- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Nonrheumatic carditis in children презентация
Содержание
- 1. Nonrheumatic carditis in children
- 2. Plan of the lecture 1. Definition
- 3. Nonrheumatic carditis (NC) NC join all inflammatory
- 4. Epidemiology According to autopsy data morbidity in
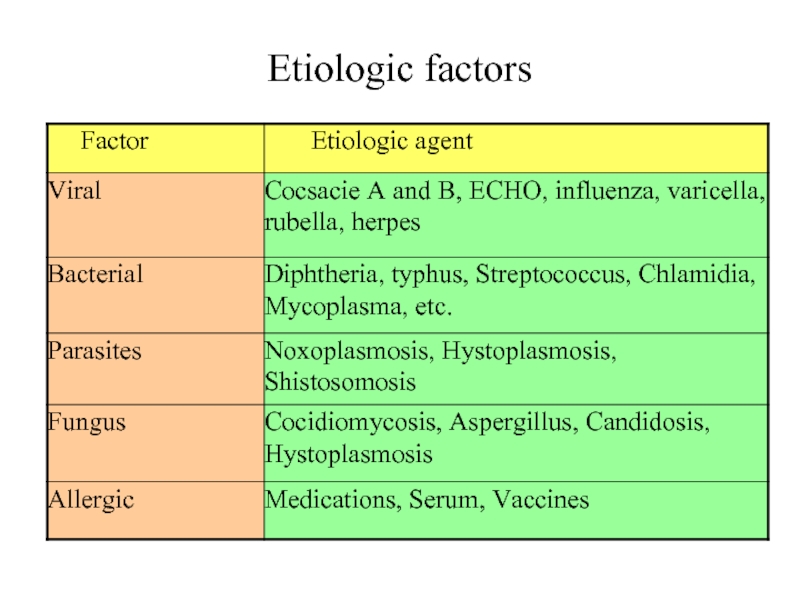
- 5. Etiologic factors
- 6. Predisposed factors Inherited myocardium hypersensitivity Inherited immune deficiency Vasculitis
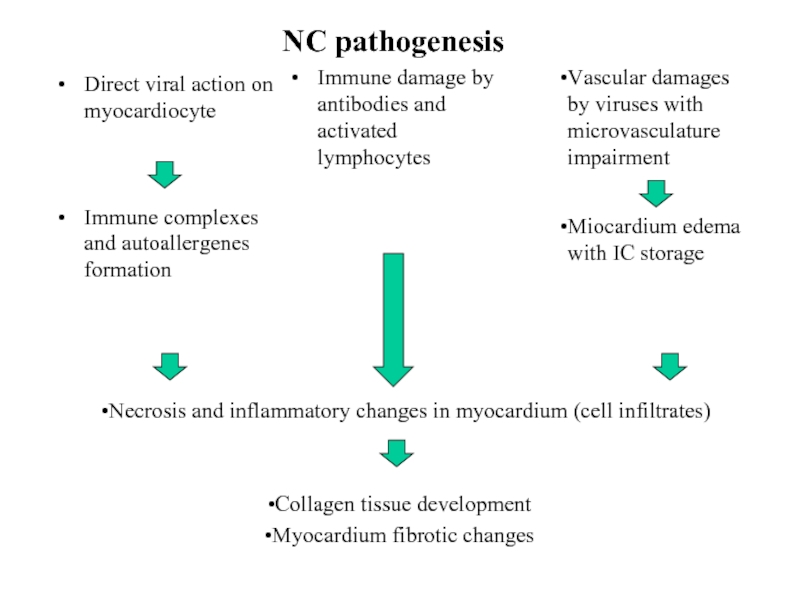
- 7. NC pathogenesis Direct viral action on myocardiocyte
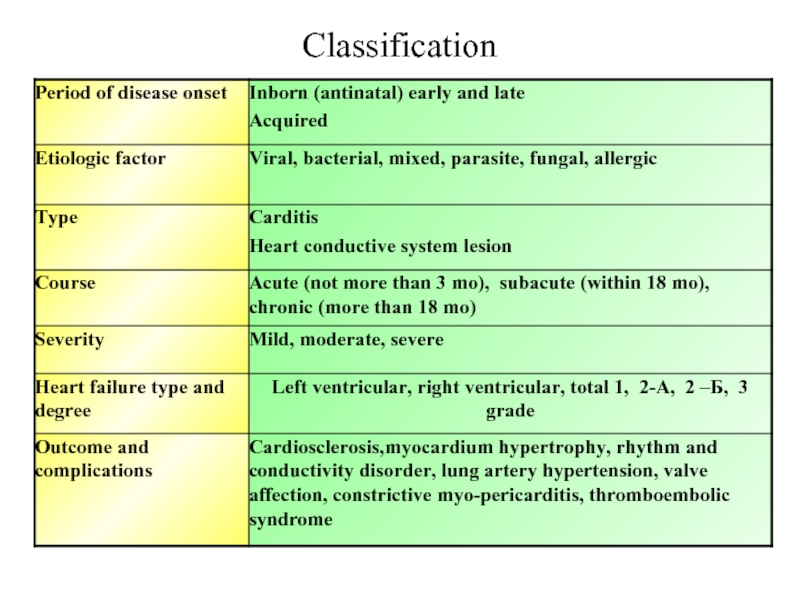
- 8. Classification
- 9. Inborn carditis ( are rare,especially isolated ones)
- 10. Clinical picture of early carditis Neonate usually
- 11. Clinical presentation of late carditis Manifest at
- 12. Objective data of inborn carditis Heart borders
- 13. Additional examining methods ECG: Sinus brady- or
- 14. Severity of carditis is dependent of 1.
- 15. Acquired myocarditis Prerequisite connection with acute
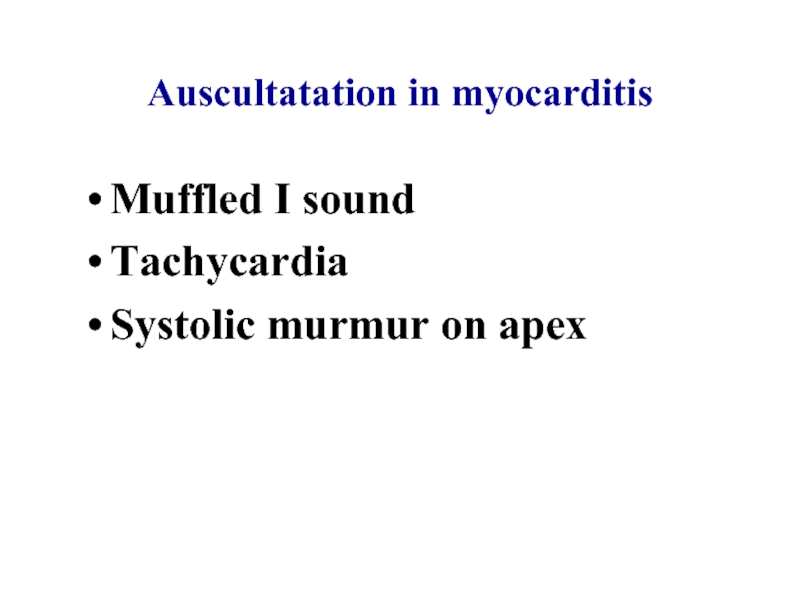
- 16. Auscultatation in myocarditis Muffled I sound Tachycardia Systolic murmur on apex
- 17. Diagnostic signs in carditis Radiology: dilation of
- 18. Treatment Strict bed regimen 8 weeks and
- 19. Medication treatment Etiologic
- 20. Medication treatment Glucocorticoids -in severe course when
- 21. Antibiotic treatment courses (in the case of
- 22. Treatment of heart failure Cardiotonic drugs: digoxin,
- 23. В-blockers: Bisoprolol: nitial dosage – 0,625 mg/day
- 24. Antiarrhythmic drugs: Amiadaron (cordaron) 10-15 mg/kg/day per
- 25. Cardiomyopathies (definition) Cardiomyopathy (CMP) is heterogeneous group
- 26. Cardiomyopathy Primary CMP-are diseases with isolated or
- 27. CMP classification 1. Ischemic CMP 2. Nonischemic
- 28. Hypertrophic CMP Is inherited disease characterized by
- 29. Hypertrophic CMP Obstructive with outflow pressure gradient
- 30. Clinical presentation Disease onset can be at
- 31. Dyspnea, chest pain, dizziness, syncope usually
- 32. Pathogenesis Ventricular septum hypertrophy so called disarray
- 33. Physical findings Appearance of patient is usual
- 34. Instrumental data ECG Chest X-ray examinig Cholter ECG monitoring Echo CG Chest scanning
- 35. ECG data Left ventricular hypertrophy signs Negative
- 36. Echo cardiography Ultrasound diagnostics is a gold
- 37. Treatment Body weight decreasing Exclude physical exertion
- 38. Dilative cardiomyopathy (DCMP) DCMP is primary myocardium
- 39. DCMP classification Primary or idiopathic family CMP
- 40. Clinical presentation Onset of disease has only
- 41. Physical examining signs Appearance: acrocyanosis, extremities edema,
- 42. Instrumental data Chest X-ray Heart dilation-cardithoracic index
- 43. Treatment Hospitalization first signs of
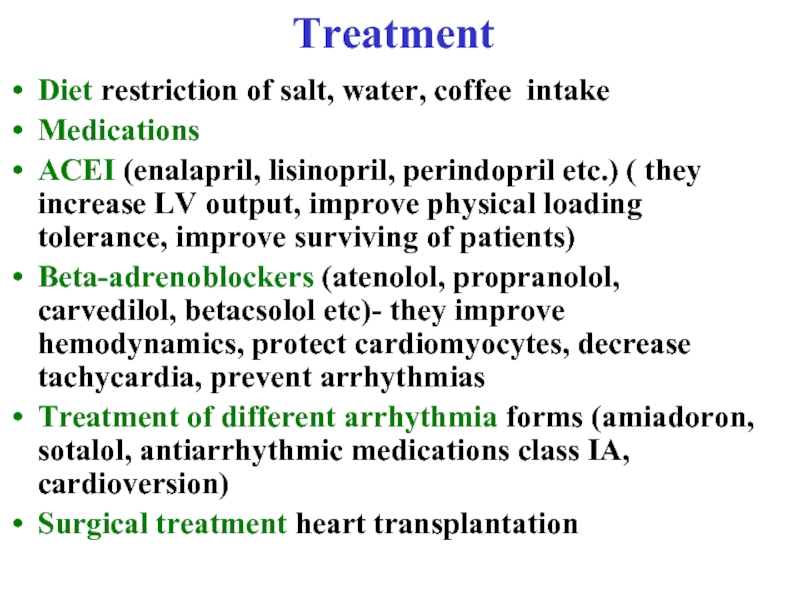
- 44. Treatment Diet restriction of salt, water, coffee
- 45. Questions Prevention of non rheumatic
Слайд 2Plan of the lecture
1. Definition of carditis
2. Etiologic factors
3.
4. Clinical presentation of carditis
5. Treatment
6. The differential diagnosis of cardiomyopathy
Слайд 3Nonrheumatic carditis (NC)
NC join all inflammatory myocardium diseases of different etiology
NC is polyetiologic disease
Слайд 4Epidemiology
According to autopsy data morbidity in children higher than in adults
Severe forms are more frequent in children especially in infants.
In children died from sudden death mortality due to NC is 17 %.
NC morbidity increased during viral disease epidemia.
Слайд 6Predisposed factors
Inherited myocardium hypersensitivity
Inherited immune deficiency
Vasculitis
Слайд 7NC pathogenesis
Direct viral action on myocardiocyte
Immune complexes and autoallergenes formation
Immune damage
Vascular damages by viruses with microvasculature impairment
Miocardium edema with IC storage
Necrosis and inflammatory changes in myocardium (cell infiltrates)
Collagen tissue development
Myocardium fibrotic changes
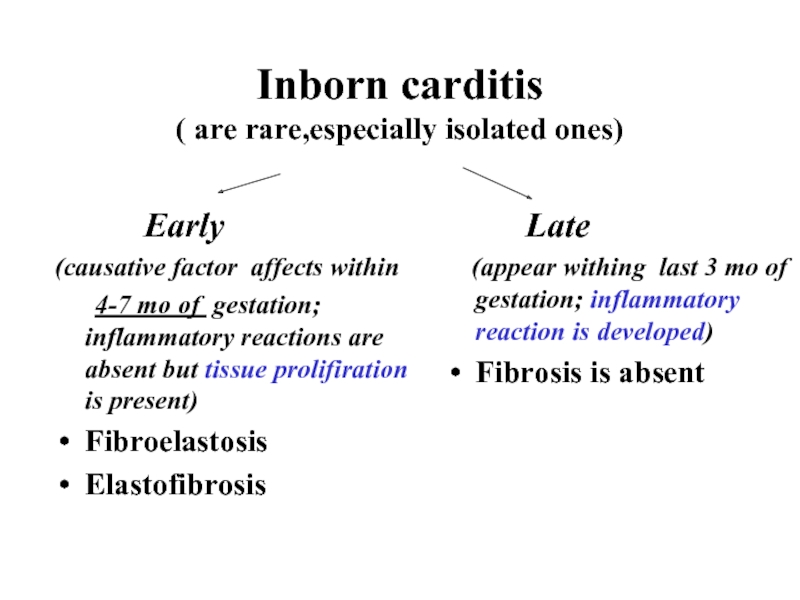
Слайд 9Inborn carditis
( are rare,especially isolated ones)
Early
(causative factor affects within
4-7 mo
Fibroelastosis
Elastofibrosis
Late
(appear withing last 3 mo of gestation; inflammatory reaction is developed)
Fibrosis is absent
Слайд 10Clinical picture of early carditis
Neonate usually has signs of carditis with
Main symptom is cardiomegaly and congestive heart disease, dyspnea, cough
Sometimes congestive heart disease manifest itself after viral diseases
Body weight gaining retardation, paleness, flaccidity, sweat, naso-labial cyanosis, weak suckling
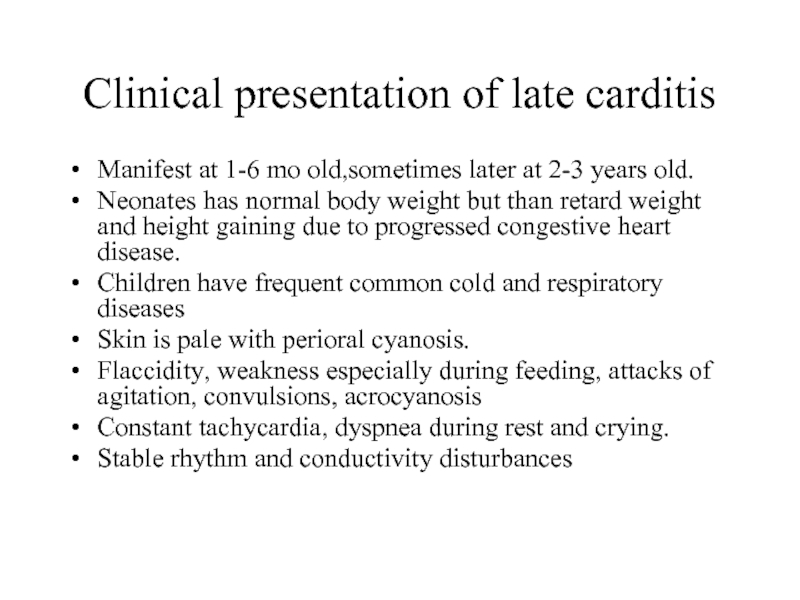
Слайд 11Clinical presentation of late carditis
Manifest at 1-6 mo old,sometimes later at
Neonates has normal body weight but than retard weight and height gaining due to progressed congestive heart disease.
Children have frequent common cold and respiratory diseases
Skin is pale with perioral cyanosis.
Flaccidity, weakness especially during feeding, attacks of agitation, convulsions, acrocyanosis
Constant tachycardia, dyspnea during rest and crying.
Stable rhythm and conductivity disturbances
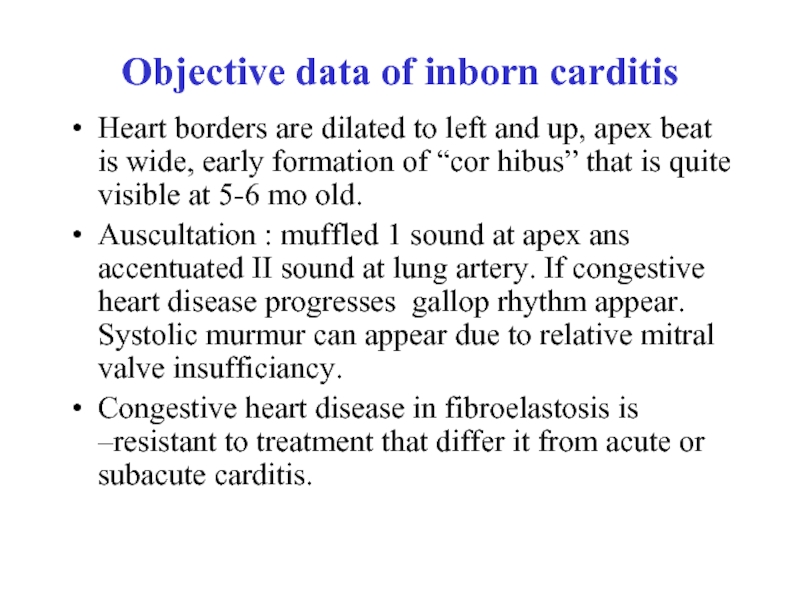
Слайд 12Objective data of inborn carditis
Heart borders are dilated to left and
Auscultation : muffled 1 sound at apex ans accentuated II sound at lung artery. If congestive heart disease progresses gallop rhythm appear. Systolic murmur can appear due to relative mitral valve insufficiancy.
Congestive heart disease in fibroelastosis is –resistant to treatment that differ it from acute or subacute carditis.
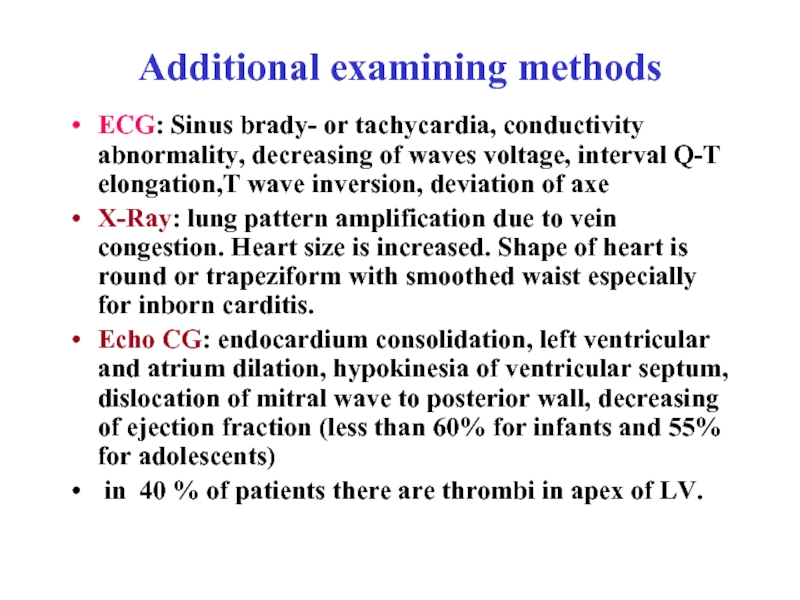
Слайд 13Additional examining methods
ECG: Sinus brady- or tachycardia, conductivity abnormality, decreasing of
X-Ray: lung pattern amplification due to vein congestion. Heart size is increased. Shape of heart is round or trapeziform with smoothed waist especially for inborn carditis.
Echo CG: endocardium consolidation, left ventricular and atrium dilation, hypokinesia of ventricular septum, dislocation of mitral wave to posterior wall, decreasing of ejection fraction (less than 60% for infants and 55% for adolescents)
in 40 % of patients there are thrombi in apex of LV.
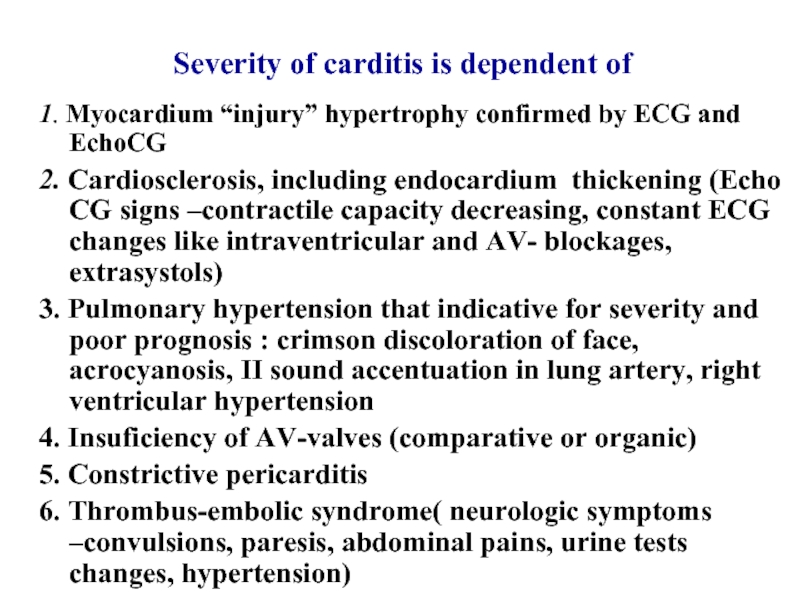
Слайд 14Severity of carditis is dependent of
1. Myocardium “injury” hypertrophy confirmed by
2. Cardiosclerosis, including endocardium thickening (Echo CG signs –contractile capacity decreasing, constant ECG changes like intraventricular and AV- blockages, extrasystols)
3. Pulmonary hypertension that indicative for severity and poor prognosis : crimson discoloration of face, acrocyanosis, II sound accentuation in lung artery, right ventricular hypertension
4. Insuficiency of AV-valves (comparative or organic)
5. Constrictive pericarditis
6. Thrombus-embolic syndrome( neurologic symptoms –convulsions, paresis, abdominal pains, urine tests changes, hypertension)
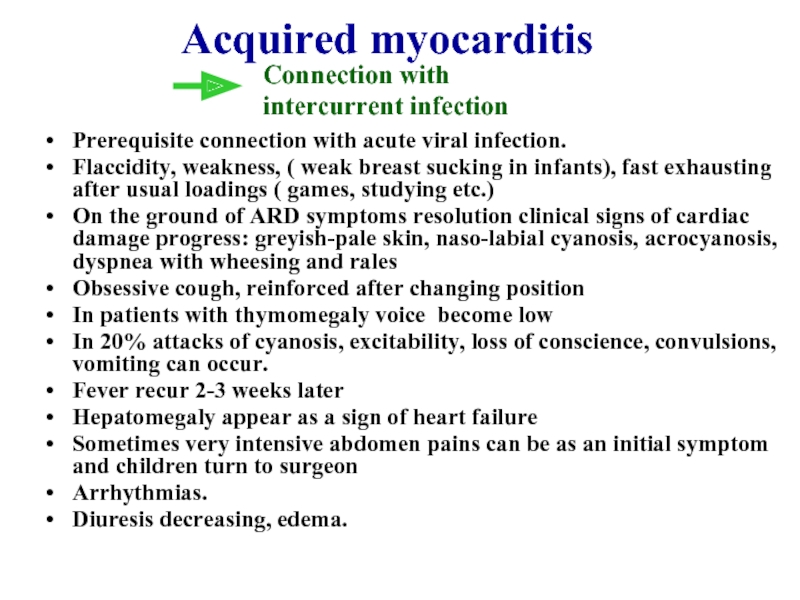
Слайд 15Acquired myocarditis
Prerequisite connection with acute viral infection.
Flaccidity, weakness, ( weak breast
On the ground of ARD symptoms resolution clinical signs of cardiac damage progress: greyish-pale skin, naso-labial cyanosis, acrocyanosis, dyspnea with wheesing and rales
Obsessive cough, reinforced after changing position
In patients with thymomegaly voice become low
In 20% attacks of cyanosis, excitability, loss of conscience, convulsions, vomiting can occur.
Fever recur 2-3 weeks later
Hepatomegaly appear as a sign of heart failure
Sometimes very intensive abdomen pains can be as an initial symptom and children turn to surgeon
Arrhythmias.
Diuresis decreasing, edema.
Connection with
intercurrent infection
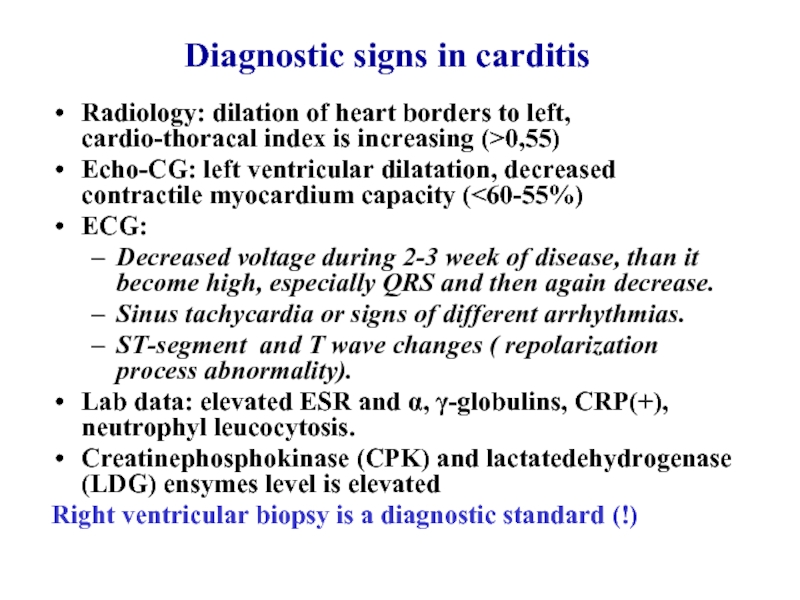
Слайд 17Diagnostic signs in carditis
Radiology: dilation of heart borders to left, cardio-thoracal
Echo-CG: left ventricular dilatation, decreased contractile myocardium capacity (<60-55%)
ECG:
Decreased voltage during 2-3 week of disease, than it become high, especially QRS and then again decrease.
Sinus tachycardia or signs of different arrhythmias.
ST-segment and T wave changes ( repolarization process abnormality).
Lab data: elevated ESR and α, γ-globulins, CRP(+), neutrophyl leucocytosis.
Creatinephosphokinase (CPK) and lactatedehydrogenase (LDG) ensymes level is elevated
Right ventricular biopsy is a diagnostic standard (!)
Слайд 18Treatment
Strict bed regimen 8 weeks and more according to functional capacity
Diet № 10. Restriction of water intake, diet is enriched by potassium containing products: raisin, dried apricots, nuts, dried plums etc. Medication corrector of Mg and K drugs are asparcam, magnerot, panangin
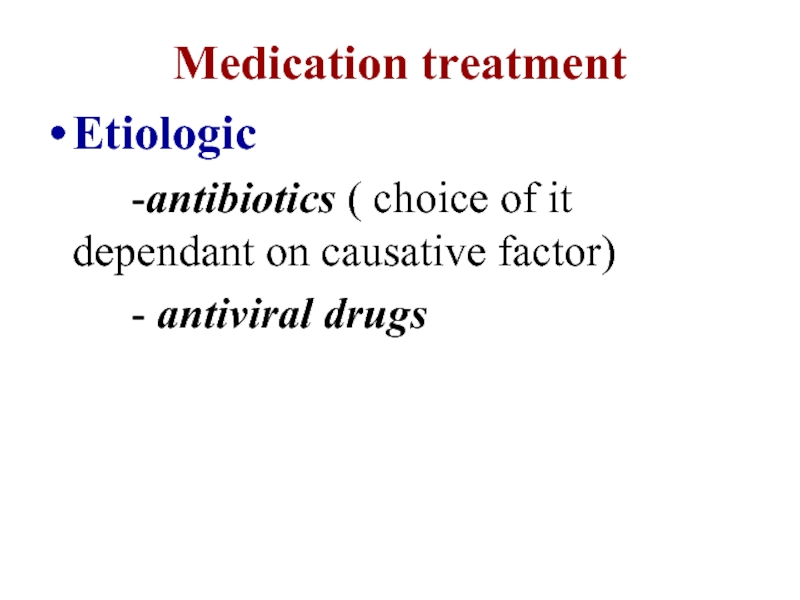
Слайд 19Medication treatment
Etiologic
-antibiotics ( choice of it dependant
- antiviral drugs
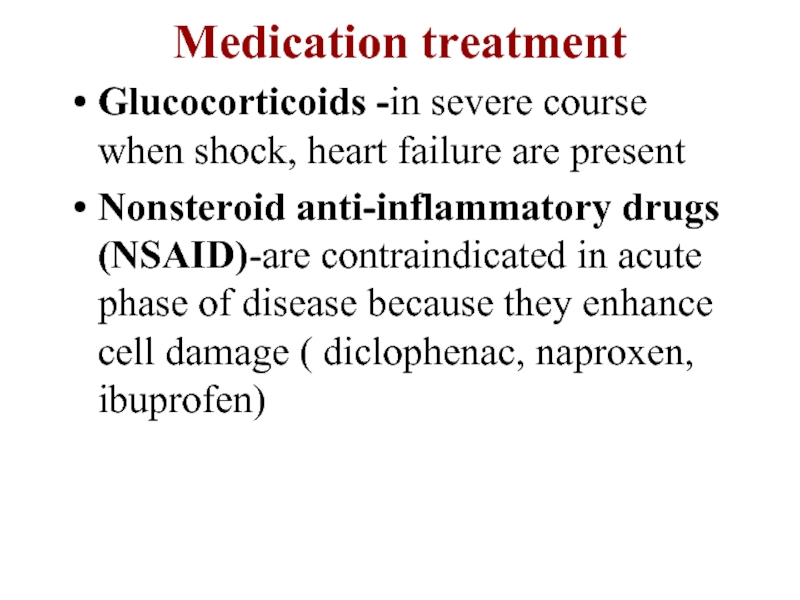
Слайд 20Medication treatment
Glucocorticoids -in severe course when shock, heart failure are present
Nonsteroid
Слайд 21Antibiotic treatment courses (in the case of intercurrent infection, surgery, exacerbation
Semisynthetic penicyllines: Augmentin, Amoxycilline 10-14 days long.
Macrolides:
Roxytromycine – 7,5mg/ kg BID;
Azythromycine – 10 mg/kg once per day;
If suspicion of infective endocarditis under suspicion parenterally: Ampicilline 100-150 mg/kg, Amicacine 2 mg/kg, Vancomicine 10-15 mg/kg
Treatment duration is dependent on etiology: Streptococcal -4 weeks, Staphylococcus – 6 weeks, Gr”-” bacteria – 4 weeks
Glucocorticoids in severe course (shock, allergy), congestive heart disease, rhythm abnormalities: Prednisolon 0,8-1,5 mg/kg/day. In viral etiology in acute phase of AVD are contraindicated as they can enhance damage of cardiomyocytes.
Nonsteroid drugs in subacute and acute course of moderate severity
In chronic and subacute courses – aminochinoline drugs minimum for 6 mo long.
Antiviral therapy – IV immuneglobulins in high dosages..
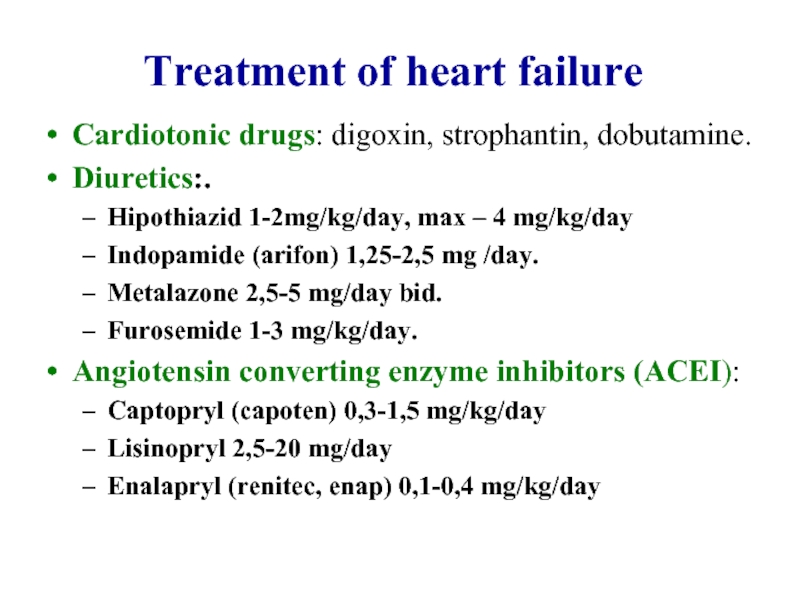
Слайд 22Treatment of heart failure
Cardiotonic drugs: digoxin, strophantin, dobutamine.
Diuretics:.
Hipothiazid 1-2mg/kg/day, max –
Indopamide (arifon) 1,25-2,5 mg /day.
Metalazone 2,5-5 mg/day bid.
Furosemide 1-3 mg/kg/day.
Angiotensin converting enzyme inhibitors (ACEI):
Captopryl (capoten) 0,3-1,5 mg/kg/day
Lisinopryl 2,5-20 mg/day
Enalapryl (renitec, enap) 0,1-0,4 mg/kg/day
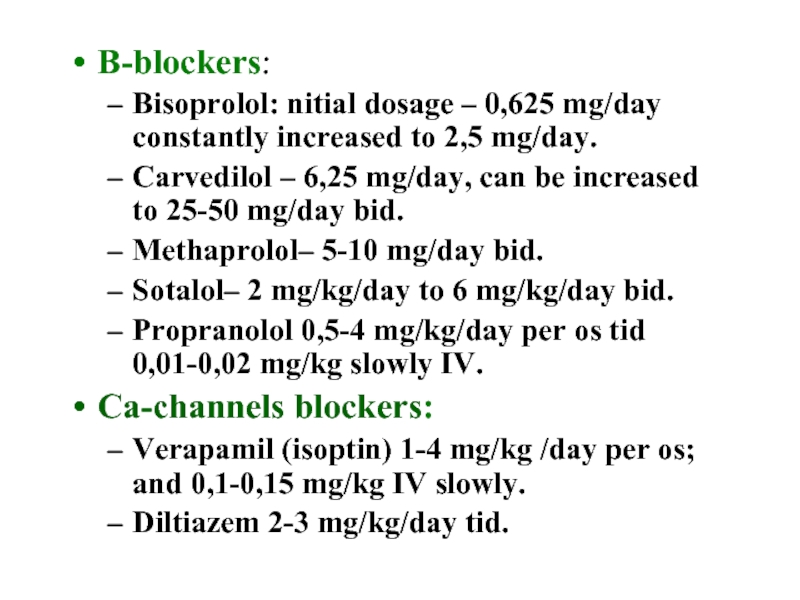
Слайд 23В-blockers:
Bisoprolol: nitial dosage – 0,625 mg/day constantly increased to 2,5 mg/day.
Carvedilol
Methaprolol– 5-10 mg/day bid.
Sotalol– 2 mg/kg/day to 6 mg/kg/day bid.
Propranolol 0,5-4 mg/kg/day per os tid 0,01-0,02 mg/kg slowly IV.
Ca-channels blockers:
Verapamil (isoptin) 1-4 mg/kg /day per os; and 0,1-0,15 mg/kg IV slowly.
Diltiazem 2-3 mg/kg/day tid.
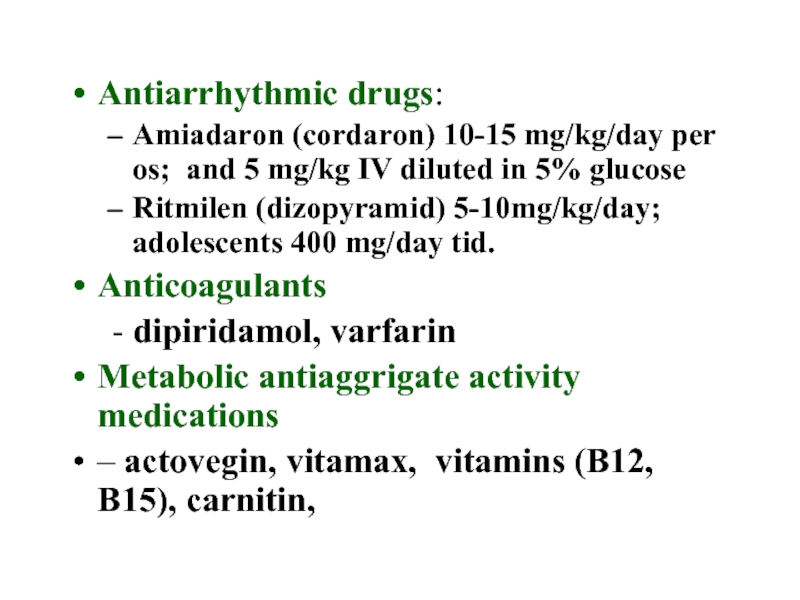
Слайд 24Antiarrhythmic drugs:
Amiadaron (cordaron) 10-15 mg/kg/day per os; and 5 mg/kg IV
Ritmilen (dizopyramid) 5-10mg/kg/day; adolescents 400 mg/day tid.
Anticoagulants
- dipiridamol, varfarin
Metabolic antiaggrigate activity medications
– actovegin, vitamax, vitamins (В12, В15), carnitin,
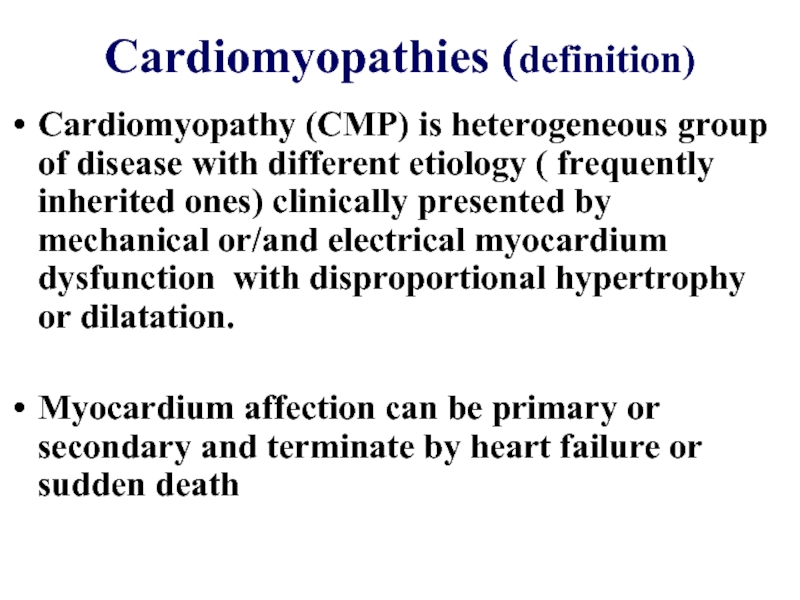
Слайд 25Cardiomyopathies (definition)
Cardiomyopathy (CMP) is heterogeneous group of disease with different etiology
Myocardium affection can be primary or secondary and terminate by heart failure or sudden death
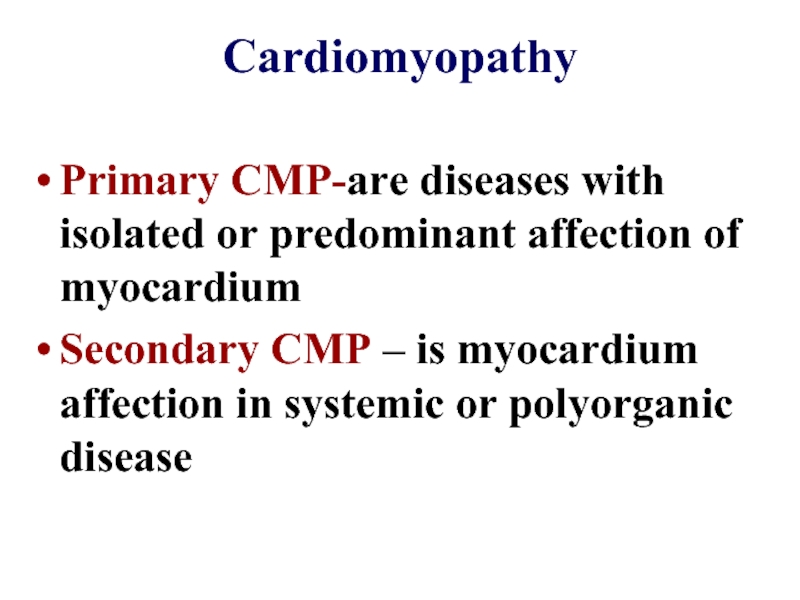
Слайд 26Cardiomyopathy
Primary CMP-are diseases with isolated or predominant affection of myocardium
Secondary CMP
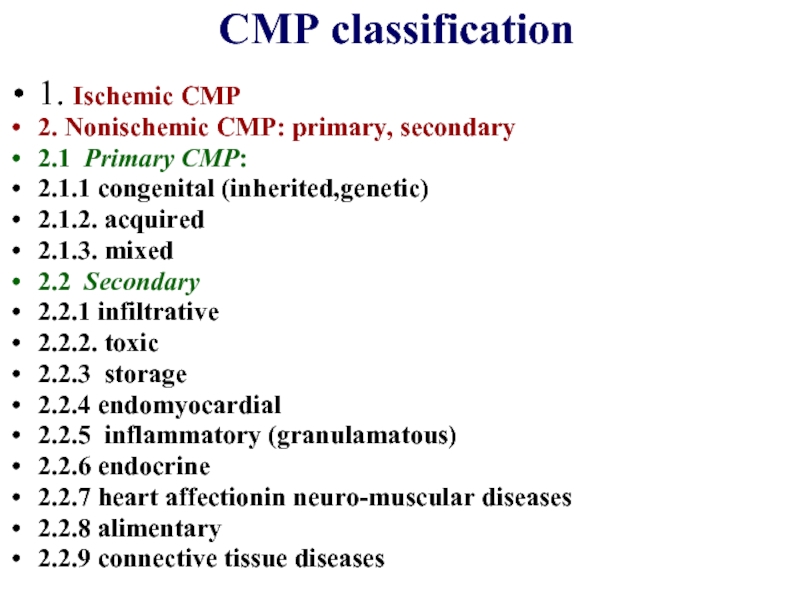
Слайд 27CMP classification
1. Ischemic CMP
2. Nonischemic CMP: primary, secondary
2.1 Primary CMP:
2.1.1 congenital
2.1.2. acquired
2.1.3. mixed
2.2 Secondary
2.2.1 infiltrative
2.2.2. toxic
2.2.3 storage
2.2.4 endomyocardial
2.2.5 inflammatory (granulamatous)
2.2.6 endocrine
2.2.7 heart affectionin neuro-muscular diseases
2.2.8 alimentary
2.2.9 connective tissue diseases
Слайд 28Hypertrophic CMP
Is inherited disease characterized by asymmetric left ventricular hypertrophy with
Слайд 29Hypertrophic CMP
Obstructive with outflow pressure gradient >30 mm Hg
Nonobstructive outflow pressure
Latent outflow pressure gradient raises more than 30 mm Hg only after loading test
Слайд 30Clinical presentation
Disease onset can be at any age.
Disease can progress in
High risk rate of sudden death
Disease progression with dyspnoe, chest pains and syncope
Congestive heart disease with LV remodelling
Atrium flutter with thromboembolia
Слайд 31
Dyspnea, chest pain, dizziness, syncope usually are due to diastolic dysfunction.
Chest pain like in stenocardia as a rule develops due to outflow obstruction and decreasing of coronary circulation. Syncope as a rule appear suddenly after emotional or physical strain due to decreased outflow. Later syncope can appear at rest
Disease can manifest by arrhythmias ( atrium, ventricular fluttering or fibrillation). Every arrhythmia episode can be fatal for patient
Слайд 32Pathogenesis
Ventricular septum hypertrophy so called disarray phenomenon of cell structure lead
Outflow obstruction develops due to disproportional ventricular septum hypertrophy predispose to leaflets contact with septum and produce increased gradient during systole.
Prolonged hypertrophy predispose for disorder of myocardium relaxation and development of ventricular walls rigidity. Diastolic dysfunction develops and later lead to systolyc heart dysfunction.
Слайд 33Physical findings
Appearance of patient is usual
Palpation: apex beat is wide and
Auscultation- systolic murmur at apex and in 4 left intercostal space near sternum. Murmur is very variable. It can be louder during physical exertion, in vertical position, during tachycardia or after nitrate or diuretic intake
Слайд 35ECG data
Left ventricular hypertrophy signs
Negative T-waves in chest leads
Atypical deep Q-wave
Arrythmia and conductivity disorders ( atrium fibrillation, different blockages
Cholter monitoring is helpful to reveal threatening to life signs like unstable ventricular tachycardia, atrium fibrillation, signs of myocardium ischemia
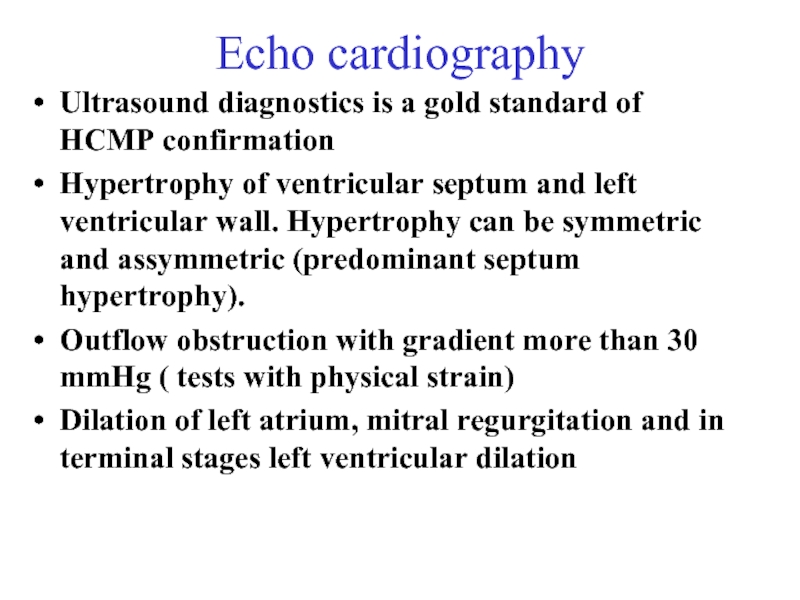
Слайд 36Echo cardiography
Ultrasound diagnostics is a gold standard of HCMP confirmation
Hypertrophy of
Outflow obstruction with gradient more than 30 mmHg ( tests with physical strain)
Dilation of left atrium, mitral regurgitation and in terminal stages left ventricular dilation
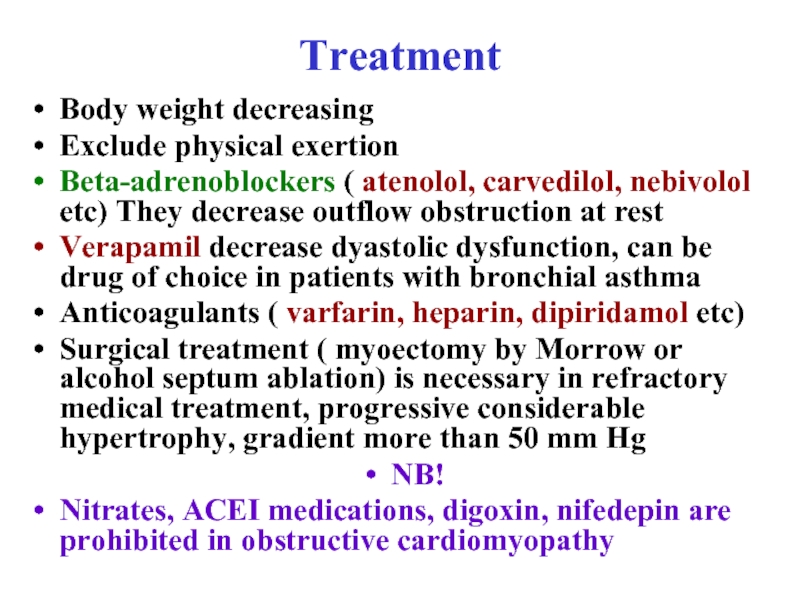
Слайд 37Treatment
Body weight decreasing
Exclude physical exertion
Beta-adrenoblockers ( atenolol, carvedilol, nebivolol etc) They
Verapamil decrease dyastolic dysfunction, can be drug of choice in patients with bronchial asthma
Anticoagulants ( varfarin, heparin, dipiridamol etc)
Surgical treatment ( myoectomy by Morrow or alcohol septum ablation) is necessary in refractory medical treatment, progressive considerable hypertrophy, gradient more than 50 mm Hg
NB!
Nitrates, ACEI medications, digoxin, nifedepin are prohibited in obstructive cardiomyopathy
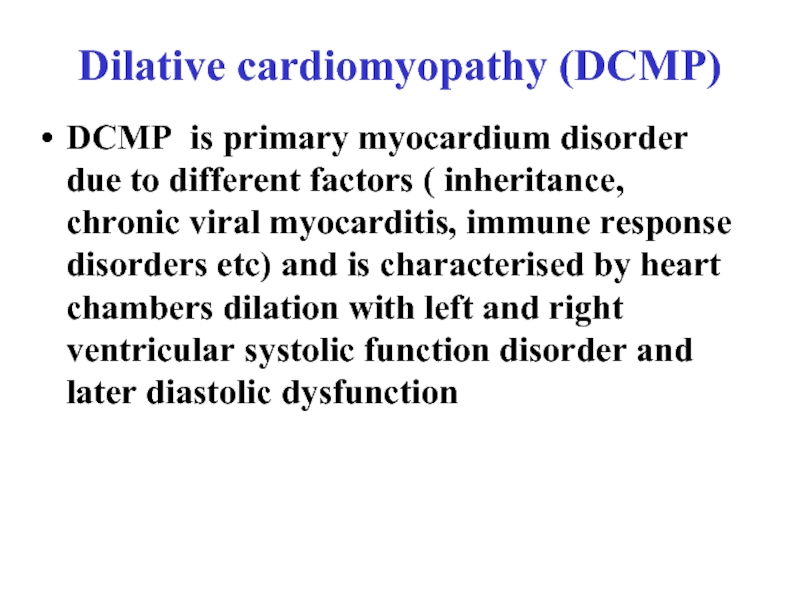
Слайд 38Dilative cardiomyopathy (DCMP)
DCMP is primary myocardium disorder due to different factors
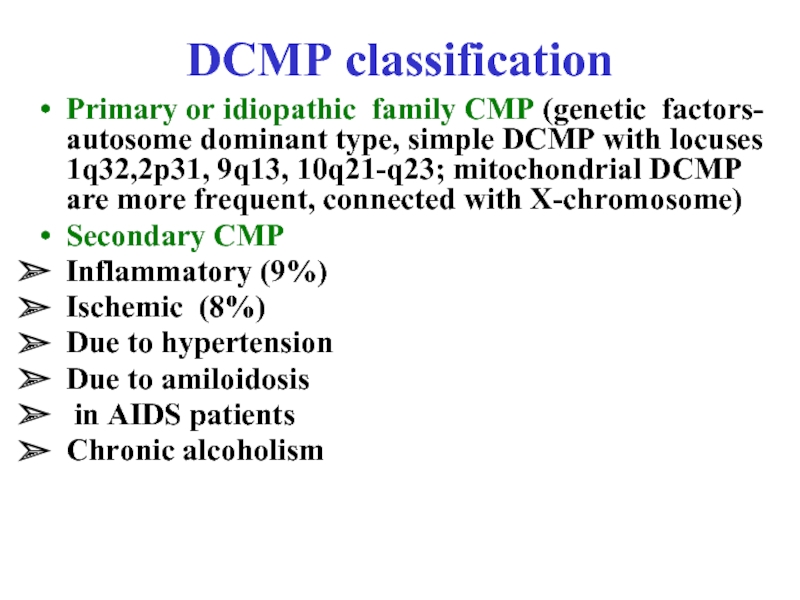
Слайд 39DCMP classification
Primary or idiopathic family CMP (genetic factors- autosome dominant type,
Secondary CMP
Inflammatory (9%)
Ischemic (8%)
Due to hypertension
Due to amiloidosis
in AIDS patients
Chronic alcoholism
Слайд 40Clinical presentation
Onset of disease has only few symptoms of congestive heart
Dyspnea, asthmatic attacks
Fatigability, muscle weakness
Ventricular arrhythmia accompanied by syncope
Atrium fibrillation, thromboembolia, systolic heart dysfunction
Right ventricular failure signs: edema of legs, hepatomegaly, ascitis
Слайд 41Physical examining signs
Appearance: acrocyanosis, extremities edema, orthopnoe position, neck veins swelling
Auscultation:
Chest palpation: enhanced, wide dislocated to left and down apex beat
Percussion: heart borders are dislocated to left and right side
Слайд 42Instrumental data
Chest X-ray Heart dilation-cardithoracic index is more than 0,5, congestion
ECG –nonspecific changes of ST segment and T-wave, voltage decrease, QRS deformation, sinus tachycardia, rhythm and conductivity disorders
Echo- CG: dilation of chambers, systolic dysfunction decreasing of LV output less than 55%, relative mitral and tricuspid regurgitation
Endomyocardial biopsy in suspicion of inflammatory CMP to evaluate myocardiocytes distruction and inflammatory cells infiltration
Слайд 43Treatment
Hospitalization
first signs of congestive heart disease to specify its
in cases of life threatening arrhythmias;
progressive congestive heart disease:
in acute conditions like heart asthma, lung edema;
complications like pneumonia, systemic embolia, arrhythmia, syncope
Слайд 44Treatment
Diet restriction of salt, water, coffee intake
Medications
ACEI (enalapril, lisinopril, perindopril etc.)
Beta-adrenoblockers (atenolol, propranolol, carvedilol, betacsolol etc)- they improve hemodynamics, protect cardiomyocytes, decrease tachycardia, prevent arrhythmias
Treatment of different arrhythmia forms (amiadoron, sotalol, antiarrhythmic medications class IA, cardioversion)
Surgical treatment heart transplantation
Слайд 45
Questions
Prevention of non rheumatic carditis
Frequency and prognosis
Common clinical symptoms of myocarditis
Characteristic
Additional (instrumental) methods of invastigations
Medical check-up
Prevention of complications of NC.
Classification of heart failure
Principles of treatment of heart failure