FRCPG
Associate Professor of cardiology
NICVD, Dhaka
- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Beta-blockers презентация
Содержание
- 1. Beta-blockers
- 2. Introduction and history Beta blockers (sometimes written
- 3. Introduction Beta blockers block the action of
- 4. Indications for beta blockers Angina pectoris
- 5. Beta blockers have also been used in
- 6. Adverse effects Adverse drug reactions(ADRs) associated
- 7. Adverse effects associated with β2-adrenergic receptor antagonist
- 8. Precautions Beta blockers must not be used
- 9. Toxicity Glucagon has been used in
- 10. β-Receptor antagonism Stimulation of β1 receptors
- 11. β-Receptor antagonism Antianginal effects result from negative
- 12. Intrinsic sympathomimetic activity Also referred to
- 13. Effects of beta blockers α1-Receptor antagonism Some
- 14. Non-selective agents Alprenolol Bucindolol Carteolol
- 15. β1-Selective agents Acebutolol (has intrinsic sympathomimetic
- 16. β2-Selective agents Butaxamine (weak α-adrenergic agonist
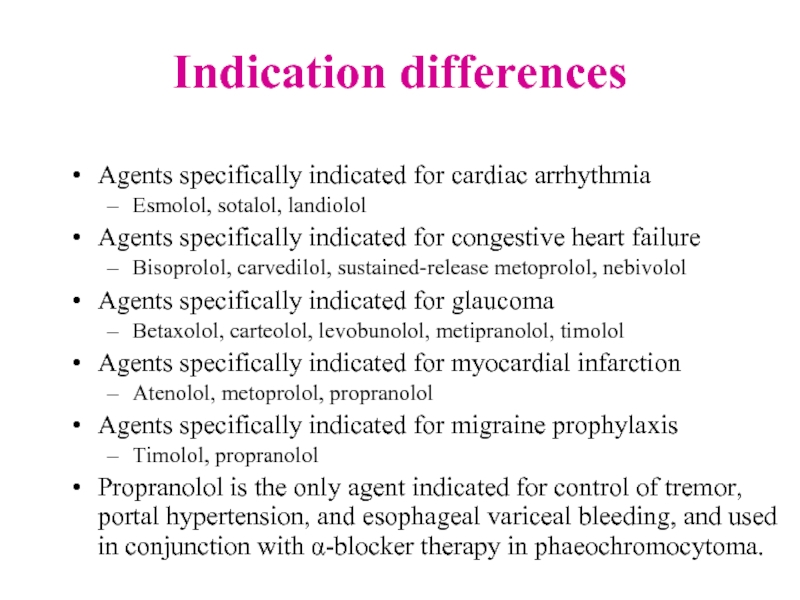
- 17. Indication differences Agents specifically indicated for
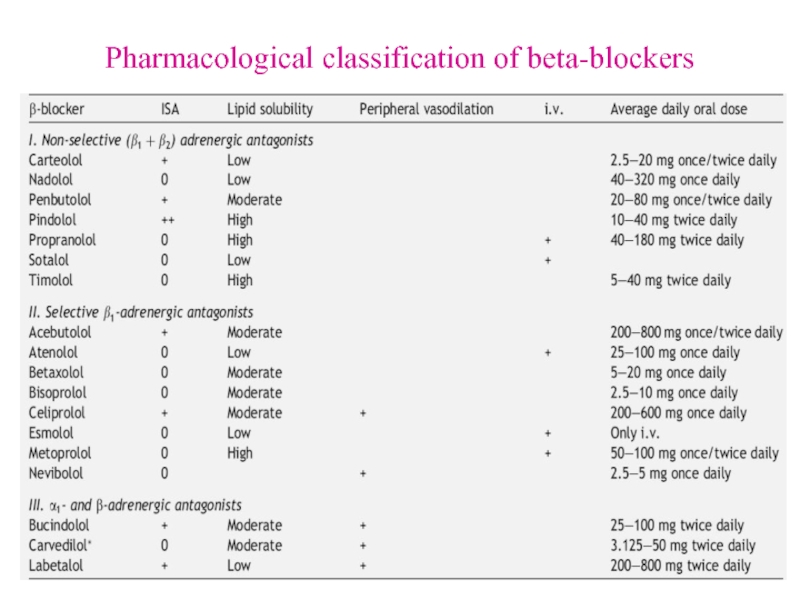
- 18. Pharmacological classification of beta-blockers
- 19. Effects mediated by beta- receptors
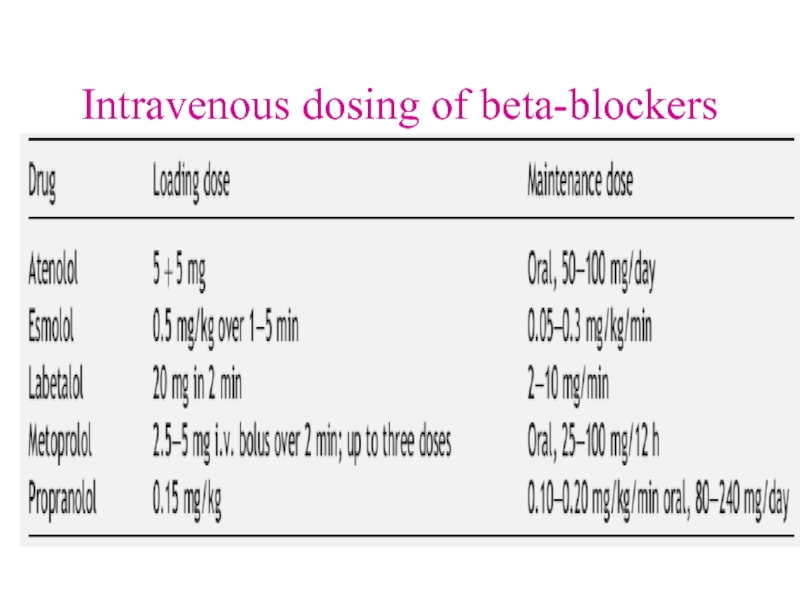
- 20. Intravenous dosing of beta-blockers
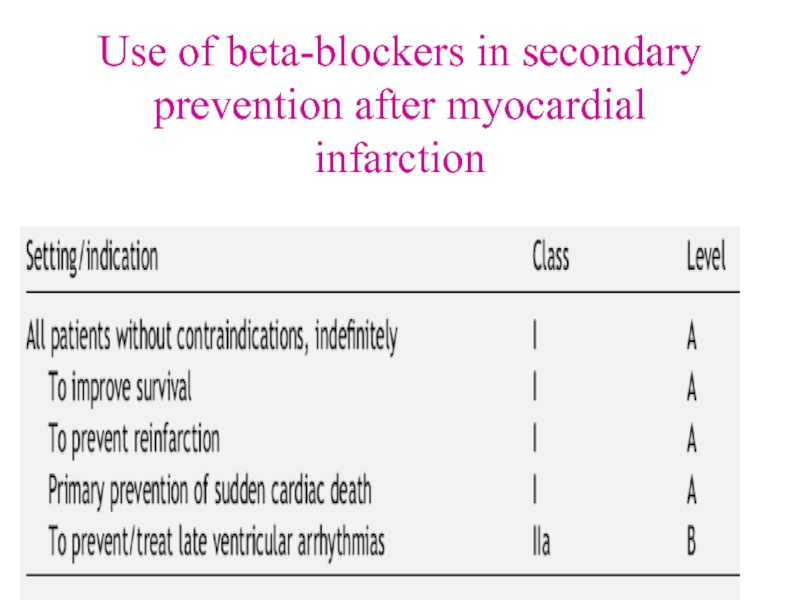
- 21. Use of beta-blockers in AMI
- 22. Use of beta-blockers in secondary prevention after myocardial infarction
- 23. Use of beta-blockers in non-ST segment elevation ACS
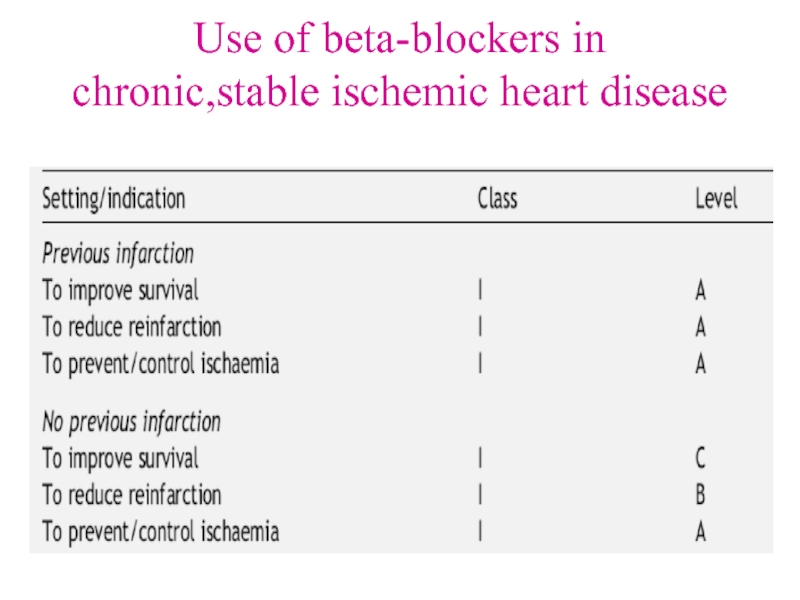
- 24. Use of beta-blockers in chronic,stable ischemic heart disease
- 25. Use of beta-blockers in chronic heart failure
- 26. Practical guidance on using b-adrenergic blockers in heart failure
- 27. Practical guidance on using b-adrenergic blockers in heart failure
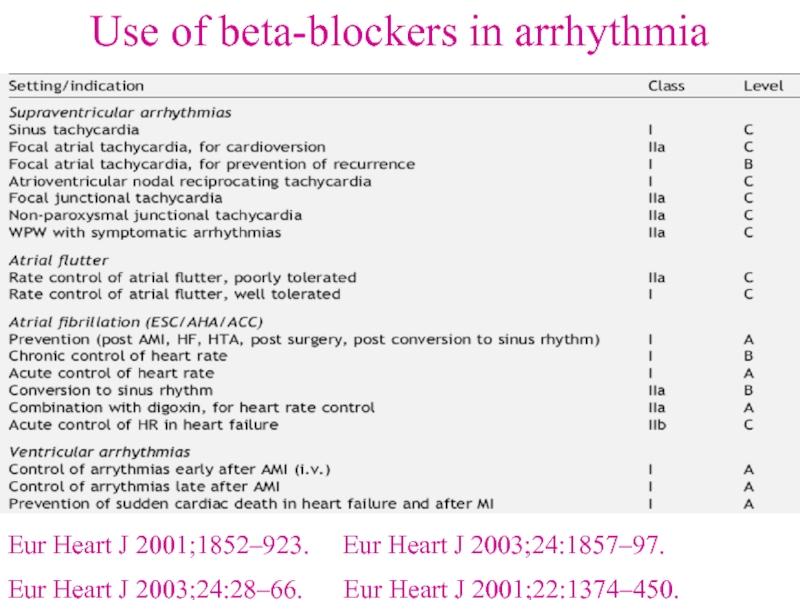
- 28. Use of beta-blockers in arrhythmia Eur Heart
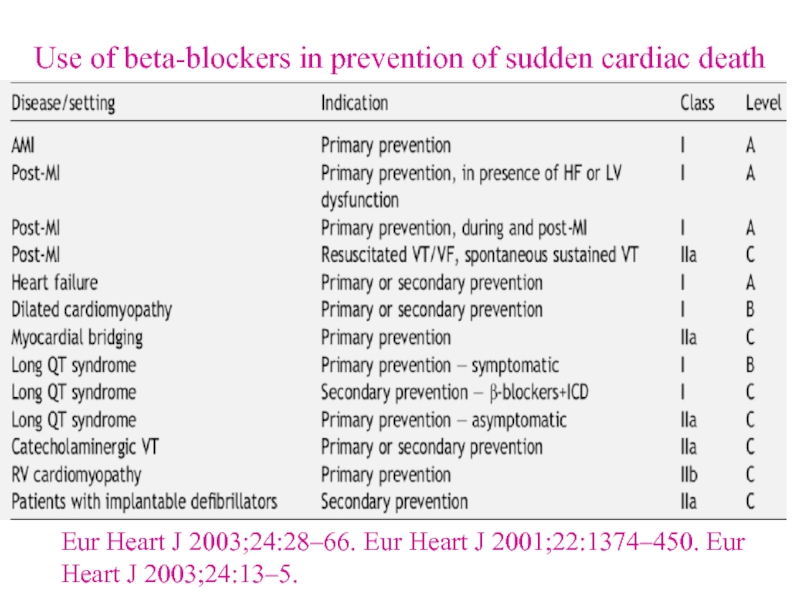
- 29. Use of beta-blockers in prevention of sudden
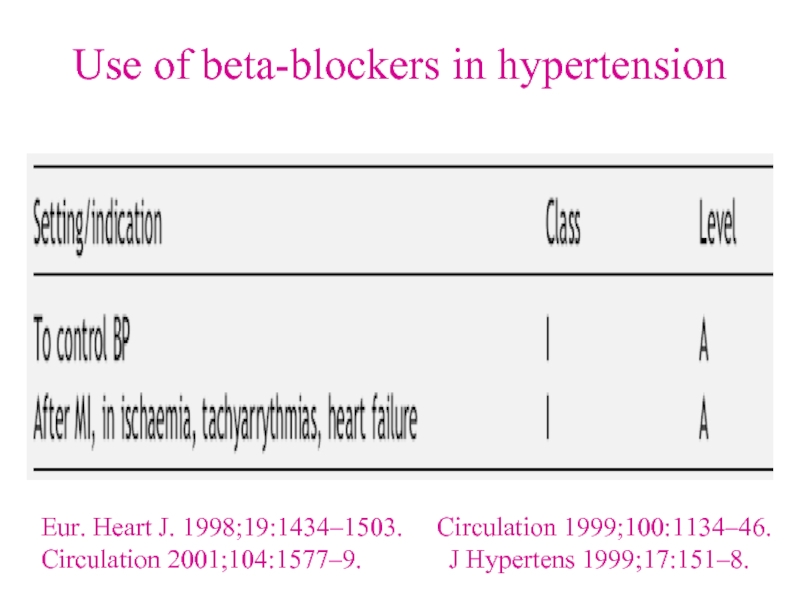
- 30. Use of beta-blockers in hypertension Eur. Heart
- 31. Use of beta-blockers in aortic dissection Eur Heart J 2001;22:1642–81.
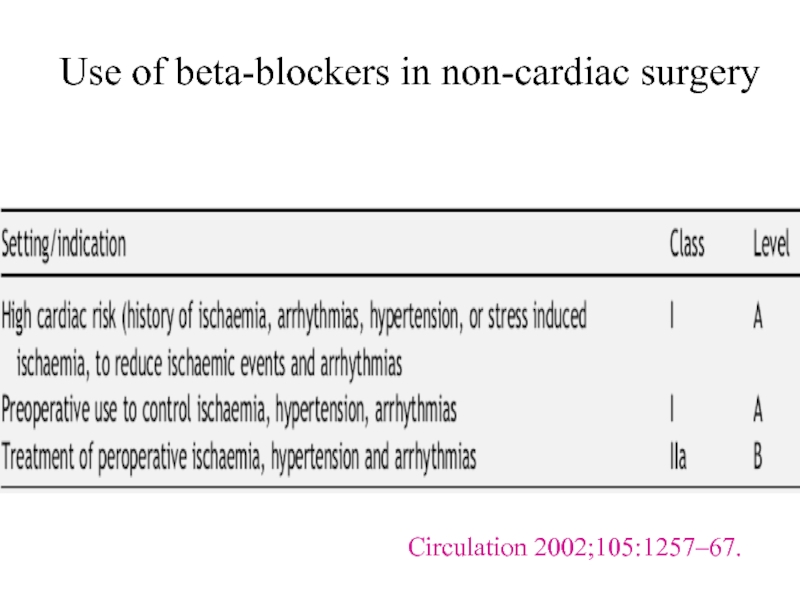
- 32. Use of beta-blockers in non-cardiac surgery Circulation 2002;105:1257–67.
- 33. Classes of Recommendations
- 34. Levels of Evidence
- 35. THANK YOU ALL
Слайд 1Beta-blockers
Dr.Md.Toufiqur Rahman
FCPS, MD, FACC, FESC, FRCPE, FSCAI, MBBS, FAHA, FSCAI,
FCCP,
Слайд 2Introduction and history
Beta blockers (sometimes written as β-blockers) or beta-adrenergic blocking
agents, beta-adrenergic antagonists, or beta antagonists, are a class of drugs used for various indications, but particularly for the management of cardiac arrhythmias, cardioprotection after myocardial infarction (heart attack), and hypertension As beta adrenergic receptor antagonists, they diminish the effects of epinephrine (adrenaline) and other stress hormones. In 1958 the first beta blocker, dichloroisoproterenol, was synthesised by Eli Lilly Laboratories, but it was Sir James W. Black in 1962, who found the first clinically significant use of beta blockers with propranolol and pronethalol; it revolutionized the medical management of angina pectoris and is considered by many to be one of the most important contributions to clinical medicine and pharmacology of the 20th century.
Слайд 3Introduction
Beta blockers block the action of endogenous catecholamines (epinephrine (adrenaline) and
norepinephrine (noradrenaline) in particular), on β-adrenergic receptors, part of the sympathetic nervous system which mediates the "fight or flight" response. There are three known types of beta receptor, designated β1, β2 and β3 receptors. β1-adrenergic receptors are located mainly in the heart and in the kidneys. β2-adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle.β3-adrenergic receptors are located in fat cells.
Слайд 4Indications for beta blockers
Angina pectoris
Atrial fibrillation
Cardiac arrhythmia
Congestive heart failure
Essential
tremor
Glaucoma
Hypertension
Migraine prophylaxis
Mitral valve prolapse
Myocardial infarction
Phaeochromocytoma, in conjunction with α-blocker
Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
Glaucoma
Hypertension
Migraine prophylaxis
Mitral valve prolapse
Myocardial infarction
Phaeochromocytoma, in conjunction with α-blocker
Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
Слайд 5Beta blockers have also been used in the following conditions
Acute aortic
dissection
Hypertrophic obstructive cardiomyopathy
Marfan syndrome (treatment with propranolol slows progression of aortic dilation and its complications)
Prevention of variceal bleeding in portal hypertension
Possible mitigation of hyperhidrosis
Social anxiety disorder and other anxiety disorders
Hypertrophic obstructive cardiomyopathy
Marfan syndrome (treatment with propranolol slows progression of aortic dilation and its complications)
Prevention of variceal bleeding in portal hypertension
Possible mitigation of hyperhidrosis
Social anxiety disorder and other anxiety disorders
Слайд 6Adverse effects
Adverse drug reactions(ADRs) associated with the use of beta blockers
include: nausea, diarrhoea, bronchospasm, dyspnea, cold extremities, exacerbation of Raynaud's syndrome, bradycardia, hypotension, heart failure, heart block, fatigue, dizziness, alopecia (hair loss), abnormal vision, hallucinations, insomnia, nightmares, sexual dysfunction, erectile dysfunction and/or alteration of glucose and lipid metabolism. Mixed α1/β-antagonist therapy is also commonly associated with orthostatic hypotension. Carvedilol therapy is commonly associated with edema.
Central nervous system (CNS) adverse effects (hallucinations, insomnia, nightmares) are more common in agents with greater lipid solubility, which are able to cross the blood-brain barrier into the CNS. Similarly, CNS adverse effects are less common in agents with greater aqueous solubility.
Central nervous system (CNS) adverse effects (hallucinations, insomnia, nightmares) are more common in agents with greater lipid solubility, which are able to cross the blood-brain barrier into the CNS. Similarly, CNS adverse effects are less common in agents with greater aqueous solubility.
Слайд 7Adverse effects associated with β2-adrenergic receptor antagonist activity (bronchospasm, peripheral vasoconstriction,
alteration of glucose and lipid metabolism) are less common with β1-selective (often termed "cardioselective") agents, however receptor selectivity diminishes at higher doses. Beta blockade, especially of the beta-1 receptor at the macula densa inhibits renin release, thus decreasing the release of aldosterone. This causes hyponatremia and hyperkalemia.
A 2007 study revealed that diuretics and beta-blockers used for hypertension increase a patient's risk of developing diabetes while ACE inhibitors and Angiotensin II receptor antagonists (Angiotensin Receptor Blockers) actually decrease the risk of diabetes. Clinical guidelines in Great Britain, but not in the United States, call for avoiding diuretics and beta-blockers as first-line treatment of hypertension due to the risk of diabetes.
A 2007 study revealed that diuretics and beta-blockers used for hypertension increase a patient's risk of developing diabetes while ACE inhibitors and Angiotensin II receptor antagonists (Angiotensin Receptor Blockers) actually decrease the risk of diabetes. Clinical guidelines in Great Britain, but not in the United States, call for avoiding diuretics and beta-blockers as first-line treatment of hypertension due to the risk of diabetes.
Adverse effects
Слайд 8Precautions
Beta blockers must not be used in the treatment of cocaine,
amphetamine, or other alpha adrenergic stimulant overdose. The blockade of only beta receptors increases hypertension, reduces coronary blood flow, left ventricular function, and cardiac output and tissue perfusion by means of leaving the alpha adrenergic system stimulation unopposed. The appropriate antihypertensive drugs to administer during hypertensive crisis resulting from stimulant abuse are vasodilators like nitroglycerin, diuretics like furosemide and alpha blockers like phentolamine.
Слайд 9Toxicity
Glucagon has been used in the treatment of overdose. Glucagon has
a positive inotropic action on the heart and decreases renal vascular resistance. It is therefore useful in patients with beta-blocker cardiotoxicity. Cardiac pacing should be reserved for patients unresponsive to pharmacological therapy.
Patients who experience bronchospasm due to the B2 blocking effects of non-selective beta-blockers may be treated with anticholinergic drugs such as Ipratropium, which are safer than beta agonists in patients with cardiovascular disease.
Patients who experience bronchospasm due to the B2 blocking effects of non-selective beta-blockers may be treated with anticholinergic drugs such as Ipratropium, which are safer than beta agonists in patients with cardiovascular disease.
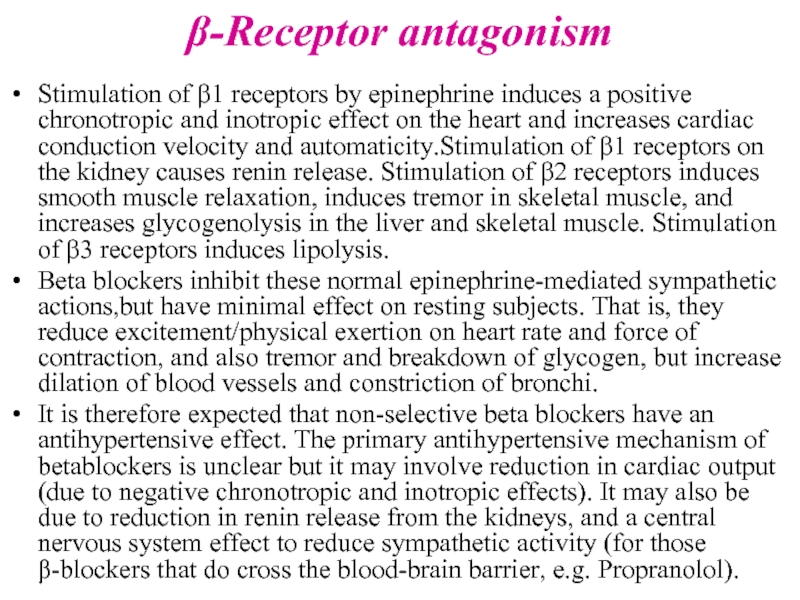
Слайд 10β-Receptor antagonism
Stimulation of β1 receptors by epinephrine induces a positive chronotropic
and inotropic effect on the heart and increases cardiac conduction velocity and automaticity.Stimulation of β1 receptors on the kidney causes renin release. Stimulation of β2 receptors induces smooth muscle relaxation, induces tremor in skeletal muscle, and increases glycogenolysis in the liver and skeletal muscle. Stimulation of β3 receptors induces lipolysis.
Beta blockers inhibit these normal epinephrine-mediated sympathetic actions,but have minimal effect on resting subjects. That is, they reduce excitement/physical exertion on heart rate and force of contraction, and also tremor and breakdown of glycogen, but increase dilation of blood vessels and constriction of bronchi.
It is therefore expected that non-selective beta blockers have an antihypertensive effect. The primary antihypertensive mechanism of betablockers is unclear but it may involve reduction in cardiac output (due to negative chronotropic and inotropic effects). It may also be due to reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity (for those β-blockers that do cross the blood-brain barrier, e.g. Propranolol).
Beta blockers inhibit these normal epinephrine-mediated sympathetic actions,but have minimal effect on resting subjects. That is, they reduce excitement/physical exertion on heart rate and force of contraction, and also tremor and breakdown of glycogen, but increase dilation of blood vessels and constriction of bronchi.
It is therefore expected that non-selective beta blockers have an antihypertensive effect. The primary antihypertensive mechanism of betablockers is unclear but it may involve reduction in cardiac output (due to negative chronotropic and inotropic effects). It may also be due to reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity (for those β-blockers that do cross the blood-brain barrier, e.g. Propranolol).
Слайд 11β-Receptor antagonism
Antianginal effects result from negative chronotropic and inotropic effects, which
decrease cardiac workload and oxygen demand. Negative chronotropic properties of beta blockers allow the lifesaving property of heart rate control. Beta blockers are readily titrated to optimal rate control in many pathologic states.
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade – resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade.
Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin angiotensin aldosterone system with a resultant decrease in blood pressure due to decreased sodium and water retention.
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade – resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade.
Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin angiotensin aldosterone system with a resultant decrease in blood pressure due to decreased sodium and water retention.
Слайд 12Intrinsic sympathomimetic activity
Also referred to as intrinsic sympathomimetic effect, this term
is used particularly with beta blockers that can show both agonism and antagonism at a given beta receptor, depending on the concentration of the agent (beta blocker) and the concentration of the antagonized agent (usually an endogenous compound such as norepinephrine.
Some beta blockers (e.g. oxprenolol, pindolol, penbutolol and acebutolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy.
Agents with ISA are not used in post-myocardial infarction as they have not been demonstrated to be beneficial. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.
Some beta blockers (e.g. oxprenolol, pindolol, penbutolol and acebutolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy.
Agents with ISA are not used in post-myocardial infarction as they have not been demonstrated to be beneficial. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.
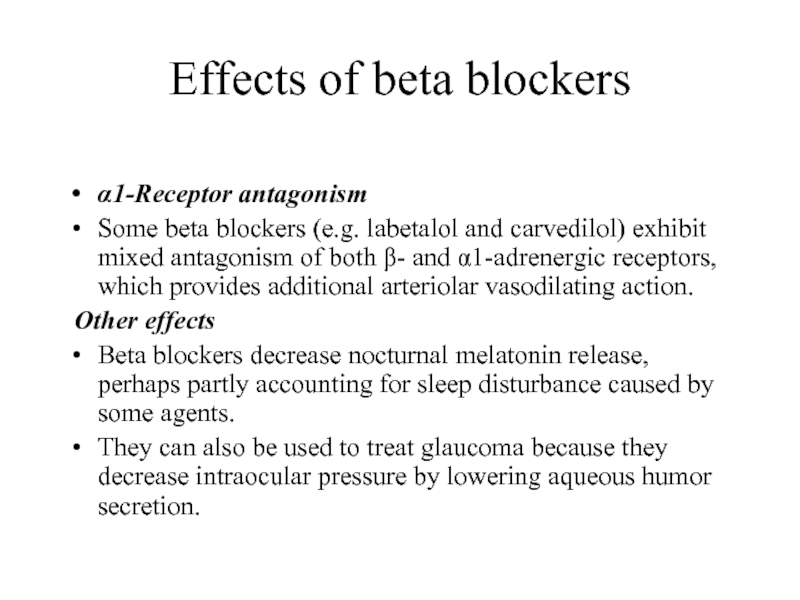
Слайд 13Effects of beta blockers
α1-Receptor antagonism
Some beta blockers (e.g. labetalol and carvedilol)
exhibit mixed antagonism of both β- and α1-adrenergic receptors, which provides additional arteriolar vasodilating action.
Other effects
Beta blockers decrease nocturnal melatonin release, perhaps partly accounting for sleep disturbance caused by some agents.
They can also be used to treat glaucoma because they decrease intraocular pressure by lowering aqueous humor secretion.
Other effects
Beta blockers decrease nocturnal melatonin release, perhaps partly accounting for sleep disturbance caused by some agents.
They can also be used to treat glaucoma because they decrease intraocular pressure by lowering aqueous humor secretion.
Слайд 14Non-selective agents
Alprenolol
Bucindolol
Carteolol
Carvedilol (has additional α-blocking activity)
Labetalol (has additional α-blocking
activity)
Nadolol
Penbutolol(has intrinsic sympathomimetic activity)
Pindolol (has intrinsic sympathomimetic activity)
Propranolol
Sotalol
Timolol
Eucommia bark (herb)
Nadolol
Penbutolol(has intrinsic sympathomimetic activity)
Pindolol (has intrinsic sympathomimetic activity)
Propranolol
Sotalol
Timolol
Eucommia bark (herb)
Слайд 15β1-Selective agents
Acebutolol (has intrinsic sympathomimetic activity)
Atenolol
Betaxolol
Bisoprolol
Celiprolol
Esmolol
Metoprolol
Nebivolol
Слайд 16β2-Selective agents
Butaxamine (weak α-adrenergic agonist activity) - No common clinical applications,
but used in experiments.
ICI-118,551 Highly selective β2-adrenergic receptor antagonist - No known clinical applications, but used in experiments due to its strong receptor specificity.
β3-Selective agents
SR 59230A (has additional α-blocking activity) - Used in experiments
ICI-118,551 Highly selective β2-adrenergic receptor antagonist - No known clinical applications, but used in experiments due to its strong receptor specificity.
β3-Selective agents
SR 59230A (has additional α-blocking activity) - Used in experiments
Слайд 17Indication differences
Agents specifically indicated for cardiac arrhythmia
Esmolol, sotalol, landiolol
Agents
specifically indicated for congestive heart failure
Bisoprolol, carvedilol, sustained-release metoprolol, nebivolol
Agents specifically indicated for glaucoma
Betaxolol, carteolol, levobunolol, metipranolol, timolol
Agents specifically indicated for myocardial infarction
Atenolol, metoprolol, propranolol
Agents specifically indicated for migraine prophylaxis
Timolol, propranolol
Propranolol is the only agent indicated for control of tremor, portal hypertension, and esophageal variceal bleeding, and used in conjunction with α-blocker therapy in phaeochromocytoma.
Bisoprolol, carvedilol, sustained-release metoprolol, nebivolol
Agents specifically indicated for glaucoma
Betaxolol, carteolol, levobunolol, metipranolol, timolol
Agents specifically indicated for myocardial infarction
Atenolol, metoprolol, propranolol
Agents specifically indicated for migraine prophylaxis
Timolol, propranolol
Propranolol is the only agent indicated for control of tremor, portal hypertension, and esophageal variceal bleeding, and used in conjunction with α-blocker therapy in phaeochromocytoma.
Слайд 28Use of beta-blockers in arrhythmia
Eur Heart J 2001;1852–923. Eur
Heart J 2003;24:1857–97.
Eur Heart J 2003;24:28–66. Eur Heart J 2001;22:1374–450.
Eur Heart J 2003;24:28–66. Eur Heart J 2001;22:1374–450.
Слайд 29Use of beta-blockers in prevention of sudden cardiac death
Eur Heart J
2003;24:28–66. Eur Heart J 2001;22:1374–450. Eur Heart J 2003;24:13–5.
Слайд 30Use of beta-blockers in hypertension
Eur. Heart J. 1998;19:1434–1503. Circulation
1999;100:1134–46. Circulation 2001;104:1577–9. J Hypertens 1999;17:151–8.