- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Investigation of the gastrointestinal tract (GIT) презентация
Содержание
- 1. Investigation of the gastrointestinal tract (GIT)
- 2. Oral contrast investigation
- 4. Single and double contrast studies are
- 7. Barium examinations
- 10. The flow
- 11. Anatomy of
- 12. The oesophagus when full of barium should
- 13. The aortic arch gives a clearly visible
- 14. Peristaltic waves can be observed during fluoroscopy.
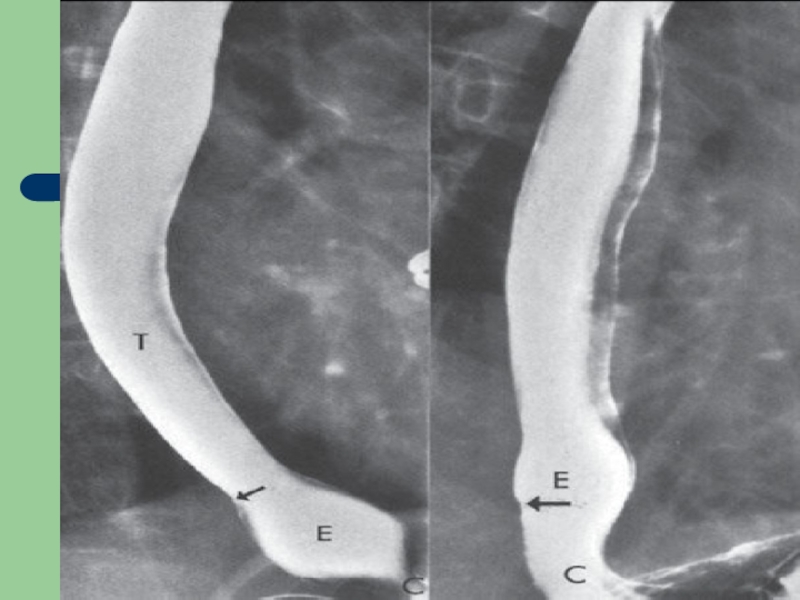
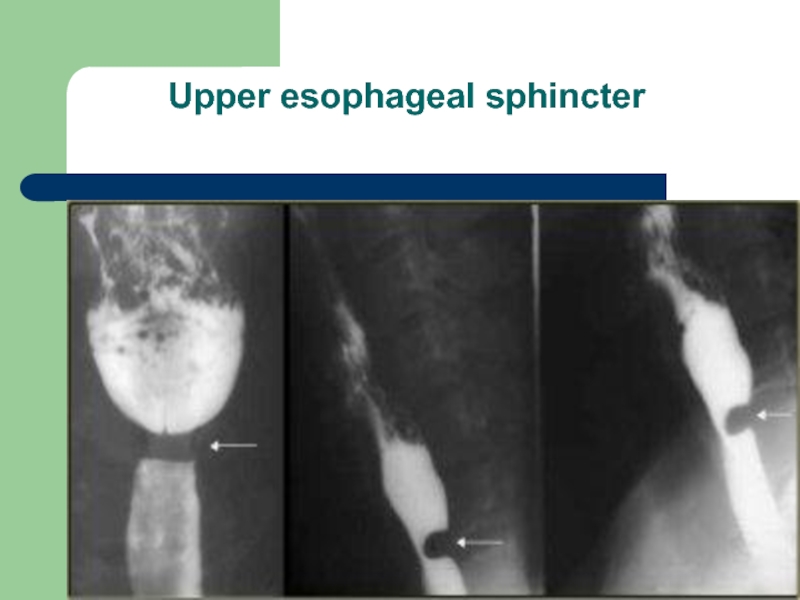
- 18. Upper esophageal sphincter
- 19. Barium examinations of the stomach
- 23. Anatomy of the
- 24. The duodenal cap or bulb should be
- 28. The outline of the lesser curve of
- 29. The duodenal cap or bulb should be
- 31. Causes of gastric displacement enlargement
- 32. Examinations of the Small Intestine
- 33. However, the peroral small bowel study is
- 34. Enteroclysis is an intubated examination of the
- 35. Retrograde examination of the small bowel involves
- 36. Anatomy of the small intestine
- 37. Depending on the degree of distention, the
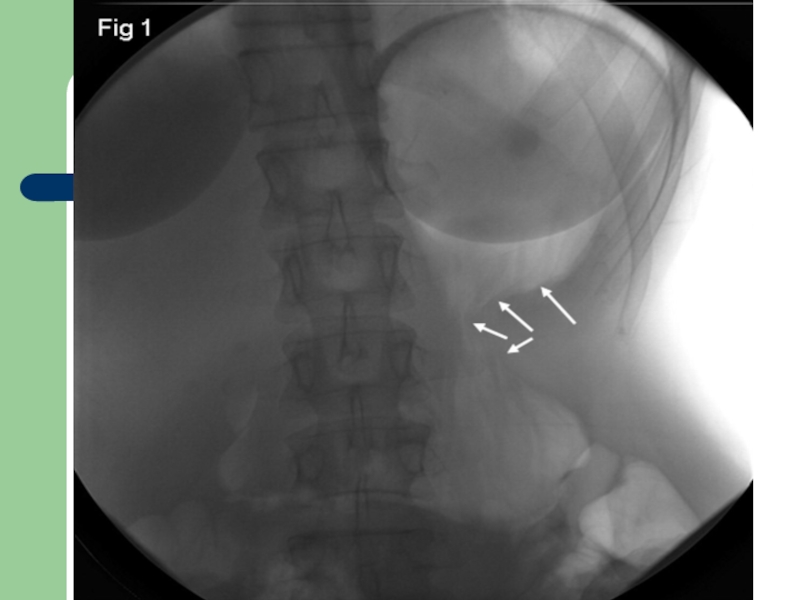
- 39. Enteroclysis
- 40. Examinations of the Large Intestine
- 41. The single-contrast method simply involves filling
- 44. Anatomy of the large intestine
- 45. The mucosal surface has a smooth
- 48. Computed Tomography (CT) Scanning Uses
- 52. Magnetic Resonance Imaging MRI imaging
- 53. Also, with the use of luminal distention
- 55. Isotope
- 57. Patient
- 58. Also, if patients are to have
- 59. Preparation for the barium enema is much
- 60. The standard preparation includes (1) a
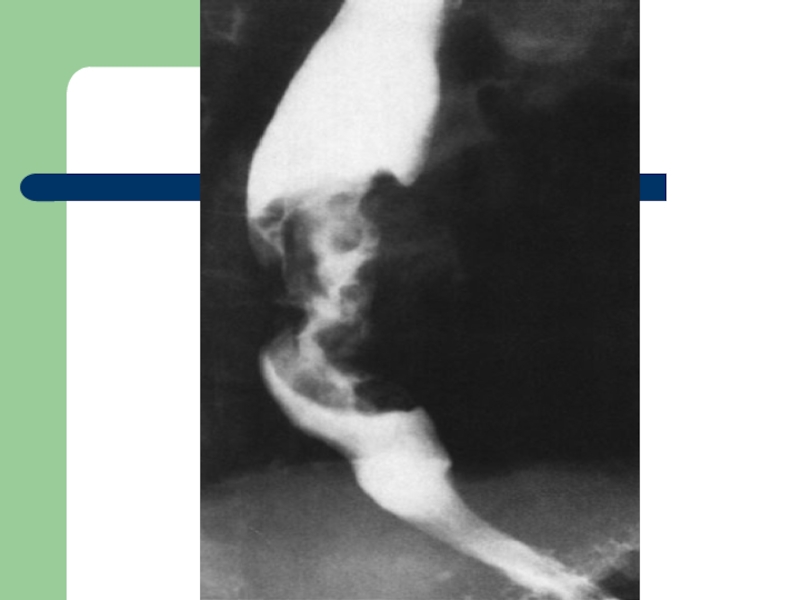
- 62. Unlike strictures of
- 63. Often, by this stage, the body of
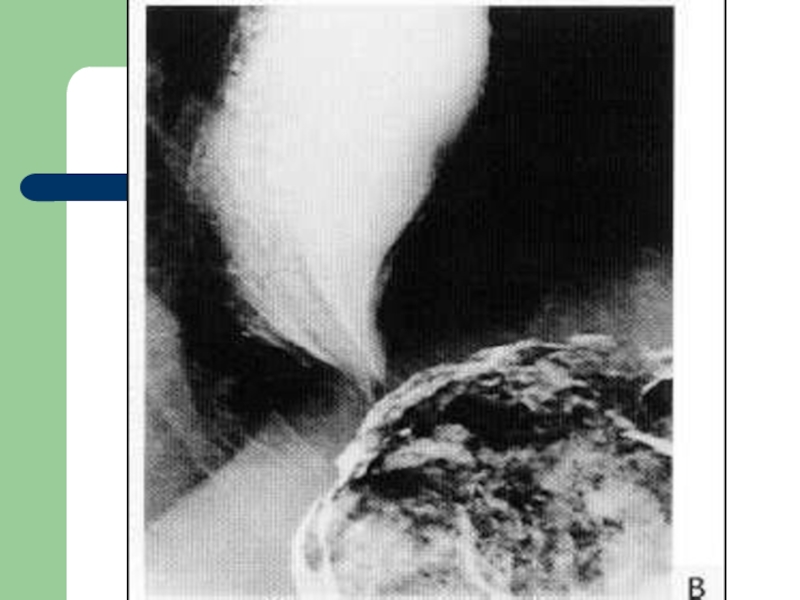
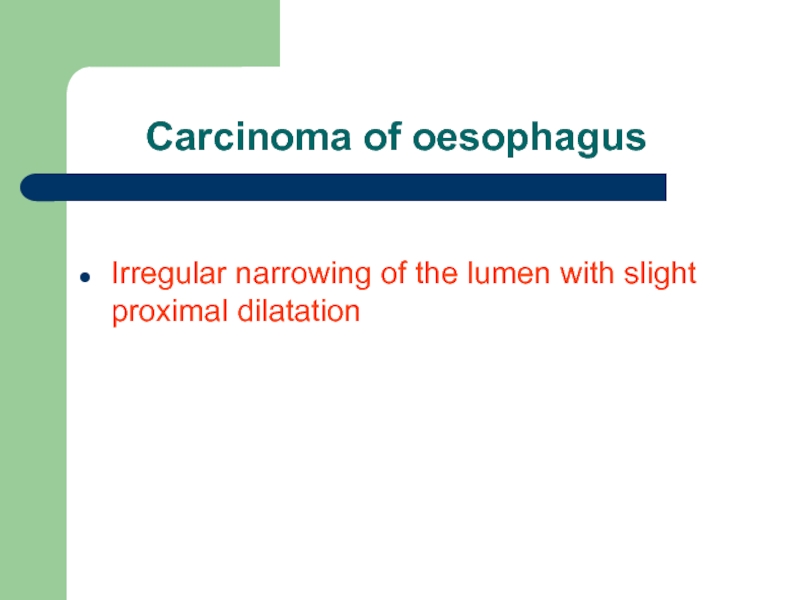
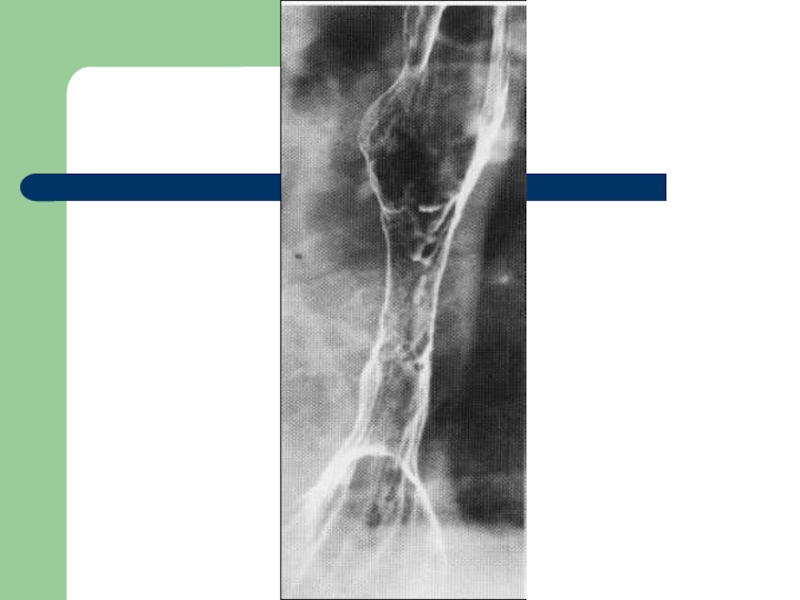
- 65. Carcinoma of oesophagus
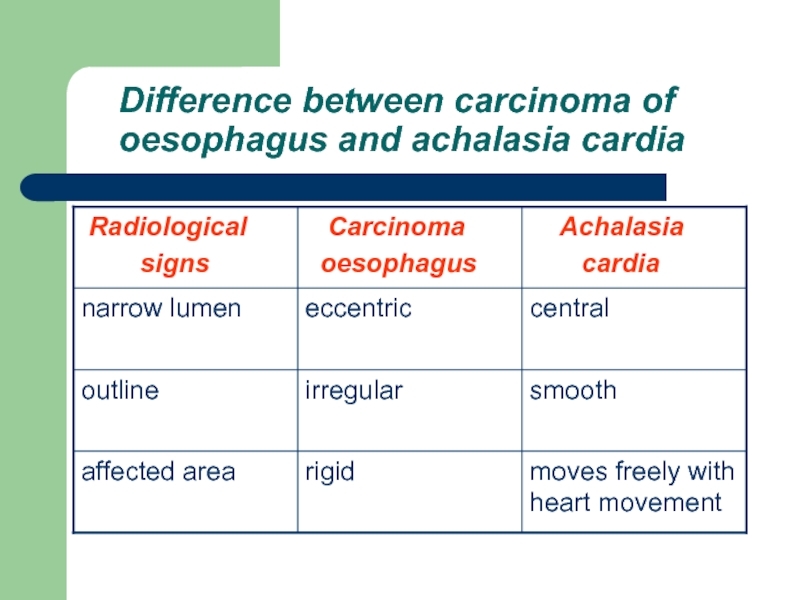
- 66. Difference between carcinoma of oesophagus and achalasia cardia
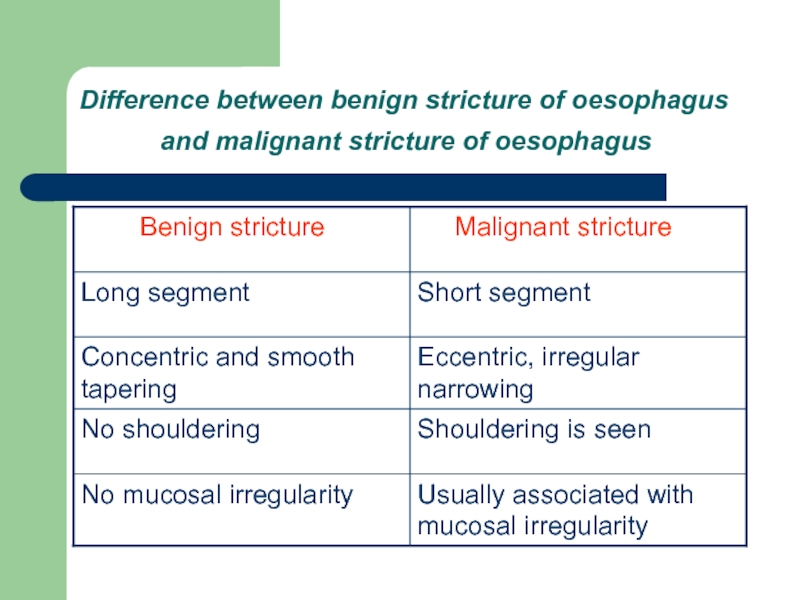
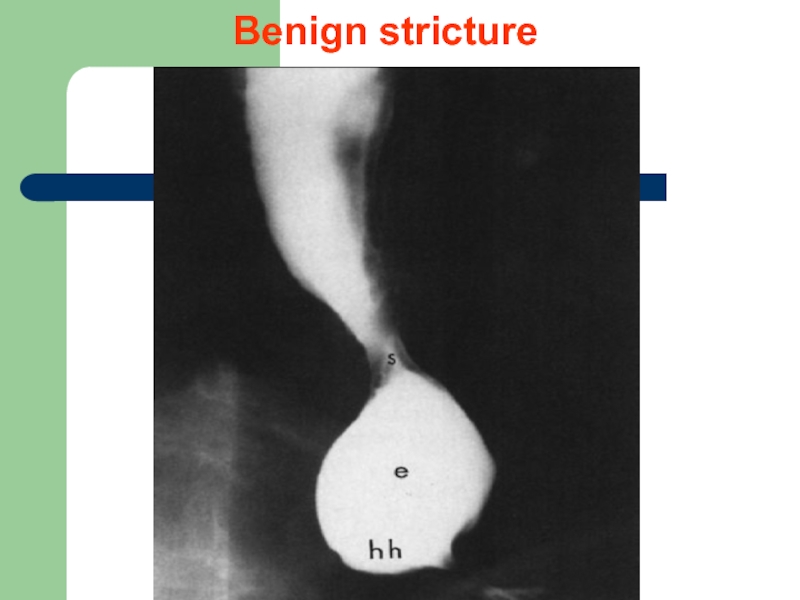
- 67. Difference between benign stricture of oesophagus
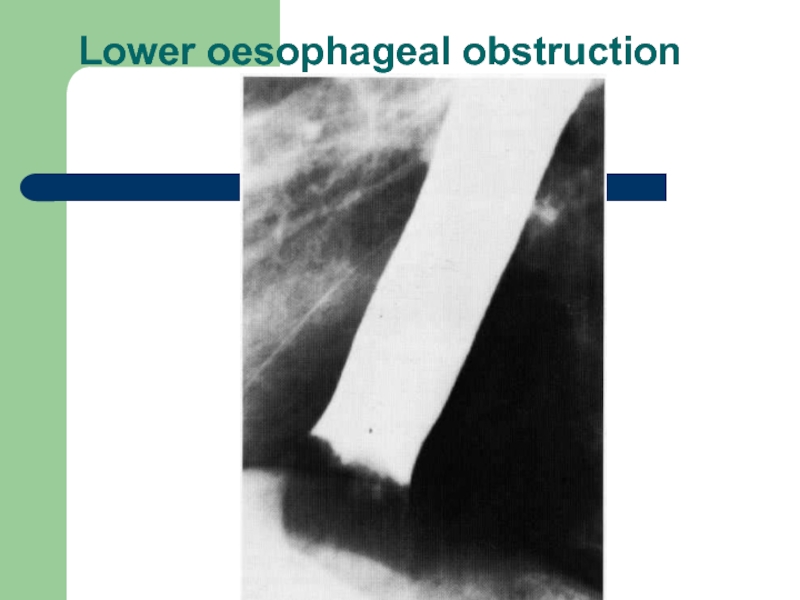
- 69. Lower oesophageal obstruction
- 70. Benign stricture
- 73. Radiological sings:
- 74. Complications: * Aspiration * Pneumonia
- 76. Zenker’s diverticulum
- 80. Radiographic signs
- 81. The en face radiographic signs of gastric
- 82. it may be demonstrated as a ‘ring’
- 83. The in profile radiographic signs of
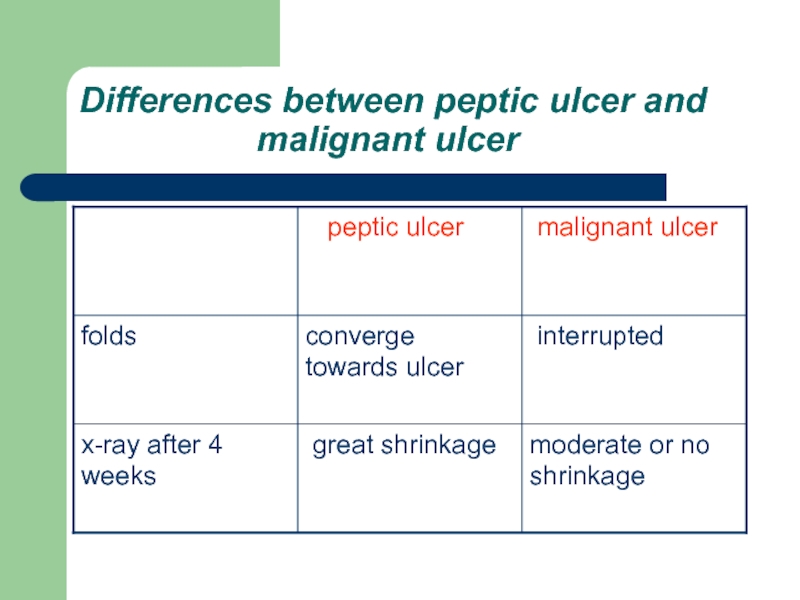
- 85. Differences between peptic ulcer and
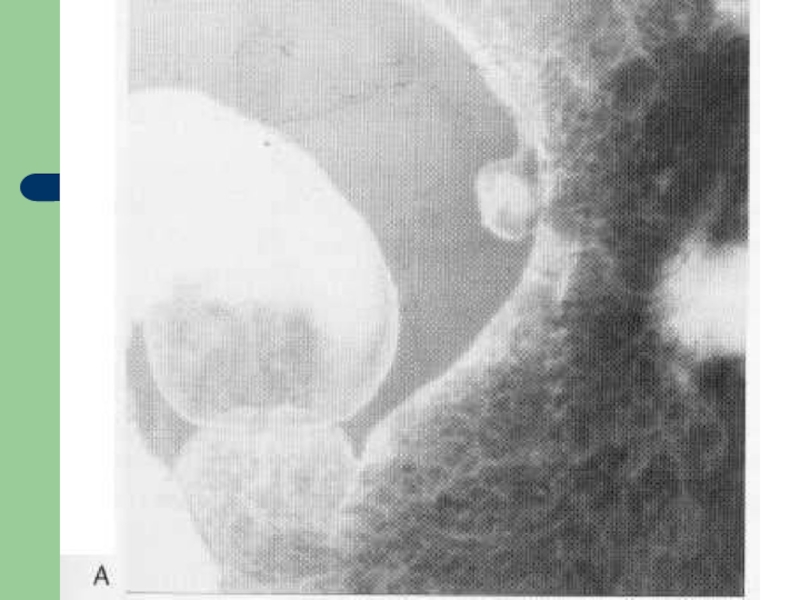
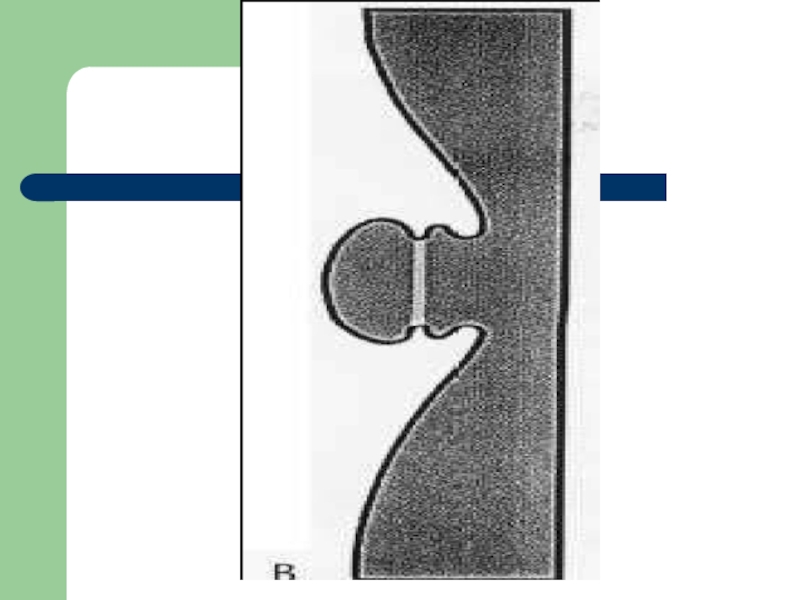
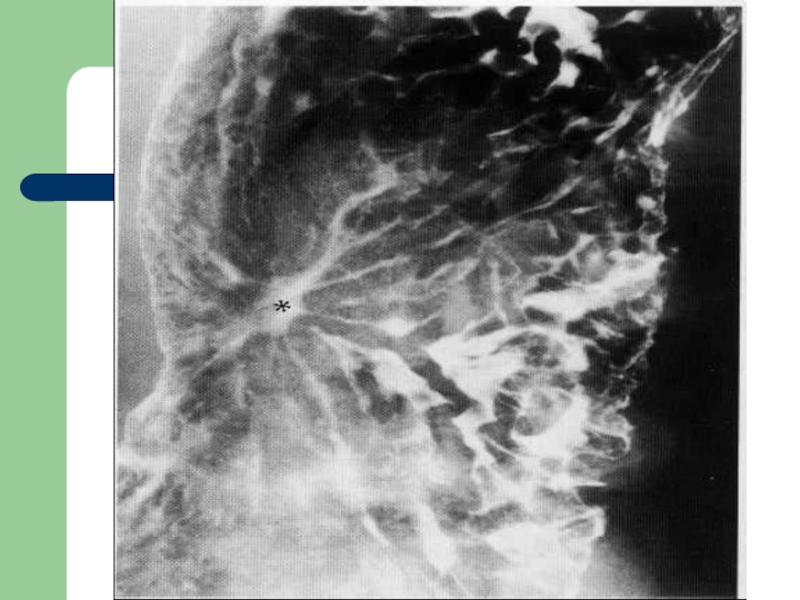
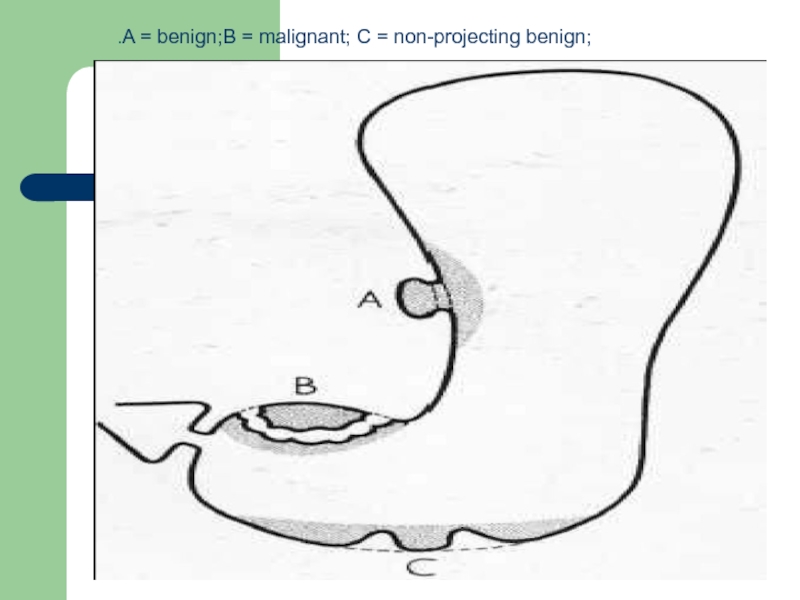
- 90. .A = benign;B = malignant; C = non-projecting benign;
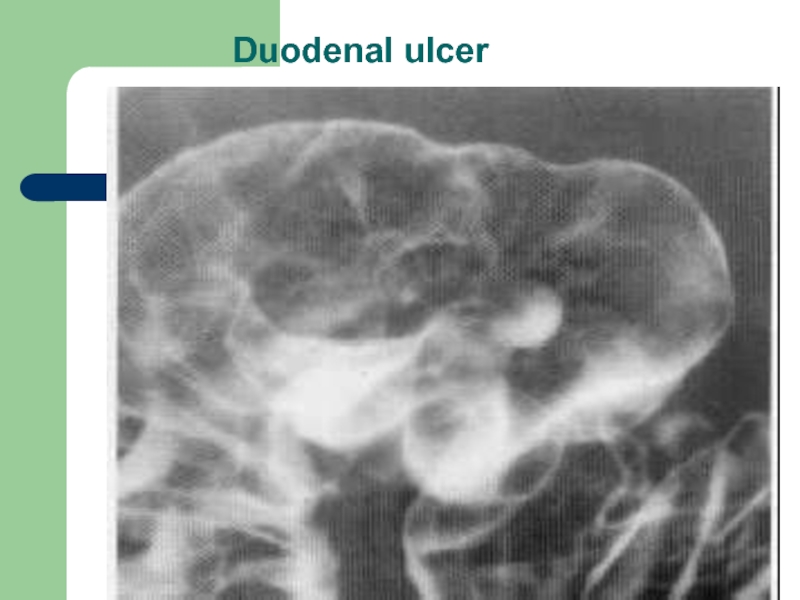
- 91. Duodenal ulcer
- 96. The most common findings are
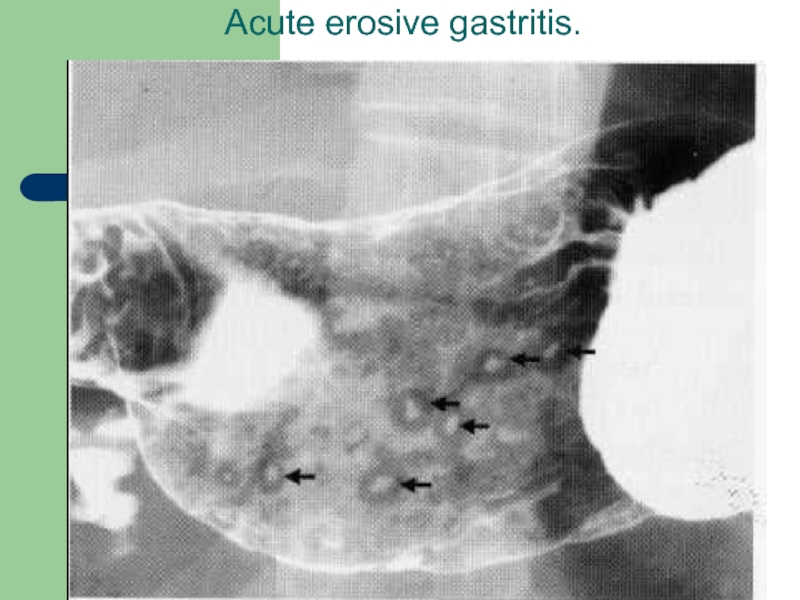
- 97. Acute erosive gastritis.
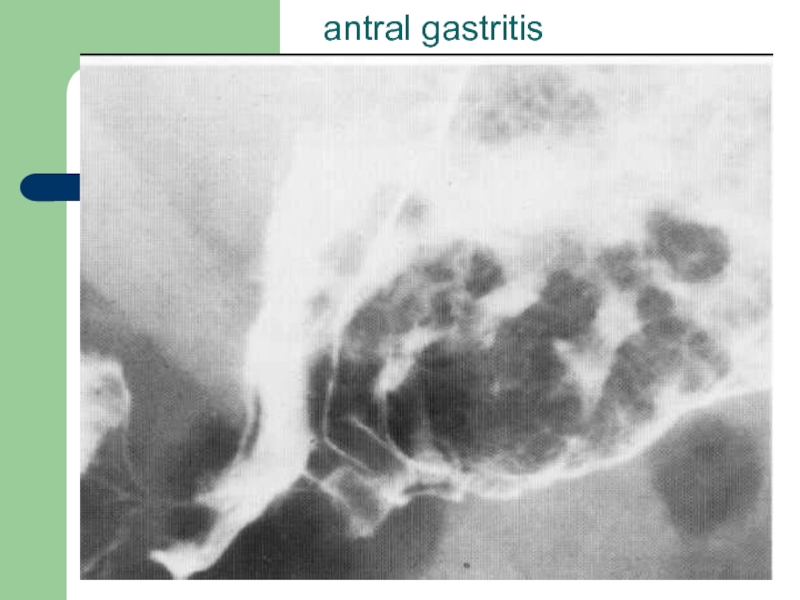
- 98. antral gastritis
- 100. Hypertrophic pyloric stenosis Hypertrophic
- 102. USG is investigation of
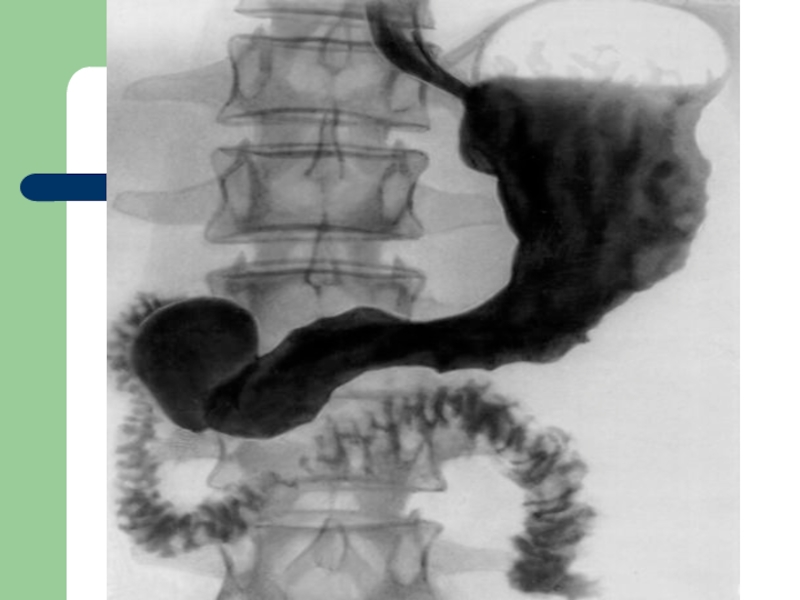
- 112. The most common presentations on the double-contrast
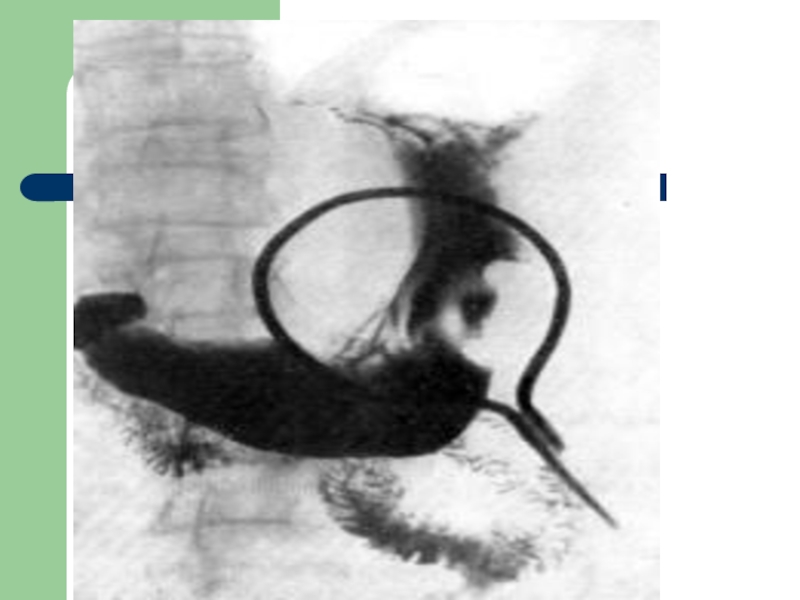
- 113. A primary neoplastic ulcer is often indistinguishable
Слайд 2 Oral contrast investigation
Barium sulphate is the best
its atomic number is high
it produces excellent opacification
good coating of the mucosa
non-absorbable
non-toxic
it is completely inert
Слайд 3 Limitations
causes chemical
extravasation into bronchial tree will cause inflammation and granuloma formation
barium inspissations in case of colonic obstruction hard stones
Слайд 4Single and double contrast studies are
In single contrast method bowel is filed only with barium.
In double contrast, the mucosa is coated with barium and introduction of gas distends the lumen of the bowel. Double contrast method demonstrates mucosal irregularities which are obscured in single contrast.
Слайд 5 Gastrograffin
Other available
The principal value of water soluble contrast media is to demonstrate leaks from the bowel and outlining fistulous tracts as they are safe in perforation cases.
Слайд 6 Barium swallow
It is the
Слайд 7 Barium examinations of the
Indications:
dysphagia (causes: corrosive strictures, carcinoma and achalasia)
motility disorders of oesophagus
pharingo-oesophageal malignancies
pharyngeal diverticula
webs
Слайд 8 Contraindications:
tracheo-oesophageal fistula
perforation
because the barium
Therefore, to diagnose these conditions water soluble non-ionic contrast media such as omnipaque, ultravist are used.
Слайд 9 Procedure
The
Слайд 10 The flow of barium is noted
pharynx
cervical oesophagus
epiphrenic oesophagus
gastro-oesophageal junction
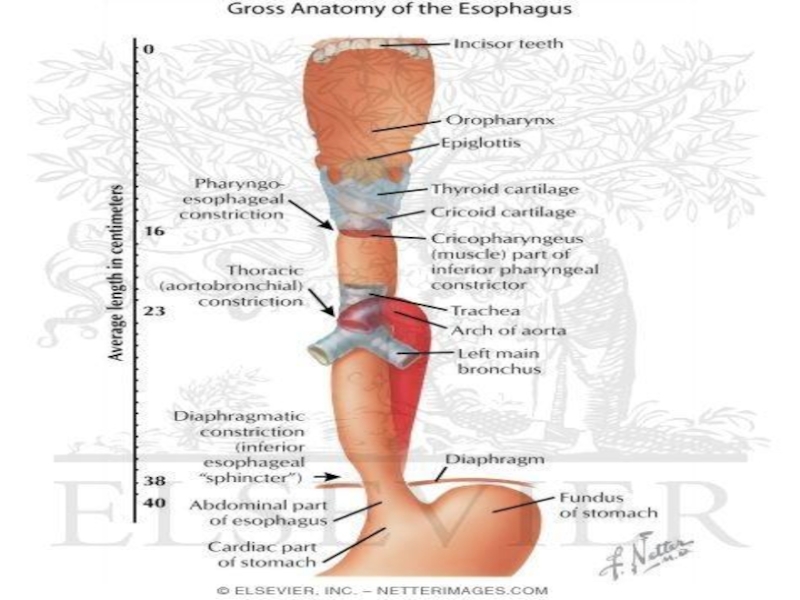
Слайд 11 Anatomy of oesophagus
The oesophagus commences at
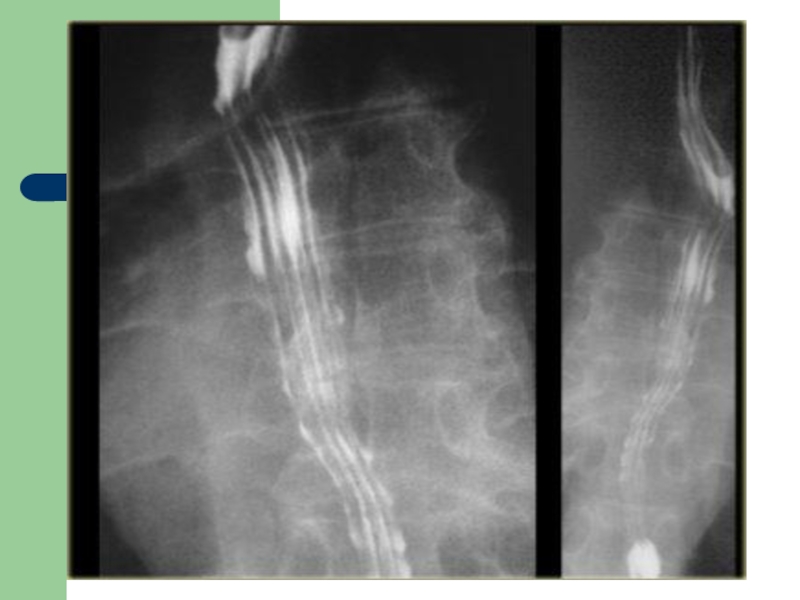
Слайд 12The oesophagus when full of barium should have a smooth outline.
Слайд 13The aortic arch gives a clearly visible impression on the left
Below the aortic impression there is often a smaller impression made by the left main bronchus.
The lower part of the oesophagus sweeps gently forward closely applied to the back of the left atrium and left ventricle.
Слайд 14Peristaltic waves can be observed during fluoroscopy. They move smoothly along
Слайд 19 Barium examinations of the stomach
It is a radiological study
Слайд 20 Indications:
suspected malignancies
gastric or duodenal obstructive lesions
gastric or duodenal ulcers
motility disorders
congenital anomalies
Слайд 21 Contraindications:
suspected gastro-duodenal perforation
large bowel
recent biopsy from GIT.
Слайд 22 Procedure
The patient
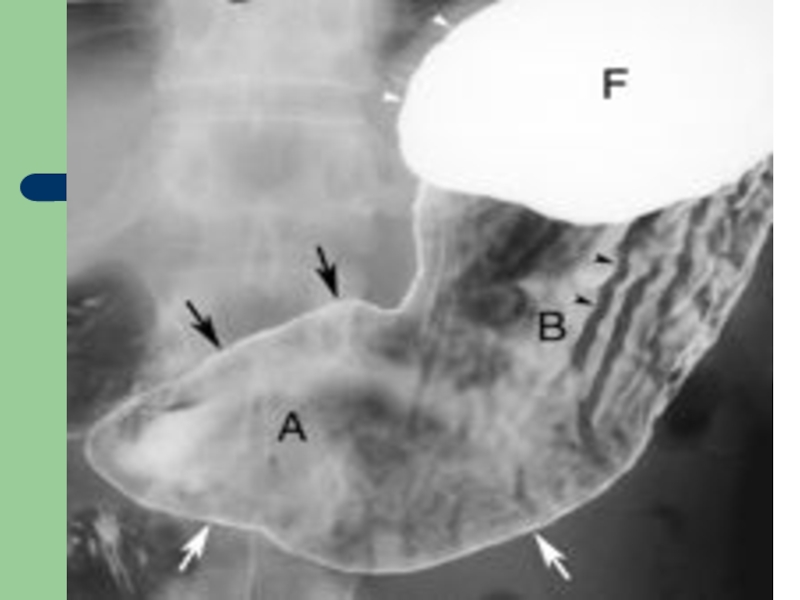
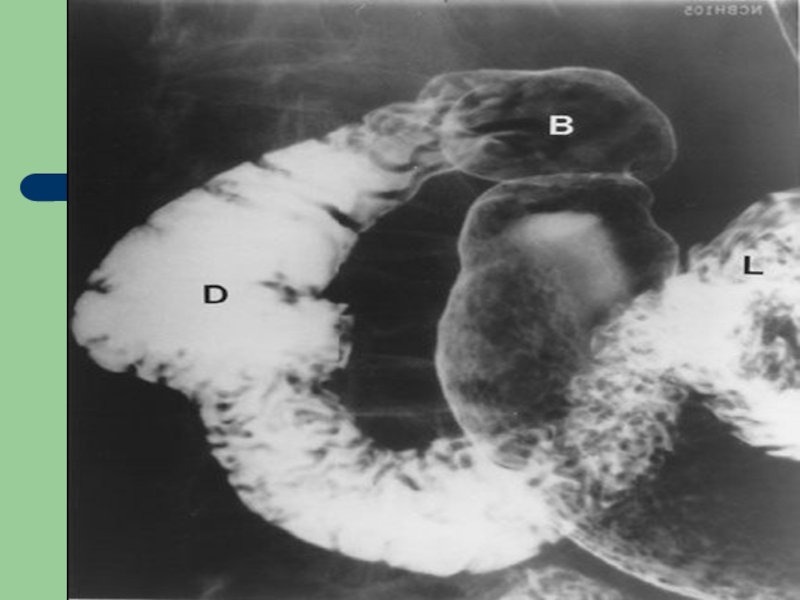
Слайд 23 Anatomy of the stomach and
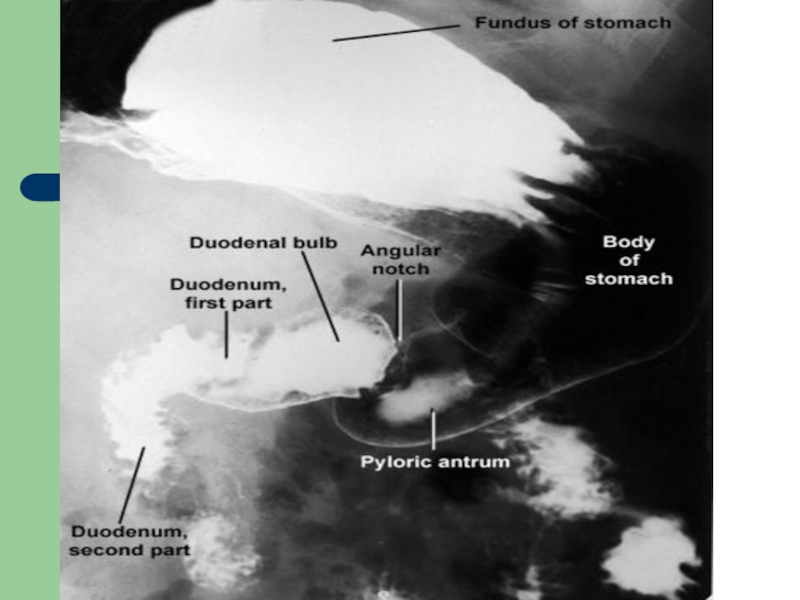
The stomach has a complex shape and varies considerably depending on the degree of distention.
Each part of the stomach and duodenum should be checked to ensure that no abnormal narrowing is present. A transient contraction wave must not be confused with a constant pathological narrowing.
Слайд 24The duodenal cap or bulb should be approximately triangular in shape.
The duodenum forms a loop around the heard of the pancreas to reach duodenojejunal flexure.
Слайд 28The outline of the lesser curve of the stomach is smooth
The duodenum is attached to the stomach at the narrow pylorus and consists of the duodenal bulb and the descending and ascending portions, although a horizontal segment is often added.
Слайд 29The duodenal cap or bulb should be approximately triangular in shape.
The duodenum forms a loop around the heard of the pancreas to reach duodenojejunal flexure.
Слайд 31 Causes of gastric displacement
enlargement of spleen causes forward and
enlargement of left kidney usually displaces the stomach forward
enlargement of left lobe of liver causes backward displacement of fundus of body
tumors of body and tail of pancreas push stomach forward
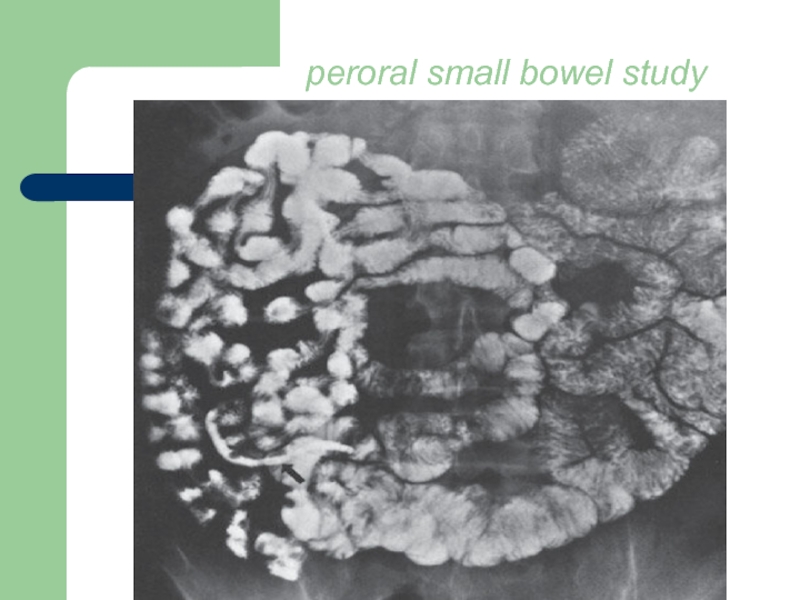
Слайд 32 Examinations of the Small Intestine
The
The following luminal contrast methods can be used to examine the small intestine:
* peroral small-bowel series;
* enteroclysis;
* various retrograde techniques (e.g., via an ileostomy).
Слайд 33However, the peroral small bowel study is probably the least effective
These include enteroclysis and CT or MR imaging with volume instillation by oral ingestion or via a tube, that is, CT or MR enterography or CT or MR enteroclysis.
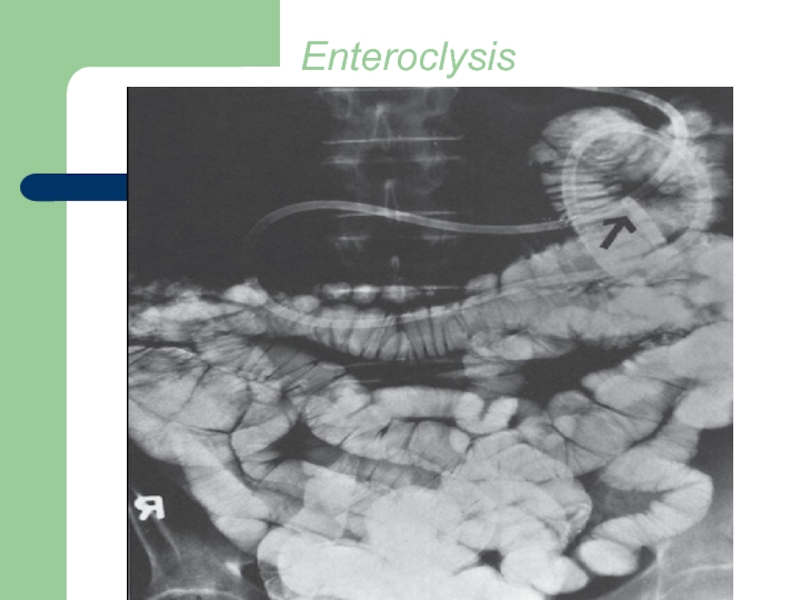
Слайд 34Enteroclysis is an intubated examination of the small intestine and can
Слайд 35Retrograde examination of the small bowel involves filling of the organ
Слайд 36 Anatomy of the small intestine
The length of the mesenteric
The jejunum comprises just over one-third of the length and the ileum the remainder, although no discrete transition is seen between the two segments. The normally distended small bowel has a caliber of 2 to 3 cm, being slightly larger more orad in the jejunum.
Слайд 37Depending on the degree of distention, the mucosal folds (valvulae conniventes)
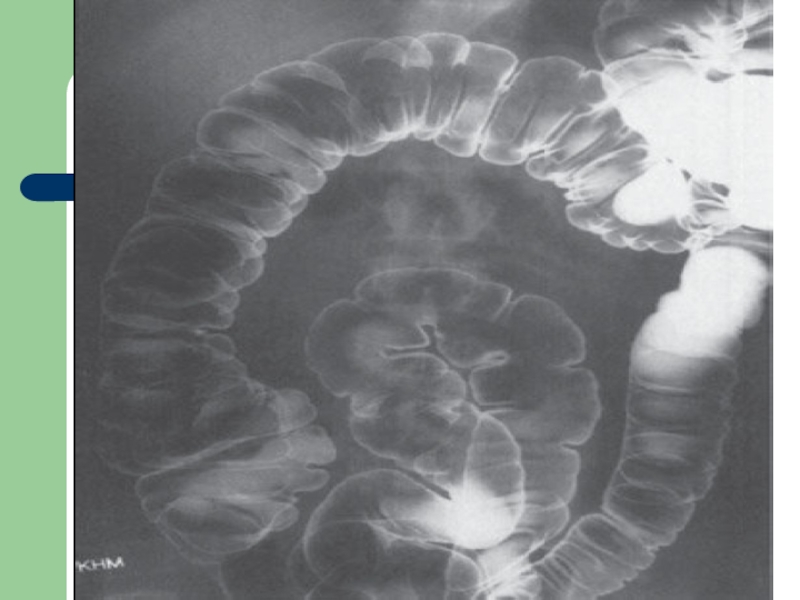
Слайд 40 Examinations of the Large Intestine
The radiographic examination of the
The colon can be evaluated by several techniques, which include single-contrast and double contrast barium enemas.
Слайд 41 The single-contrast method simply involves filling the colon with a
In both methods, large and small compression images of all segments of the colon are obtained.
Слайд 42 Indications
change in
hemorrhage
investigation of an abdominal mass
location of the site of large-bowel obstruction
Слайд 43 Contraindication
toxic megacolon
pseudomembranous colitis
full thickness bowel wall biopsy
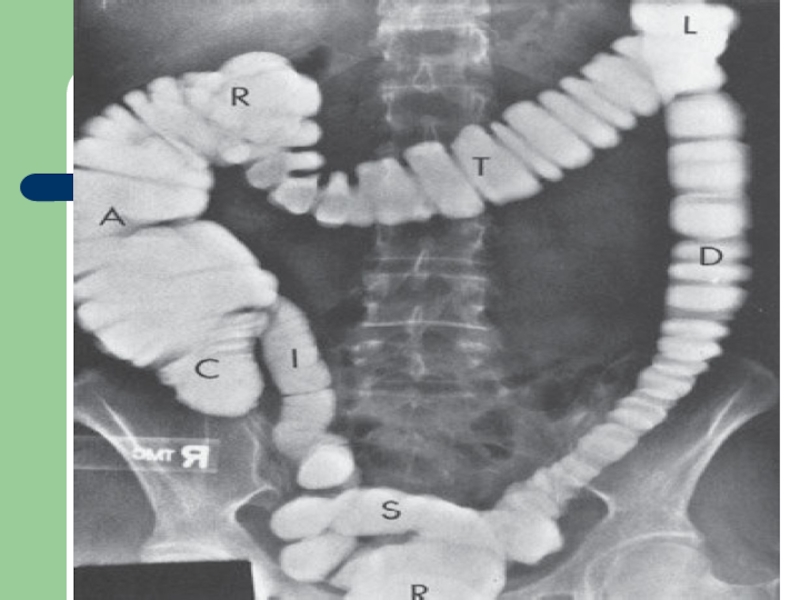
Слайд 44 Anatomy of the large intestine
The large intestine consists of
The length of the colon varies considerably, mainly because of differences in length and redundancy of the sigmoid colon and colic flexures. The colon also varies in caliber depending on location and luminal distention achieved.
Слайд 45 The mucosal surface has a smooth appearance, and the colonic
The ileocecal valve has a variety of appearances and may be large if infiltrated by fat.
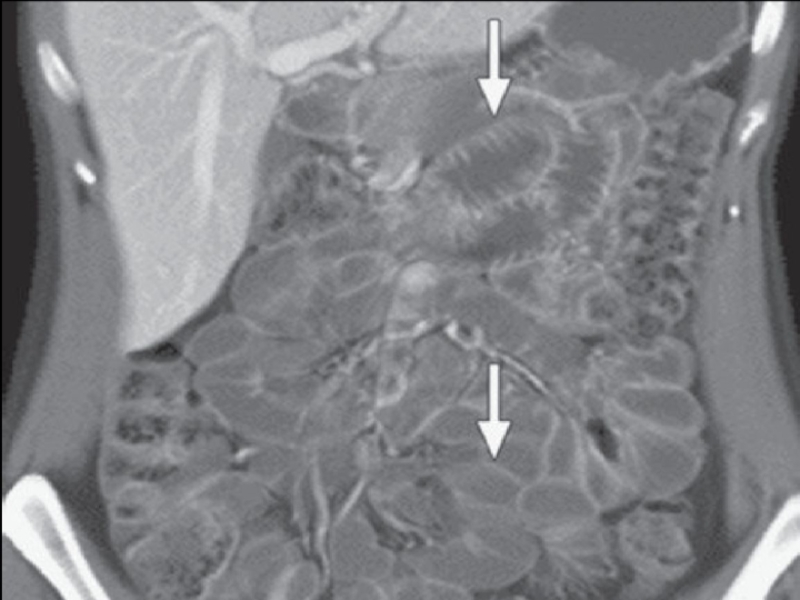
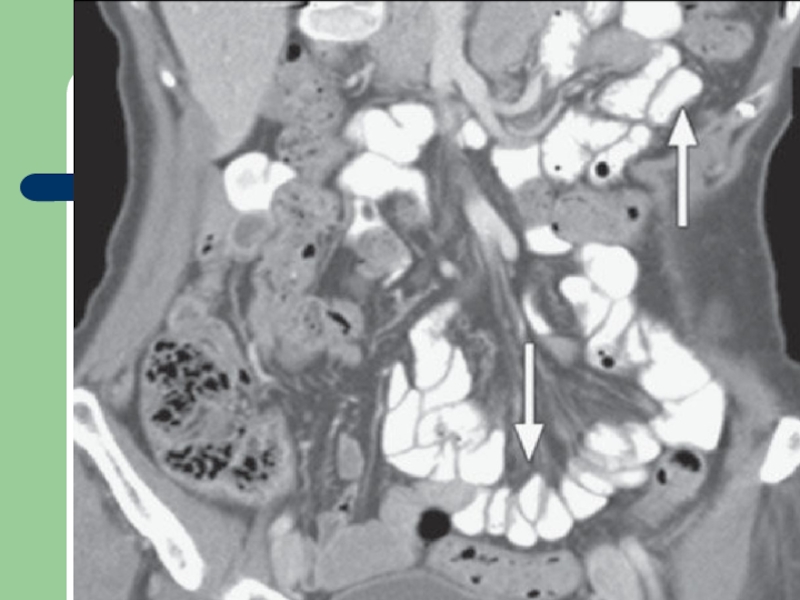
Слайд 48Computed Tomography (CT) Scanning
Uses in the gastrointestinal tract include:
Staging
Localizing abscess
As an aid to biopsy and drainage procedures
Слайд 52 Magnetic Resonance Imaging
MRI imaging of the hollow organs of
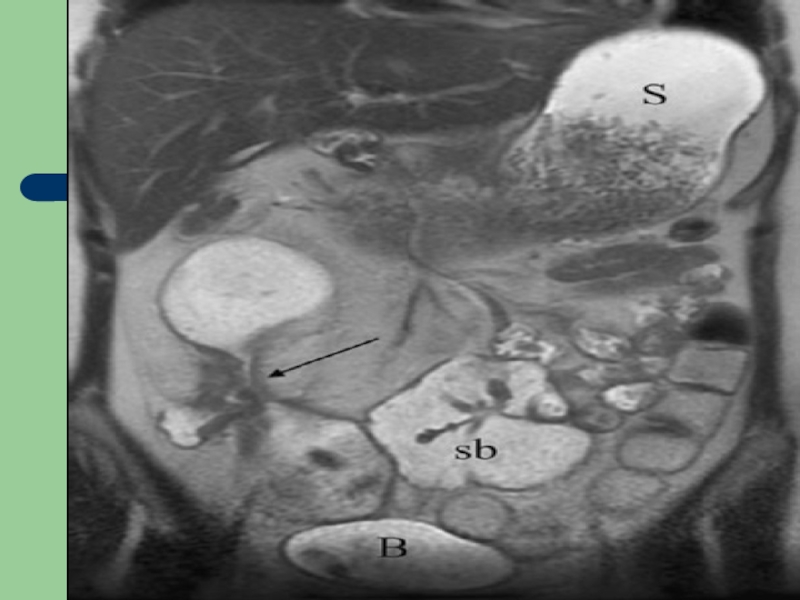
Слайд 53Also, with the use of luminal distention and intravenous agents of
Слайд 55 Isotope scanning
Technetium-99 pertechnetate
gastric emptying
gastrointestinal hemorrhage
detection of a Meckel’s diverticulum 9accumulation in ectopic gastric mucosa)
Слайд 56 Arteriography
Contrast injection into
Слайд 57 Patient Preparation
For an upper gastrointestinal
Слайд 58 Also, if patients are to have other imaging examinations that
Слайд 59Preparation for the barium enema is much more complicated, but must
Слайд 60The standard preparation includes
(1) a 24-hour clear liquid diet
(2)
(3) a saline cathartic (e.g., magnesium citrate) in the afternoon;
(4) an irritant cathartic (e.g., castor oil) in the early evening; and
(5) a tap-water cleansing enema the morning of the radiographic examination (30 to 60 minutes before the barium enema).
Слайд 61 ACHALASIA
Achalasia
Слайд 62 Unlike strictures of the oesophagus, which initially
The earliest changes are characterized by defective distal peristalsis associated with a slight narrowing at the gastro-oesophageal junction.
As the disease progresses, the characteristic ‘bird beak’ or ‘rat’s tail’ appearance of the gastro-oesophageal junction is observed.
Слайд 63Often, by this stage, the body of the oesophagus has become
With severe achalasia there is substantial dilatation of the oesophagus that contains a huge residue of food and fluid debris.
Absent gastric fundal air bubble
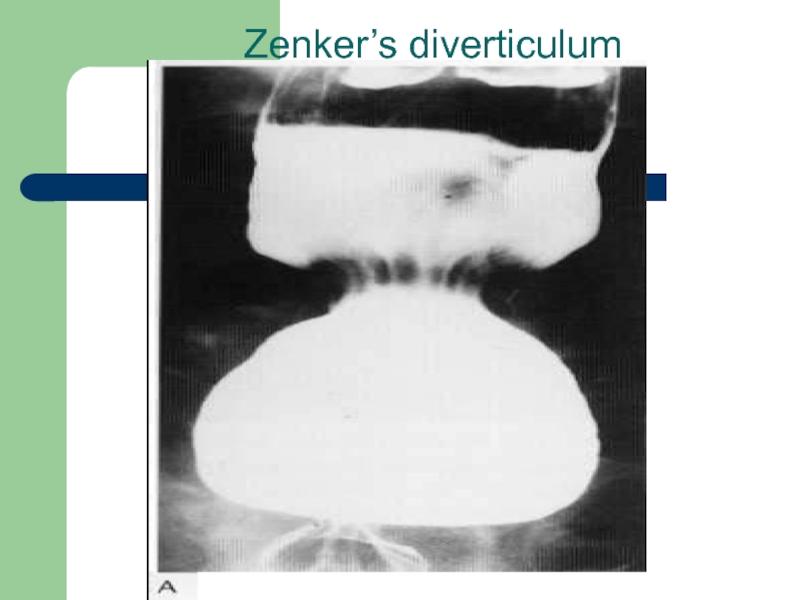
Слайд 72
Esophageal Diverticula
In the lower cervical region, sometimes a pharyngeal diverticulum (Zenker’s diverticulum) projects posteriorly. Food can be caught in this, causing dysphagia. It due to impaired crico-pharengeal relaxation between the oblique and horizontal fibres of inferior constrictor muscle. The mucosa prolapses out through the muscles.
Слайд 73 Radiological sings:
widened retro-tracheal soft tissue
pulsion type of diverticulum
Слайд 75 Tractional diverticulae:
secondary to fibrosis
the wall of the diverticula contains all the layers
Pulsion diverticula:
the wall composed of only mucosa and submucosa herniating the muscularis
usually it is acquired condition
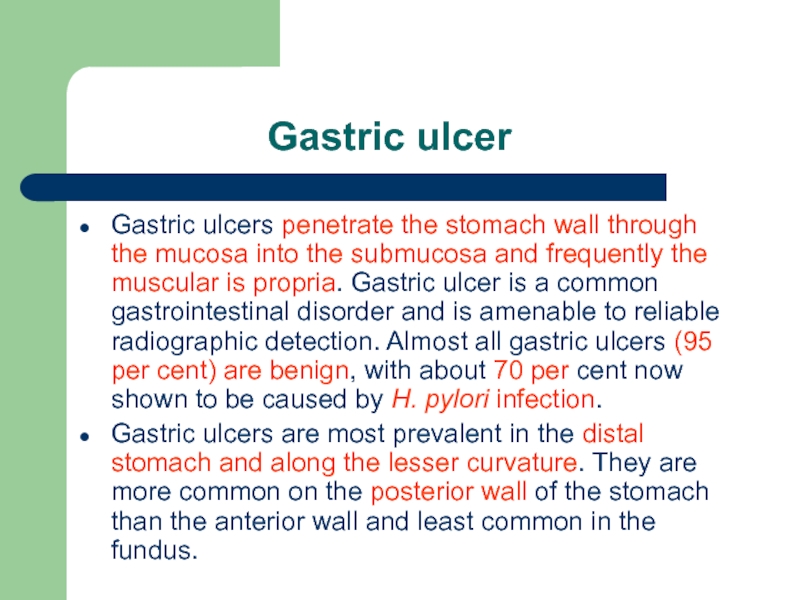
Слайд 79 Gastric ulcer
Gastric ulcers penetrate the stomach wall through the mucosa into the submucosa and frequently the muscular is propria. Gastric ulcer is a common gastrointestinal disorder and is amenable to reliable radiographic detection. Almost all gastric ulcers (95 per cent) are benign, with about 70 per cent now shown to be caused by H. pylori infection.
Gastric ulcers are most prevalent in the distal stomach and along the lesser curvature. They are more common on the posterior wall of the stomach than the anterior wall and least common in the fundus.
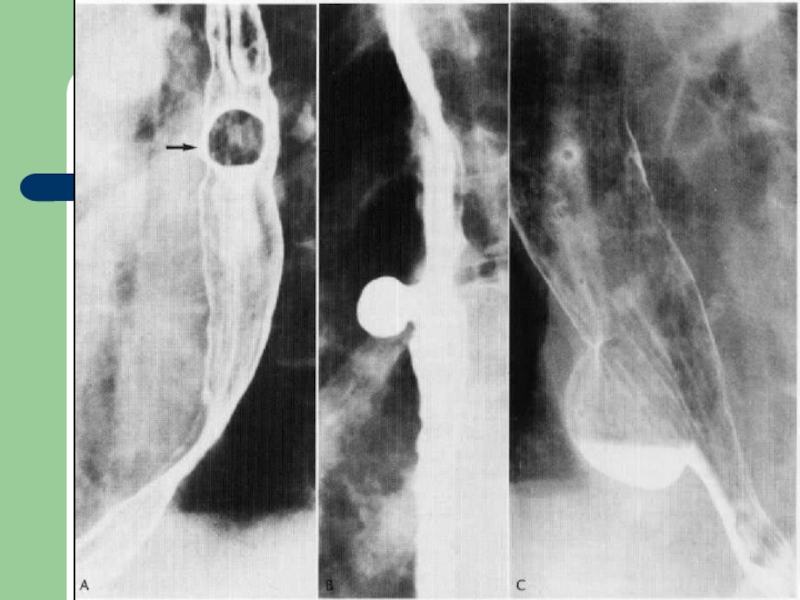
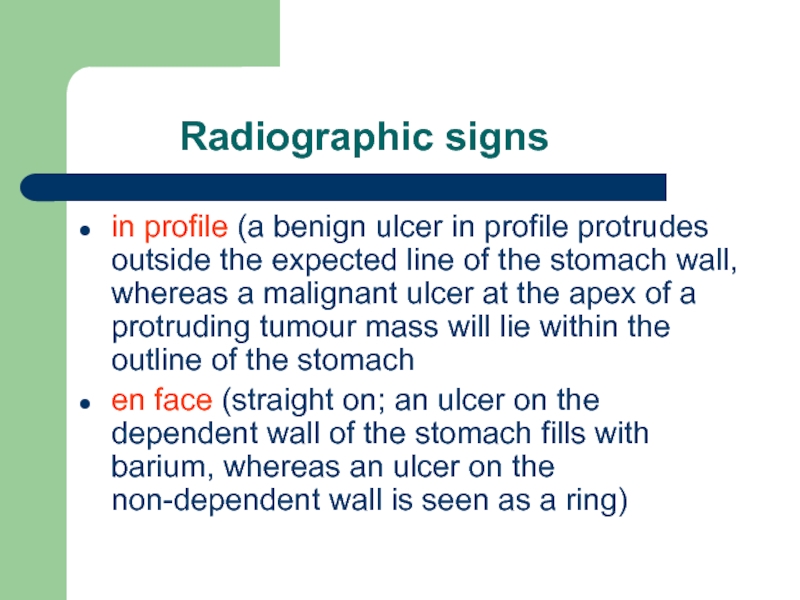
Слайд 80 Radiographic signs
in profile (a benign
en face (straight on; an ulcer on the dependent wall of the stomach fills with barium, whereas an ulcer on the non-dependent wall is seen as a ring)
Слайд 81The en face radiographic signs of gastric ulcers are best seen
collection of barium on the dependent wall
most benign ulcers are round or oval
some may have tear-drop or linear contour
Слайд 82it may be demonstrated as a ‘ring’ shadow, with barium coating
edema is often seen surrounding the ulcer crater causing a circular filling defect
radiating folds seen in healing ulcers should be smooth and symmetric and continue to the edge of the crater
Слайд 83 The in profile radiographic signs of
‘ulcer niche’, projects beyond the lumen of the stomach
sometimes a pencil-thin line of lucency is present crossing the base of the ulcer
more often there is a thicker (2–4 mm) smooth rim of lucency at the base of the ulcer termed the ulcer collar
oedema associated with an ulcer it forms an ulcer mound
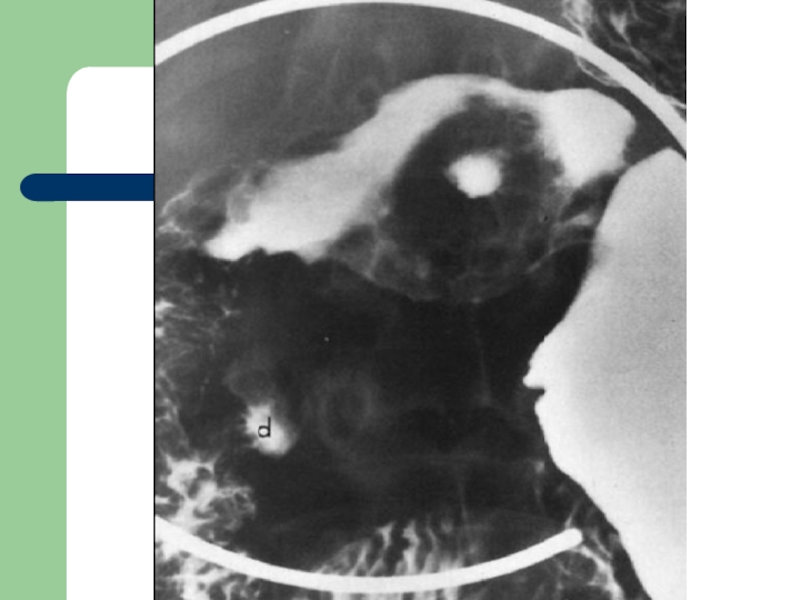
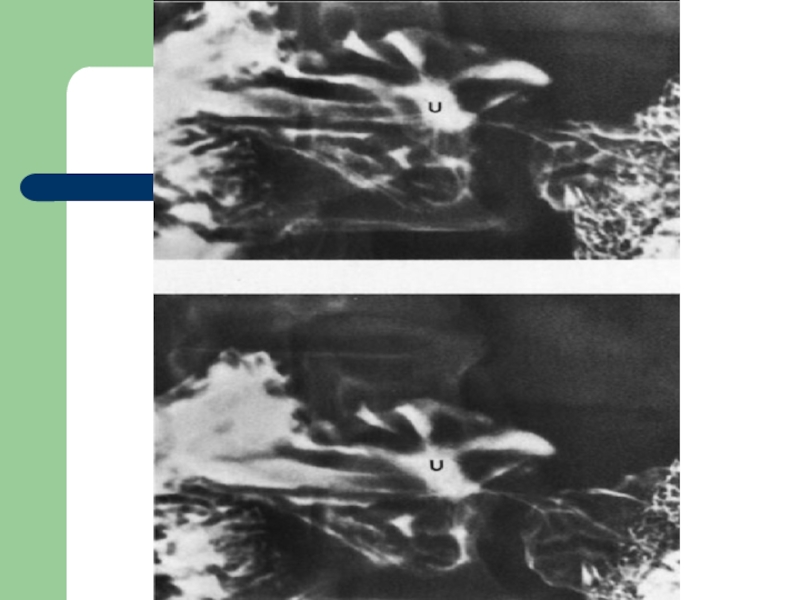
Слайд 84 Duodenal ulcer
Radiological signs:
deformity
barium in the crater may appear a niche projection from the general contour of the cap, if it is seen tangentially
if it is seen en face after compression, it appears as as isolated spot, the surrounding edema causing a translucent area
if the ulcer is chronic, the folds may converge towards it giving a stellate appearance
Слайд 95
Gastritis is a descriptive term with sometimes conflicting pathological, endoscopic and radiographic definitions.
Слайд 96 The most common findings are
thick (>5 mm) folds with
erosions, while less commonly seen, are a frequent sign of H. pylori gastritis
antral narrowing
inflammatory polyps
The radiological findings are similar to endoscopic findings.
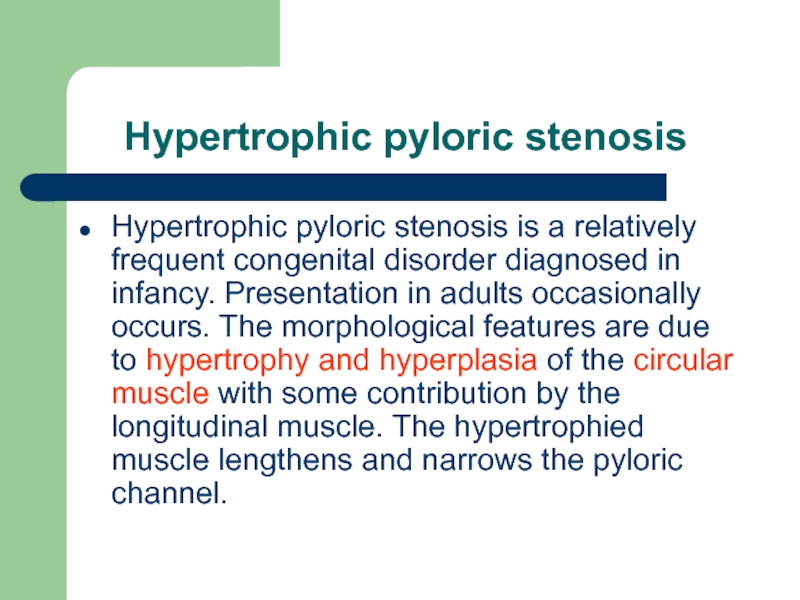
Слайд 100 Hypertrophic pyloric stenosis
Hypertrophic pyloric stenosis is a relatively
Слайд 101 Radiographically:
shoulder sign
beak sign – this occurs where the barium column extending into the narrowed pyloric canal is cut off similar to a beak
double track – parallel mucosal folds extending through the elongated pyloric canal
string sign – a thin streak of barium may be seen extending between the pyloric antrum and the duodenal cap
Слайд 102 USG is investigation of choice and
pyloric canal length>16 mm
transverse pyloric diameter >11 mm
pyloric canal does not open, therefore, decreased gastric emptying
increased gastric peristalsis proxomaly
Слайд 105
Hyperplastic polyps are by far the most common benign neoplasm of the stomach. These polyps are not considered to have malignant potential, but do occur more commonly in patients who have other risk factors for developing gastric malignancy, such as atrophic gastritis, and in patients with gastric resections and bile reflux gastritis.
Слайд 106 Radiographically:
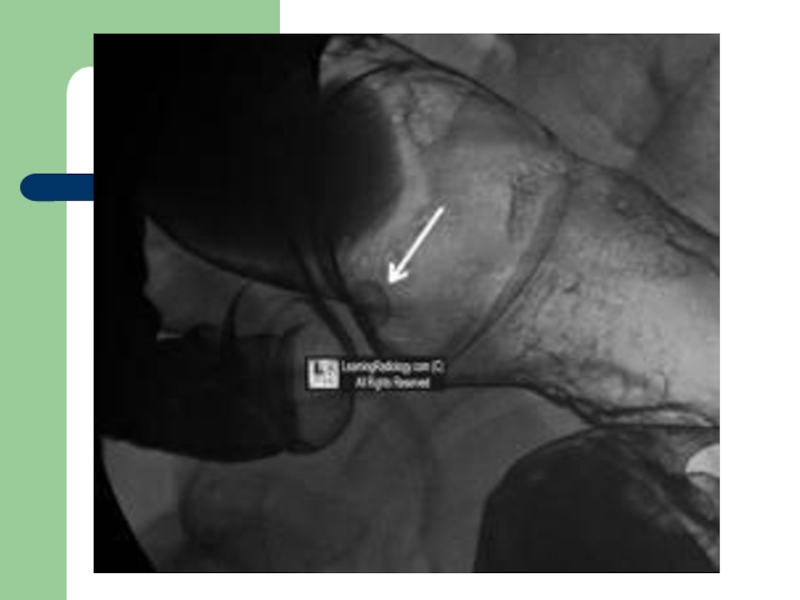
round filling defect
smooth sessile
they are usually multiple and of uniform size (5–10 mm)
they are most common in the fundus and body of the
Слайд 112The most common presentations on the double-contrast upper gastrointestinal examination are
a filling defect
a shallow ulceration with converging folds
the folds are often thickened, irregular or nodular in shape and may have a club-like appearance
the folds may appear to converge; this appearance is due to a fibrous reaction induced by many of these tumours
when the antrum is primarily involved by tumour, it may be severely narrowed or obstructed
rigidity of the gastric wall and decreased peristalsis indicate submucosa spread of the tumor
Слайд 113A primary neoplastic ulcer is often indistinguishable from a simple ulcer.
Filling
Hour glass stomach due to annular constricting type of growth.
Narrow irregular gastric outline due to submucous, diffuse, infiltrating neoplasm.