- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Population Health Management:Your Current State of Health Analysis презентация
Содержание
- 1. Population Health Management:Your Current State of Health Analysis
- 2. YESTERDAY: CLAIMS-BASED PREDICTIVE MODELS For years, healthcare
- 3. Most physicians are highly skeptical of
- 4. These models lack a correlation to
- 5. FURTHER CONSIDERATIONS Current thinking and efforts create
- 6. VITAL PROGRESS Today, most large physician groups
- 7. CLOSED-LOOP CMP Using real-time clinical data from
- 8. Population SOH Stratification State of health stratification
- 9. Origins of SOH Models Nationally accepted clinical
- 10. Figure 2 Population SOH (Risk) Stratification by Physician
- 11. Chronic Disease Management Patients who comply with
- 12. Care Coordination Physicians who improved the state
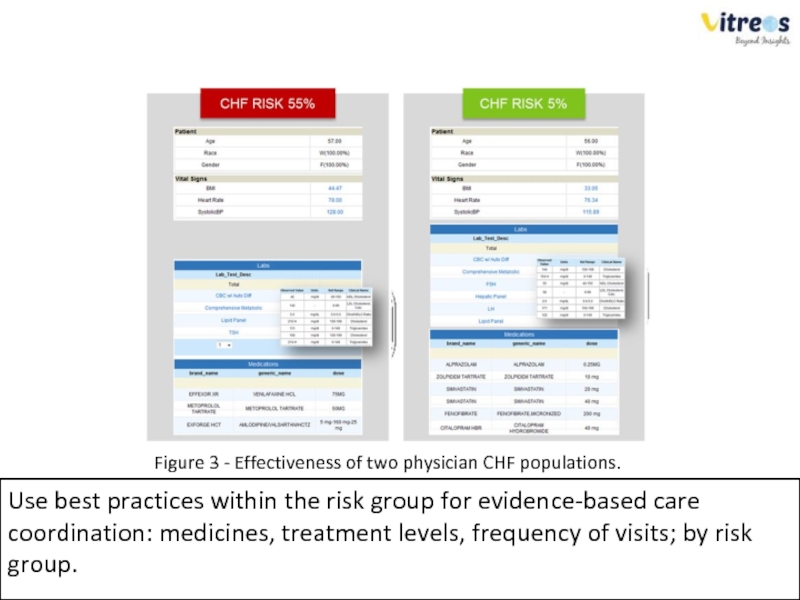
- 13. Figure 3 - Effectiveness of two physician
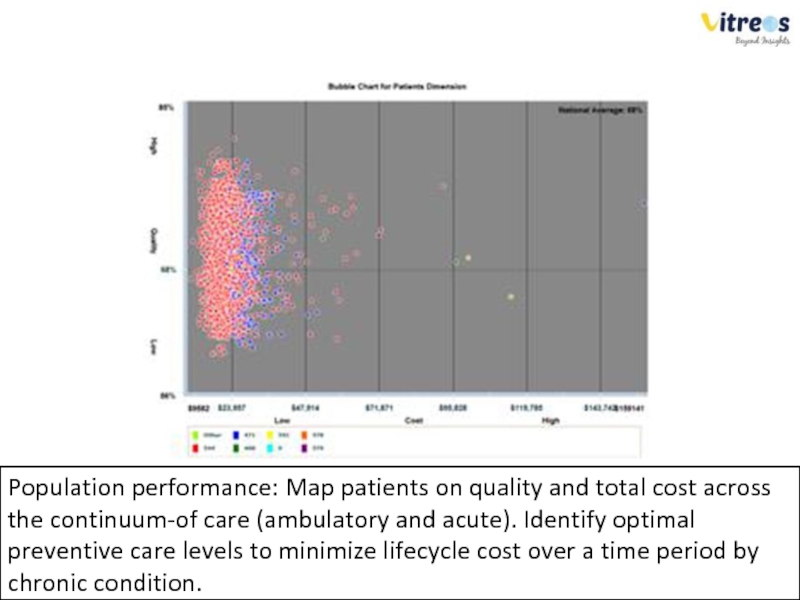
- 14. Population performance: Map patients on quality and
- 15. Incentive management If financial incentives for health
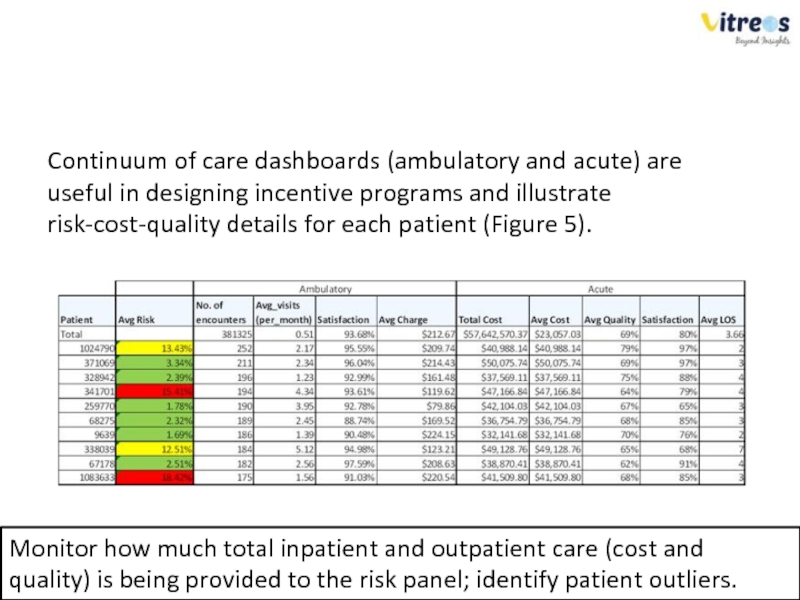
- 16. Continuum of care dashboards (ambulatory and
- 17. Patient SOH scores can be rolled
- 19. Validating the SOH Model APPROACH To validate
- 20. Inpatient Admissions Figure 7 shows total hospitalized
- 21. Creating a SOH Composite Figure 8 shows
- 22. WORK SMARTER USING SOH MODELS State of
- 23. Healthcare providers can enable continuous improvement
- 24. MCNT has pioneered the SOH-based population
- 25. SUMMARY To lower health costs, physician networks
Слайд 2YESTERDAY: CLAIMS-BASED PREDICTIVE MODELS
For years, healthcare insurance companies (payers) have mined
While this approach has seen some success, limitations far outweigh merits.
Data used by payers to flag high risk patients is historical claims data — primarily costs, admissions, and diagnoses. Furthermore, regression and time series risk models are typically updated only annually.
Слайд 3
Most physicians are highly skeptical of claims based predictive models because
Moreover, there is a complete lack of causation, "Why is a patient considered high-risk? What are the clinical reasons for the score? How do we lower the patient's risk score? How does the score measure the effectiveness of my care management program?“
http://healthcarecostmonitor.thehastingscenter.org/kimberlyswartz/projected-costs-ofchronic- diseases/
http://www.ahrq.gov/research/ria19/expendria.htm
Слайд 4
These models lack a correlation to clinical information.
Claims-based risk scores
Not only are today’s calculations unsuitable for determining a patient’s true risk, they provide no insight on how an individual’s score improves or deteriorates after each clinical visit.
Слайд 5FURTHER CONSIDERATIONS
Current thinking and efforts create a disproportionate focus on existing
A better approach is to monitor all patients, healthy and chronic, for risk of hospitalizations.
Unfortunately, current claims-based predictive risk models allow no room for this approach.
Слайд 6VITAL PROGRESS
Today, most large physician groups and medical homes already use
CMS predicts that by 2014, more than fifty percent of all eligible medical professionals in the U.S. will use EHR.
This is a transformational shift, because for the first time in history, clinical information is digitally available in real time, with reasonable availability of laboratory results and patient vital data.
Слайд 7CLOSED-LOOP CMP
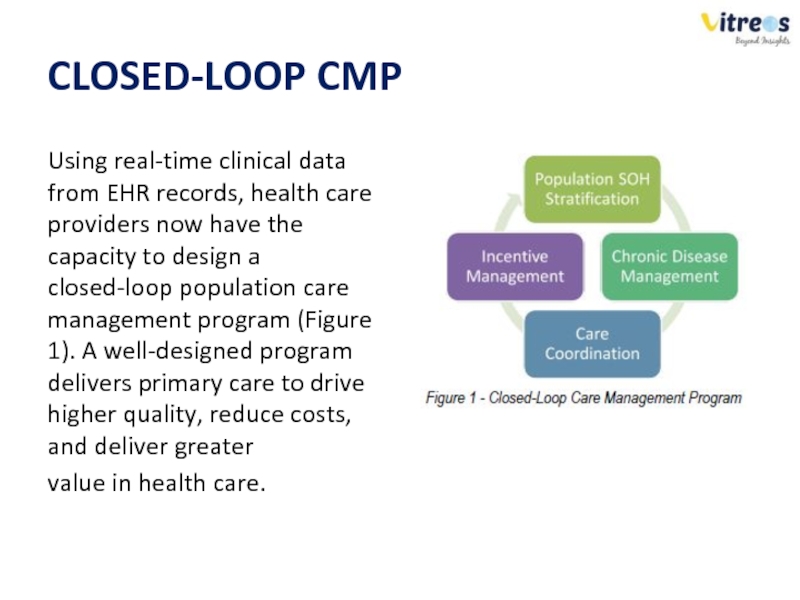
Using real-time clinical data from EHR records, health care providers
value in health care.
Слайд 8Population SOH Stratification
State of health stratification provides actionable and measurable information
SOH is a “risk predictor”. However, it is also an indicator of the quality of care delivered.
If the score trends down, the quality of care is good,
because health is improving.
Слайд 9Origins of SOH Models
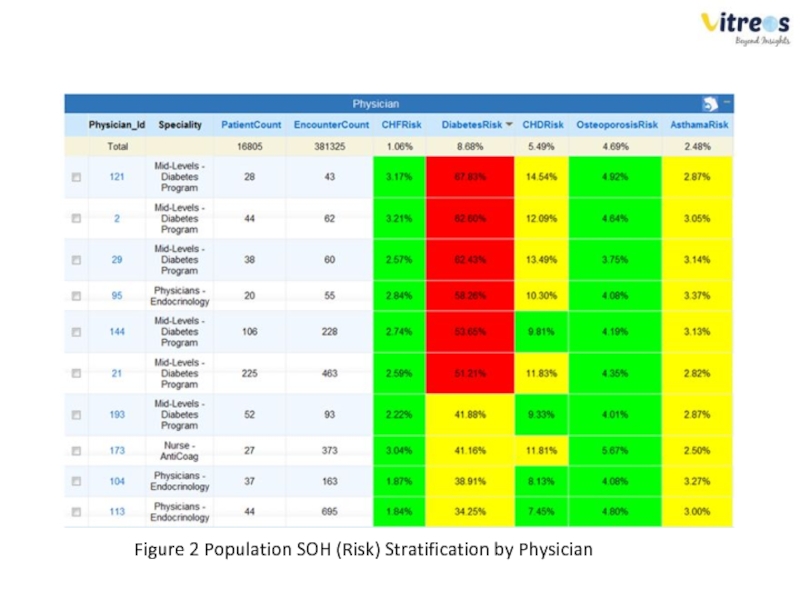
Nationally accepted clinical models are the basis for
SOH scores are calculated at the patient level and rolled up to a population level (Figure 2).
In this example, each row corresponds to a physician's patient population. It shows the patient count, the number of office visits (encounter) and the average population SOH score for each chronic disease.
Слайд 11Chronic Disease Management
Patients who comply with prescribed care programs are typically
This is where care coordinators play an important role.
Monitoring gaps in care established by evidence-based care, patients’ SOH trends, and underlying clinical drivers over time, care coordinators can identify patients that need their attention.
Слайд 12Care Coordination
Physicians who improved the state of health for their population
In one instance, one physician’s CHF population risk increased to 55%, while another’s dropped to 5%.
Слайд 13Figure 3 - Effectiveness of two physician CHF populations.
Use best practices
Слайд 14Population performance: Map patients on quality and total cost across the
Слайд 15Incentive management
If financial incentives for health care professionals are not aligned
Effective incentive programs distinctly drive higher quality and reduce costs for greater value in health care.
Incentive programs reward care teams for reducing population risk scores, improving patient satisfaction scores, and reducing overall patient costs.
Слайд 16
Continuum of care dashboards (ambulatory and acute) are useful in designing
Figure 5 - Continuum of Care Analysis by Patient, Preventive Care Impact on Acute Care Costs
Monitor how much total inpatient and outpatient care (cost and quality) is being provided to the risk panel; identify patient outliers.
Слайд 17
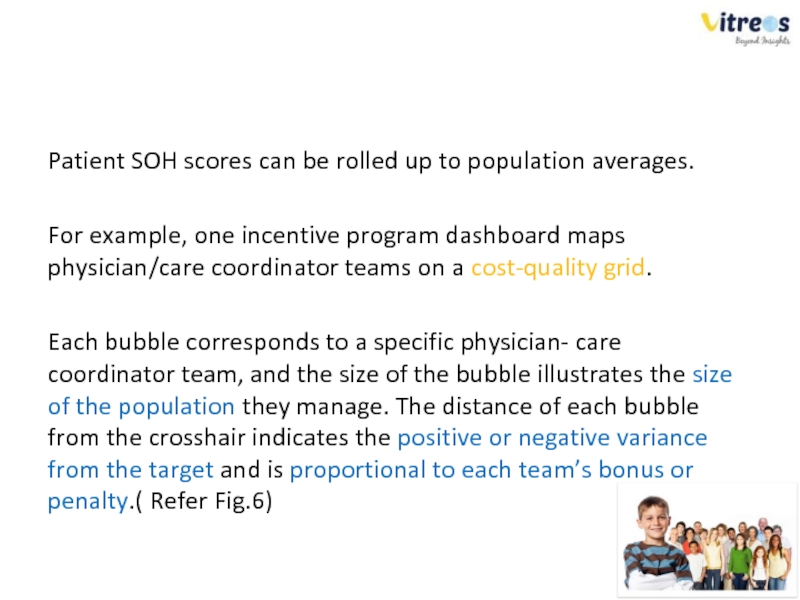
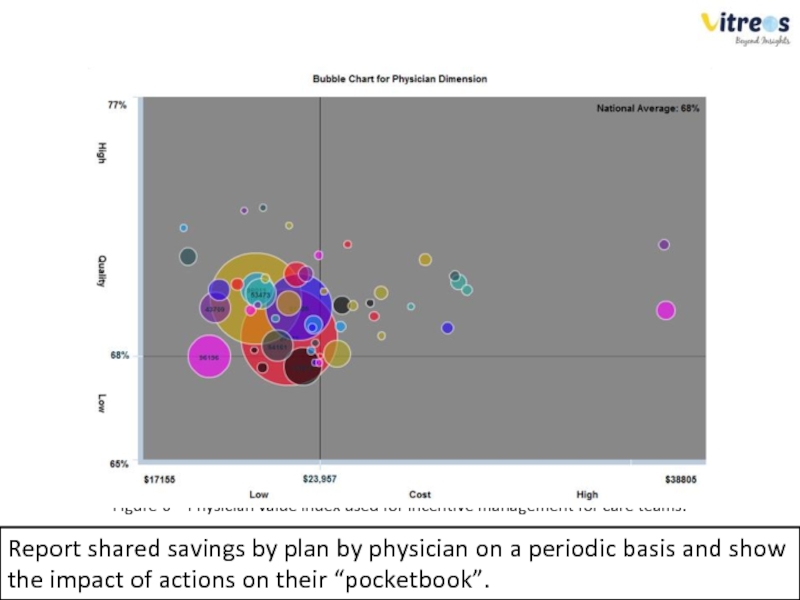
Patient SOH scores can be rolled up to population averages.
For
Each bubble corresponds to a specific physician- care coordinator team, and the size of the bubble illustrates the size of the population they manage. The distance of each bubble from the crosshair indicates the positive or negative variance from the target and is proportional to each team’s bonus or penalty.( Refer Fig.6)
Слайд 18
Figure 6 – Physician value index used for incentive management for
Report shared savings by plan by physician on a periodic basis and show the impact of actions on their “pocketbook”.
Слайд 19Validating the SOH Model APPROACH
To validate the models, researchers compared the
For the SOH model, researchers used real-time clinical data. The SOH model did not include past ER or IP admissions data.
Next, researchers calculated a SOH score for each patient using historical data over two years
Слайд 20Inpatient Admissions
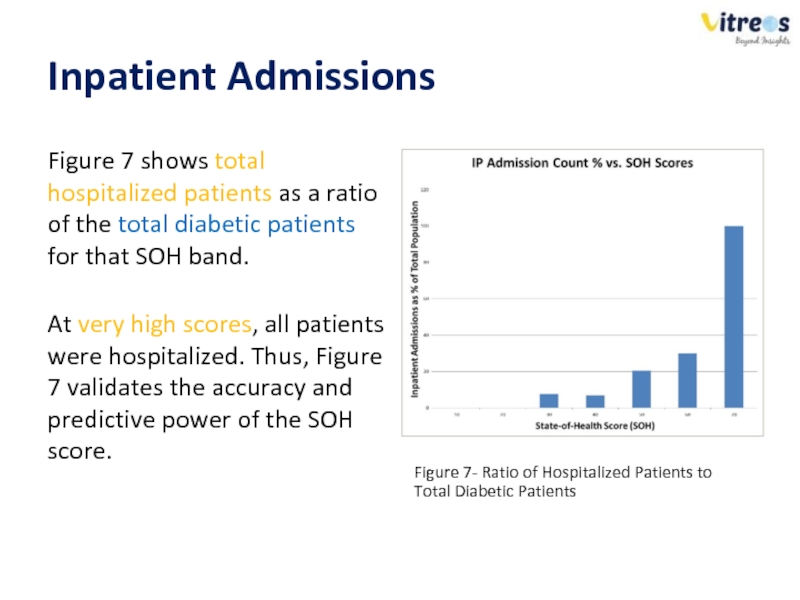
Figure 7 shows total hospitalized patients as a ratio of
At very high scores, all patients were hospitalized. Thus, Figure 7 validates the accuracy and predictive power of the SOH score.
Figure 7- Ratio of Hospitalized Patients to Total Diabetic Patients
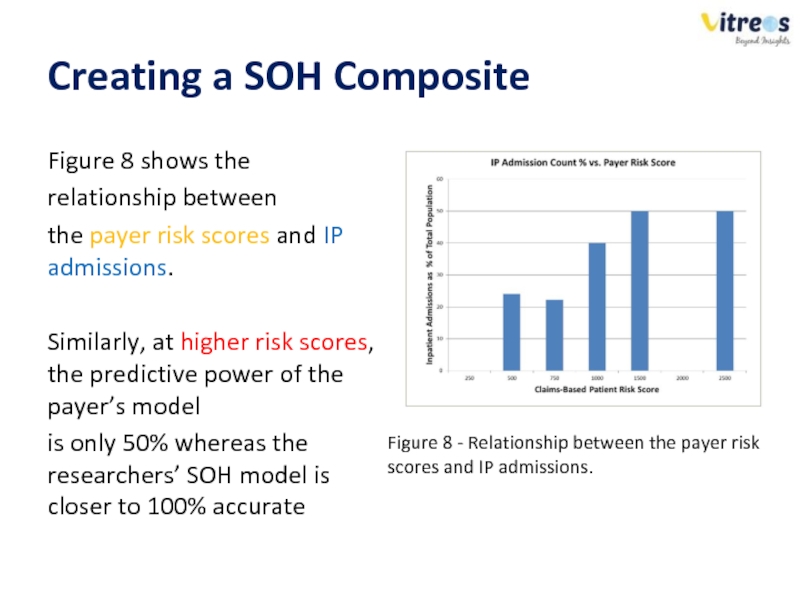
Слайд 21Creating a SOH Composite
Figure 8 shows the
relationship between
the payer
Similarly, at higher risk scores, the predictive power of the payer’s model
is only 50% whereas the researchers’ SOH model is closer to 100% accurate
Figure 8 - Relationship between the payer risk scores and IP admissions.
Слайд 22WORK SMARTER USING SOH MODELS
State of health models are highly accurate
Using SOH scores, care coordinators can correctly identify and focus on high risk patients with a great risk of hospitalization in the short term.
Given the rapid adoption of EHRs among primary care physicians and groups, the data required to build SOH models is readily available now, and will continue to expand over the next two years.
Слайд 23
Healthcare providers can enable continuous improvement using SOH models together with
Слайд 24
MCNT has pioneered the SOH-based population management approach.
MCNT experienced a
Overall performance index improved in Facility Outpatient (-5%), Other Medical Services (-6%), and Professional (-1%) categories, relative to the market. An enviable performance considering the challenges healthcare provider markets are facing with the influx of market changes.
Слайд 25SUMMARY
To lower health costs, physician networks and medical homes must employ
To become masters in their population management programs, they need decision support systems such as population SOH (risk) stratification and predictive models.