- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Modes of ventilation презентация
Содержание
- 1. Modes of ventilation
- 2. Modes of Ventilation The main indication for ventilatory support is Respiratory Failure
- 3. Categories of Respiratory Failure HYPOXEMIC
- 4. HYPERCARBIC OBSTRUCTION TO
- 5. ECE CENTRAL
- 6. A MECHANICAL VENTILATOR is a pump providing
- 7. NO = Nitric Oxide
- 8. GENERAL CLASSES OF VENTILATORS Negative pressure
- 9. Negative Pressure Ventilators - Perithoracic pump for
- 10. Negative Pressure Ventilators 1876 1930-1950 1960
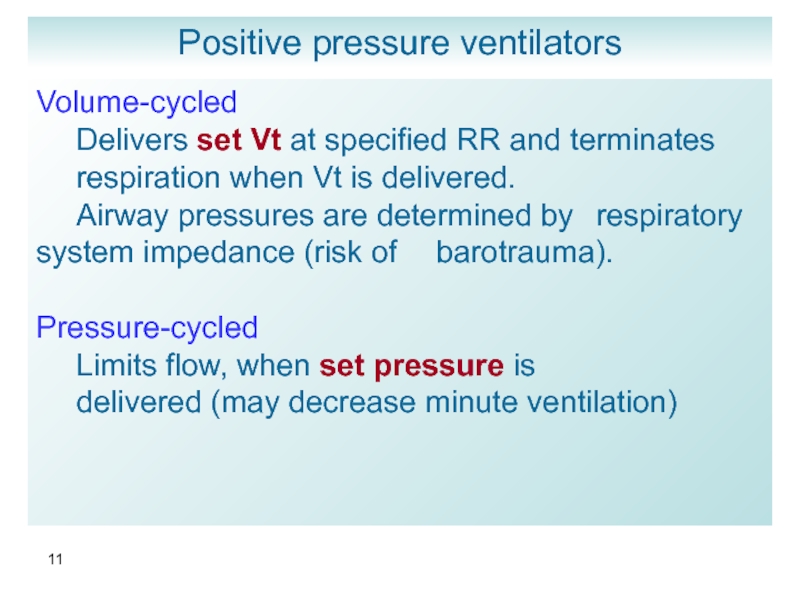
- 11. Positive pressure ventilators Volume-cycled Delivers
- 12. Positive pressure ventilators Evita 2 Dragger - Germany
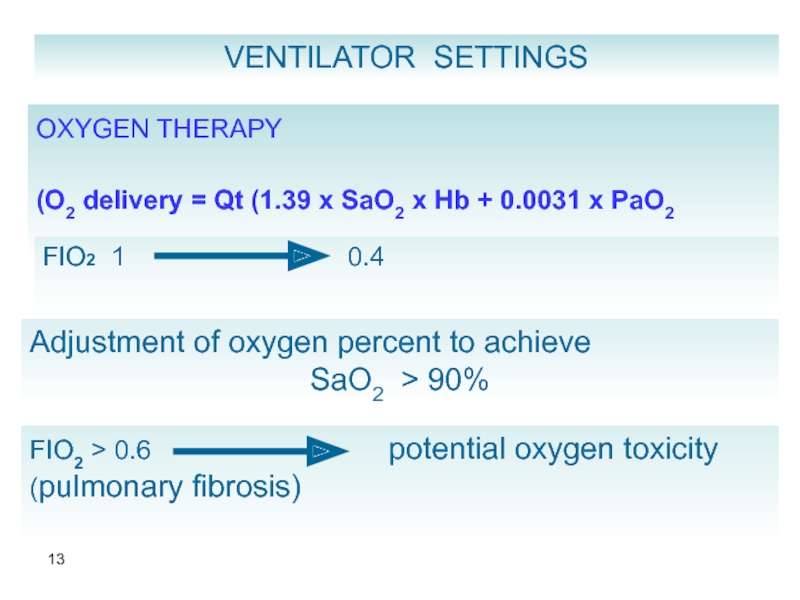
- 13. VENTILATOR SETTINGS OXYGEN THERAPY
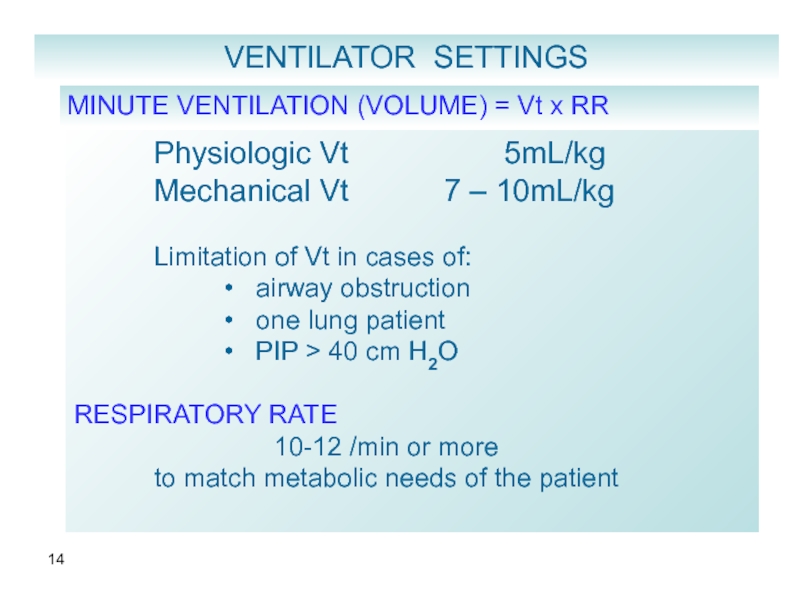
- 14. MINUTE VENTILATION (VOLUME) = Vt x RR
- 15. Inspiratory Flow Rate
- 16. CMV : Controlled Mandatory Ventilation Full mechanical
- 17. CMV fixed rate fixed
- 18. ASSIST / CONTROL ⮞ Mechanical breath initiated
- 19. IMV INTERMITTENT MANDATORY VENTILATION
- 20. SIMV SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION ⮞
- 22. IMV / SIMV Advantages
- 23. IMV / SIMV Disadvantages
- 24. PEEP and CPAP During continuous mechanical
- 25. PEEP and CPAP During spontaneous breathing
- 27. Goals
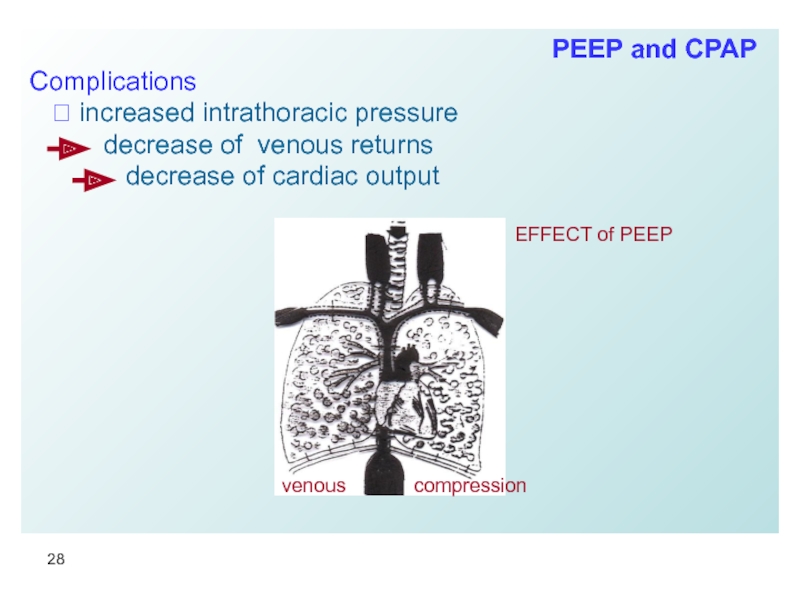
- 28. Complications ⮞ increased
- 29. Complications
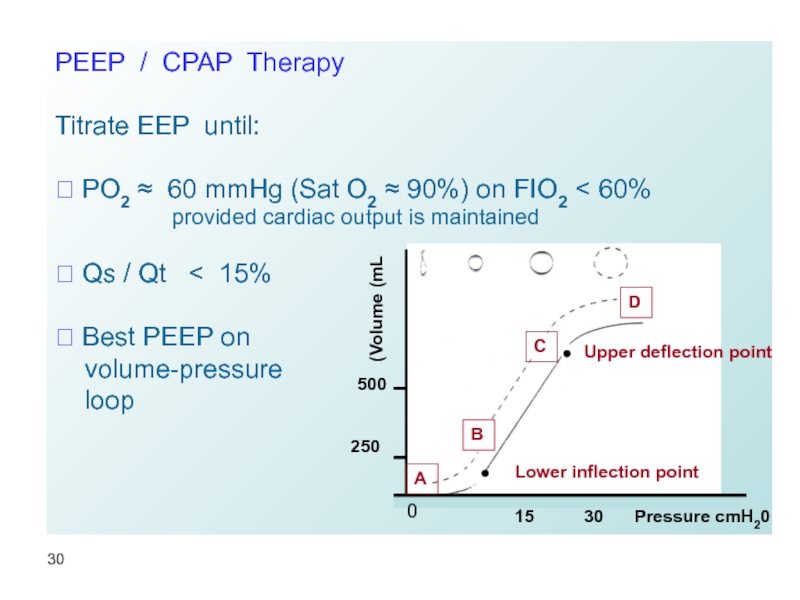
- 30. PEEP / CPAP Therapy Titrate EEP
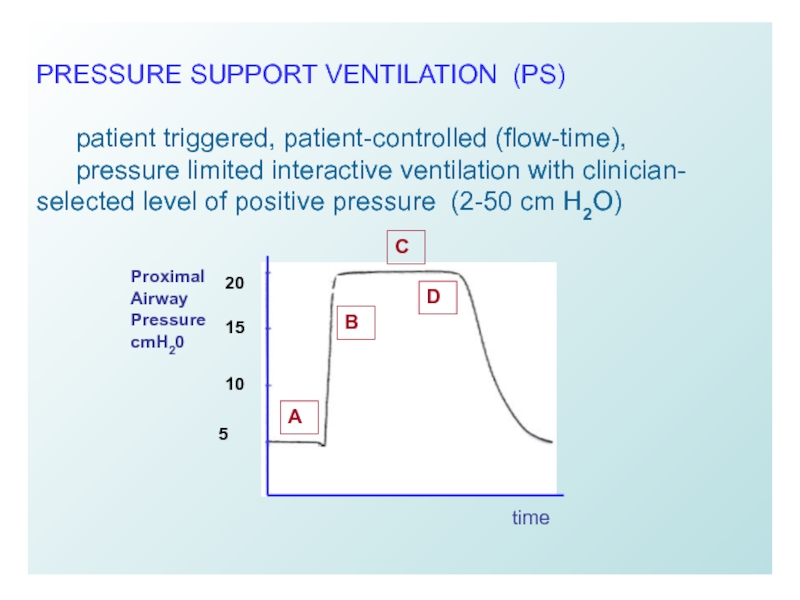
- 31. PRESSURE SUPPORT VENTILATION (PS) patient
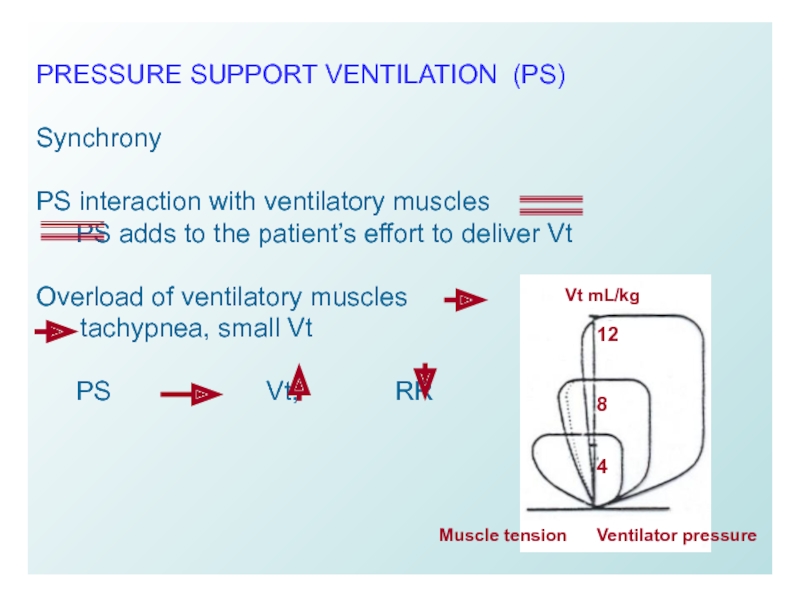
- 32. PRESSURE SUPPORT VENTILATION (PS) Synchrony
- 33. PRESSURE SUPPORT VENTILATION (PS)
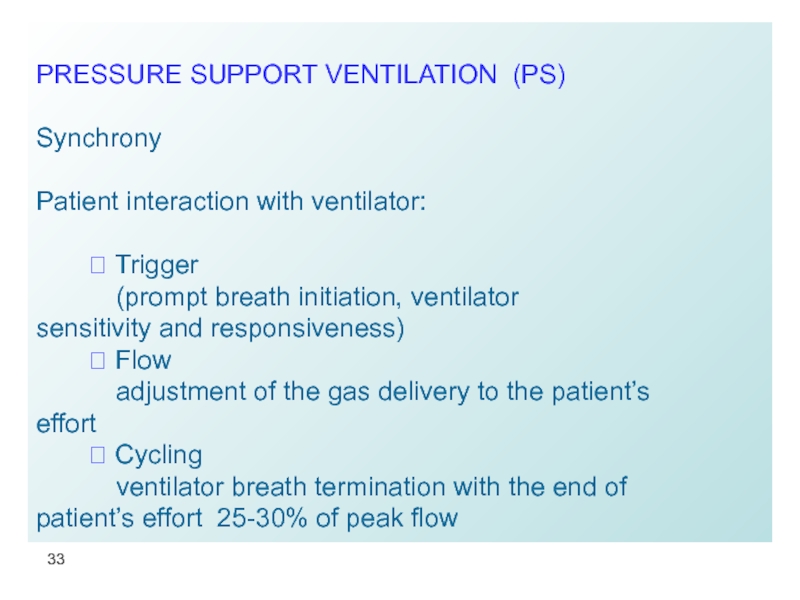
- 34. PRESSURE SUPPORT VENTILATION (PS) Titration
- 35. PRESSURE CONTROL VENTILATION Time and
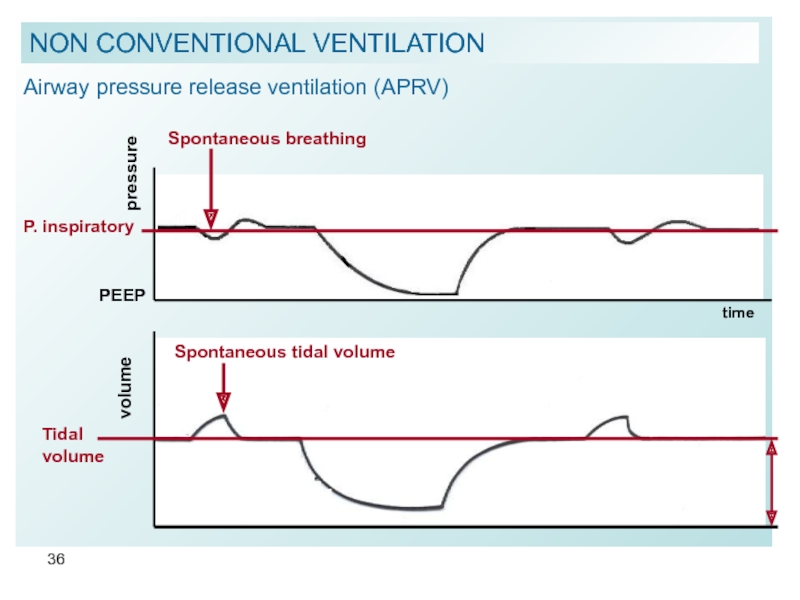
- 36. Airway pressure release ventilation (APRV)
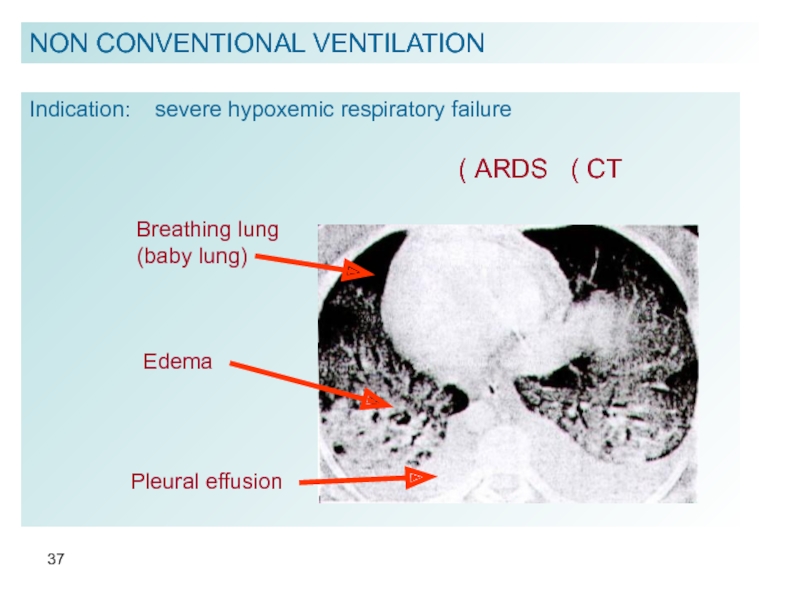
- 37. NON CONVENTIONAL VENTILATION Indication: severe hypoxemic
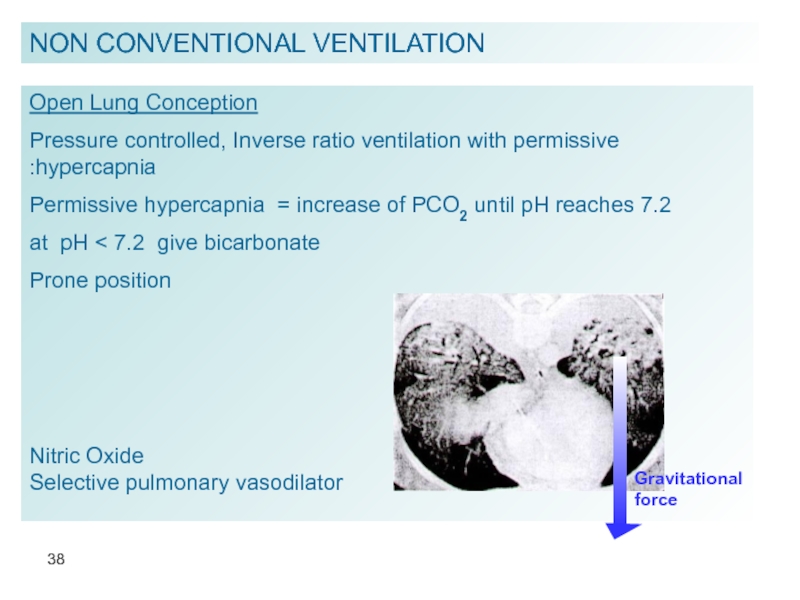
- 38. NON CONVENTIONAL VENTILATION Open Lung Conception Pressure
- 39. NON CONVENTIONAL VENTILATION Proportional assist ventilation for
- 40. HIGH FREQUENCY VENTILATION RR
- 41. VEANING FROM MECHANICAL VENTILATION Necessary conditions
- 42. VEANING FROM MECHANICAL VENTILATION
Слайд 3Categories of Respiratory Failure
HYPOXEMIC
ARDS
PULMONARY EDEMA
PULMONARY HEMORRHAGE
PNEUMONIA
Low compliance lung disease:
Low PO2,
Слайд 4
HYPERCARBIC
OBSTRUCTION TO AIRFLOW
NEUROMUSCULAR DISORDERS
DRUG
ENDOCRINOPATHIES
Increase in PCO2
Respiratory acidosis
Decrease in pH
Categories of Respiratory Failure
Слайд 5ECE
CENTRAL
DECREASED LEVEL OF
CONSCIOUSNESS
ACUTE MEDICAL AND SURGICAL
CONDITIONS
MECHANICAL VENTILATION IS USED TO
DECREASE WORK OF BREATHING
Categories of Respiratory Failure
Слайд 6A MECHANICAL VENTILATOR is
a pump providing an external source of energy
Ventilator’s Changeable parameters
Vt = Tidal Volume
FIO2 = Fraction of Inspired Oxygen
RR = Respiratory Rate
I:E = Inspiratory to Expiratory ratio
EEP = End Expiratory Pressure
PIP = Peak Inspiratory Pressure Inspiratory Flow Rate
Слайд 7
NO = Nitric Oxide
Orientation of patient’s body in gravitational
OTHER MEANS AFFECTING VENTILATION
Слайд 8GENERAL CLASSES OF VENTILATORS
Negative pressure
application of negative pressure at the
Positive pressure
application of positive pressure at airway opening
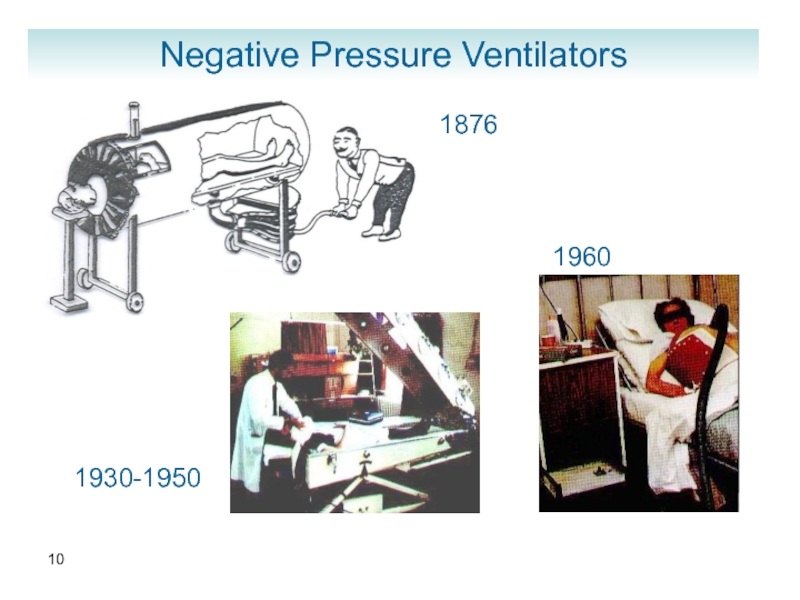
Слайд 9Negative Pressure Ventilators
-
Perithoracic pump for replacement failing patients’ muscles, wide-spread use
Manually operated ventilator (Woillez, 1876)
Tank respirator “iron lung”, cuirass, body suits
(1930 - 1950)
Patient care problems:
airway obstruction, low efficacy in interstitial lung diseases, patient’s discomfort
Слайд 11Positive pressure ventilators
Volume-cycled
Delivers set Vt at specified RR and
respiration when Vt is delivered.
Airway pressures are determined by respiratory system impedance (risk of barotrauma).
Pressure-cycled
Limits flow, when set pressure is
delivered (may decrease minute ventilation)
Слайд 13VENTILATOR SETTINGS
OXYGEN THERAPY
O2 delivery = Qt
FIO2 1 0.4
Adjustment of oxygen percent to achieve
SaO2 > 90%
FIO2 > 0.6 potential oxygen toxicity
(pulmonary fibrosis)
Слайд 14MINUTE VENTILATION (VOLUME) = Vt x RR
Physiologic Vt
Mechanical Vt 7 – 10mL/kg
Limitation of Vt in cases of:
airway obstruction
one lung patient
PIP > 40 cm H2O
RESPIRATORY RATE
10-12 /min or more
to match metabolic needs of the patient
VENTILATOR SETTINGS
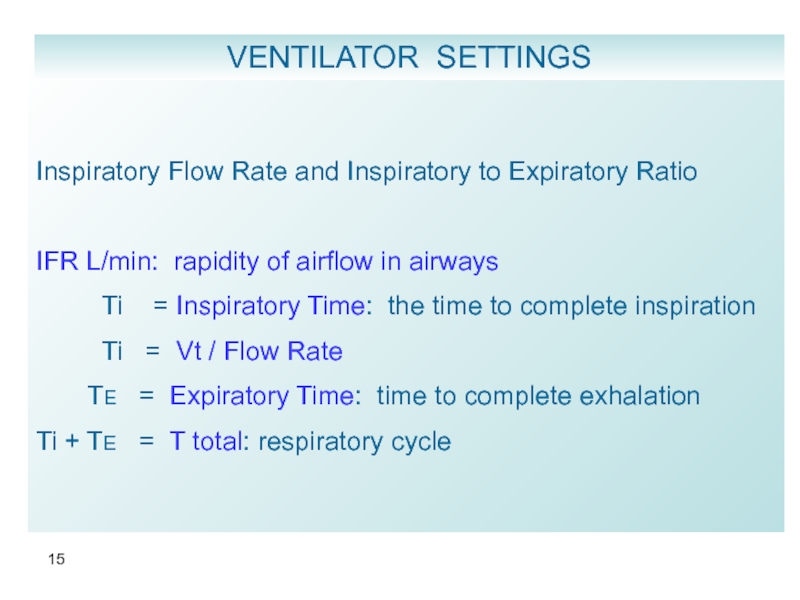
Слайд 15
Inspiratory Flow Rate and Inspiratory to Expiratory Ratio
IFR L/min: rapidity
Ti = Inspiratory Time: the time to complete inspiration
Ti = Vt / Flow Rate
TE = Expiratory Time: time to complete exhalation
Ti + TE = T total: respiratory cycle
VENTILATOR SETTINGS
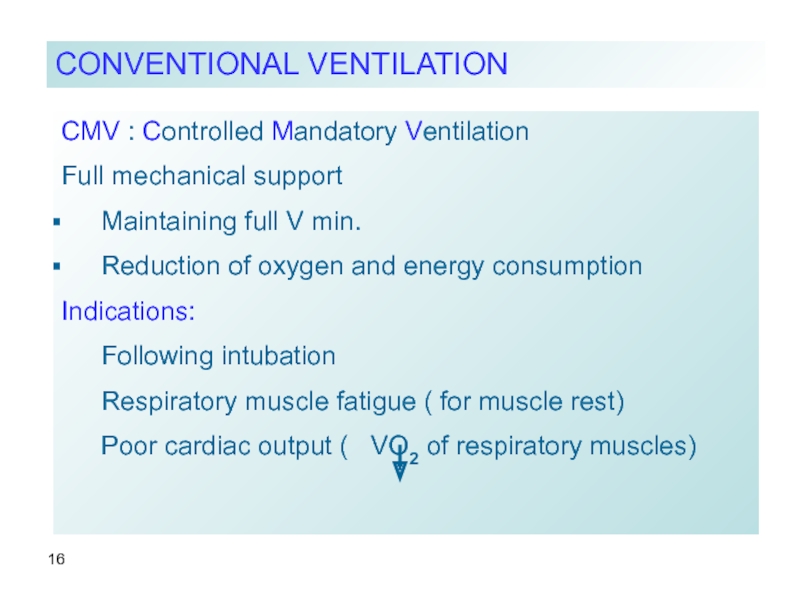
Слайд 16CMV : Controlled Mandatory Ventilation
Full mechanical support
Maintaining full V min.
Reduction of
Indications:
Following intubation
Respiratory muscle fatigue ( for muscle rest)
Poor cardiac output ( VO2 of respiratory muscles)
CONVENTIONAL VENTILATION
Слайд 17CMV
fixed rate
fixed Vt
fixed flow rate
FIO2
Disadvantages:
need for sedatives + relaxants
unresponsiveness
muscle atrophy
CONVENTIONAL VENTILATION
Airway pressure
Flow
inspirium
expirium
Patient’s spontaneous effort
Слайд 18ASSIST / CONTROL
⮞ Mechanical breath initiated by patient’s negative pressure.
⮞ Every
Disadvantages:
alkalosis
intrinsic PEEP
barotrauma: pneumothorax, pneumomediastinum,
subcutaneous emphysema, tension air cyst
CONVENTIONAL VENTILATION
Airway pressure
Flow
inspirium
expirium
Patient’s spontaneous effort
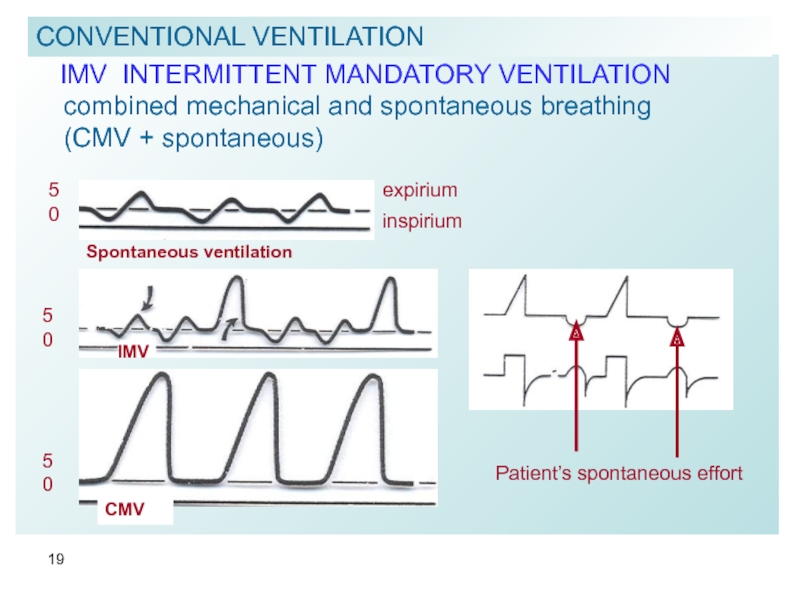
Слайд 19 IMV INTERMITTENT MANDATORY VENTILATION
combined mechanical and spontaneous
(CMV + spontaneous)
CONVENTIONAL VENTILATION
Spontaneous ventilation
5
0
inspirium
expirium
IMV
5
0
5
0
CMV
Patient’s spontaneous effort
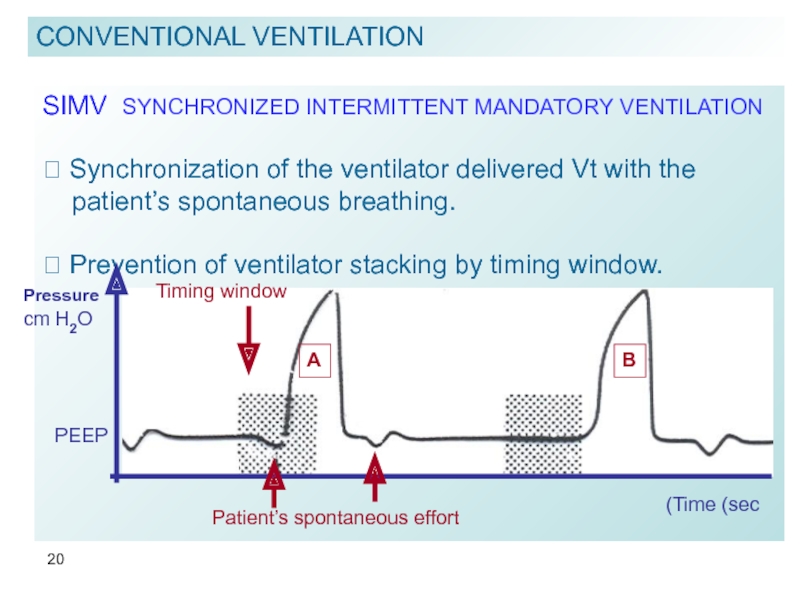
Слайд 20SIMV SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION
⮞ Synchronization of the ventilator delivered Vt
patient’s spontaneous breathing.
⮞ Prevention of ventilator stacking by timing window.
CONVENTIONAL VENTILATION
A
B
Timing window
Patient’s spontaneous effort
Time (sec)
Pressure
cm H2O
PEEP
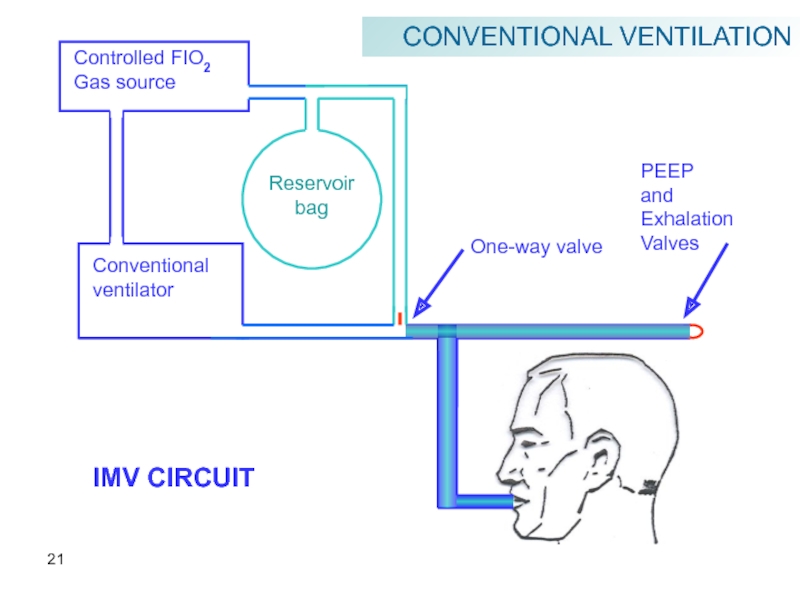
Слайд 21
Controlled FIO2
Gas source
Reservoir
bag
Conventional
ventilator
One-way valve
PEEP
and
Exhalation
Valves
IMV CIRCUIT
CONVENTIONAL VENTILATION
Слайд 22
IMV / SIMV
Advantages
⮞ decreased need in sedatives
prevention of muscle
⮞ lower airway pressure and intrathoracic pressure
hemodynamic stability
⮞ reduction in alkalosis
patient’s ability to regulate his rate and Vt according to metabolic requirements
CONVENTIONAL VENTILATION
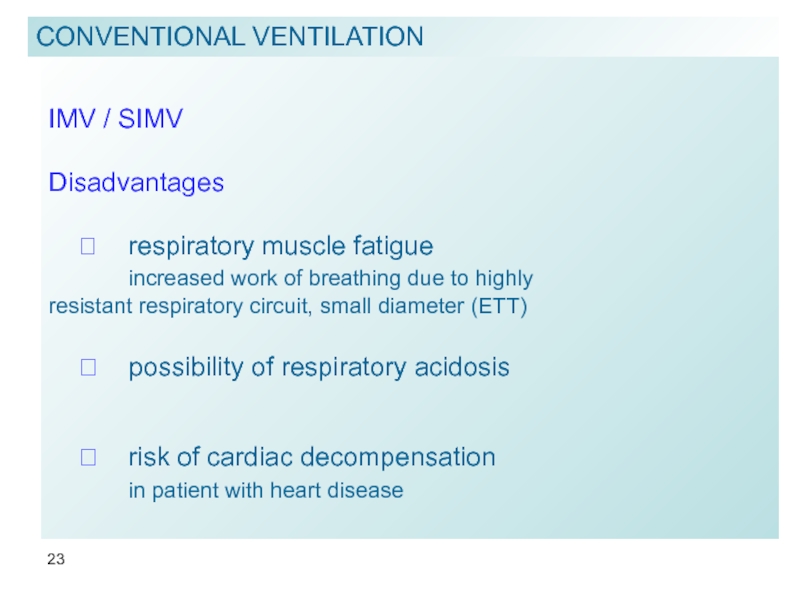
Слайд 23
IMV / SIMV
Disadvantages
⮞ respiratory muscle fatigue
increased work
⮞ possibility of respiratory acidosis
⮞ risk of cardiac decompensation
in patient with heart disease
CONVENTIONAL VENTILATION
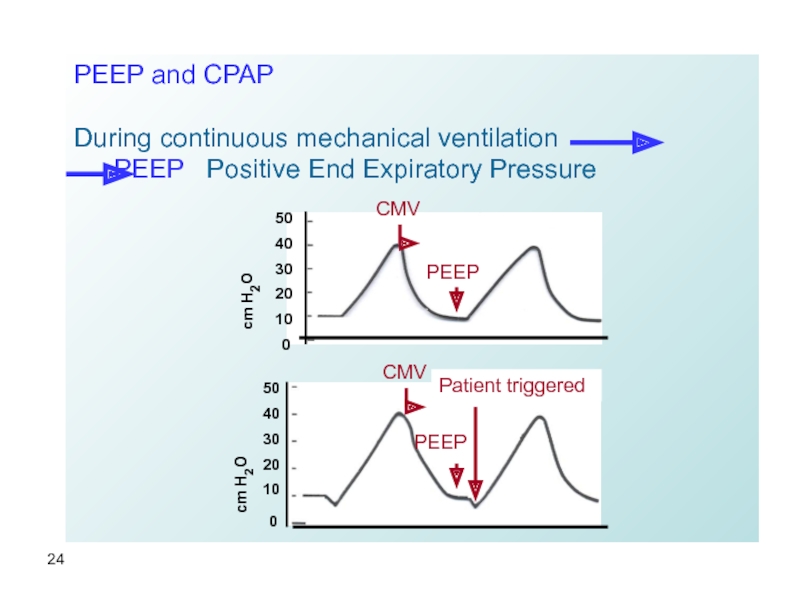
Слайд 24PEEP and CPAP
During continuous mechanical ventilation
PEEP Positive
50
40
30
20
10
0
cm H2O
CMV
PEEP
50
40
30
20
10
0
CMV
PEEP
Patient triggered
cm H2O
Слайд 25PEEP and CPAP
During spontaneous breathing
with or without inspiratory
CPAP Continuous Positive Airway Pressure
15
10
5
0
- 5
inspiration
expiration
PEEP
Слайд 26
Mechanism
- Decreases Qs/Qt
without reducing edema
- Reduces number
of flooded alveoli
- Redistributes edema to
peribroncho vascular
interstitial spaces
- Decreases work
of breathing
- Decreases preload
NON PEEP
PEEP
78.6 μ
146.8 μ
80%
20 %
Qs / Qt 23.8 % 5.1 %
PEEP & CPAP
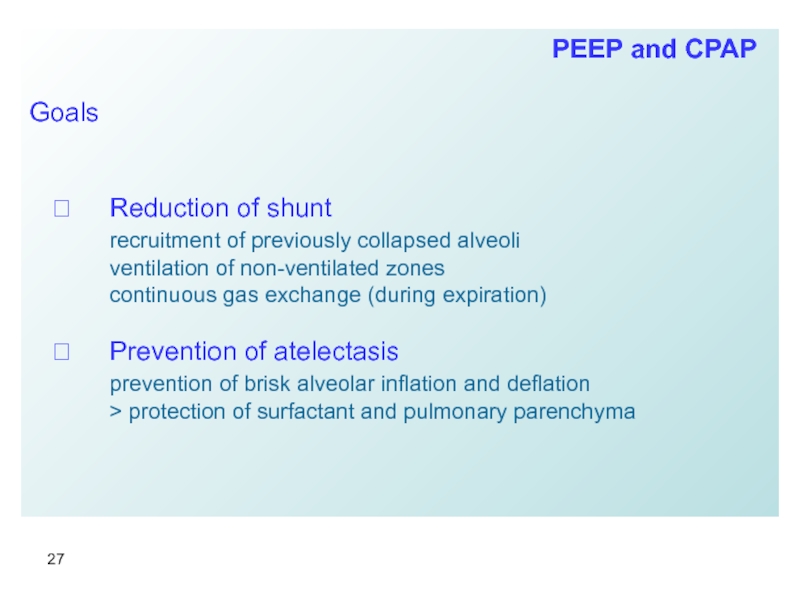
Слайд 27
Goals
⮞ Reduction of shunt
recruitment of previously collapsed alveoli
ventilation of
continuous gas exchange (during expiration)
⮞ Prevention of atelectasis
prevention of brisk alveolar inflation and deflation
> protection of surfactant and pulmonary parenchyma
PEEP and CPAP
Слайд 28
Complications
⮞ increased intrathoracic pressure
decrease of cardiac output
EFFECT of PEEP
venous
compression
PEEP and CPAP
Слайд 29
Complications
⮞ Increased ADH secretion, decrease of renal artery
decrease of urinary output and creatinine clearance
⮞ decreased venous return from brain
increased ICP
decrease of CPP
⮞ barotrauma – induced by PEEP ≈ 20%
PEEP and CPAP
Слайд 30PEEP / CPAP Therapy
Titrate EEP until:
⮞ PO2 ≈ 60 mmHg (Sat
provided cardiac output is maintained
⮞ Qs / Qt < 15%
⮞ Best PEEP on
volume-pressure
loop
15
30
B
D
C
A
Lower inflection point
Upper deflection point
500
250
Volume (mL)
Pressure cmH20
0
Слайд 31
PRESSURE SUPPORT VENTILATION (PS)
patient triggered, patient-controlled (flow-time),
pressure limited interactive ventilation with
20
15
10
5
B
C
A
D
time
Proximal
Airway
Pressure
cmH20
Слайд 32
PRESSURE SUPPORT VENTILATION (PS)
Synchrony
PS interaction with ventilatory muscles
PS adds to
Overload of ventilatory muscles
tachypnea, small Vt
PS Vt, RR
Vt mL/kg
Ventilator pressure
Muscle tension
12
8
4
Слайд 33
PRESSURE SUPPORT VENTILATION (PS)
Synchrony
Patient interaction with
⮞ Trigger
(prompt breath initiation, ventilator sensitivity and responsiveness)
⮞ Flow
adjustment of the gas delivery to the patient’s effort
⮞ Cycling
ventilator breath termination with the end of patient’s effort 25-30% of peak flow
Слайд 34
PRESSURE SUPPORT VENTILATION (PS)
Titration of PS
⮞ to overcome endotracheal tube
(6-10 cmH2O)
⮞ to achieve effective Vt and V min without
causing respiratory overload
⮞ non-invasive application
BIPAP* = CPAP + Pressure Support
*Bi-level Positive Airway Pressure
Слайд 35
PRESSURE CONTROL VENTILATION
Time and pressure controlled
Exhalation is passive
Vt and V min
(compliance and resistance)
Inverse ratio ventilation (IRV) I : E 3:1
Mandatory BIPAP
PEEP
pressure
T- inspiratory
T- expiratory
P. inspiratory
Tidal volume
volume
NON CONVENTIONAL VENTILATION
Слайд 36
Airway pressure release ventilation (APRV)
pressure
PEEP
Spontaneous breathing
time
volume
Spontaneous tidal volume
Tidal volume
P. inspiratory
NON CONVENTIONAL
Слайд 37NON CONVENTIONAL VENTILATION
Indication: severe hypoxemic respiratory failure
Breathing lung
(baby lung)
Edema
ARDS
Pleural effusion
Слайд 38NON CONVENTIONAL VENTILATION
Open Lung Conception
Pressure controlled, Inverse ratio ventilation with permissive
Permissive hypercapnia = increase of PCO2 until pH reaches 7.2
at pH < 7.2 give bicarbonate
Prone position
Nitric Oxide
Selective pulmonary vasodilator
Gravitational force
Слайд 39NON CONVENTIONAL VENTILATION
Proportional assist ventilation for spontaneously breathing patients
⮞
lung compliance and resistance
Perflubron liquid ventilation
⮞ injection of perfluorocarbon into the trachea aiming to recruiting
collapsed alveoli.
ECMO Extra Corporeal Membrane Oxygenator
IVOX IntraVenous Oxygenator (membrane “lung” inserted in inferior
vena cava
Слайд 40
HIGH FREQUENCY VENTILATION
RR 60 – 3600 / min
CONVECTION
DIFFUSION
TYPES
I. HFPPV
II. HFO high frequency oscillation
III. HFJT high frequency jet ventilation
INDICATIONS
I. Broncho-pleural fistula
II. Hypoxemic respiratory failure
NON CONVENTIONAL VENTILATION
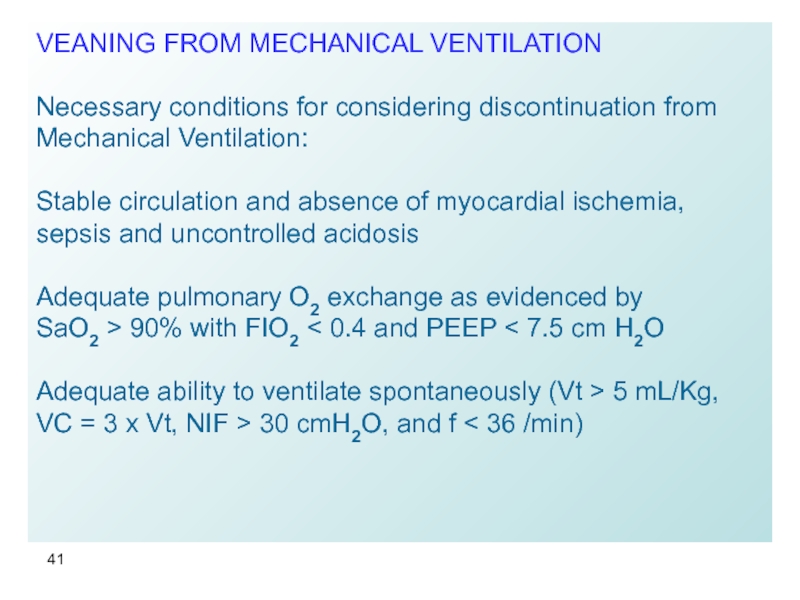
Слайд 41VEANING FROM MECHANICAL VENTILATION
Necessary conditions for considering discontinuation from Mechanical Ventilation:
Stable
Adequate pulmonary O2 exchange as evidenced by
SaO2 > 90% with FIO2 < 0.4 and PEEP < 7.5 cm H2O
Adequate ability to ventilate spontaneously (Vt > 5 mL/Kg, VC = 3 x Vt, NIF > 30 cmH2O, and f < 36 /min)
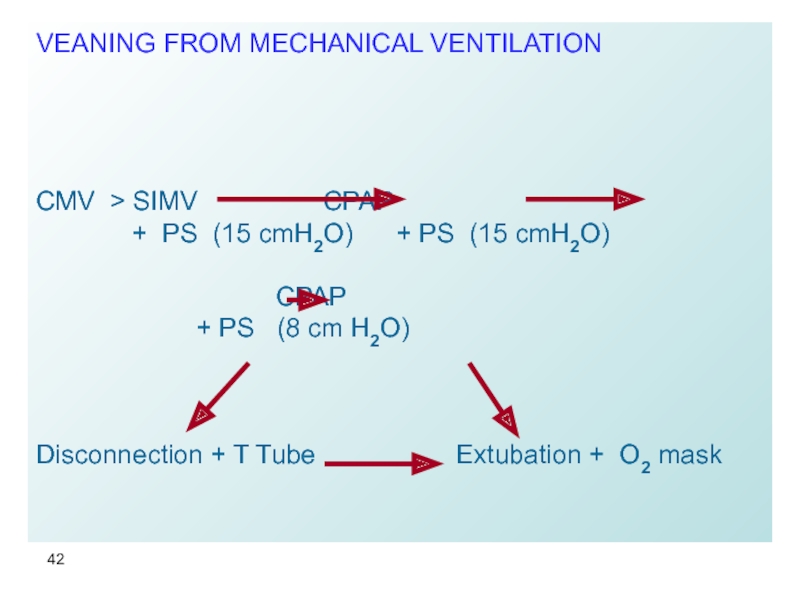
Слайд 42VEANING FROM MECHANICAL VENTILATION
CMV > SIMV CPAP
CPAP
+ PS (8 cm H2O)
Disconnection + T Tube Extubation + O2 mask