin and Elise Becher
Annals of Internal Medicine, 2002
Слайд 22Human Factors
• Human factors engineering focuses on human beings and
• Human factors leverages what we know about human behavior, abilities, limitations, and other characteristics to ensure safer, more reliable outcomes.
Слайд 27Error Proofing
1. Simplification
2. Standardization
3. Reduce reliance on memory
4. Improve access to
5. Use forcing functions and constraints
Слайд 28Error Proofing
6. Use visual controls
7. Leverage high-performance teams
8. Deploy redundancies
9.
10. Make errors more visible
Слайд 34Model for Improvement
Three Questions
1) What is the aim?
2) How will
improvement?
3) What changes can we make that will result in
an improvement?
Слайд 36Shewhart Cycle
Plan
Do
Check
Act
Identify customer
needs/expectations
Describe the
Measure and
analyze data
Identify improvement
opportunities
Identify root causes
of problems
Generate and choose
solutions
Plan and implement
a pilot of the solutions
Evaluate results of pilot
Draw conclusions
Standardize the change
Monitor the change
and hold the gains
The Tradiotnal PDCA Model
Слайд 38FOCUS – PDCA MODEL
F = FIND A PROBLEM
O = ORGANIZE TEAM
C
U = UNDERSTAND SOURCES OF VARIATION
S = SELECT THE PROCESS IMPROVEMENT
PLAN THE NECESSARY STEPS
DO ALL NECESSARY TO IMPLEMENT
CHECK THE RESULT OF ACTION
ACT FULLY IMPLEMENT
(Useful for REDESIGN of a new process or QI)
Слайд 39F.O.C.U.S.
Find an improvement project (initiative):
Review related standards & documents
Analysis
Identify problems & desired outcomes
Слайд 40F. O .C.U.S.
Organize ad hoc (task force) team:
Identify & involve stakeholders
Cover all related departments to the improvement initiative
Select team members who best do or know the process to be improved
O
Слайд 41F.O.C.U.S.
Clarify current process & desired outcomes:
Fully understand the current process by
Draw flow chart to clarify the process variation/problem
Collect data from all affected areas relevant to process & desired outcomes
C
Слайд 43F.O.C.U.S.
Select the best practice procedure:
Analyze alternative solutions related to process improvement
Choose
Develop approval with a summary of required information about expected outcomes, resources needed, time-frame, responsibilities ..etc
S
Слайд 48Lean Methodology
LEAN: An effective approach for improving patient safety by process
Слайд 49Focus Area of Lean
Lean:
Lean pioneered by Toyota, focuses on the efficient
Focus areas:
Remove non-value added steps to:
Reduce cycle time
Improve quality
Align production with demand
Reduce inventory
Improve process safety and efficiency
Слайд 51Core Attributes for Safe, Reliable Systems
• Well-defined workflows
• Mistake-proofing principles
• Measurement
• Team members who share responsibility to provide safe, reliable care
Слайд 52The Science of Patient Safety
• New concepts: science of error causation
• New attitudes: teamwork, discipline, professionalism, balancing “no blame” with accountability, disclosure…
• New skills: error analysis, leadership, change management...
Слайд 53
“We think that the anxiety, demoralization, and sense of loss of
Berwick and Finkelstein, Acad Med, 2010