- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
DRUG TREATMENT OF PSYCHOSIS презентация
Содержание
- 1. DRUG TREATMENT OF PSYCHOSIS
- 2. Psychiatric Nosology (Classification of disease) Psychosis Cognitive
- 3. Psychosis Psychosis is a thought disorder characterized
- 4. Schizophrenia Pathogenesis is unknown. Onset of schizophrenia
- 5. Schizophrenia It is a thought disorder.
- 6. Schizophrenia Positive Symptoms. Hallucinations, delusions, paranoia,
- 8. Etiology of Schizophrenia Idiopathic Biological Correlates Genetic Factors Neurodevelopmental abnormalities. Environmental stressors.
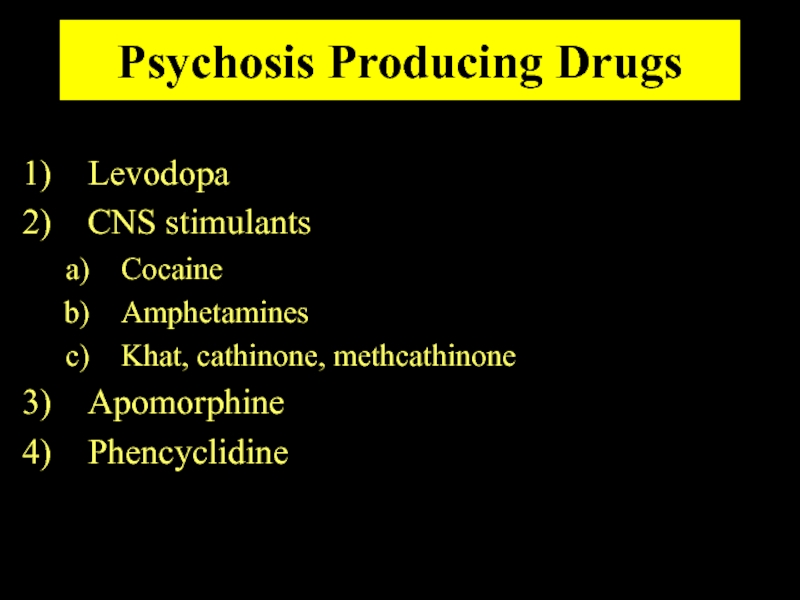
- 9. Psychosis Producing Drugs Levodopa CNS stimulants Cocaine
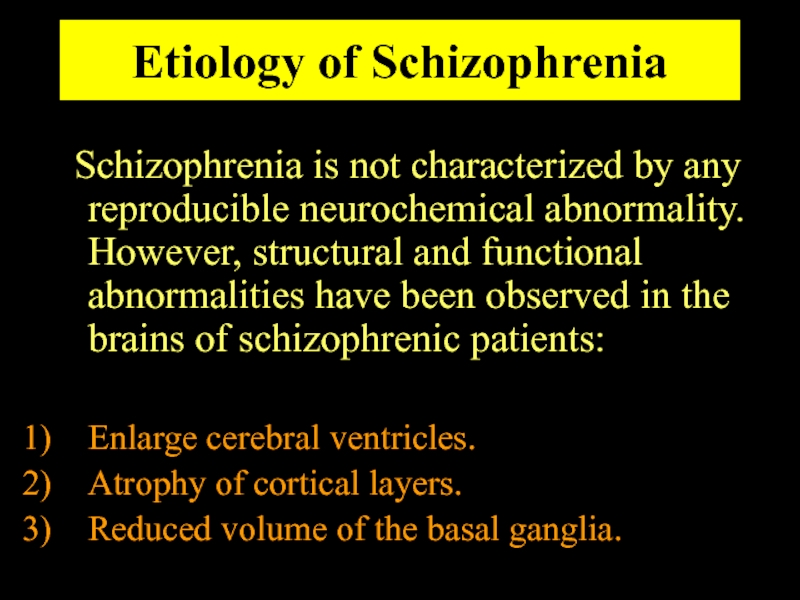
- 10. Etiology of Schizophrenia Schizophrenia is not characterized
- 11. Dopamine Theory of Schizophrenia Many lines
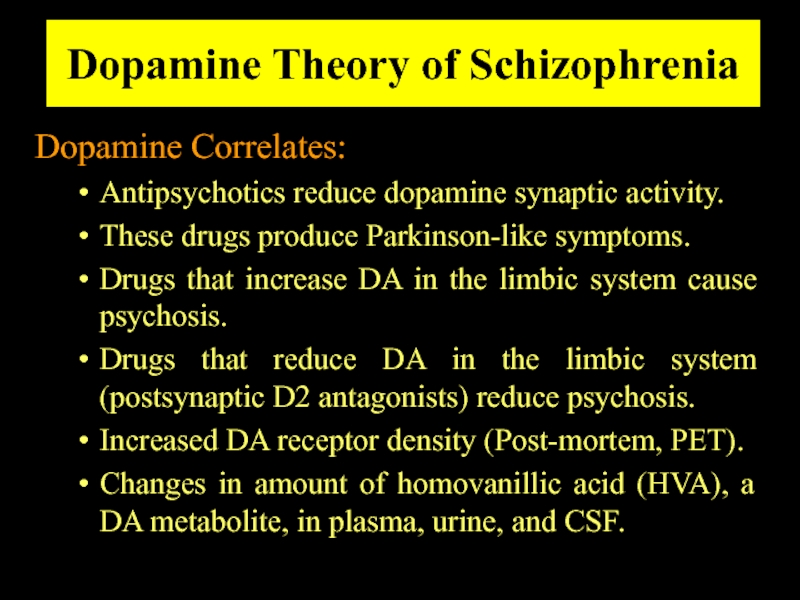
- 12. Dopamine Theory of Schizophrenia Dopamine Correlates: Antipsychotics
- 13. Pharmacodynamics Anatomic Correlates of Schizophrenia... Frontal cortex
- 14. Dopamine Theory of Schizophrenia Evidence against the
- 15. Dopamine System There are four major pathways
- 16. THE DOPAMINERGIC SYSTEM
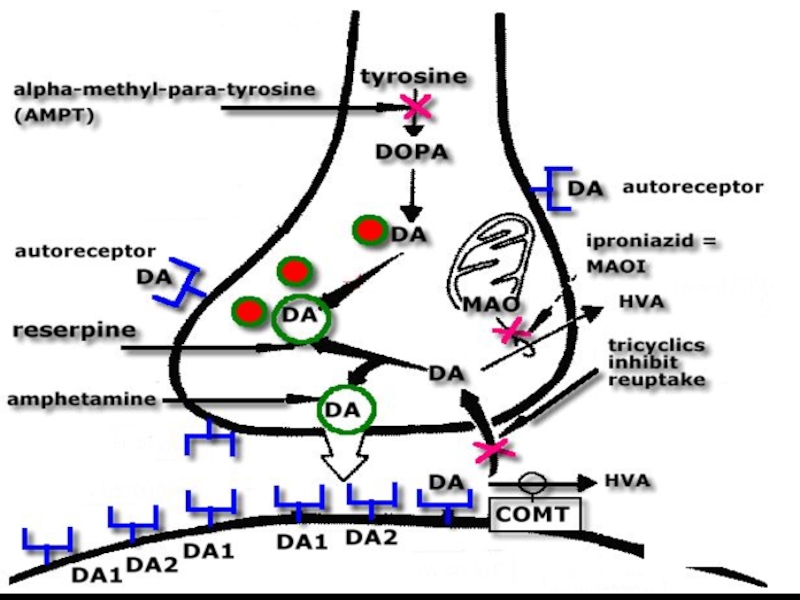
- 17. Catecholamines Tyrosine ⇓ Tyrosine hydroxylase L-Dopa
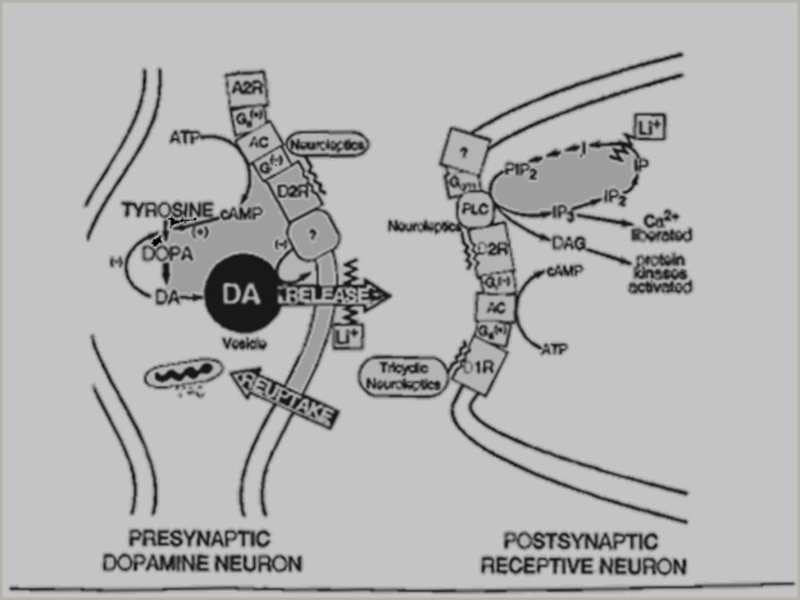
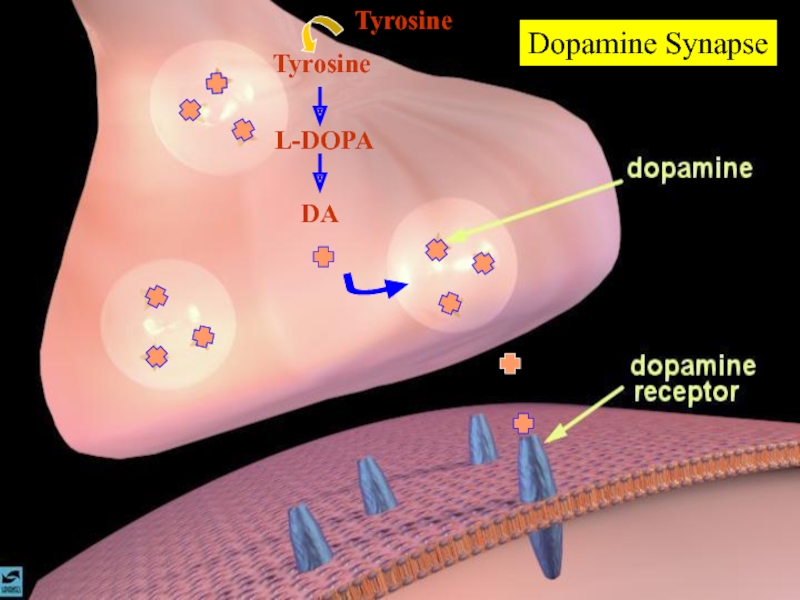
- 18. Dopamine Synapse DA L-DOPA Tyrosine Tyrosine
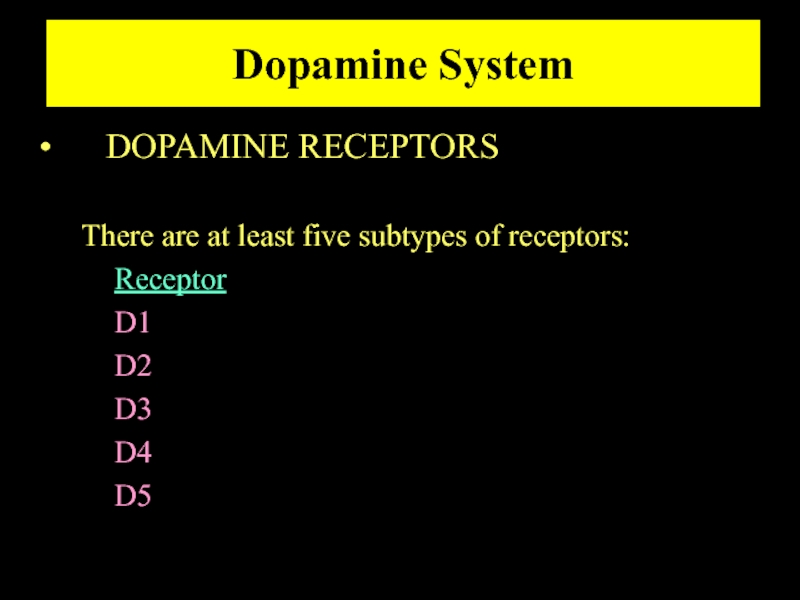
- 19. Dopamine System DOPAMINE RECEPTORS There
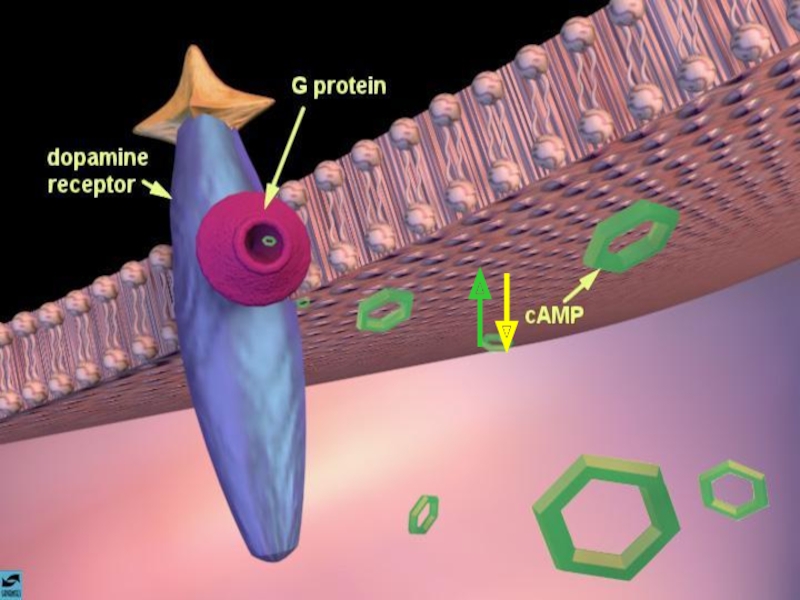
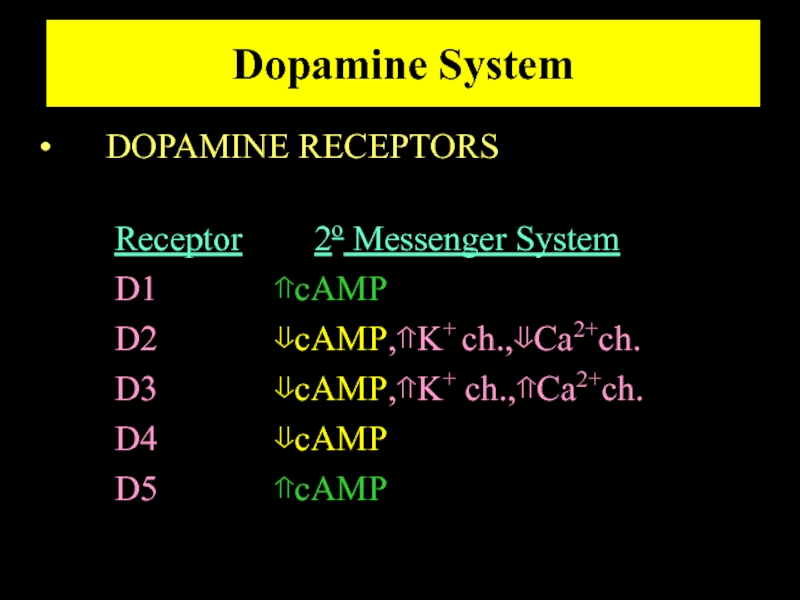
- 21. Dopamine System DOPAMINE RECEPTORS Receptor 2o Messenger
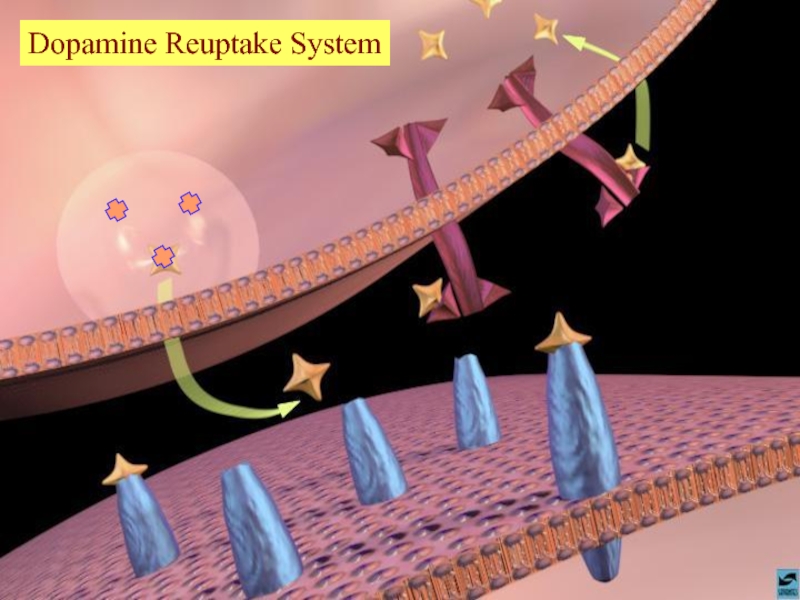
- 22. Dopamine Reuptake System
- 23. Antipsychotic treatments SCHIZOPHRENIA IS FOR LIFE There is no remission
- 24. Antipsychotic treatments Schizophrenia has been around perhaps,
- 25. Antipsychotic treatments In 1940’s Phenothiazenes were isolated
- 26. Antipsychotics treatment Antipsychotics/Neuroleptics Antipsychotics are the
- 27. Antipsychotics/Neuroleptics Although the antipsychotic/neuroleptics are drugs used
- 28. Antipsychotics/Neuroleptics NON-compliance is the major reason for relapse.
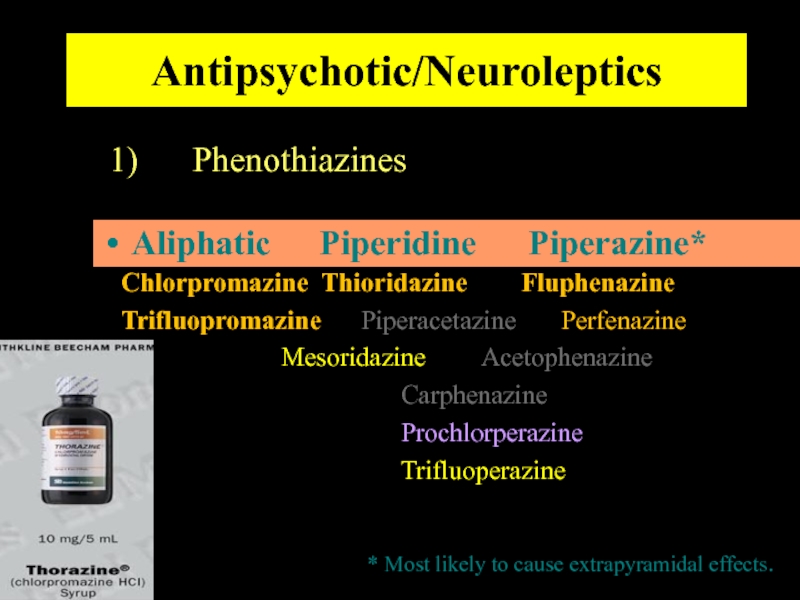
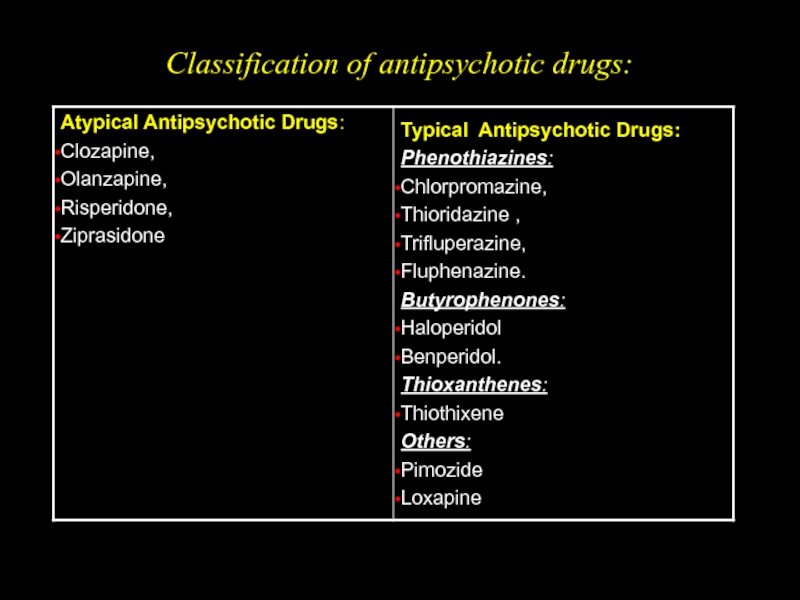
- 29. Antipsychotic/Neuroleptics Three major groups : Phenothiazines Thioxanthine Butyrophenones OLDER DRUGS
- 30. Antipsychotic/Neuroleptics Phenothiazines Chlorpromazine Thioridazine Fluphenazine Trifluopromazine Piperacetazine Perfenazine
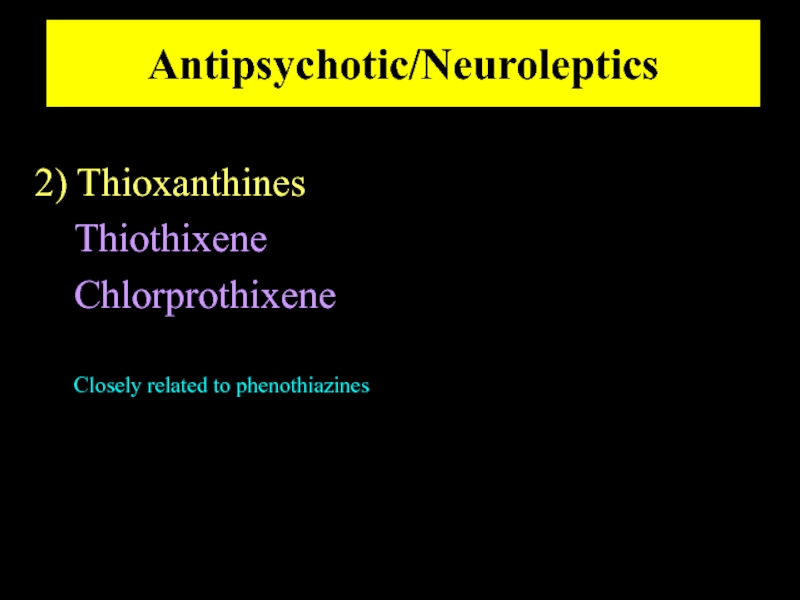
- 31. Antipsychotic/Neuroleptics 2) Thioxanthines Thiothixene Chlorprothixene Closely related to phenothiazines
- 32. Antipsychotic/Neuroleptics 3) Butyrophenones Haloperidol Droperidol* *Not marketed in the USA
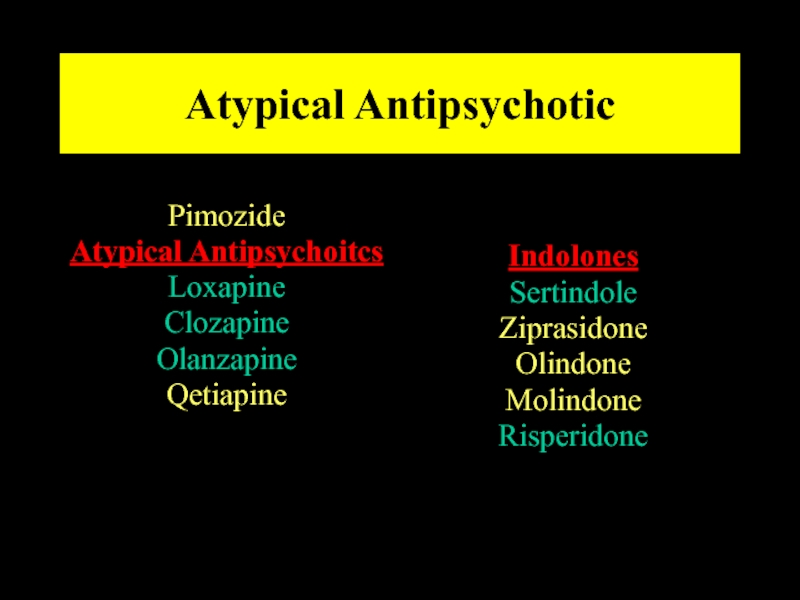
- 34. Atypical Antipsychotic Pimozide Atypical Antipsychoitcs
- 35. Classification of antipsychotic drugs:
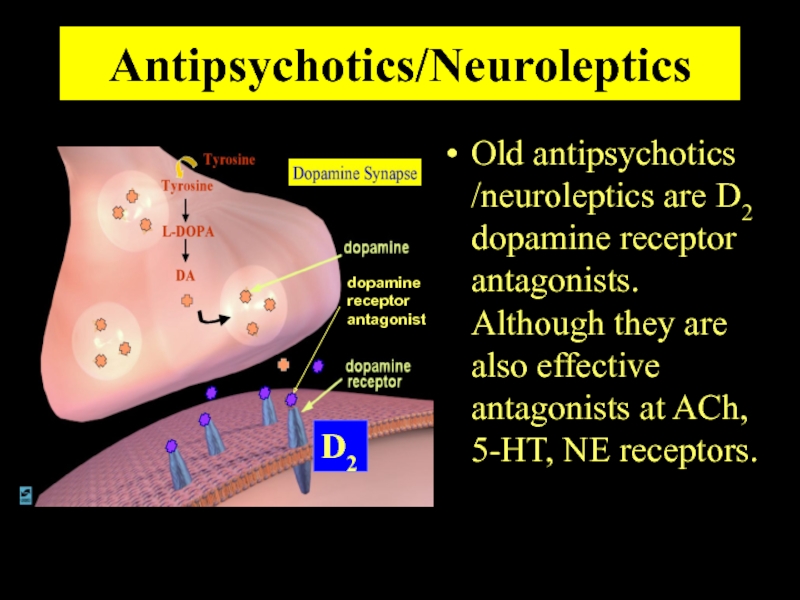
- 36. Antipsychotics/Neuroleptics Old antipsychotics /neuroleptics are D2 dopamine
- 37. Antipsychotics/Neuroleptics It appears that the specific interaction
- 38. Antipsychotics/Neuroleptics Both D1 and D2 receptors are
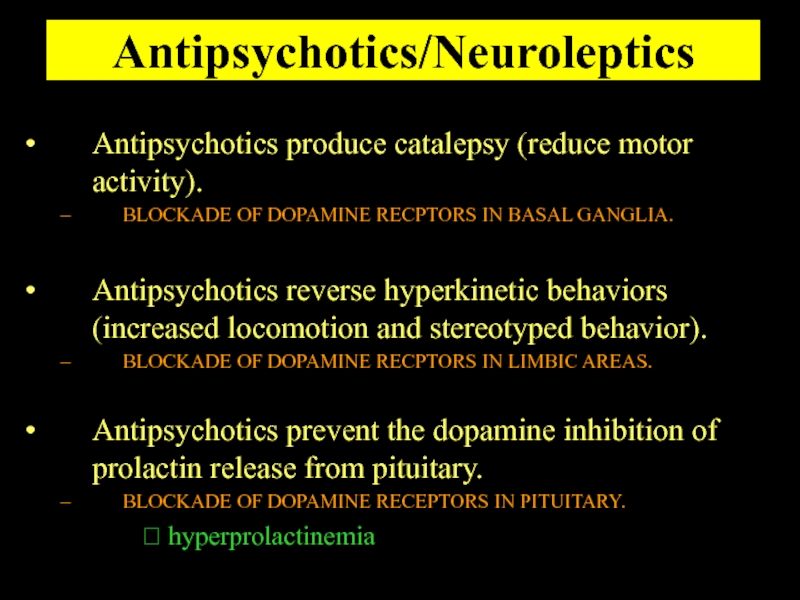
- 39. Antipsychotics/Neuroleptics Antipsychotics produce catalepsy (reduce motor activity).
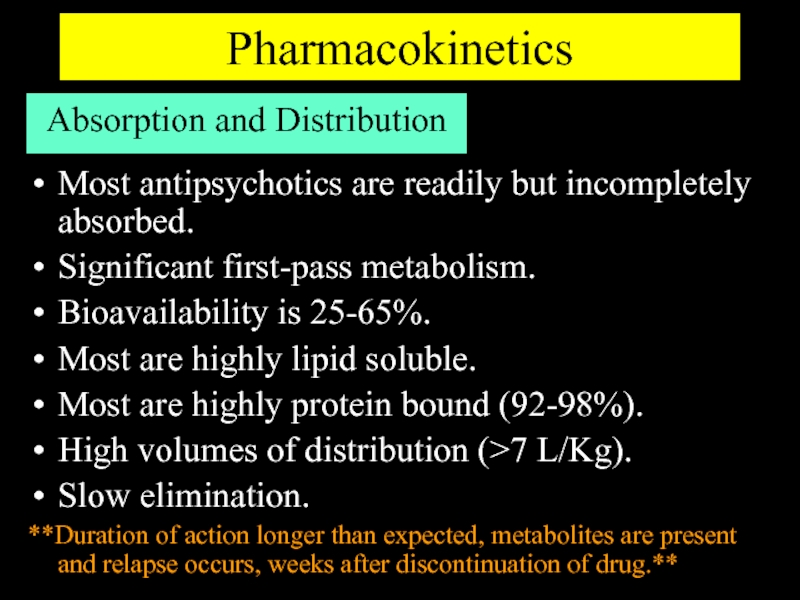
- 40. Pharmacokinetics Absorption and Distribution Most antipsychotics are
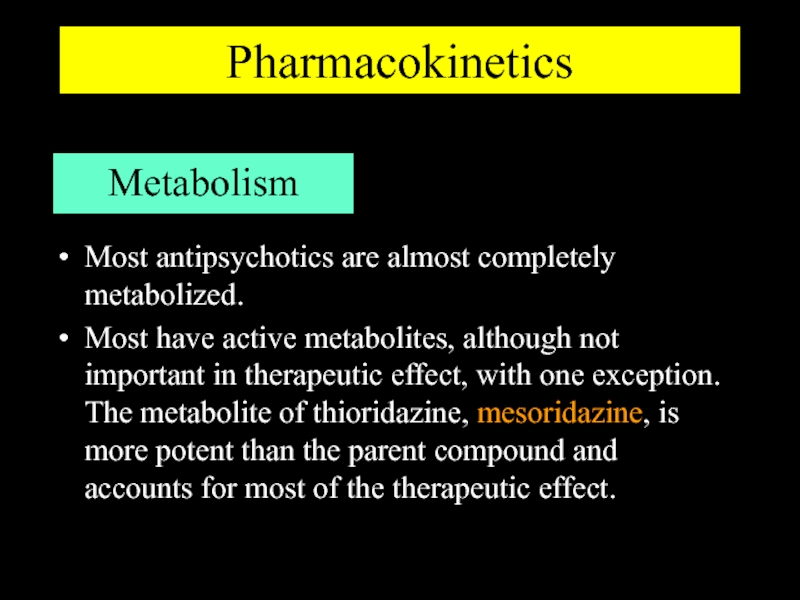
- 41. Pharmacokinetics Metabolism Most antipsychotics are almost completely
- 42. Pharmacokinetics Excretion Antipsychotics are almost completely metabolized
- 43. Antipsychotic/Neuroleptics [Drug dose] Effect
- 44. Antipsychotic/Neuroleptics [Drug dose] Effect
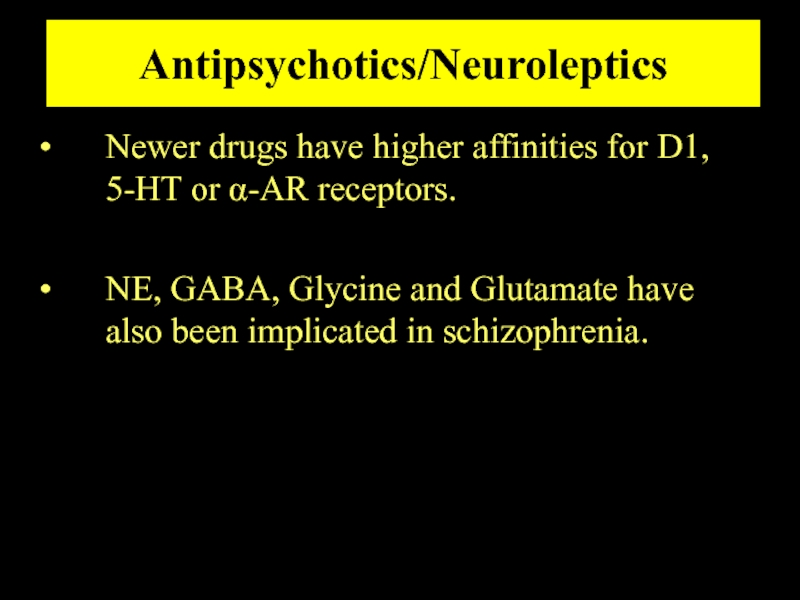
- 45. Antipsychotics/Neuroleptics Newer drugs have higher affinities for
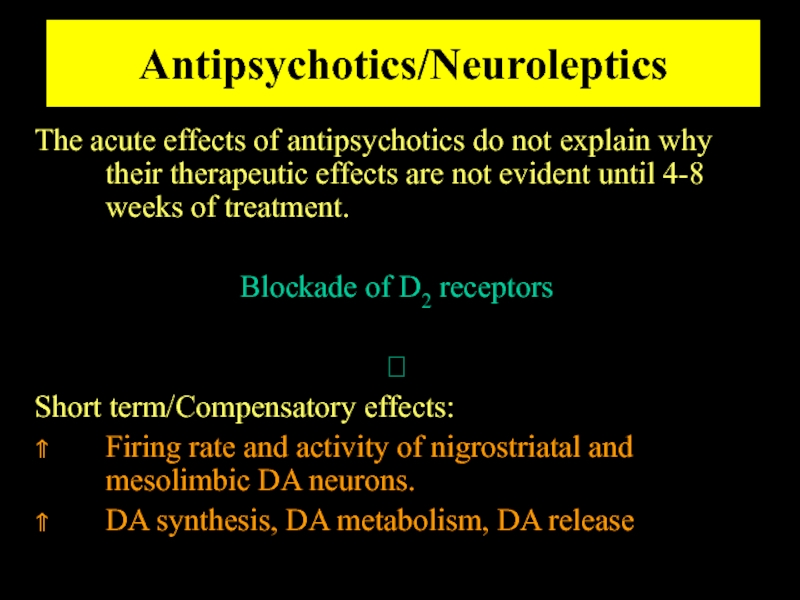
- 46. Antipsychotics/Neuroleptics The acute effects of antipsychotics do
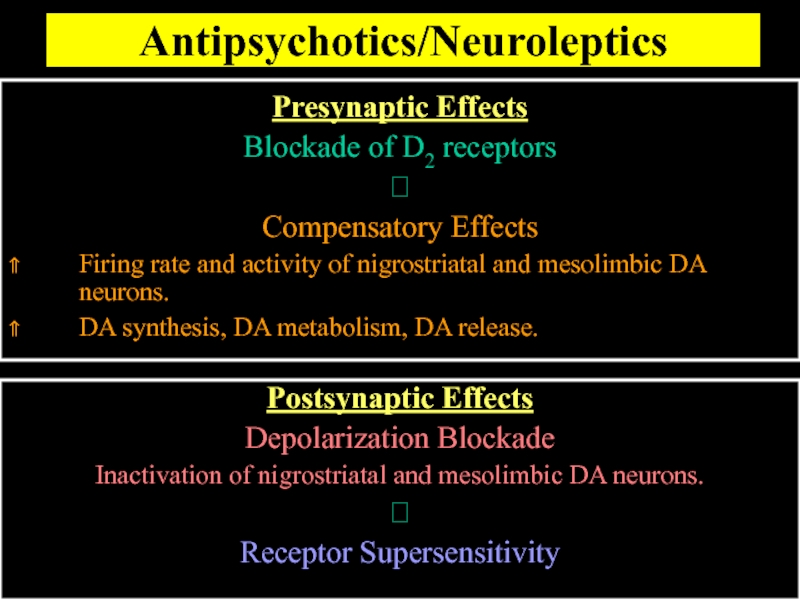
- 49. Antipsychotics/Neuroleptics Presynaptic Effects Blockade of D2 receptors
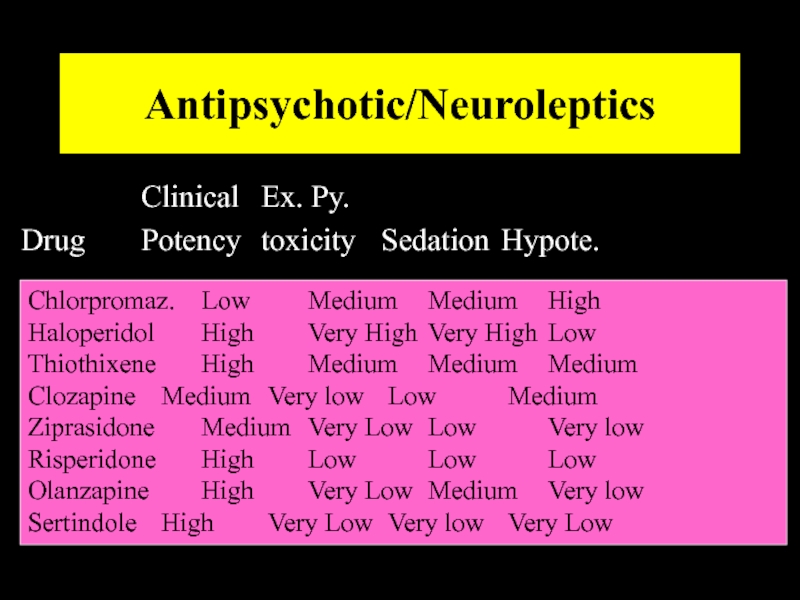
- 50. Antipsychotic/Neuroleptics Clinical Ex. Py. Drug Potency toxicity Sedation Hypote. Chlorpromaz.
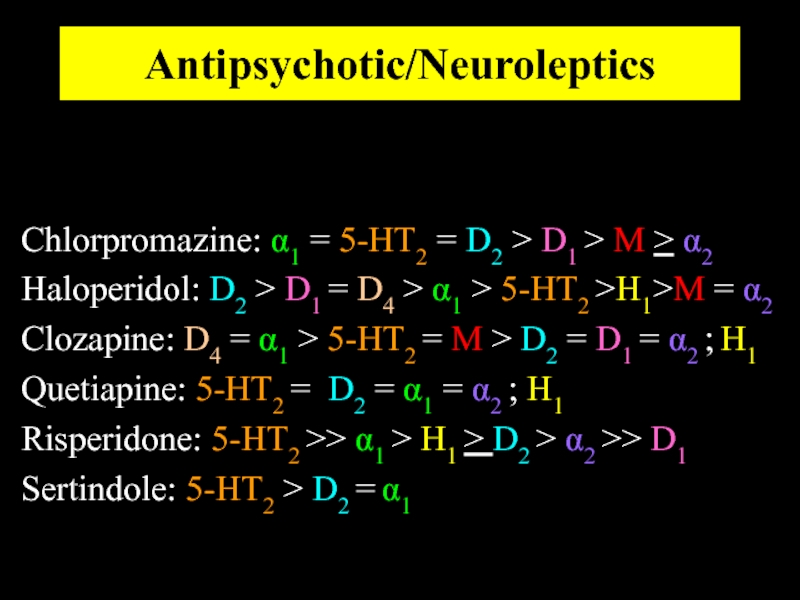
- 51. Antipsychotic/Neuroleptics Chlorpromazine: α1 = 5-HT2 = D2
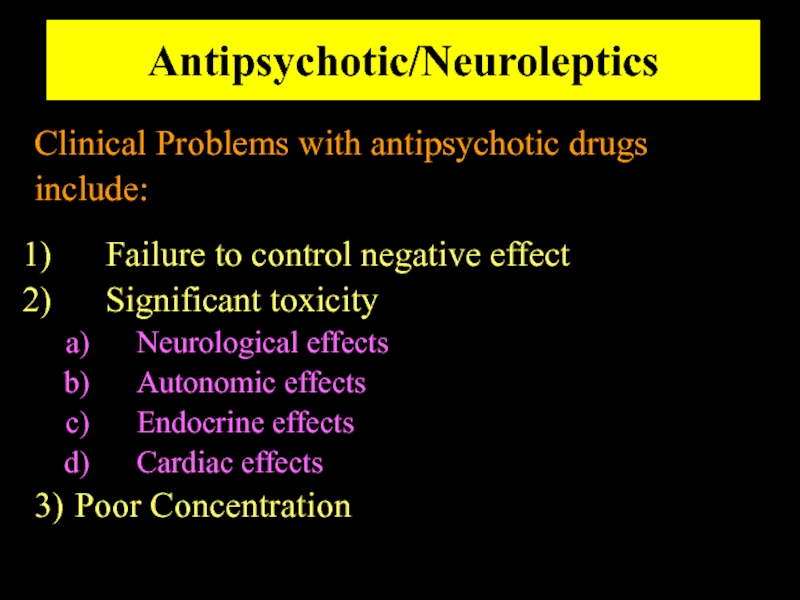
- 52. Antipsychotic/Neuroleptics Clinical Problems with antipsychotic drugs include:
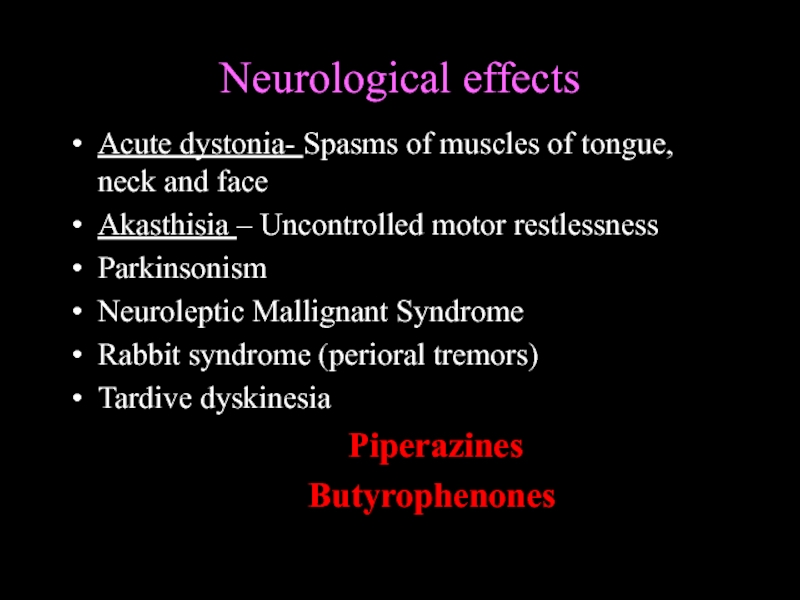
- 53. Neurological effects Acute dystonia- Spasms of
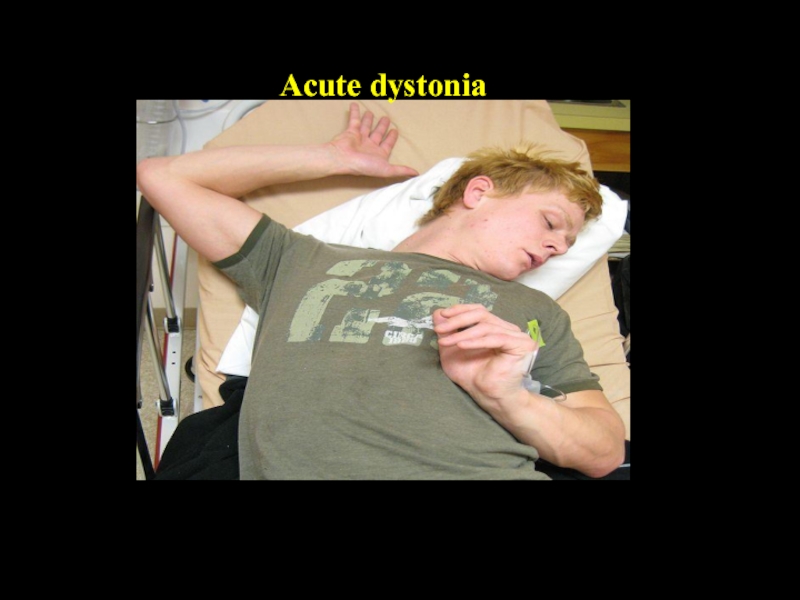
- 54. Acute dystonia
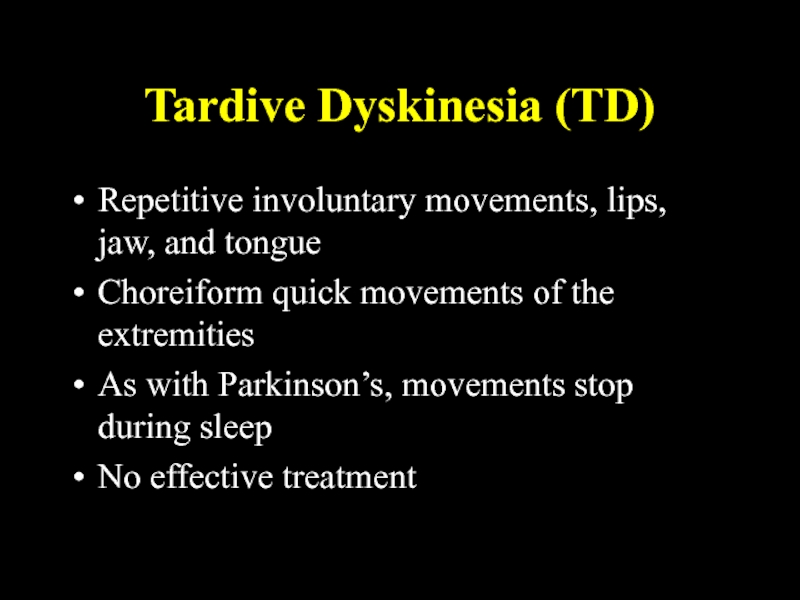
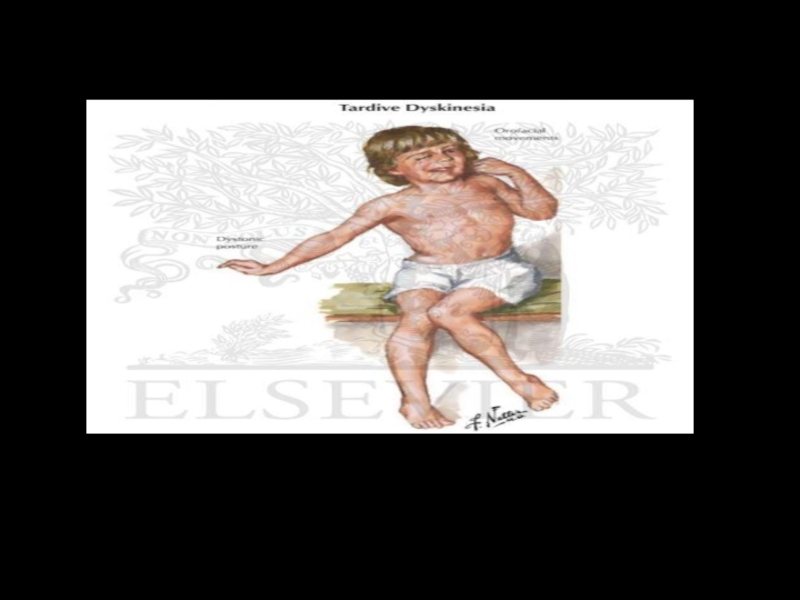
- 55. Tardive Dyskinesia (TD) Repetitive involuntary movements, lips,
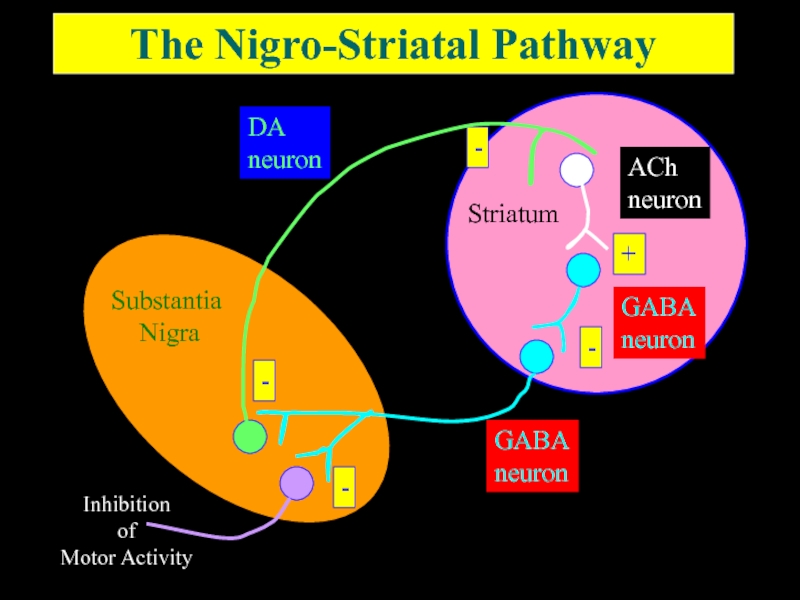
- 57. The Nigro-Striatal Pathway
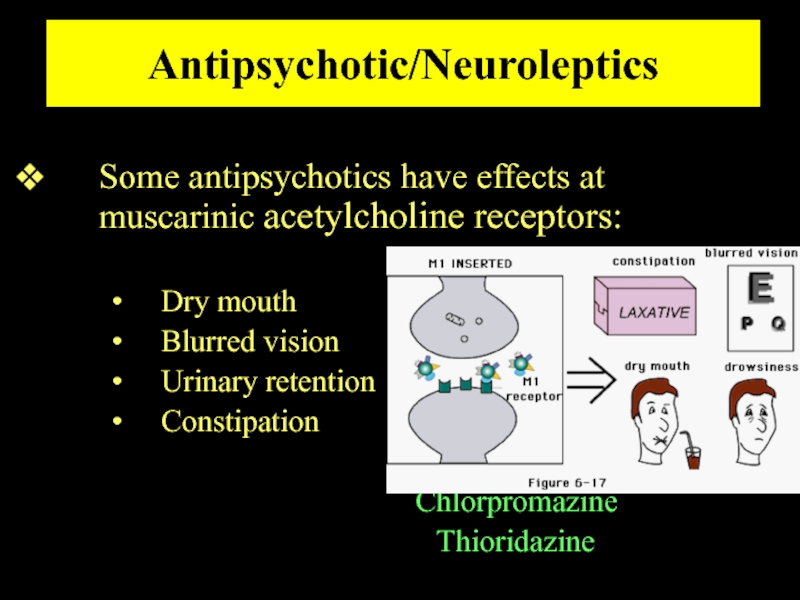
- 58. Antipsychotic/Neuroleptics Some antipsychotics have effects at muscarinic
- 59. Antipsychotic/Neuroleptics Some antipsychotics have effects at α−adrenergic
- 60. Antipsychotic/Neuroleptics Blockade of D2 receptors in lactotrophs
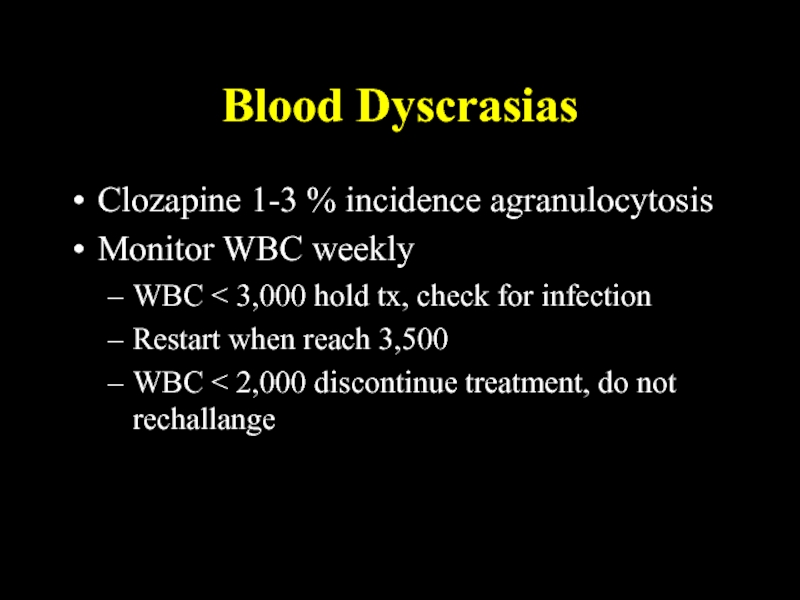
- 61. Blood Dyscrasias Clozapine 1-3 % incidence agranulocytosis
- 62. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Is a
- 63. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Occurs in pts.
- 64. Antipsychotic/Neuroleptics Neuroleptic Malignant Syndrome Treatment
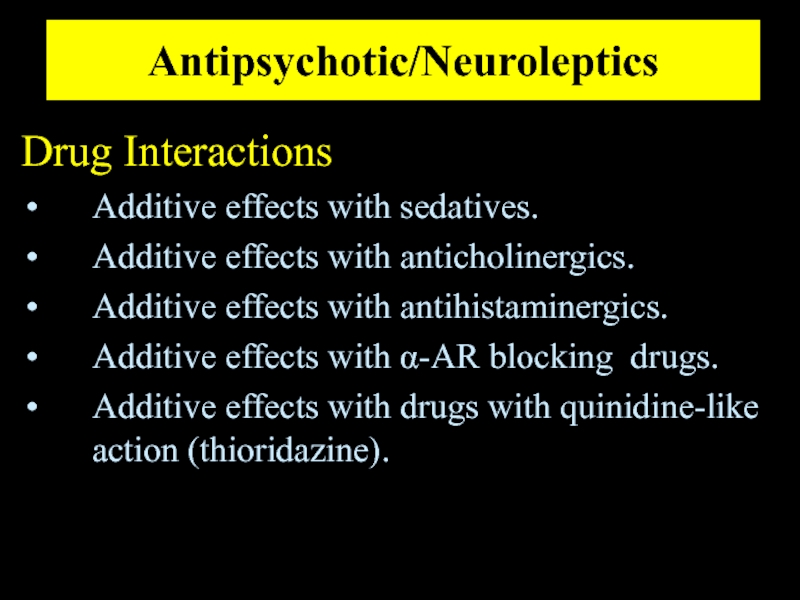
- 65. Antipsychotic/Neuroleptics Drug Interactions Additive effects with sedatives.
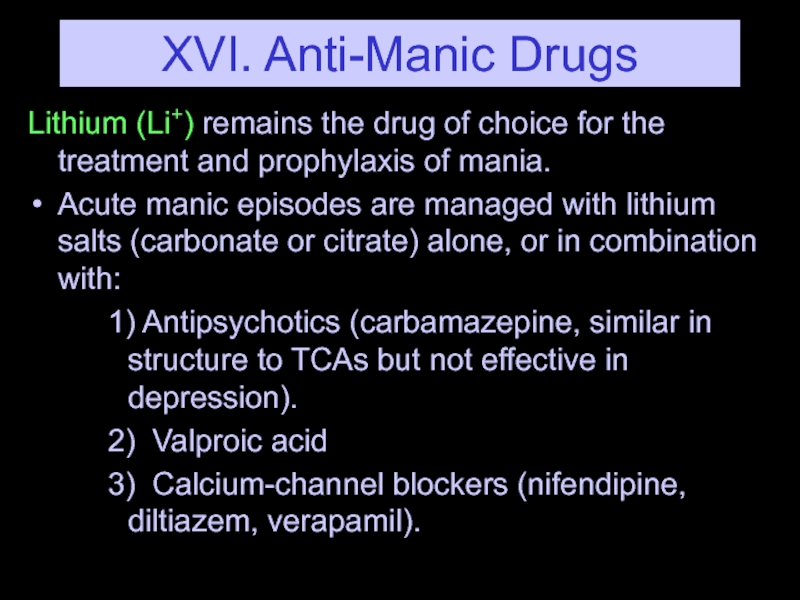
- 66. XVI. Anti-Manic Drugs Lithium (Li+) remains the
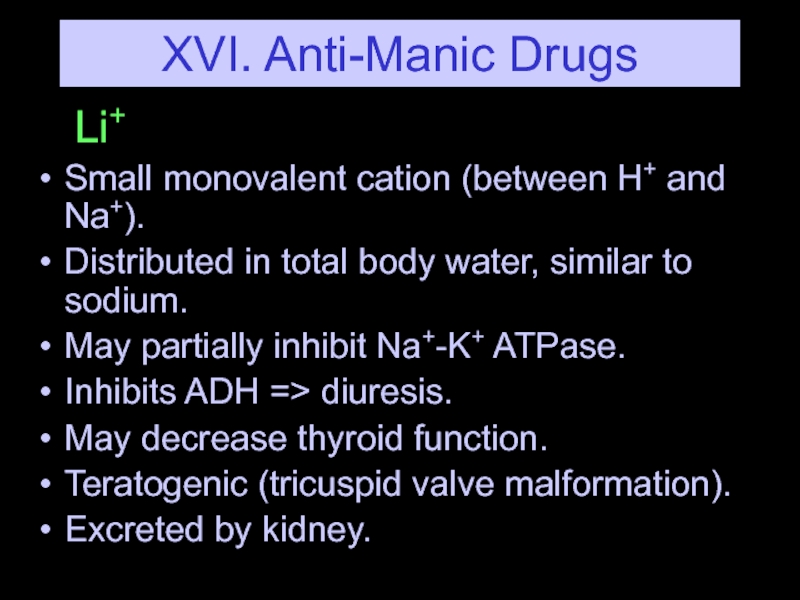
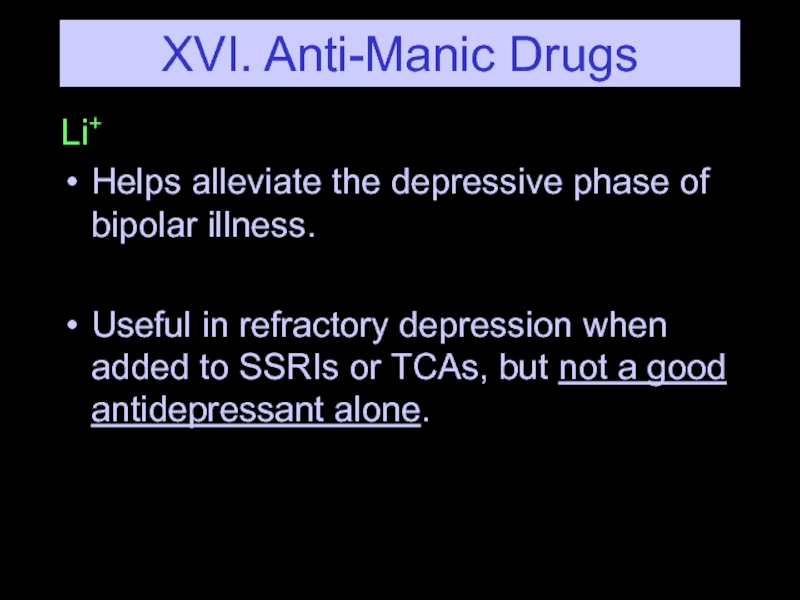
- 67. XVI. Anti-Manic Drugs Li+ Small monovalent cation
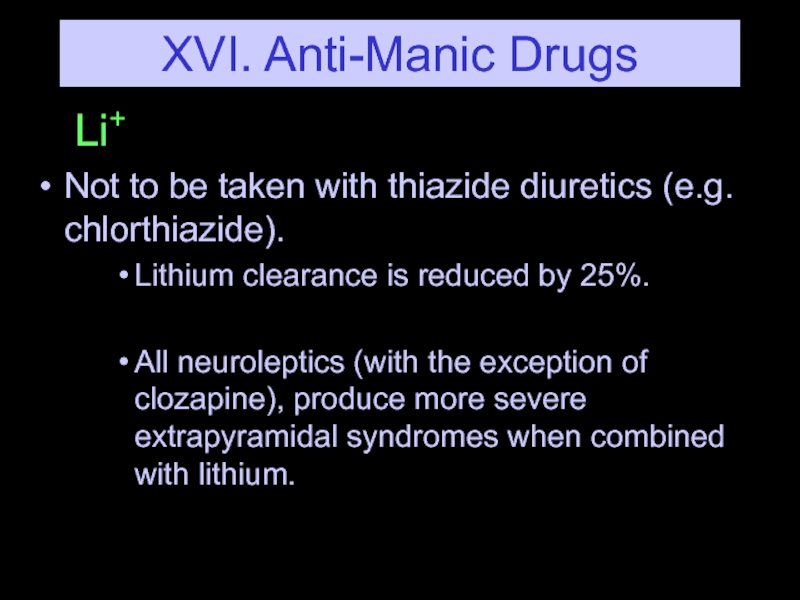
- 68. XVI. Anti-Manic Drugs Li+ Not to be
- 69. XVI. Anti-Manic Drugs Li+ Helps alleviate the
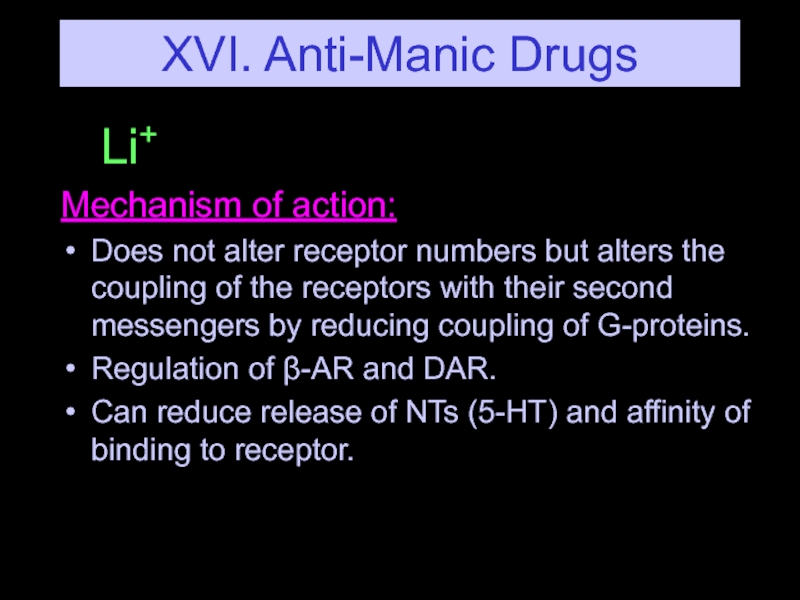
- 70. XVI. Anti-Manic Drugs Li+ Mechanism of action:
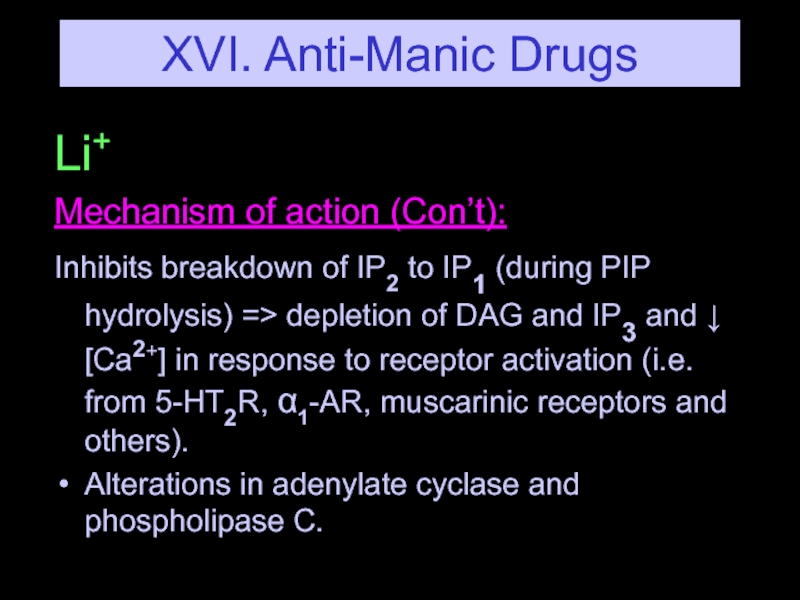
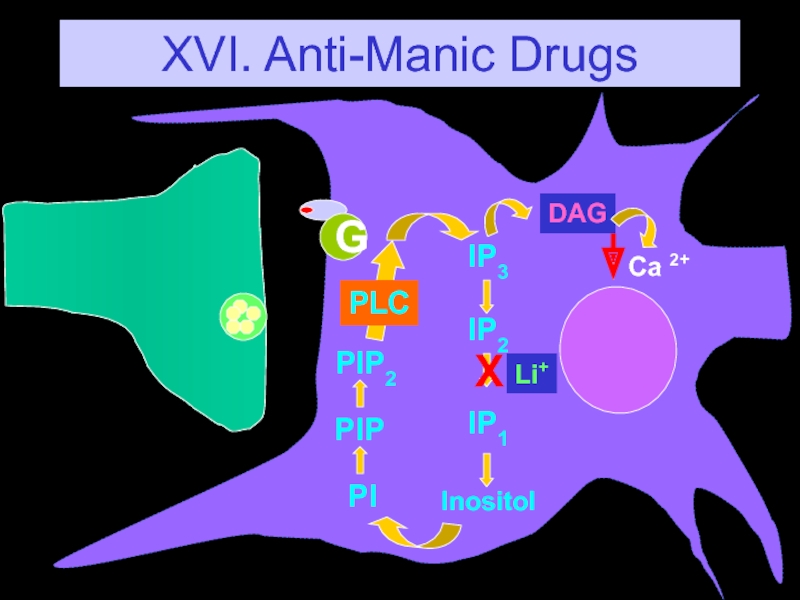
- 71. XVI. Anti-Manic Drugs Li+ Mechanism of action
- 72. XVI. Anti-Manic Drugs
- 73. XVI. Anti-Manic Drugs Valproic Acid A well
- 74. XVI. Anti-Manic Drugs Carbamazepine Effective as an
- 75. XVI. Anti-Manic Drugs Ca2+ Channel blockers Nifedeipine Verapamil Mechanism of action (Con’t): NT Release?
Слайд 2Psychiatric Nosology
(Classification of disease)
Psychosis
Cognitive disorders: confusion, disorientation, memory disturbances and behavioral
disorganization (delirium and dementia)
Mood disorders
Anxiety disorders
Personality disorders
Mood disorders
Anxiety disorders
Personality disorders
Слайд 3Psychosis
Psychosis is a thought disorder characterized by :
Disturbances of reality and
perception
Impaired cognitive functioning
Inappropriate or diminished affect (mood)
Psychosis denotes many mental disorders.
Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance.
Impaired cognitive functioning
Inappropriate or diminished affect (mood)
Psychosis denotes many mental disorders.
Schizophrenia is a particular kind of psychosis characterized mainly by a clear sensorium but a marked thinking disturbance.
Слайд 4Schizophrenia
Pathogenesis is unknown.
Onset of schizophrenia is in the late teens early
twenties.
Genetic predisposition -- Familial incidence.
Multiple genes are involved.
Afflicts 1% of the population worldwide.
May or may not be present with anatomical changes.
Genetic predisposition -- Familial incidence.
Multiple genes are involved.
Afflicts 1% of the population worldwide.
May or may not be present with anatomical changes.
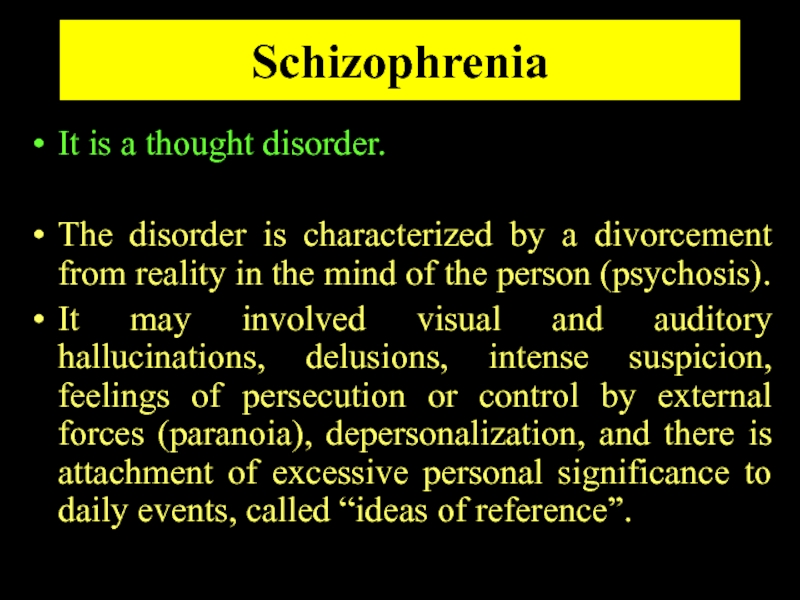
Слайд 5Schizophrenia
It is a thought disorder.
The disorder is characterized by a divorcement
from reality in the mind of the person (psychosis).
It may involved visual and auditory hallucinations, delusions, intense suspicion, feelings of persecution or control by external forces (paranoia), depersonalization, and there is attachment of excessive personal significance to daily events, called “ideas of reference”.
It may involved visual and auditory hallucinations, delusions, intense suspicion, feelings of persecution or control by external forces (paranoia), depersonalization, and there is attachment of excessive personal significance to daily events, called “ideas of reference”.
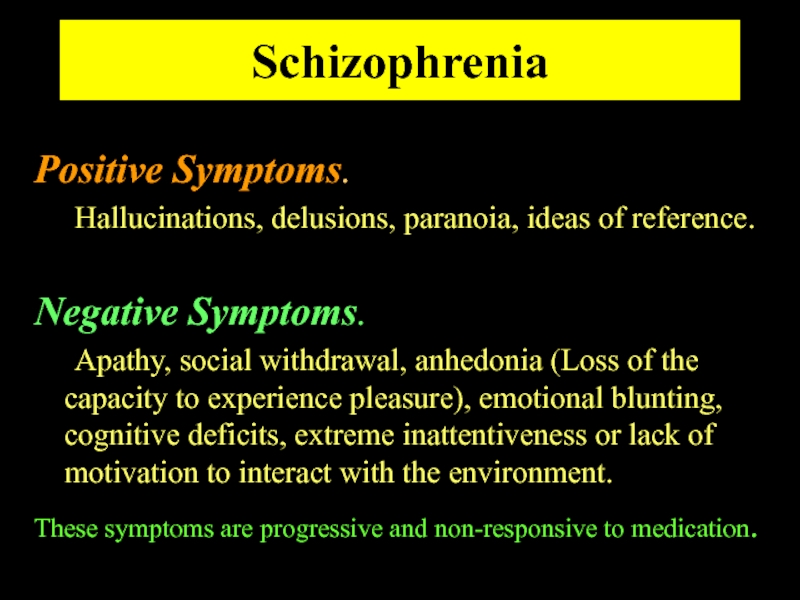
Слайд 6Schizophrenia
Positive Symptoms.
Hallucinations, delusions, paranoia, ideas of reference.
Negative Symptoms.
Apathy, social
withdrawal, anhedonia (Loss of the capacity to experience pleasure), emotional blunting, cognitive deficits, extreme inattentiveness or lack of motivation to interact with the environment.
These symptoms are progressive and non-responsive to medication.
These symptoms are progressive and non-responsive to medication.
Слайд 8Etiology of Schizophrenia
Idiopathic
Biological Correlates
Genetic Factors
Neurodevelopmental abnormalities.
Environmental stressors.
Слайд 9Psychosis Producing Drugs
Levodopa
CNS stimulants
Cocaine
Amphetamines
Khat, cathinone, methcathinone
Apomorphine
Phencyclidine
Слайд 10Etiology of Schizophrenia
Schizophrenia is not characterized by any reproducible neurochemical abnormality.
However, structural and functional abnormalities have been observed in the brains of schizophrenic patients:
Enlarge cerebral ventricles.
Atrophy of cortical layers.
Reduced volume of the basal ganglia.
Enlarge cerebral ventricles.
Atrophy of cortical layers.
Reduced volume of the basal ganglia.
Слайд 11Dopamine Theory of Schizophrenia
Many lines of evidence point to the
aberrant increased activity of the dopaminergic system as being critical in the symptomatology of schizophrenia.
Слайд 12Dopamine Theory of Schizophrenia
Dopamine Correlates:
Antipsychotics reduce dopamine synaptic activity.
These drugs produce
Parkinson-like symptoms.
Drugs that increase DA in the limbic system cause psychosis.
Drugs that reduce DA in the limbic system (postsynaptic D2 antagonists) reduce psychosis.
Increased DA receptor density (Post-mortem, PET).
Changes in amount of homovanillic acid (HVA), a DA metabolite, in plasma, urine, and CSF.
Drugs that increase DA in the limbic system cause psychosis.
Drugs that reduce DA in the limbic system (postsynaptic D2 antagonists) reduce psychosis.
Increased DA receptor density (Post-mortem, PET).
Changes in amount of homovanillic acid (HVA), a DA metabolite, in plasma, urine, and CSF.
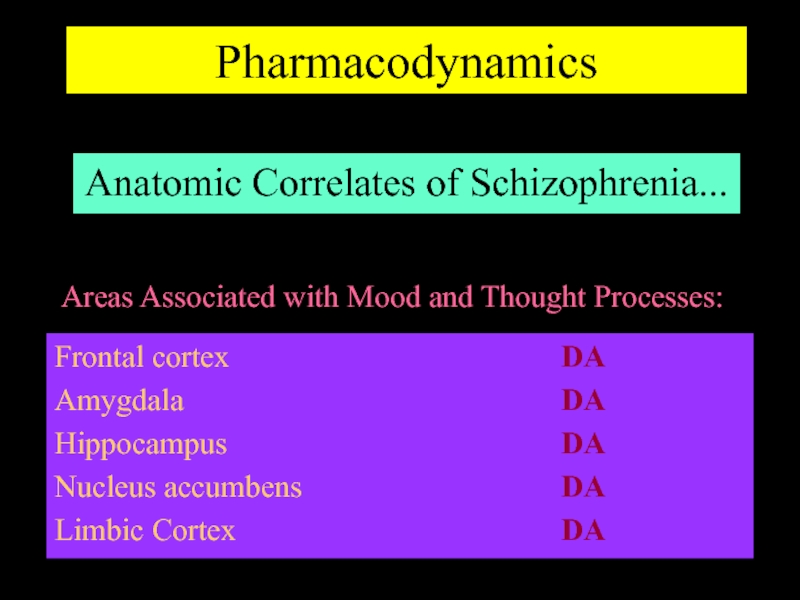
Слайд 13Pharmacodynamics
Anatomic Correlates of Schizophrenia...
Frontal cortex
Amygdala
Hippocampus
Nucleus accumbens
Limbic Cortex
Areas Associated with Mood and
Thought Processes:
DA
DA
DA
DA
DA
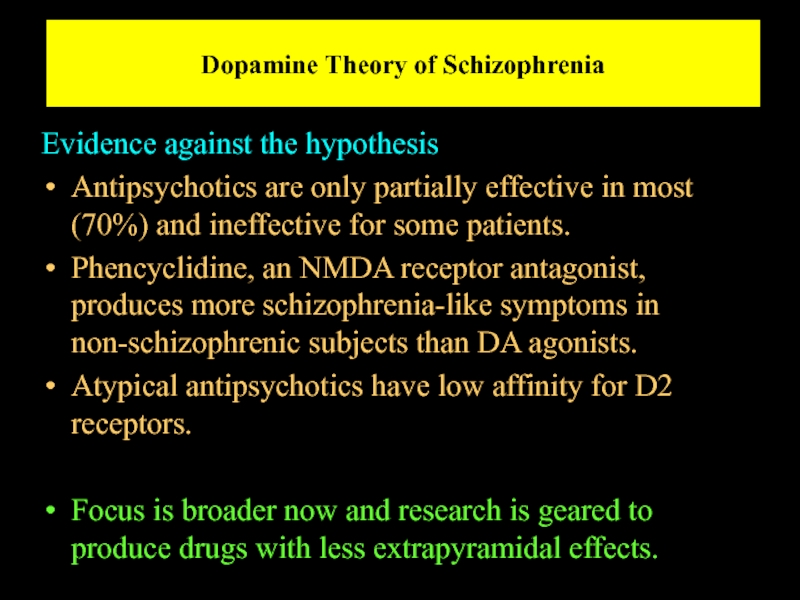
Слайд 14Dopamine Theory of Schizophrenia
Evidence against the hypothesis
Antipsychotics are only partially effective
in most (70%) and ineffective for some patients.
Phencyclidine, an NMDA receptor antagonist, produces more schizophrenia-like symptoms in non-schizophrenic subjects than DA agonists.
Atypical antipsychotics have low affinity for D2 receptors.
Focus is broader now and research is geared to produce drugs with less extrapyramidal effects.
Phencyclidine, an NMDA receptor antagonist, produces more schizophrenia-like symptoms in non-schizophrenic subjects than DA agonists.
Atypical antipsychotics have low affinity for D2 receptors.
Focus is broader now and research is geared to produce drugs with less extrapyramidal effects.
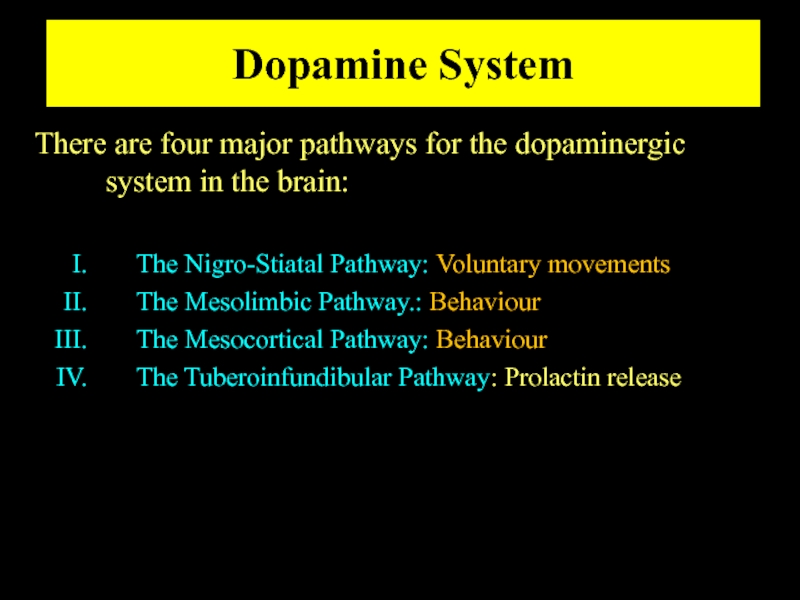
Слайд 15Dopamine System
There are four major pathways for the dopaminergic system in
the brain:
The Nigro-Stiatal Pathway: Voluntary movements
The Mesolimbic Pathway.: Behaviour
The Mesocortical Pathway: Behaviour
The Tuberoinfundibular Pathway: Prolactin release
The Nigro-Stiatal Pathway: Voluntary movements
The Mesolimbic Pathway.: Behaviour
The Mesocortical Pathway: Behaviour
The Tuberoinfundibular Pathway: Prolactin release
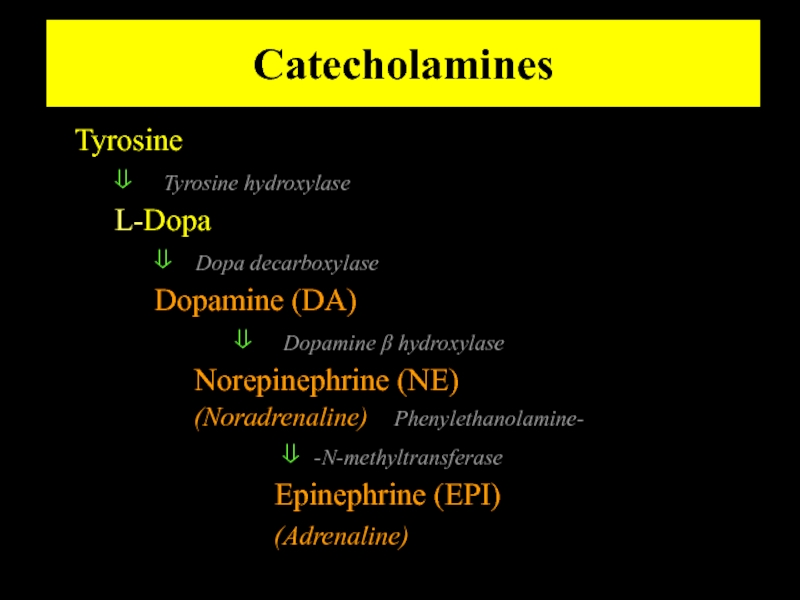
Слайд 17Catecholamines
Tyrosine
⇓ Tyrosine hydroxylase
L-Dopa
⇓ Dopa decarboxylase
Dopamine (DA)
⇓ Dopamine β
hydroxylase
Norepinephrine (NE)
(Noradrenaline) Phenylethanolamine-
⇓ -N-methyltransferase
Epinephrine (EPI)
(Adrenaline)
Norepinephrine (NE)
(Noradrenaline) Phenylethanolamine-
⇓ -N-methyltransferase
Epinephrine (EPI)
(Adrenaline)
Слайд 19Dopamine System
DOPAMINE RECEPTORS
There are at least five subtypes of receptors:
Receptor
D1
D2
D3
D4
D5
Слайд 21Dopamine System
DOPAMINE RECEPTORS
Receptor 2o Messenger System
D1 ⇑cAMP
D2 ⇓cAMP,⇑K+ ch.,⇓Ca2+ch.
D3 ⇓cAMP,⇑K+ ch.,⇑Ca2+ch.
D4 ⇓cAMP
D5 ⇑cAMP
Слайд 24Antipsychotic treatments
Schizophrenia has been around perhaps, since the beginning of humankind,
however, it was not until the last century that it was established as a separate entity amongst other mental disorders.
Many treatments have been devise:
Hydrotherapy:
“The pouring of cold water in a stream, from a height of at least four feet onto the forehead, is one of the most certain means of subsiding violent, maniacal excitement that we have ever seen tried”... wrote an anonymous physician in the early 1800’s.
Many treatments have been devise:
Hydrotherapy:
“The pouring of cold water in a stream, from a height of at least four feet onto the forehead, is one of the most certain means of subsiding violent, maniacal excitement that we have ever seen tried”... wrote an anonymous physician in the early 1800’s.
Слайд 25Antipsychotic treatments
In 1940’s Phenothiazenes were isolated and were used as pre-anesthetic
medication, but quickly were adopted by psychiatrists to calm down their mental patients.
In 1955, chlorpromazine was developed as an antihistaminic agent by Rhône-Pauline Laboratories in France. In-patients at Mental Hospitals dropped by 1/3.
In 1955, chlorpromazine was developed as an antihistaminic agent by Rhône-Pauline Laboratories in France. In-patients at Mental Hospitals dropped by 1/3.
Слайд 26Antipsychotics treatment
Antipsychotics/Neuroleptics
Antipsychotics are the drugs currently used in the prevention
of psychosis.
They have also been termed neuroleptics, because they suppress motor activity and emotionality.
** These drugs are not a cure **
Schizophrenics must be treated with medications indefinitely, in as much as the disease is lifelong and it is preferable to prevent the psychotic episodes than to treat them.
They have also been termed neuroleptics, because they suppress motor activity and emotionality.
** These drugs are not a cure **
Schizophrenics must be treated with medications indefinitely, in as much as the disease is lifelong and it is preferable to prevent the psychotic episodes than to treat them.
Слайд 27Antipsychotics/Neuroleptics
Although the antipsychotic/neuroleptics are drugs used mainly in the treatment of
schizophrenia, they are also used in the treatment of :
Psychoses associated with depression
Manic-depressive illness
Psychosis associated with alzheimer’s disease.
These conditions are life-long and disabling.
Psychoses associated with depression
Manic-depressive illness
Psychosis associated with alzheimer’s disease.
These conditions are life-long and disabling.
Слайд 29Antipsychotic/Neuroleptics
Three major groups :
Phenothiazines
Thioxanthine
Butyrophenones
OLDER DRUGS
Слайд 30Antipsychotic/Neuroleptics
Phenothiazines
Chlorpromazine Thioridazine Fluphenazine
Trifluopromazine Piperacetazine Perfenazine
Mesoridazine Acetophenazine
Carphenazine
Prochlorperazine
Trifluoperazine
Aliphatic Piperidine Piperazine*
* Most likely to
cause extrapyramidal effects.
Слайд 31Antipsychotic/Neuroleptics
2) Thioxanthines
Thiothixene
Chlorprothixene
Closely related to phenothiazines
Слайд 34Atypical Antipsychotic
Pimozide
Atypical Antipsychoitcs
Loxapine
Clozapine
Olanzapine
Qetiapine
Indolones
Sertindole
Ziprasidone
Olindone
Molindone
Risperidone
Слайд 36Antipsychotics/Neuroleptics
Old antipsychotics /neuroleptics are D2 dopamine receptor antagonists. Although they are
also effective antagonists at ACh, 5-HT, NE receptors.
dopamine
receptor
antagonist
D2
Слайд 37Antipsychotics/Neuroleptics
It appears that the specific interaction of antipsychotic drugs with D2
receptors is important to their therapeutic action.
The affinities of most older “classical” agents for the D2 receptors correlate with their clinical potencies as antipsychotics.
The affinities of most older “classical” agents for the D2 receptors correlate with their clinical potencies as antipsychotics.
Слайд 38Antipsychotics/Neuroleptics
Both D1 and D2 receptors are found in high concentrations in
the striatum and the nucleus accumbens.
Clozapine has a higher affinity for the D4 receptors than for D2.
Recently it has been found that most antipsychotic drugs may also bind D3 receptors (therefore, they are non-selective).
Clozapine has a higher affinity for the D4 receptors than for D2.
Recently it has been found that most antipsychotic drugs may also bind D3 receptors (therefore, they are non-selective).
Слайд 39Antipsychotics/Neuroleptics
Antipsychotics produce catalepsy (reduce motor activity).
BLOCKADE OF DOPAMINE RECPTORS IN BASAL
GANGLIA.
Antipsychotics reverse hyperkinetic behaviors (increased locomotion and stereotyped behavior).
BLOCKADE OF DOPAMINE RECPTORS IN LIMBIC AREAS.
Antipsychotics prevent the dopamine inhibition of prolactin release from pituitary.
BLOCKADE OF DOPAMINE RECEPTORS IN PITUITARY.
? hyperprolactinemia
Antipsychotics reverse hyperkinetic behaviors (increased locomotion and stereotyped behavior).
BLOCKADE OF DOPAMINE RECPTORS IN LIMBIC AREAS.
Antipsychotics prevent the dopamine inhibition of prolactin release from pituitary.
BLOCKADE OF DOPAMINE RECEPTORS IN PITUITARY.
? hyperprolactinemia
Слайд 40Pharmacokinetics
Absorption and Distribution
Most antipsychotics are readily but incompletely absorbed.
Significant first-pass metabolism.
Bioavailability
is 25-65%.
Most are highly lipid soluble.
Most are highly protein bound (92-98%).
High volumes of distribution (>7 L/Kg).
Slow elimination.
**Duration of action longer than expected, metabolites are present and relapse occurs, weeks after discontinuation of drug.**
Most are highly lipid soluble.
Most are highly protein bound (92-98%).
High volumes of distribution (>7 L/Kg).
Slow elimination.
**Duration of action longer than expected, metabolites are present and relapse occurs, weeks after discontinuation of drug.**
Слайд 41Pharmacokinetics
Metabolism
Most antipsychotics are almost completely metabolized.
Most have active metabolites, although not
important in therapeutic effect, with one exception. The metabolite of thioridazine, mesoridazine, is more potent than the parent compound and accounts for most of the therapeutic effect.
Слайд 42Pharmacokinetics
Excretion
Antipsychotics are almost completely metabolized and thus, very little is eliminated
unchanged.
Elimination half-lives are 10-24 hrs.
Elimination half-lives are 10-24 hrs.
Слайд 45Antipsychotics/Neuroleptics
Newer drugs have higher affinities for D1, 5-HT or α-AR receptors.
NE,
GABA, Glycine and Glutamate have also been implicated in schizophrenia.
Слайд 46Antipsychotics/Neuroleptics
The acute effects of antipsychotics do not explain why their therapeutic
effects are not evident until 4-8 weeks of treatment.
Blockade of D2 receptors
?
Short term/Compensatory effects:
Firing rate and activity of nigrostriatal and mesolimbic DA neurons.
DA synthesis, DA metabolism, DA release
Blockade of D2 receptors
?
Short term/Compensatory effects:
Firing rate and activity of nigrostriatal and mesolimbic DA neurons.
DA synthesis, DA metabolism, DA release
Слайд 49Antipsychotics/Neuroleptics
Presynaptic Effects
Blockade of D2 receptors
?
Compensatory Effects
Firing rate and activity of nigrostriatal
and mesolimbic DA neurons.
DA synthesis, DA metabolism, DA release.
Postsynaptic Effects
Depolarization Blockade
Inactivation of nigrostriatal and mesolimbic DA neurons.
?
Receptor Supersensitivity
DA synthesis, DA metabolism, DA release.
Postsynaptic Effects
Depolarization Blockade
Inactivation of nigrostriatal and mesolimbic DA neurons.
?
Receptor Supersensitivity
Слайд 50Antipsychotic/Neuroleptics
Clinical Ex. Py.
Drug Potency toxicity Sedation Hypote.
Chlorpromaz. Low Medium Medium High
Haloperidol High Very High Very High Low
Thiothixene High Medium Medium Medium
Clozapine Medium Very low Low Medium
Ziprasidone
Medium Very Low Low Very low
Risperidone High Low Low Low
Olanzapine High Very Low Medium Very low
Sertindole High Very Low Very low Very Low
Risperidone High Low Low Low
Olanzapine High Very Low Medium Very low
Sertindole High Very Low Very low Very Low
Слайд 51Antipsychotic/Neuroleptics
Chlorpromazine: α1 = 5-HT2 = D2 > D1 > M >
α2
Haloperidol: D2 > D1 = D4 > α1 > 5-HT2 >H1>M = α2
Clozapine: D4 = α1 > 5-HT2 = M > D2 = D1 = α2 ; H1
Quetiapine: 5-HT2 = D2 = α1 = α2 ; H1
Risperidone: 5-HT2 >> α1 > H1 > D2 > α2 >> D1
Sertindole: 5-HT2 > D2 = α1
Haloperidol: D2 > D1 = D4 > α1 > 5-HT2 >H1>M = α2
Clozapine: D4 = α1 > 5-HT2 = M > D2 = D1 = α2 ; H1
Quetiapine: 5-HT2 = D2 = α1 = α2 ; H1
Risperidone: 5-HT2 >> α1 > H1 > D2 > α2 >> D1
Sertindole: 5-HT2 > D2 = α1
Слайд 52Antipsychotic/Neuroleptics
Clinical Problems with antipsychotic drugs
include:
Failure to control negative effect
Significant toxicity
Neurological effects
Autonomic
effects
Endocrine effects
Cardiac effects
3) Poor Concentration
Endocrine effects
Cardiac effects
3) Poor Concentration
Слайд 53Neurological effects
Acute dystonia- Spasms of muscles of tongue, neck and face
Akasthisia
– Uncontrolled motor restlessness
Parkinsonism
Neuroleptic Mallignant Syndrome
Rabbit syndrome (perioral tremors)
Tardive dyskinesia
Piperazines
Butyrophenones
Parkinsonism
Neuroleptic Mallignant Syndrome
Rabbit syndrome (perioral tremors)
Tardive dyskinesia
Piperazines
Butyrophenones
Слайд 55Tardive Dyskinesia (TD)
Repetitive involuntary movements, lips, jaw, and tongue
Choreiform quick movements
of the extremities
As with Parkinson’s, movements stop during sleep
No effective treatment
As with Parkinson’s, movements stop during sleep
No effective treatment
Слайд 58Antipsychotic/Neuroleptics
Some antipsychotics have effects at muscarinic acetylcholine receptors:
Dry mouth
Blurred vision
Urinary retention
Constipation
Clozapine
Chlorpromazine
Thioridazine
Слайд 59Antipsychotic/Neuroleptics
Some antipsychotics have effects at α−adrenergic receptors:
orthostatic hypotension
Chlorpromazine
Thioridazine
Some antipsychotics have effects
at H1-histaminergic receptors:
sedation
Risperidone
Haloperidol
sedation
Risperidone
Haloperidol
Слайд 60Antipsychotic/Neuroleptics
Blockade of D2 receptors in lactotrophs in breast increase prolactin concentration
and may produce breast engorgement and galactorrhea.
Слайд 61Blood Dyscrasias
Clozapine 1-3 % incidence agranulocytosis
Monitor WBC weekly
WBC < 3,000 hold
tx, check for infection
Restart when reach 3,500
WBC < 2,000 discontinue treatment, do not rechallange
Restart when reach 3,500
WBC < 2,000 discontinue treatment, do not rechallange
Слайд 62Antipsychotic/Neuroleptics
Neuroleptic Malignant Syndrome
Is a rare but serious side effect of neuroleptic
(antipsychotic) therapy that can be lethal. It can arise at any time in the course of treatment and shows no predilection for age, duration of treatment, antipsychotic medication, or dose.
Слайд 63Antipsychotic/Neuroleptics
Neuroleptic Malignant Syndrome
Occurs in pts. hypersensitive to the Ex.Py. effects of
antipsychotics.
Due to excessively rapid blockade of postsynaptic dopamine receptors.
The syndrome begins with marked muscle rigidity.
If sweating is impaired, a fever may ensue. The stress leukocytosis and high fever associated with this syndrome may be mistaken for an infection.
Autonomic instability with altered blood pressure and heart rate is another midbrain manifestation.
Creatine kinase isozymes are usually elevated, reflecting muscle damage.
Due to excessively rapid blockade of postsynaptic dopamine receptors.
The syndrome begins with marked muscle rigidity.
If sweating is impaired, a fever may ensue. The stress leukocytosis and high fever associated with this syndrome may be mistaken for an infection.
Autonomic instability with altered blood pressure and heart rate is another midbrain manifestation.
Creatine kinase isozymes are usually elevated, reflecting muscle damage.
Слайд 64Antipsychotic/Neuroleptics
Neuroleptic Malignant Syndrome
Treatment
Vigorous treatment with antiparkinsonian drugs is recommended as
soon as possible.
Muscle relaxants such as diazepam, dantrolene or bromocriptine may be helpful.
Muscle relaxants such as diazepam, dantrolene or bromocriptine may be helpful.
Слайд 65Antipsychotic/Neuroleptics
Drug Interactions
Additive effects with sedatives.
Additive effects with anticholinergics.
Additive effects with antihistaminergics.
Additive
effects with α-AR blocking drugs.
Additive effects with drugs with quinidine-like action (thioridazine).
Additive effects with drugs with quinidine-like action (thioridazine).
Слайд 66XVI. Anti-Manic Drugs
Lithium (Li+) remains the drug of choice for the
treatment and prophylaxis of mania.
Acute manic episodes are managed with lithium salts (carbonate or citrate) alone, or in combination with:
1) Antipsychotics (carbamazepine, similar in structure to TCAs but not effective in depression).
2) Valproic acid
3) Calcium-channel blockers (nifendipine, diltiazem, verapamil).
Acute manic episodes are managed with lithium salts (carbonate or citrate) alone, or in combination with:
1) Antipsychotics (carbamazepine, similar in structure to TCAs but not effective in depression).
2) Valproic acid
3) Calcium-channel blockers (nifendipine, diltiazem, verapamil).
Слайд 67XVI. Anti-Manic Drugs
Li+
Small monovalent cation (between H+ and Na+).
Distributed in total
body water, similar to sodium.
May partially inhibit Na+-K+ ATPase.
Inhibits ADH => diuresis.
May decrease thyroid function.
Teratogenic (tricuspid valve malformation).
Excreted by kidney.
May partially inhibit Na+-K+ ATPase.
Inhibits ADH => diuresis.
May decrease thyroid function.
Teratogenic (tricuspid valve malformation).
Excreted by kidney.
Слайд 68XVI. Anti-Manic Drugs
Li+
Not to be taken with thiazide diuretics (e.g. chlorthiazide).
Lithium
clearance is reduced by 25%.
All neuroleptics (with the exception of clozapine), produce more severe extrapyramidal syndromes when combined with lithium.
All neuroleptics (with the exception of clozapine), produce more severe extrapyramidal syndromes when combined with lithium.
Слайд 69XVI. Anti-Manic Drugs
Li+
Helps alleviate the depressive phase of bipolar illness.
Useful in
refractory depression when added to SSRIs or TCAs, but not a good antidepressant alone.
Слайд 70XVI. Anti-Manic Drugs
Li+
Mechanism of action:
Does not alter receptor numbers but alters
the coupling of the receptors with their second messengers by reducing coupling of G-proteins.
Regulation of β-AR and DAR.
Can reduce release of NTs (5-HT) and affinity of binding to receptor.
Regulation of β-AR and DAR.
Can reduce release of NTs (5-HT) and affinity of binding to receptor.
Слайд 71XVI. Anti-Manic Drugs
Li+
Mechanism of action (Con’t):
Inhibits breakdown of IP2 to IP1
(during PIP hydrolysis) => depletion of DAG and IP3 and ↓ [Ca2+] in response to receptor activation (i.e. from 5-HT2R, α1-AR, muscarinic receptors and others).
Alterations in adenylate cyclase and phospholipase C.
Alterations in adenylate cyclase and phospholipase C.
Слайд 73XVI. Anti-Manic Drugs
Valproic Acid
A well known antiepileptic has been found to
have antimanic effects. Shows efficacy equivalent as that of lithium during the early weeks of treatment and is being evaluated for maintenance treatment. Titrated well, the sedation can be controlled. Nausea being the only limiting factor in some patients.
May be used as first line treatment for mania, although it may not be as effective in maintenance treatment as lithium for some patients.
Mechanism of action: ???
May be used as first line treatment for mania, although it may not be as effective in maintenance treatment as lithium for some patients.
Mechanism of action: ???
Слайд 74XVI. Anti-Manic Drugs
Carbamazepine
Effective as an antimania medication
Mechanism of action (Con’t):
May be
due to decrease overexcitability of neurons (anticonvulsive effect).



![Antipsychotic/Neuroleptics[Drug dose]EffectPiperazineAliphaticPiperidine](/img/tmb/3/283261/a210a653ba3dc503353523a8f093ee3e-800x.jpg)
![Antipsychotic/Neuroleptics[Drug dose]EffectPhenothiazine d.Thioxanthene d.Butyrophenone d.](/img/tmb/3/283261/594572680d102485db8ec3e1e8914d07-800x.jpg)