- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
systemic diseases and the eye презентация
Содержание
- 1. systemic diseases and the eye
- 2. ENDOCRINE DISORDERS AND THE EYE
- 3. FOREWORD The eye is a mirror which
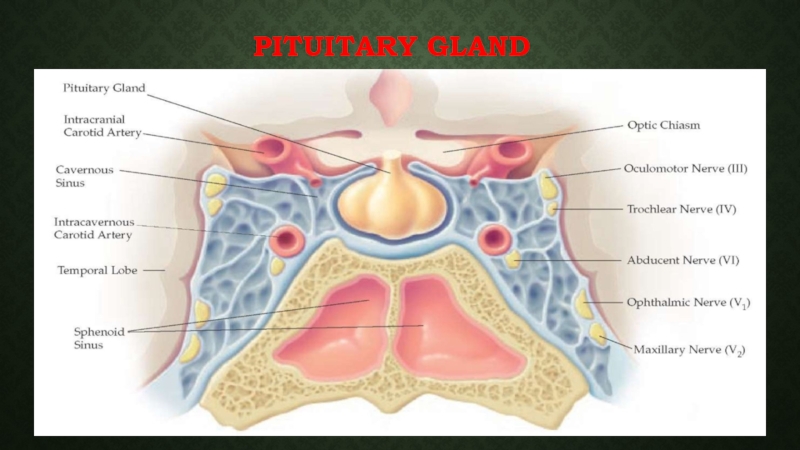
- 5. PITUITARY GLAND
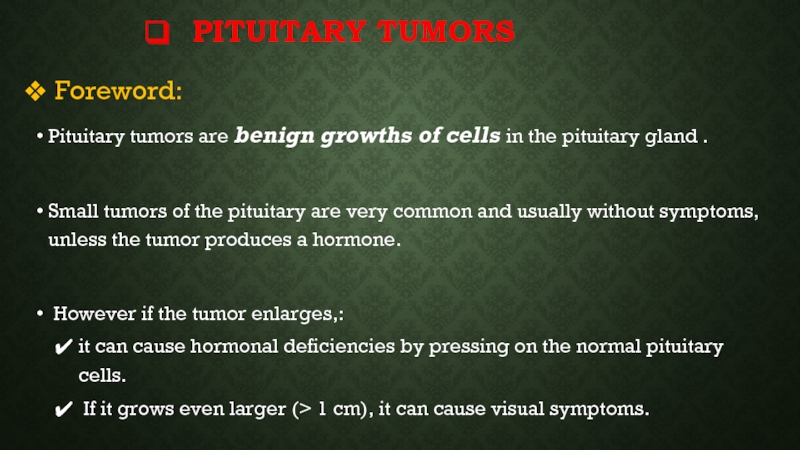
- 6. PITUITARY TUMORS Foreword: Pituitary tumors are
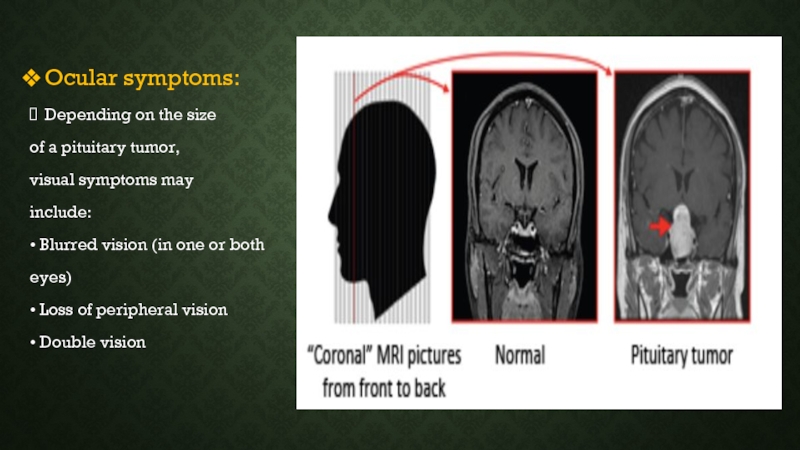
- 7. Ocular symptoms: Depending on the size
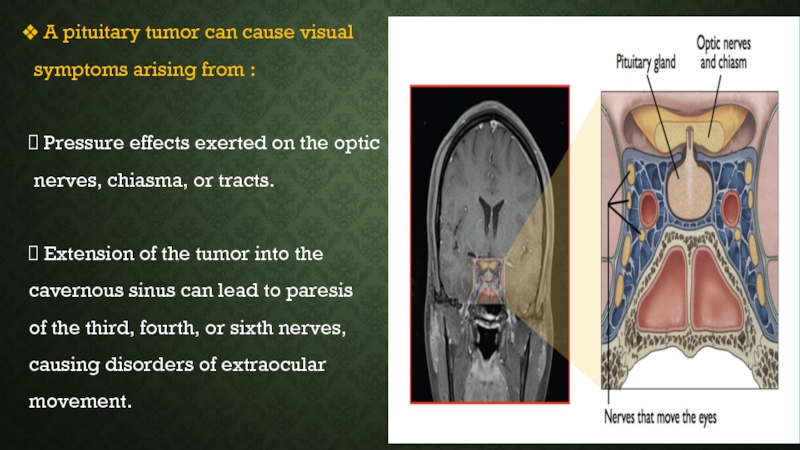
- 8. A pituitary tumor can cause visual
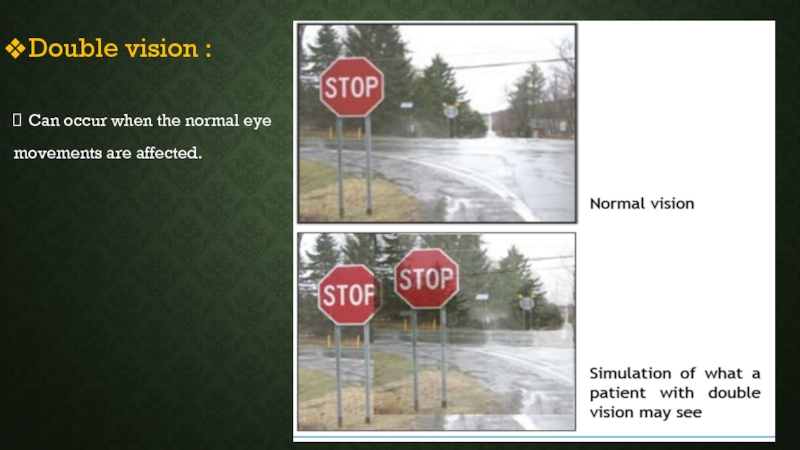
- 9. Double vision : Can occur when the normal eye movements are affected.
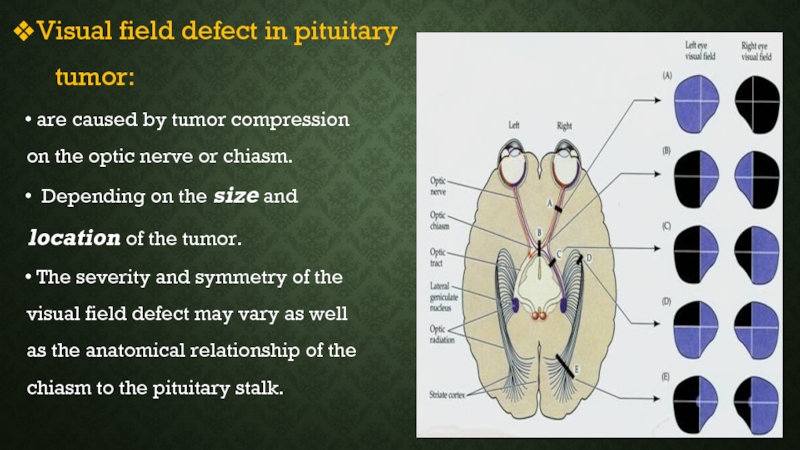
- 10. Visual field defect in pituitary
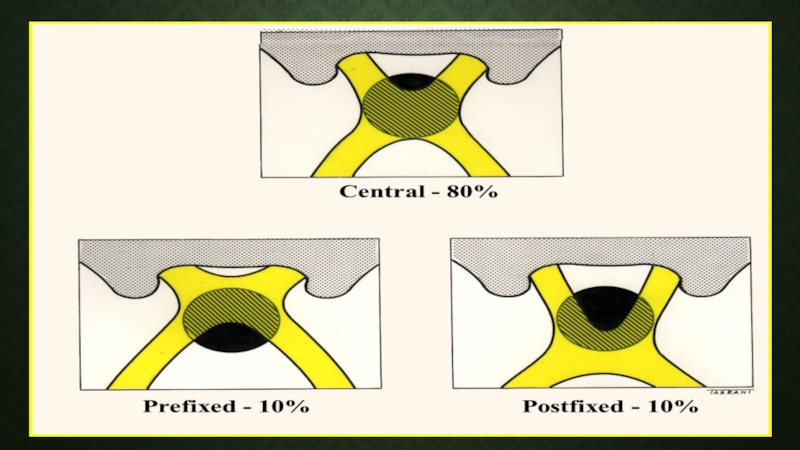
- 12. TYPES OF VISUAL FIELD DEFECT Monocular
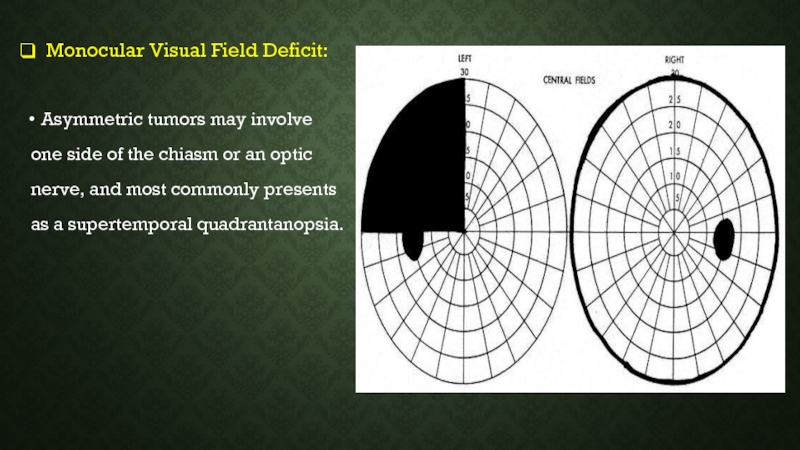
- 13. Monocular Visual Field Deficit: Asymmetric
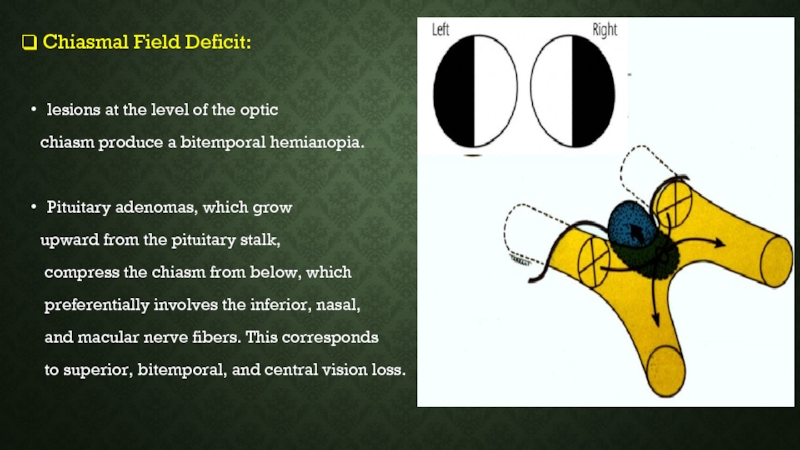
- 14. Chiasmal Field Deficit: lesions at
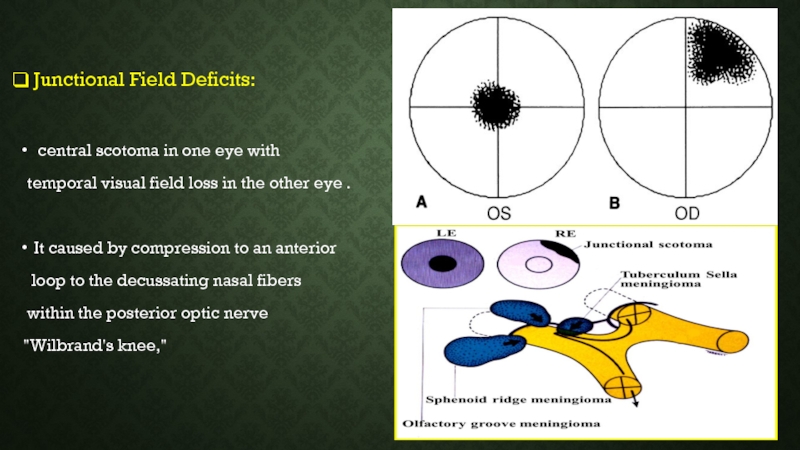
- 15. Junctional Field Deficits: central
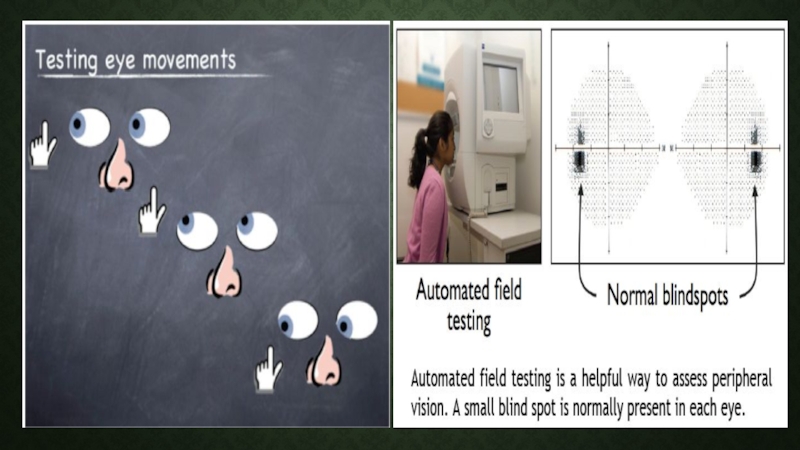
- 16. Diagnosis: The doctor will examine: •
- 17. Papilledema is a rare finding in
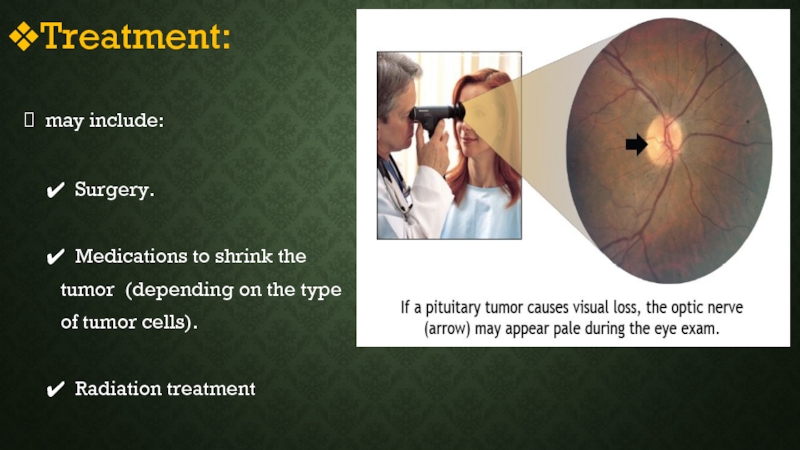
- 19. Treatment: may include:
- 20. Treatments for double vision include:
- 21. Prognosis: Visual loss : often improve after
- 22. The three phases of improvement
- 23. the most common Hypothalmic –pituitary syndromes
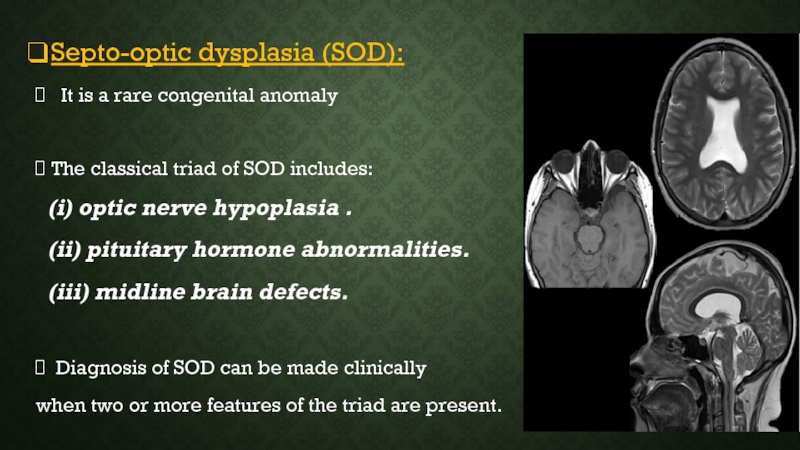
- 24. Septo-optic dysplasia (SOD): It is
- 25. Ocular manifestations: varying degrees of visual
- 26. Kallman's syndrome: A rare genetic
- 27. Empty sella syndrome: Is defined
- 29. Ocular manifestations: Diminished visual acuity .
- 30. Oliver Mcfarlane syndrome:
- 31. THYROID EYE DISEASES Foreword:
- 32. GRAVES’ DISEASE Foreword:
- 33. Clinical features: I. Eye features.
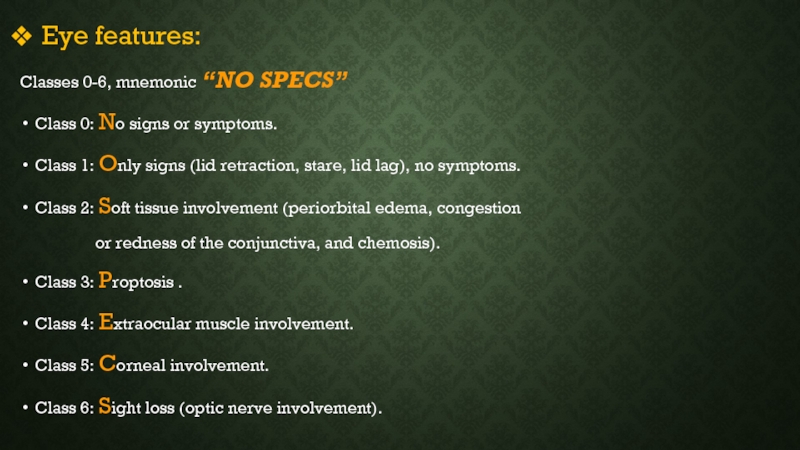
- 34. Eye features: Classes 0-6, mnemonic “NO
- 35. Lid lag
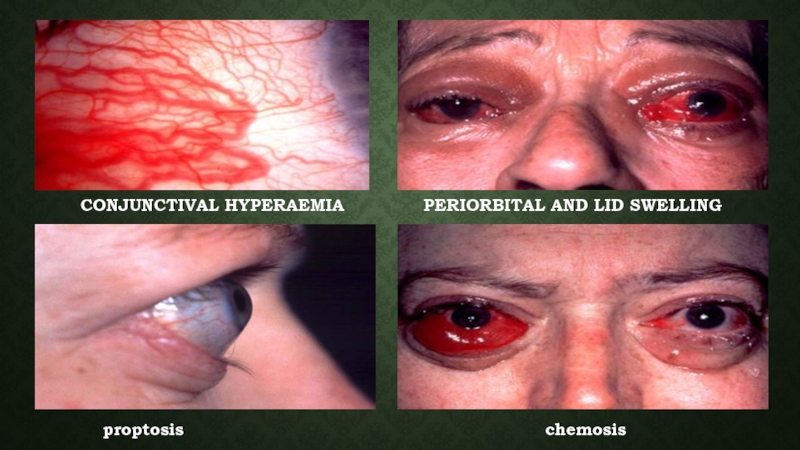
- 36. CONJUNCTIVAL HYPERAEMIA
- 37. Diagnosis: Low TSH, High FT4
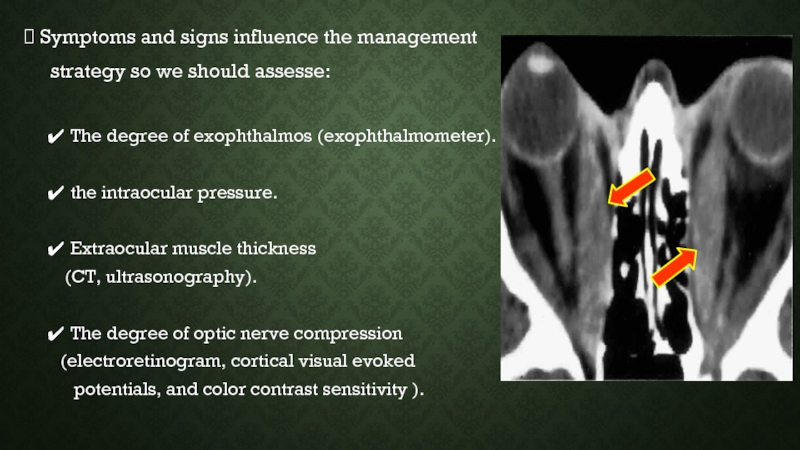
- 38. Symptoms and signs influence the management
- 39. Treatment: Medical therapy. Surgical therapy. Radioactive iodine therapy.
- 40. Management of opthalmopathy: Management
- 41. For more severely affected eyes, immunosuppressive
- 43. periorbital swelling loss of the outer third of the eyebrow.
- 44. PARATHYROID EYE DISEASE There are four
- 45. Hyperparathyroidism: Hyperparathyroidism may be subdivided
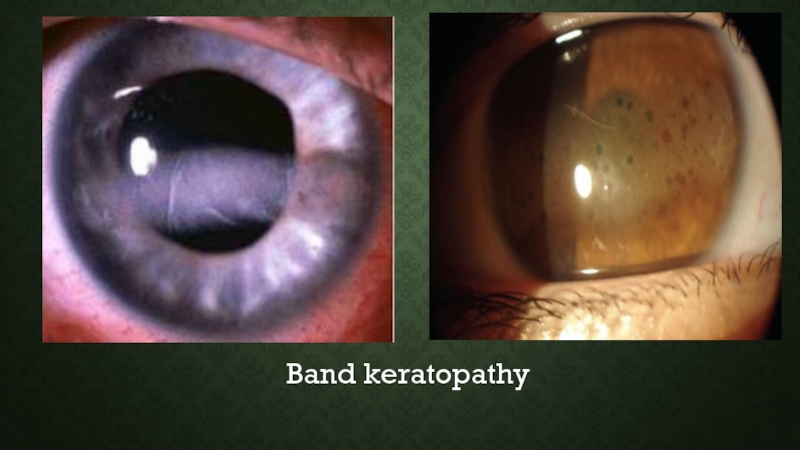
- 46. Band keratopathy
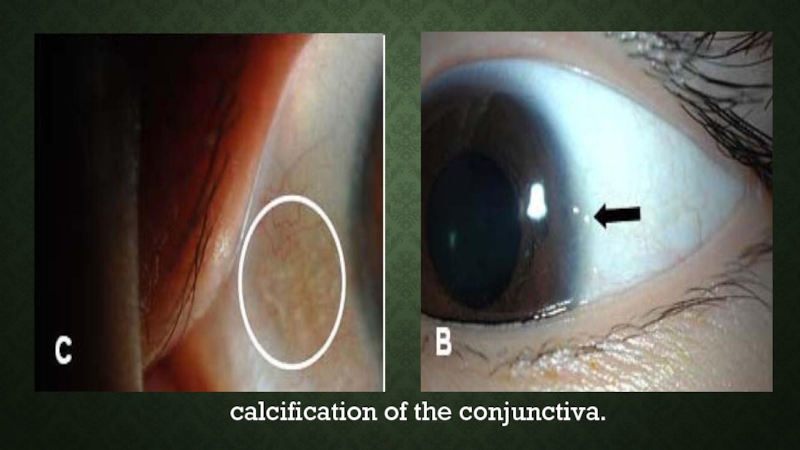
- 47. calcification of the conjunctiva.
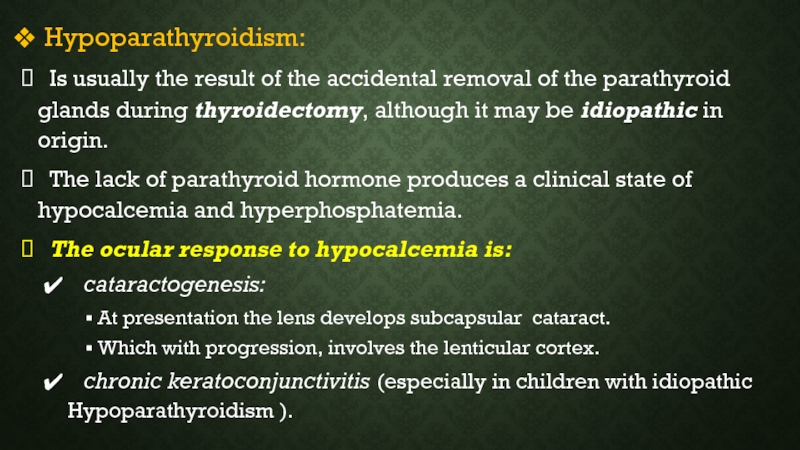
- 48. Hypoparathyroidism: Is usually the result
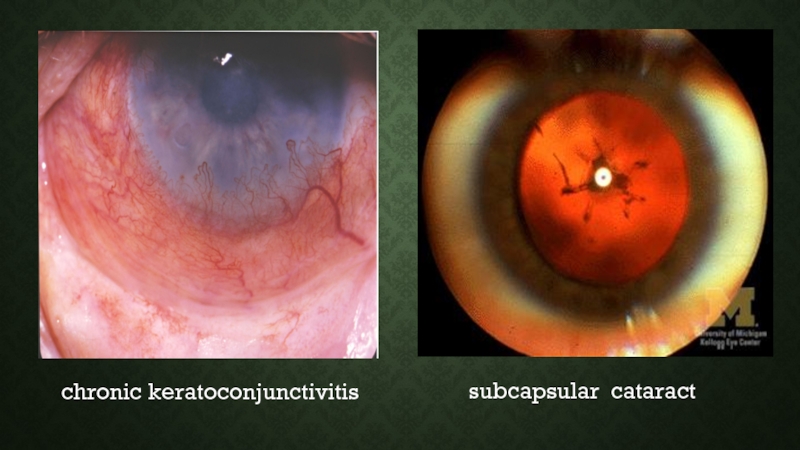
- 49. subcapsular cataract chronic keratoconjunctivitis
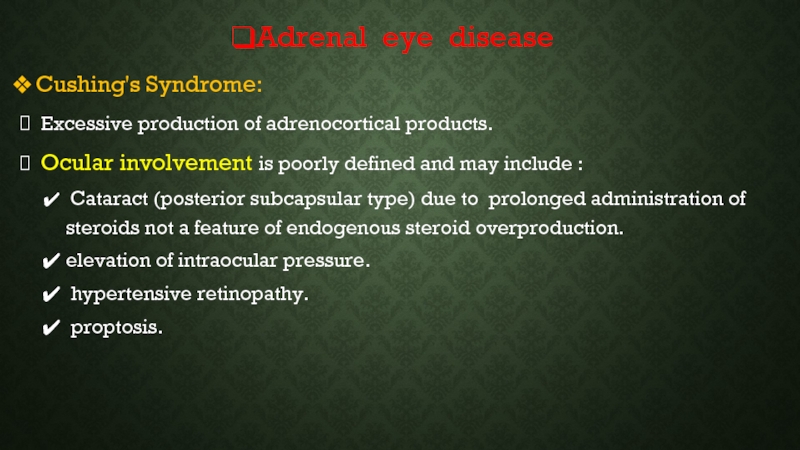
- 50. Adrenal eye disease Cushing's Syndrome: Excessive
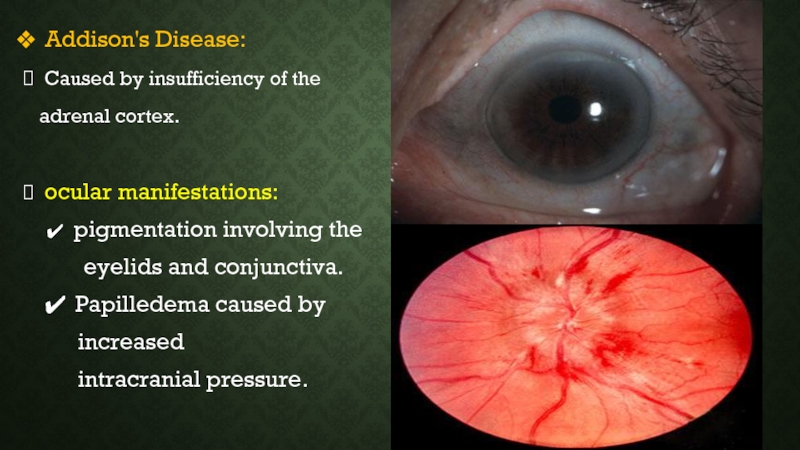
- 51. Addison's Disease: Caused by insufficiency
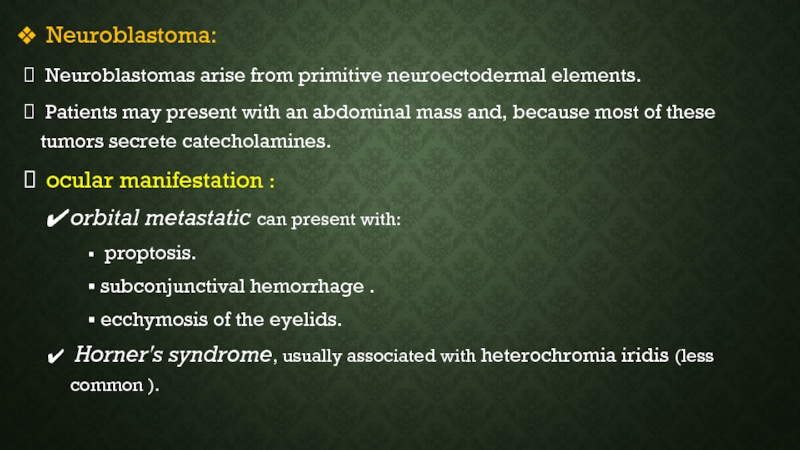
- 52. Neuroblastoma: Neuroblastomas arise from primitive
- 53. ecchymosis of the eyelids heterochromia iridis
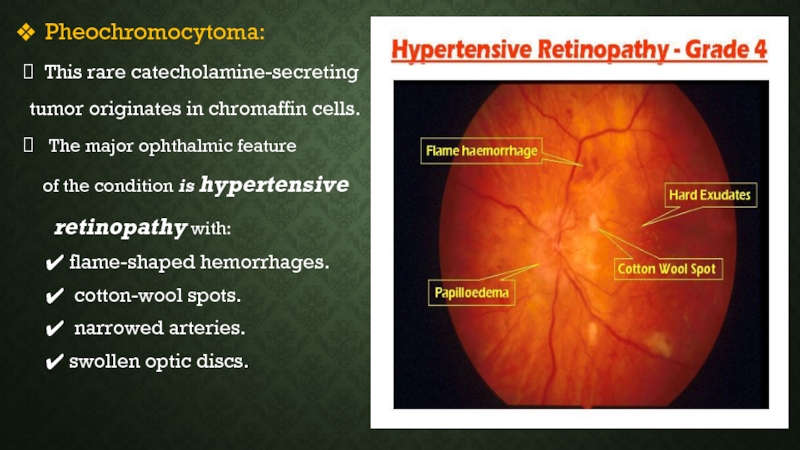
- 54. Pheochromocytoma: This rare catecholamine-secreting
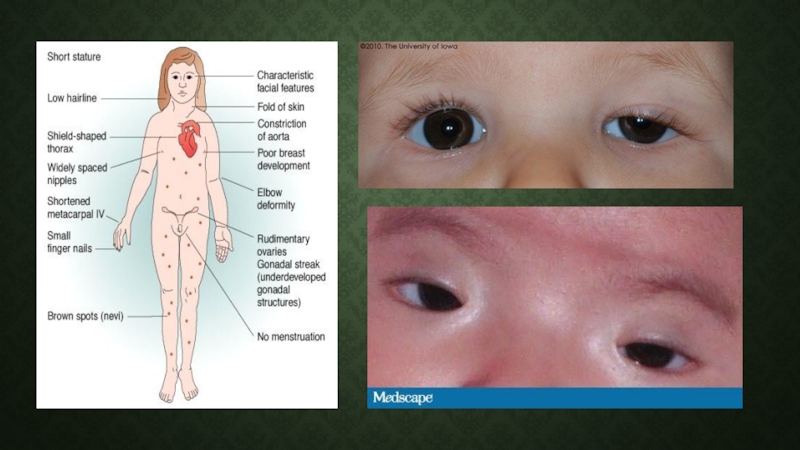
- 55. Gonadal Disorders: Turner syndrome: Turner syndrome
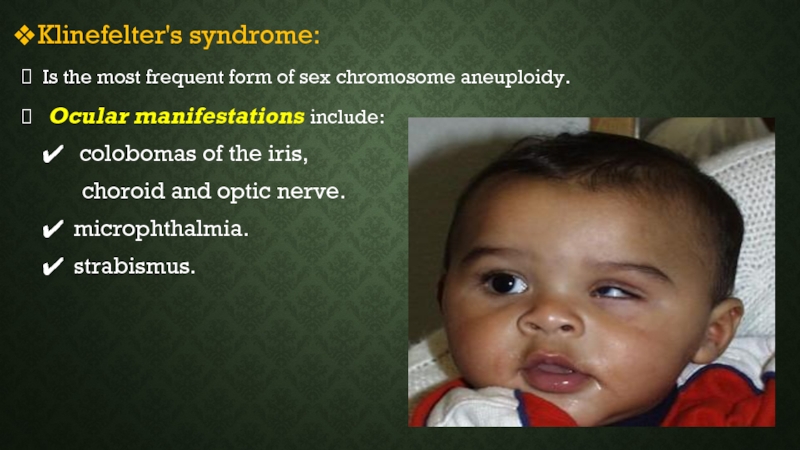
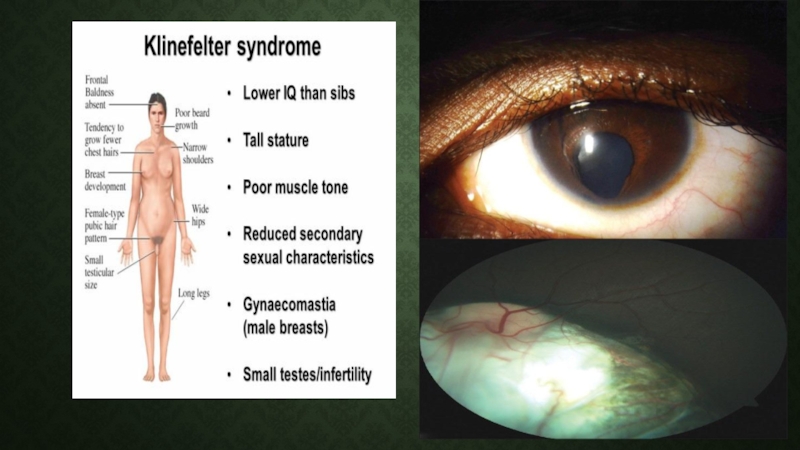
- 57. Klinefelter's syndrome: Is the most frequent
- 59. Thanks
Слайд 3FOREWORD
The eye is a mirror which reflect the health of other
systems in the human body.
The human eye, as an organ, can offer critical clues to the diagnosis of various systemic illnesses.
Ocular changes are common in various endocrine disorders such as diabetes mellitus and Graves’ disease.
Awareness of the associations between the ocular manifestations and endocrine disorders is the first step in the diagnosis and management of these complex patients.
The human eye, as an organ, can offer critical clues to the diagnosis of various systemic illnesses.
Ocular changes are common in various endocrine disorders such as diabetes mellitus and Graves’ disease.
Awareness of the associations between the ocular manifestations and endocrine disorders is the first step in the diagnosis and management of these complex patients.
Слайд 6PITUITARY TUMORS
Foreword:
Pituitary tumors are benign growths of cells in the
pituitary gland .
Small tumors of the pituitary are very common and usually without symptoms, unless the tumor produces a hormone.
However if the tumor enlarges,:
it can cause hormonal deficiencies by pressing on the normal pituitary cells.
If it grows even larger (> 1 cm), it can cause visual symptoms.
Small tumors of the pituitary are very common and usually without symptoms, unless the tumor produces a hormone.
However if the tumor enlarges,:
it can cause hormonal deficiencies by pressing on the normal pituitary cells.
If it grows even larger (> 1 cm), it can cause visual symptoms.
Слайд 7
Ocular symptoms:
Depending on the size
of a pituitary tumor,
visual symptoms may
include:
• Blurred
vision (in one or both
eyes)
• Loss of peripheral vision
• Double vision
eyes)
• Loss of peripheral vision
• Double vision
Слайд 8A pituitary tumor can cause visual
symptoms arising from :
Pressure effects
exerted on the optic
nerves, chiasma, or tracts.
Extension of the tumor into the
cavernous sinus can lead to paresis
of the third, fourth, or sixth nerves,
causing disorders of extraocular
movement.
nerves, chiasma, or tracts.
Extension of the tumor into the
cavernous sinus can lead to paresis
of the third, fourth, or sixth nerves,
causing disorders of extraocular
movement.
Слайд 10Visual field defect in pituitary
tumor:
are caused by tumor
compression
on the optic nerve or chiasm.
Depending on the size and
location of the tumor.
The severity and symmetry of the
visual field defect may vary as well
as the anatomical relationship of the
chiasm to the pituitary stalk.
on the optic nerve or chiasm.
Depending on the size and
location of the tumor.
The severity and symmetry of the
visual field defect may vary as well
as the anatomical relationship of the
chiasm to the pituitary stalk.
Слайд 12TYPES OF VISUAL FIELD DEFECT
Monocular Visual Field Deficit.
Chiasmal Field
Deficit.
Junctional Field Deficits.
Junctional Field Deficits.
Слайд 13 Monocular Visual Field Deficit:
Asymmetric tumors may involve
one side of
the chiasm or an optic
nerve, and most commonly presents
as a supertemporal quadrantanopsia.
nerve, and most commonly presents
as a supertemporal quadrantanopsia.
Слайд 14Chiasmal Field Deficit:
lesions at the level of the optic
chiasm produce a bitemporal hemianopia.
Pituitary adenomas, which grow
upward from the pituitary stalk,
compress the chiasm from below, which
preferentially involves the inferior, nasal,
and macular nerve fibers. This corresponds
to superior, bitemporal, and central vision loss.
Pituitary adenomas, which grow
upward from the pituitary stalk,
compress the chiasm from below, which
preferentially involves the inferior, nasal,
and macular nerve fibers. This corresponds
to superior, bitemporal, and central vision loss.
Слайд 15
Junctional Field Deficits:
central scotoma in one eye with
temporal visual
field loss in the other eye .
It caused by compression to an anterior
loop to the decussating nasal fibers
within the posterior optic nerve
"Wilbrand's knee,"
It caused by compression to an anterior
loop to the decussating nasal fibers
within the posterior optic nerve
"Wilbrand's knee,"
Слайд 16Diagnosis:
The doctor will examine:
• Visual acuity
• Color vision
• Peripheral vision
.
• Eye movements
• The appearance of the
retina and optic nerve .
• Eye movements
• The appearance of the
retina and optic nerve .
Слайд 17 Papilledema is a rare finding in pituitary tumors.
because of
the slow –growing nature of these tumors which cause secondary optic atrophy before the tumor enlarges sufficiently to increase ICP.
Слайд 19Treatment:
may include:
Surgery.
Medications to shrink the
tumor (depending
on the type
of tumor cells).
Radiation treatment
of tumor cells).
Radiation treatment
Слайд 20Treatments for double vision
include:
• Blocking the vision from one
eye.
• Prisms in eyeglasses.
• Surgery on eye muscles to correct
the alignment of the eyes.
• Prisms in eyeglasses.
• Surgery on eye muscles to correct
the alignment of the eyes.
Слайд 21Prognosis:
Visual loss :
often improve after a pituitary tumor is treated.
Or may
be permanent if it has been present for a long time or is severe.
Visual field:
The pattern of recovery after decompression suggests at least three phases of improvement.
Visual field:
The pattern of recovery after decompression suggests at least three phases of improvement.
Слайд 22
The three phases of improvement :
The early fast phase
(surgery to 1 week) may lead to normalization in some individuals.
The early slow phase (1-4 months) is the period of most notable improvement .
A late phase (6 months to 3 years) of mild improvement doesn't appear significant over all but maybe marked in some individuals.
The early slow phase (1-4 months) is the period of most notable improvement .
A late phase (6 months to 3 years) of mild improvement doesn't appear significant over all but maybe marked in some individuals.
Слайд 23 the most common Hypothalmic –pituitary syndromes
Septo-optic dysplasia (SOD).
Kallman's
syndrome.
Empty sella syndrome.
Oliver Mcfarlane syndrome.
Empty sella syndrome.
Oliver Mcfarlane syndrome.
Слайд 24Septo-optic dysplasia (SOD):
It is a rare congenital anomaly
The classical
triad of SOD includes:
(i) optic nerve hypoplasia .
(ii) pituitary hormone abnormalities.
(iii) midline brain defects.
Diagnosis of SOD can be made clinically
when two or more features of the triad are present.
(i) optic nerve hypoplasia .
(ii) pituitary hormone abnormalities.
(iii) midline brain defects.
Diagnosis of SOD can be made clinically
when two or more features of the triad are present.
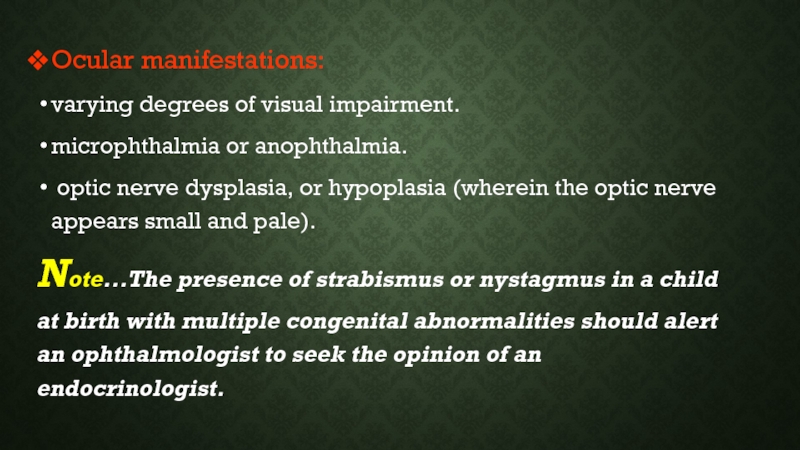
Слайд 25Ocular manifestations:
varying degrees of visual impairment.
microphthalmia or anophthalmia.
optic nerve
dysplasia, or hypoplasia (wherein the optic nerve appears small and pale).
Note...The presence of strabismus or nystagmus in a child at birth with multiple congenital abnormalities should alert an ophthalmologist to seek the opinion of an endocrinologist.
Note...The presence of strabismus or nystagmus in a child at birth with multiple congenital abnormalities should alert an ophthalmologist to seek the opinion of an endocrinologist.
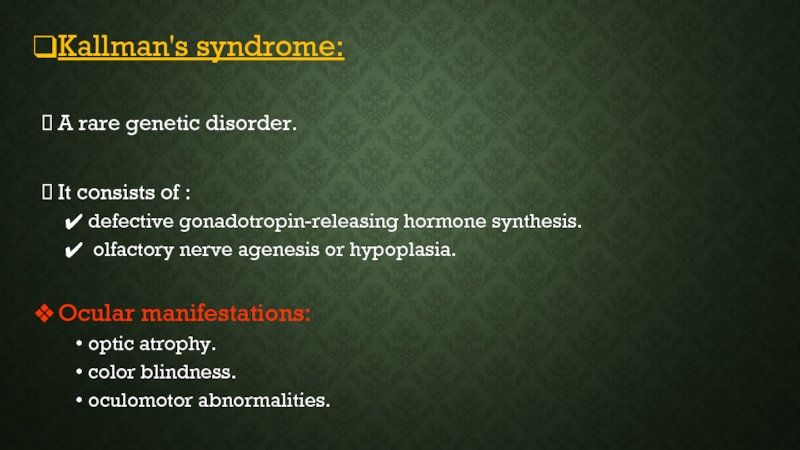
Слайд 26Kallman's syndrome:
A rare genetic disorder.
It consists of :
defective gonadotropin-releasing hormone
synthesis.
olfactory nerve agenesis or hypoplasia.
Ocular manifestations:
optic atrophy.
color blindness.
oculomotor abnormalities.
olfactory nerve agenesis or hypoplasia.
Ocular manifestations:
optic atrophy.
color blindness.
oculomotor abnormalities.
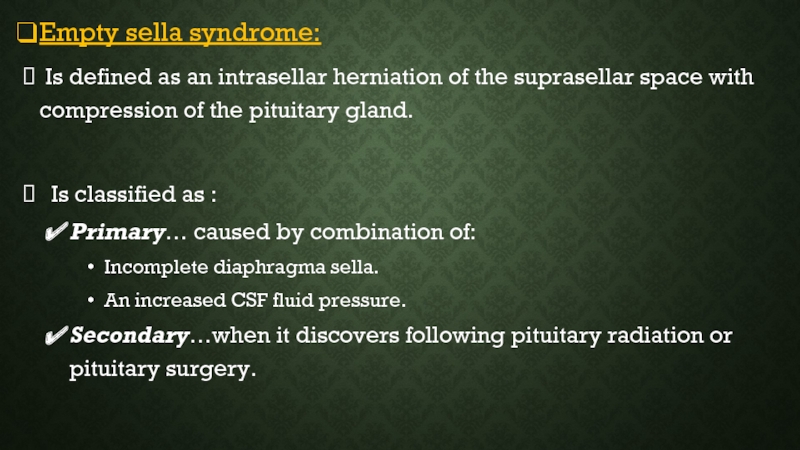
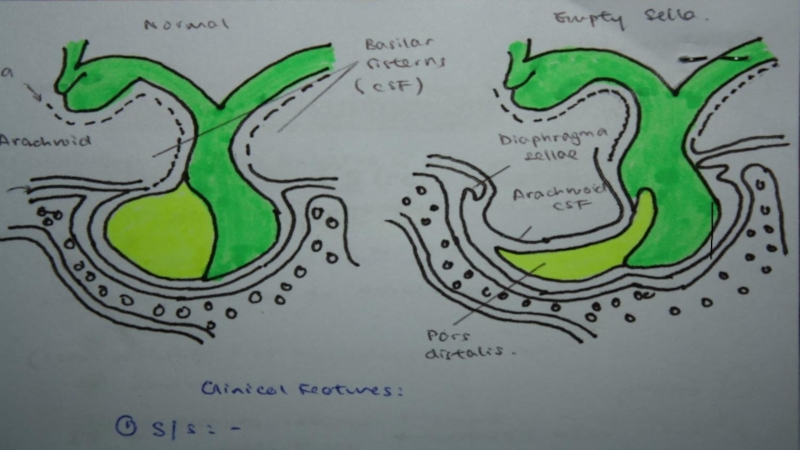
Слайд 27Empty sella syndrome:
Is defined as an intrasellar herniation of
the suprasellar space with compression of the pituitary gland.
Is classified as :
Primary… caused by combination of:
Incomplete diaphragma sella.
An increased CSF fluid pressure.
Secondary…when it discovers following pituitary radiation or pituitary surgery.
Is classified as :
Primary… caused by combination of:
Incomplete diaphragma sella.
An increased CSF fluid pressure.
Secondary…when it discovers following pituitary radiation or pituitary surgery.
Слайд 29Ocular manifestations:
Diminished visual acuity .
Visual field defects such as
peripheral field constriction, bitemporal hemianopia, or quadrantanopia.
Note…... Patients with secondary empty sella predominantly present with visual abnormality occurring due to arachnoidal adhesions and traction on the optic chiasma.
Note…... Patients with secondary empty sella predominantly present with visual abnormality occurring due to arachnoidal adhesions and traction on the optic chiasma.
Слайд 30 Oliver Mcfarlane syndrome:
It is an extremely rare condition
associated with :
chorioretinal degeneration, patients usually present with marked decrease in vision.
Dwarfism with growth hormone deficiency.
Hair abnormalities.
Cerebellar dysfunction.
chorioretinal degeneration, patients usually present with marked decrease in vision.
Dwarfism with growth hormone deficiency.
Hair abnormalities.
Cerebellar dysfunction.
Слайд 31THYROID EYE DISEASES
Foreword:
An autoimmune condition, which means that the
body’s immune system mistakenly targets its own tissues.
It occurs with :
an overactive thyroid in :
Grave’s disease.
Toxic nodular goitre.
Hypothyroidism, for example
with Hashimoto’s disease.
It occurs with :
an overactive thyroid in :
Grave’s disease.
Toxic nodular goitre.
Hypothyroidism, for example
with Hashimoto’s disease.
Слайд 32GRAVES’ DISEASE
Foreword:
Autoimmune disease, in which immunoglobulins are
directed against the TSH receptors on the thyroid cellular membrane.
Most common form of thyrotoxicosis.
May occur at any age but mostly from 20-40.
Is a condition that predominantly affects females.
Most common form of thyrotoxicosis.
May occur at any age but mostly from 20-40.
Is a condition that predominantly affects females.
Слайд 33 Clinical features:
I. Eye features.
II. Goitre.
III. Thyroid dermopathy
(pretibial myxedema).
IV. Heat intolerance.
V. Cardiovascular.
VI. Gastrointestinal.
VII. Reproductive.
VIII. Bone.
IX. Neuromuscular.
X. Skin.
IV. Heat intolerance.
V. Cardiovascular.
VI. Gastrointestinal.
VII. Reproductive.
VIII. Bone.
IX. Neuromuscular.
X. Skin.
Слайд 34 Eye features:
Classes 0-6, mnemonic “NO SPECS”
Class 0: No signs or
symptoms.
Class 1: Only signs (lid retraction, stare, lid lag), no symptoms.
Class 2: Soft tissue involvement (periorbital edema, congestion
or redness of the conjunctiva, and chemosis).
Class 3: Proptosis .
Class 4: Extraocular muscle involvement.
Class 5: Corneal involvement.
Class 6: Sight loss (optic nerve involvement).
Class 1: Only signs (lid retraction, stare, lid lag), no symptoms.
Class 2: Soft tissue involvement (periorbital edema, congestion
or redness of the conjunctiva, and chemosis).
Class 3: Proptosis .
Class 4: Extraocular muscle involvement.
Class 5: Corneal involvement.
Class 6: Sight loss (optic nerve involvement).
Слайд 37 Diagnosis:
Low TSH, High FT4 and/or FT3.
If eye signs are present,
the diagnosis of Graves’ disease can be made without further tests.
If eye signs are absent and the patient is hyperthyroid with or without a goitre, we need other tests for diagnosis (radioiodine, ………).
If eye signs are absent and the patient is hyperthyroid with or without a goitre, we need other tests for diagnosis (radioiodine, ………).
Слайд 38Symptoms and signs influence the management
strategy so
we should assesse:
The degree of exophthalmos (exophthalmometer).
the intraocular pressure.
Extraocular muscle thickness
(CT, ultrasonography).
The degree of optic nerve compression
(electroretinogram, cortical visual evoked
potentials, and color contrast sensitivity ).
The degree of exophthalmos (exophthalmometer).
the intraocular pressure.
Extraocular muscle thickness
(CT, ultrasonography).
The degree of optic nerve compression
(electroretinogram, cortical visual evoked
potentials, and color contrast sensitivity ).
Слайд 40 Management of opthalmopathy:
Management involves cooperation between the endocrinologist and
the opthalmologist.
Keep head elevated at night to diminish periorbital edema.
If the cornea is exposed, it is important to prescribe artificial tears as a means of corneal lubrication.
Keep head elevated at night to diminish periorbital edema.
If the cornea is exposed, it is important to prescribe artificial tears as a means of corneal lubrication.
Слайд 41 For more severely affected eyes, immunosuppressive therapy with glucocorticoids benefit
approximately 60% of patients with thyroid-associated opthalmopathy.
If steroid therapy is not effective external x-ray therapy to the retrobulbar area may be helpful.
If vision is threatened orbital decompression ( surgical) can be used.
If steroid therapy is not effective external x-ray therapy to the retrobulbar area may be helpful.
If vision is threatened orbital decompression ( surgical) can be used.
Слайд 42
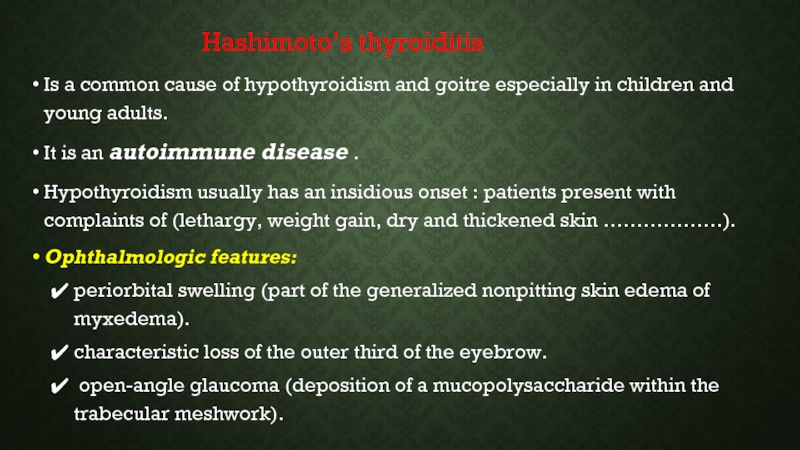
Hashimoto’s thyroiditis
Is a common cause of hypothyroidism and goitre especially in children and young adults.
It is an autoimmune disease .
Hypothyroidism usually has an insidious onset : patients present with complaints of (lethargy, weight gain, dry and thickened skin ………………).
Ophthalmologic features:
periorbital swelling (part of the generalized nonpitting skin edema of myxedema).
characteristic loss of the outer third of the eyebrow.
open-angle glaucoma (deposition of a mucopolysaccharide within the trabecular meshwork).
Is a common cause of hypothyroidism and goitre especially in children and young adults.
It is an autoimmune disease .
Hypothyroidism usually has an insidious onset : patients present with complaints of (lethargy, weight gain, dry and thickened skin ………………).
Ophthalmologic features:
periorbital swelling (part of the generalized nonpitting skin edema of myxedema).
characteristic loss of the outer third of the eyebrow.
open-angle glaucoma (deposition of a mucopolysaccharide within the trabecular meshwork).
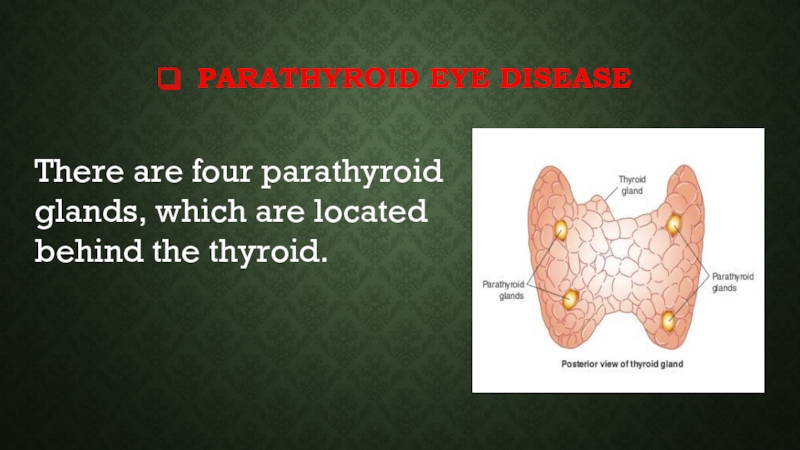
Слайд 44PARATHYROID EYE DISEASE
There are four parathyroid glands, which are located
behind the thyroid.
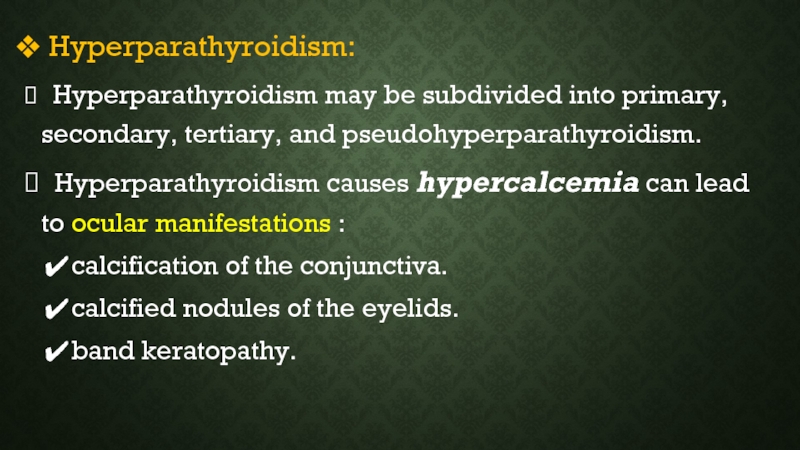
Слайд 45 Hyperparathyroidism:
Hyperparathyroidism may be subdivided into primary, secondary, tertiary, and
pseudohyperparathyroidism.
Hyperparathyroidism causes hypercalcemia can lead to ocular manifestations :
calcification of the conjunctiva.
calcified nodules of the eyelids.
band keratopathy.
Hyperparathyroidism causes hypercalcemia can lead to ocular manifestations :
calcification of the conjunctiva.
calcified nodules of the eyelids.
band keratopathy.
Слайд 48 Hypoparathyroidism:
Is usually the result of the accidental removal of
the parathyroid glands during thyroidectomy, although it may be idiopathic in origin.
The lack of parathyroid hormone produces a clinical state of hypocalcemia and hyperphosphatemia.
The ocular response to hypocalcemia is:
cataractogenesis:
At presentation the lens develops subcapsular cataract.
Which with progression, involves the lenticular cortex.
chronic keratoconjunctivitis (especially in children with idiopathic Hypoparathyroidism ).
The lack of parathyroid hormone produces a clinical state of hypocalcemia and hyperphosphatemia.
The ocular response to hypocalcemia is:
cataractogenesis:
At presentation the lens develops subcapsular cataract.
Which with progression, involves the lenticular cortex.
chronic keratoconjunctivitis (especially in children with idiopathic Hypoparathyroidism ).
Слайд 50Adrenal eye disease
Cushing's Syndrome:
Excessive production of adrenocortical products.
Ocular involvement
is poorly defined and may include :
Cataract (posterior subcapsular type) due to prolonged administration of steroids not a feature of endogenous steroid overproduction.
elevation of intraocular pressure.
hypertensive retinopathy.
proptosis.
Cataract (posterior subcapsular type) due to prolonged administration of steroids not a feature of endogenous steroid overproduction.
elevation of intraocular pressure.
hypertensive retinopathy.
proptosis.
Слайд 51 Addison's Disease:
Caused by insufficiency of the
adrenal cortex.
ocular manifestations:
pigmentation involving the
eyelids and conjunctiva.
Papilledema caused by
increased
intracranial pressure.
pigmentation involving the
eyelids and conjunctiva.
Papilledema caused by
increased
intracranial pressure.
Слайд 52 Neuroblastoma:
Neuroblastomas arise from primitive neuroectodermal elements.
Patients may present
with an abdominal mass and, because most of these tumors secrete catecholamines.
ocular manifestation :
orbital metastatic can present with:
proptosis.
subconjunctival hemorrhage .
ecchymosis of the eyelids.
Horner's syndrome, usually associated with heterochromia iridis (less common ).
ocular manifestation :
orbital metastatic can present with:
proptosis.
subconjunctival hemorrhage .
ecchymosis of the eyelids.
Horner's syndrome, usually associated with heterochromia iridis (less common ).
Слайд 54 Pheochromocytoma:
This rare catecholamine-secreting
tumor originates in chromaffin cells.
The
major ophthalmic feature
of the condition is hypertensive
retinopathy with:
flame-shaped hemorrhages.
cotton-wool spots.
narrowed arteries.
swollen optic discs.
of the condition is hypertensive
retinopathy with:
flame-shaped hemorrhages.
cotton-wool spots.
narrowed arteries.
swollen optic discs.
Слайд 55Gonadal Disorders:
Turner syndrome:
Turner syndrome is a condition in which there
is an absence or structural abnormality of one X chromosome in phenotypic females.
Ocular manifestations:
strabismus
ptosis
hypertelorism.
epicanthus.
red–green color deficiency.
Ocular hypertension and glaucoma.
Ocular manifestations:
strabismus
ptosis
hypertelorism.
epicanthus.
red–green color deficiency.
Ocular hypertension and glaucoma.
Слайд 57Klinefelter's syndrome:
Is the most frequent form of sex chromosome aneuploidy.
Ocular manifestations include:
colobomas of the iris,
choroid and optic nerve.
microphthalmia.
strabismus.
colobomas of the iris,
choroid and optic nerve.
microphthalmia.
strabismus.