- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Mmunophysiology of liver. Immunophysiology of liver functions of liver and immune system презентация
Содержание
- 1. Mmunophysiology of liver. Immunophysiology of liver functions of liver and immune system
- 6. Immunological and metabolic roles of hepatocytes. Hepatocytes
- 9. Liver and immune system can regulate metabolic
- 11. Most cytokine research on obesity-related diseases has
- 14. Figure. Hypothesis explaining the progression of NAFLD/NASH.
- 16. In addition to the perisinusoidal stellate cells,
- 19. Vasoactive agents, produced by KC (Kupffer cells)
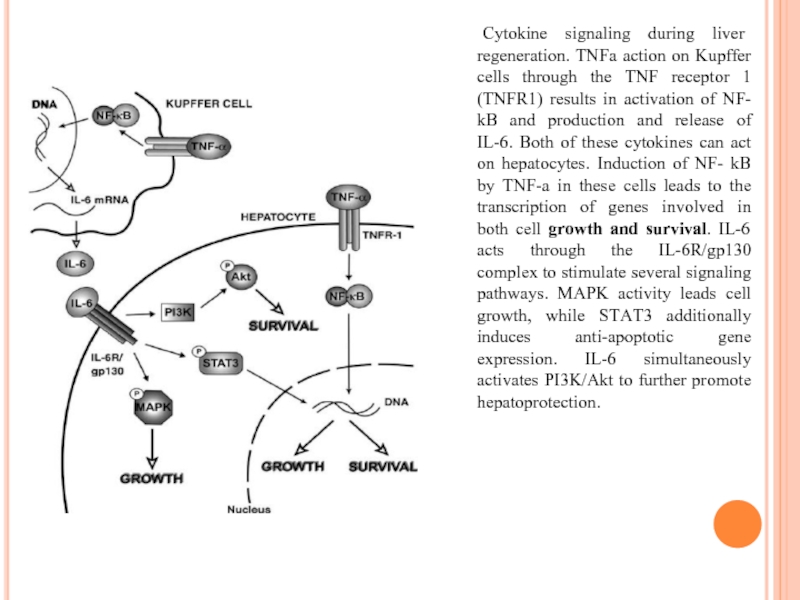
- 21. Cytokine signaling during liver regeneration. TNFa action
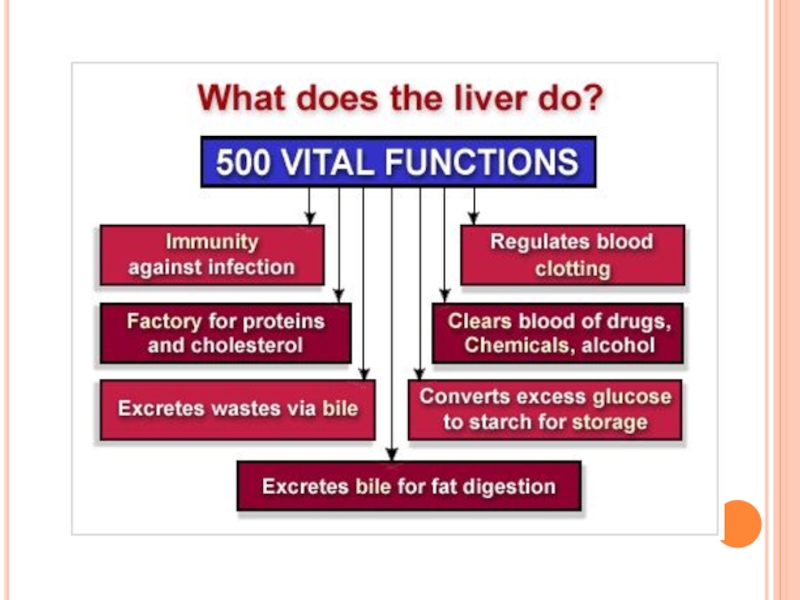
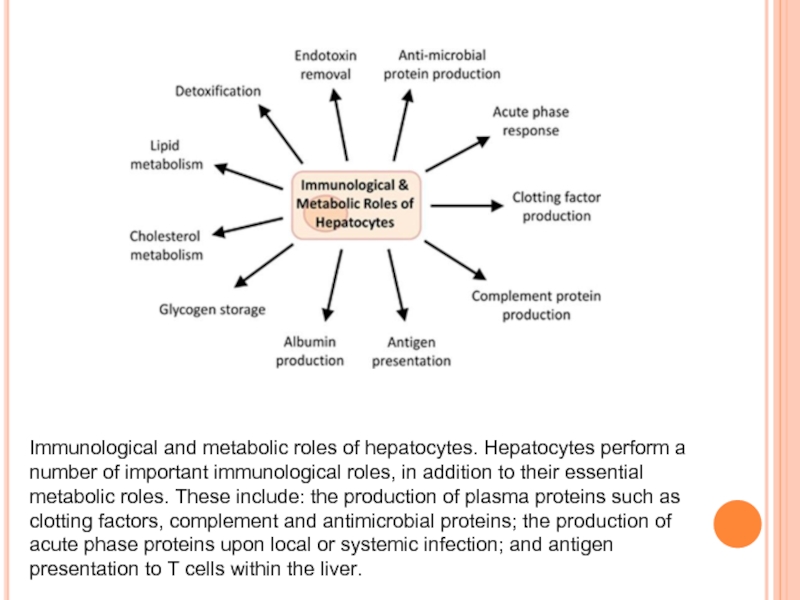
Слайд 6Immunological and metabolic roles of hepatocytes. Hepatocytes perform a number of
important immunological roles, in addition to their essential metabolic roles. These include: the production of plasma proteins such as clotting factors, complement and antimicrobial proteins; the production of acute phase proteins upon local or systemic infection; and antigen presentation to T cells within the liver.
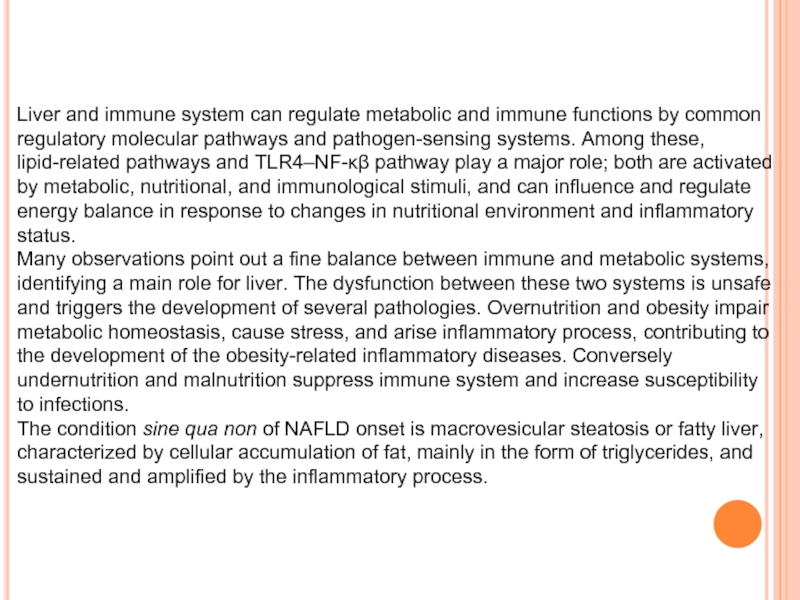
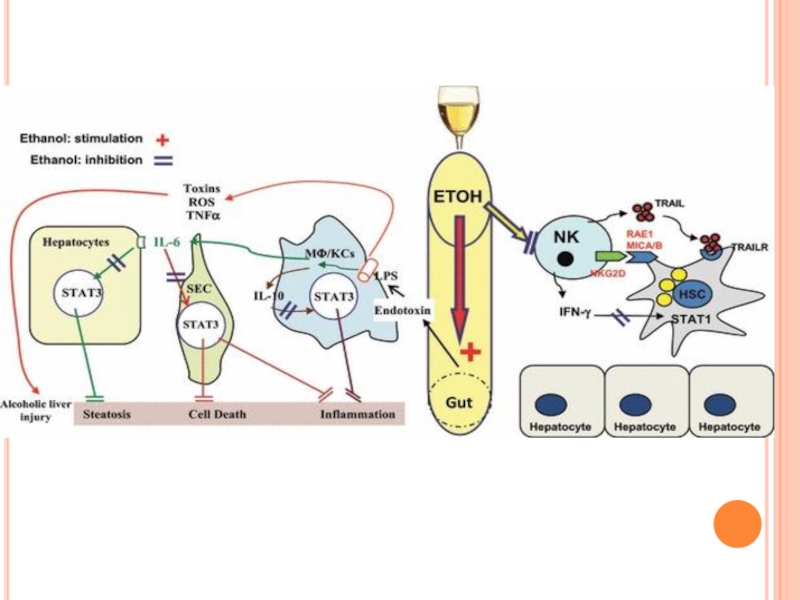
Слайд 9Liver and immune system can regulate metabolic and immune functions by
common regulatory molecular pathways and pathogen-sensing systems. Among these, lipid-related pathways and TLR4–NF-κβ pathway play a major role; both are activated by metabolic, nutritional, and immunological stimuli, and can influence and regulate energy balance in response to changes in nutritional environment and inflammatory status.
Many observations point out a fine balance between immune and metabolic systems, identifying a main role for liver. The dysfunction between these two systems is unsafe and triggers the development of several pathologies. Overnutrition and obesity impair metabolic homeostasis, cause stress, and arise inflammatory process, contributing to the development of the obesity-related inflammatory diseases. Conversely undernutrition and malnutrition suppress immune system and increase susceptibility to infections.
The condition sine qua non of NAFLD onset is macrovesicular steatosis or fatty liver, characterized by cellular accumulation of fat, mainly in the form of triglycerides, and sustained and amplified by the inflammatory process.
Many observations point out a fine balance between immune and metabolic systems, identifying a main role for liver. The dysfunction between these two systems is unsafe and triggers the development of several pathologies. Overnutrition and obesity impair metabolic homeostasis, cause stress, and arise inflammatory process, contributing to the development of the obesity-related inflammatory diseases. Conversely undernutrition and malnutrition suppress immune system and increase susceptibility to infections.
The condition sine qua non of NAFLD onset is macrovesicular steatosis or fatty liver, characterized by cellular accumulation of fat, mainly in the form of triglycerides, and sustained and amplified by the inflammatory process.
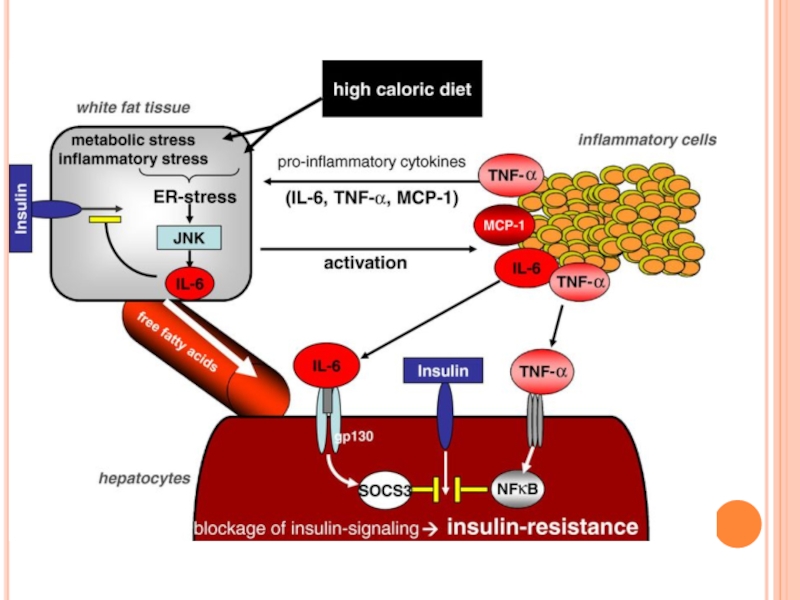
Слайд 11Most cytokine research on obesity-related diseases has centered on IL-6, which
was among the first cytokine to be implicated as a predictor or pathogenetic marker of Insulin Resistance (IR) and cardiovascular disease. This cytokine plays a key role in the onset of hepatic IR, which was found reduced in obese mice on high fat diet treated with anti-IL-6 antibodies.
A definite answer to the role of IL-6 in IR will be only possible when more clinical data will be available on the use of IL-6-neutralizing antibody in diabetic and/or IR patients. To date only two small clinical trials, however, suggest a beneficial effect.
A definite answer to the role of IL-6 in IR will be only possible when more clinical data will be available on the use of IL-6-neutralizing antibody in diabetic and/or IR patients. To date only two small clinical trials, however, suggest a beneficial effect.
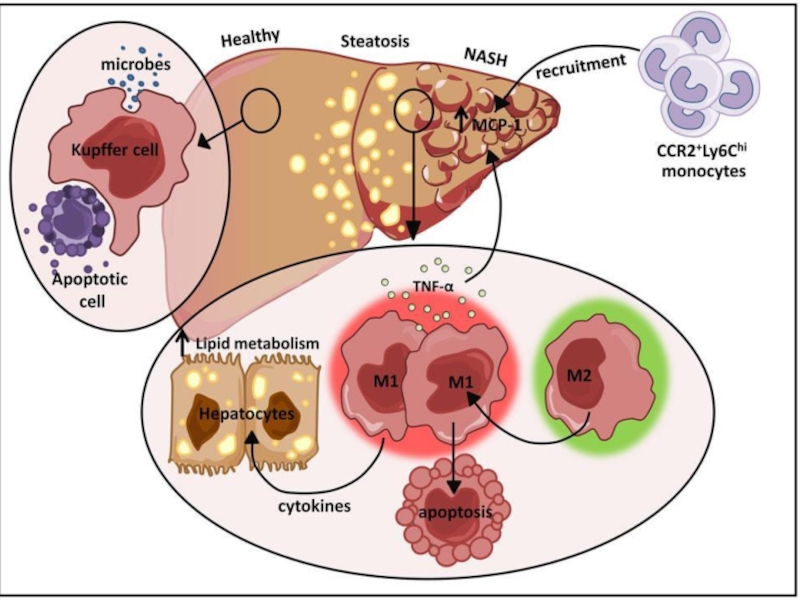
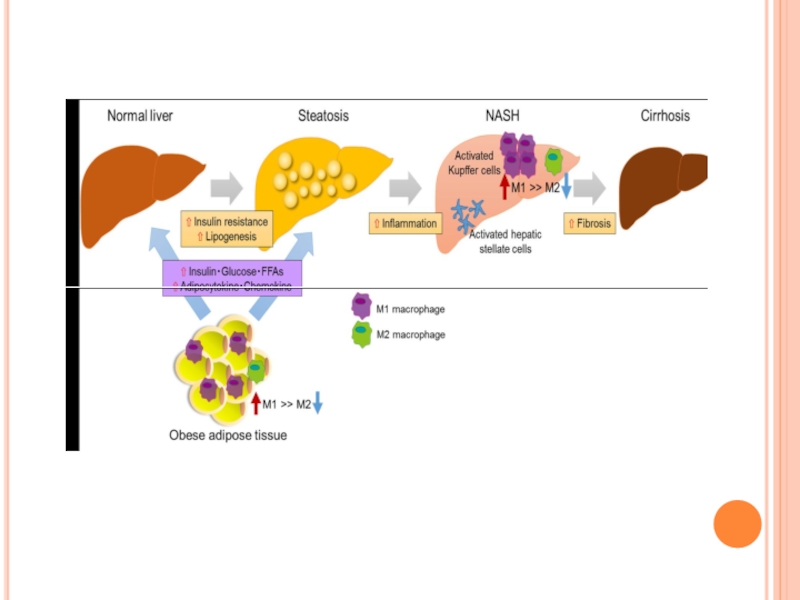
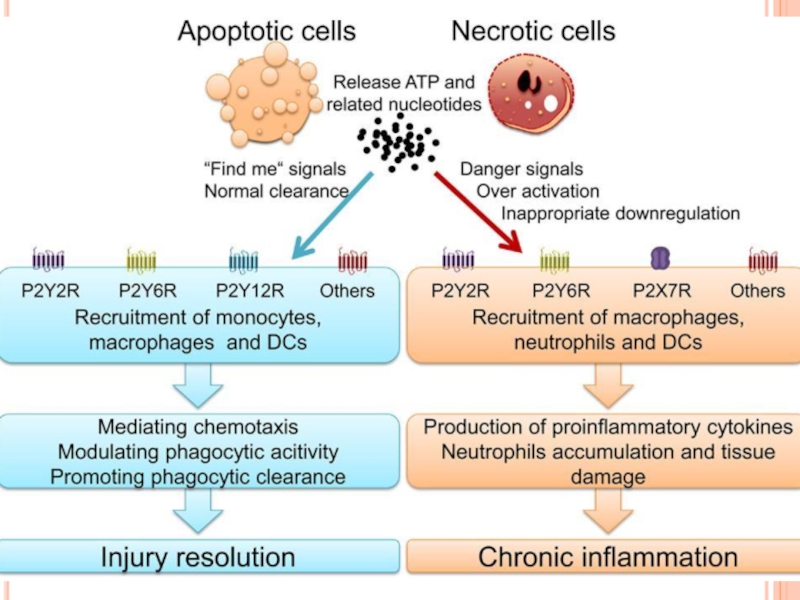
Слайд 14Figure. Hypothesis explaining the progression of NAFLD/NASH.
Overnutrition or inactivity leads
to adipocyte hypertrophy and dysfunction, which are linked to chronic inflammation and insulin resistance through the recruitment and activation of immune cells such as macrophages and T-cells.
Excess fat intake and obesity lead to hyperglycemia, hyperlipidemia, and the oversecretion of adipocytokines and the chemokines tumor necrosis factor (TNF)-a, interleukin (IL)-1, and monocyte chemoattractant protein (MCP)-1/C-C chemokine ligand 2 (CCL2). These factors further contribute to the development of systemic insulin resistance and hepatic steatosis. The latter causes hepatic
inflammation and induces NASH and even cirrhosis. Hepatic inflammation involves the recruitment of macrophages/Kupffer cells and an M1-dominant phenotypic shift in macrophages in the liver, activating hepatic stellate cells and finally leading to liver fibrosis.
Excess fat intake and obesity lead to hyperglycemia, hyperlipidemia, and the oversecretion of adipocytokines and the chemokines tumor necrosis factor (TNF)-a, interleukin (IL)-1, and monocyte chemoattractant protein (MCP)-1/C-C chemokine ligand 2 (CCL2). These factors further contribute to the development of systemic insulin resistance and hepatic steatosis. The latter causes hepatic
inflammation and induces NASH and even cirrhosis. Hepatic inflammation involves the recruitment of macrophages/Kupffer cells and an M1-dominant phenotypic shift in macrophages in the liver, activating hepatic stellate cells and finally leading to liver fibrosis.
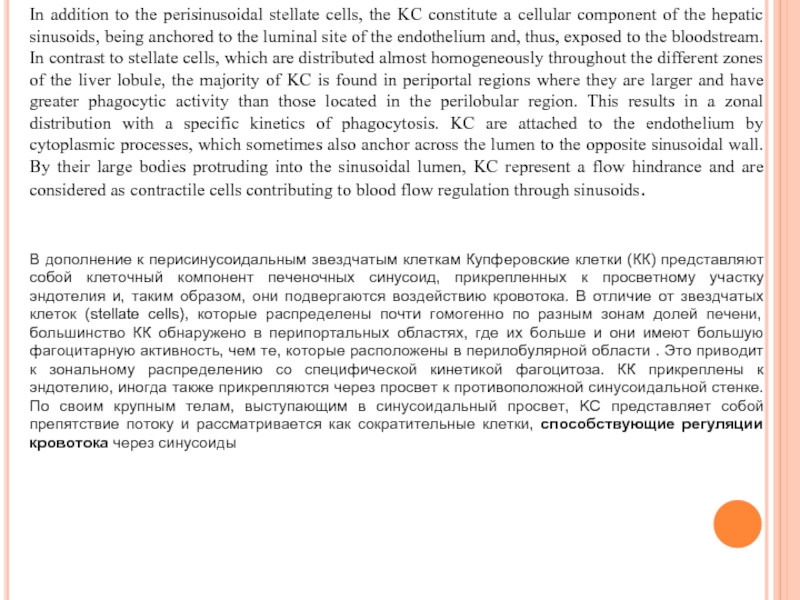
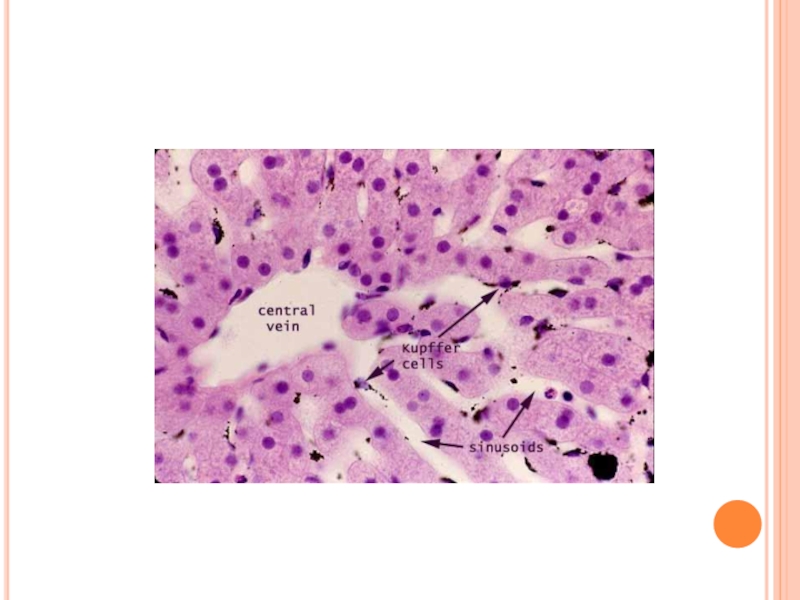
Слайд 16In addition to the perisinusoidal stellate cells, the KC constitute a
cellular component of the hepatic sinusoids, being anchored to the luminal site of the endothelium and, thus, exposed to the bloodstream. In contrast to stellate cells, which are distributed almost homogeneously throughout the different zones of the liver lobule, the majority of KC is found in periportal regions where they are larger and have greater phagocytic activity than those located in the perilobular region. This results in a zonal distribution with a specific kinetics of phagocytosis. KC are attached to the endothelium by cytoplasmic processes, which sometimes also anchor across the lumen to the opposite sinusoidal wall. By their large bodies protruding into the sinusoidal lumen, KC represent a flow hindrance and are considered as contractile cells contributing to blood flow regulation through sinusoids.
В дополнение к перисинусоидальным звездчатым клеткам Купферовские клетки (КК) представляют собой клеточный компонент печеночных синусоид, прикрепленных к просветному участку эндотелия и, таким образом, они подвергаются воздействию кровотока. В отличие от звездчатых клеток (stellate cells), которые распределены почти гомогенно по разным зонам долей печени, большинство КК обнаружено в перипортальных областях, где их больше и они имеют большую фагоцитарную активность, чем те, которые расположены в перилобулярной области . Это приводит к зональному распределению со специфической кинетикой фагоцитоза. КК прикреплены к эндотелию, иногда также прикрепляются через просвет к противоположной синусоидальной стенке. По своим крупным телам, выступающим в синусоидальный просвет, KC представляет собой препятствие потоку и рассматривается как сократительные клетки, способствующие регуляции кровотока через синусоиды
В дополнение к перисинусоидальным звездчатым клеткам Купферовские клетки (КК) представляют собой клеточный компонент печеночных синусоид, прикрепленных к просветному участку эндотелия и, таким образом, они подвергаются воздействию кровотока. В отличие от звездчатых клеток (stellate cells), которые распределены почти гомогенно по разным зонам долей печени, большинство КК обнаружено в перипортальных областях, где их больше и они имеют большую фагоцитарную активность, чем те, которые расположены в перилобулярной области . Это приводит к зональному распределению со специфической кинетикой фагоцитоза. КК прикреплены к эндотелию, иногда также прикрепляются через просвет к противоположной синусоидальной стенке. По своим крупным телам, выступающим в синусоидальный просвет, KC представляет собой препятствие потоку и рассматривается как сократительные клетки, способствующие регуляции кровотока через синусоиды
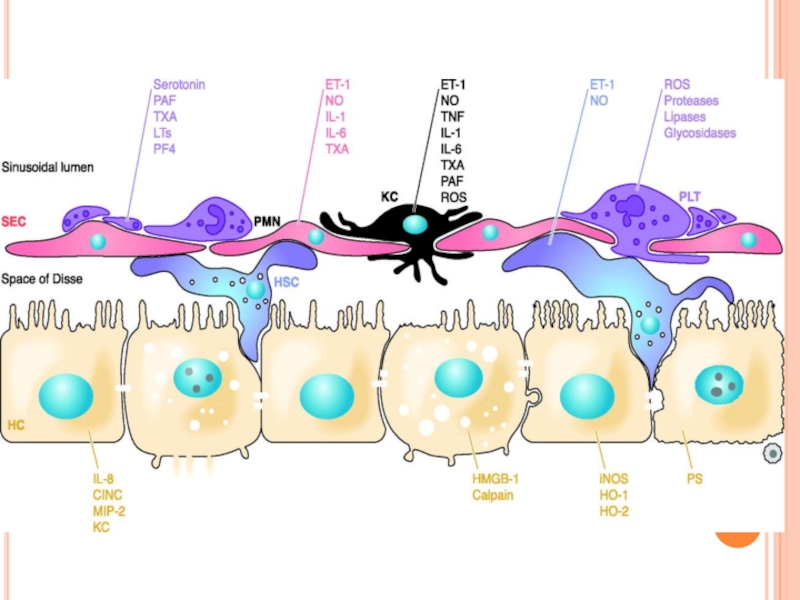
Слайд 19Vasoactive agents, produced by KC (Kupffer cells)
Agents Function
Thromboxane A2 Vasoconstriction,
platelet activation and aggregation, leukocyte adhesion,
2. Nitric oxide Vasodilation
3. Endothelin-1 Vasoconstriction Vasodilation
4. Carbon monoxide Vasodilation
2. Nitric oxide Vasodilation
3. Endothelin-1 Vasoconstriction Vasodilation
4. Carbon monoxide Vasodilation
Слайд 21 Cytokine signaling during liver regeneration. TNFa action on Kupffer cells through
the TNF receptor 1 (TNFR1) results in activation of NF- kB and production and release of IL-6. Both of these cytokines can act on hepatocytes. Induction of NF- kB by TNF-a in these cells leads to the transcription of genes involved in both cell growth and survival. IL-6 acts through the IL-6R/gp130 complex to stimulate several signaling pathways. MAPK activity leads cell growth, while STAT3 additionally induces anti-apoptotic gene expression. IL-6 simultaneously activates PI3K/Akt to further promote hepatoprotection.