- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Ecg interpretations. How to analyze a rhythm. Normal sinus rhythm. Heart arrhythmias. Diagnosing a myocardial infarction презентация
Содержание
- 1. Ecg interpretations. How to analyze a rhythm. Normal sinus rhythm. Heart arrhythmias. Diagnosing a myocardial infarction
- 2. Course Objectives To recognize the normal rhythm
- 3. Learning Modules ECG Basics How to Analyze
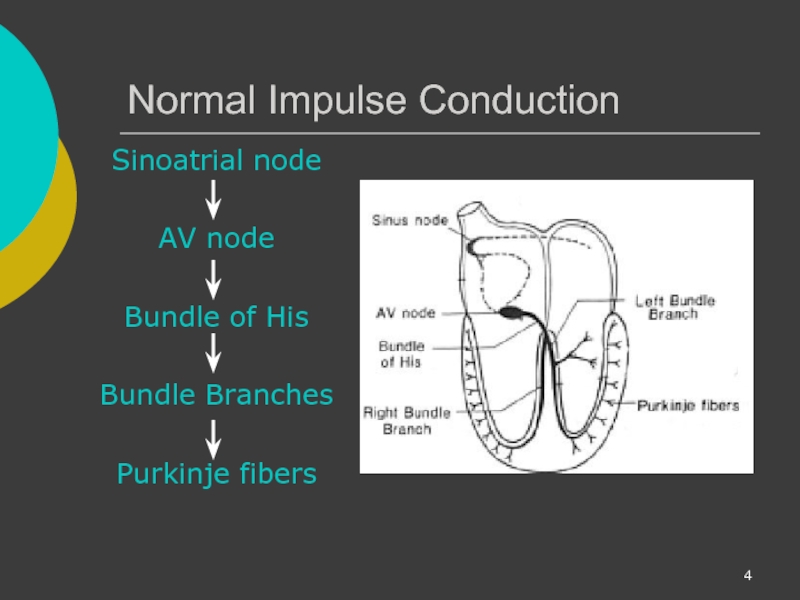
- 4. Normal Impulse Conduction Sinoatrial node AV
- 5. Impulse Conduction & the ECG Sinoatrial node
- 6. The “PQRST” P wave - Atrial
- 7. The PR Interval Atrial depolarization +
- 8. Pacemakers of the Heart SA Node -
- 9. The ECG Paper Horizontally One small box
- 10. The ECG Paper (cont) Every 3
- 11. ECG Rhythm Interpretation Really Very Easy How to Analyze a Rhythm
- 12. Rhythm Analysis Step 1: Calculate rate.
- 13. Step 1: Calculate Rate Option
- 14. Step 1: Calculate Rate
- 15. Step 1: Calculate Rate
- 16. Step 2: Determine regularity Look
- 17. Step 3: Assess the P waves
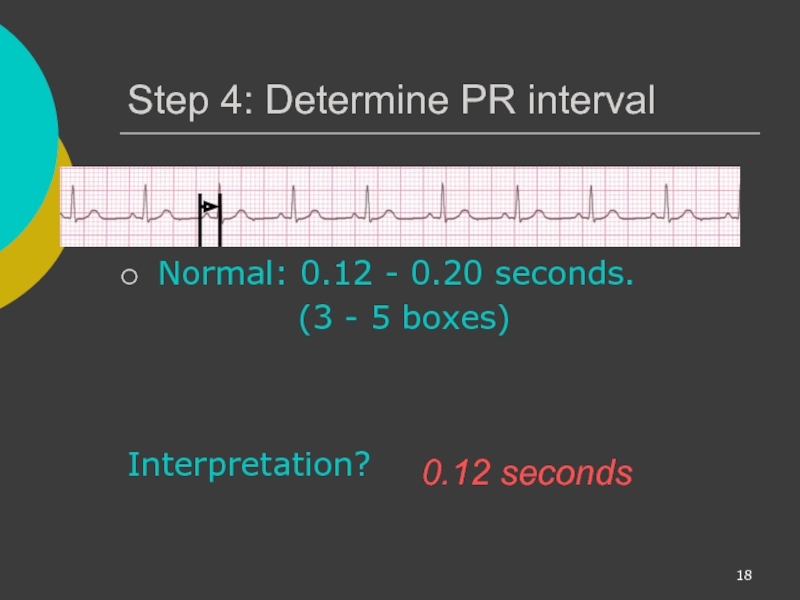
- 18. Step 4: Determine PR interval
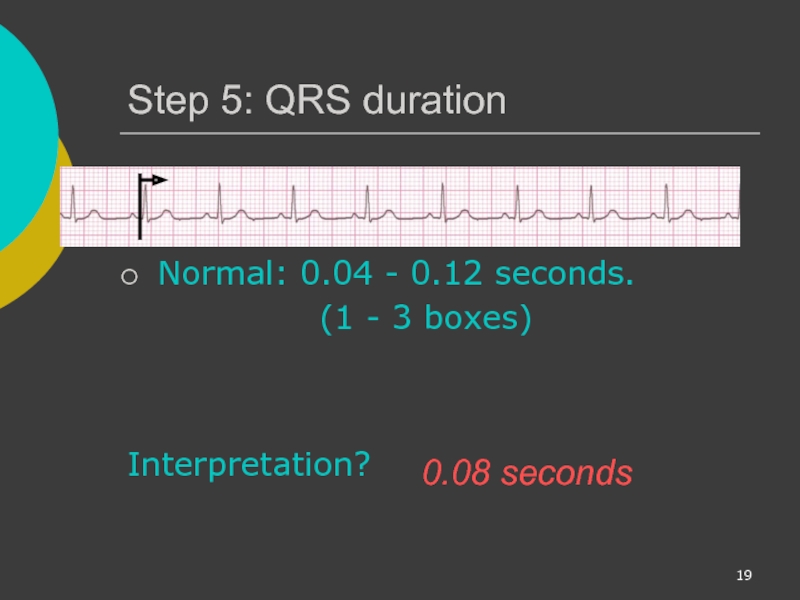
- 19. Step 5: QRS duration Normal:
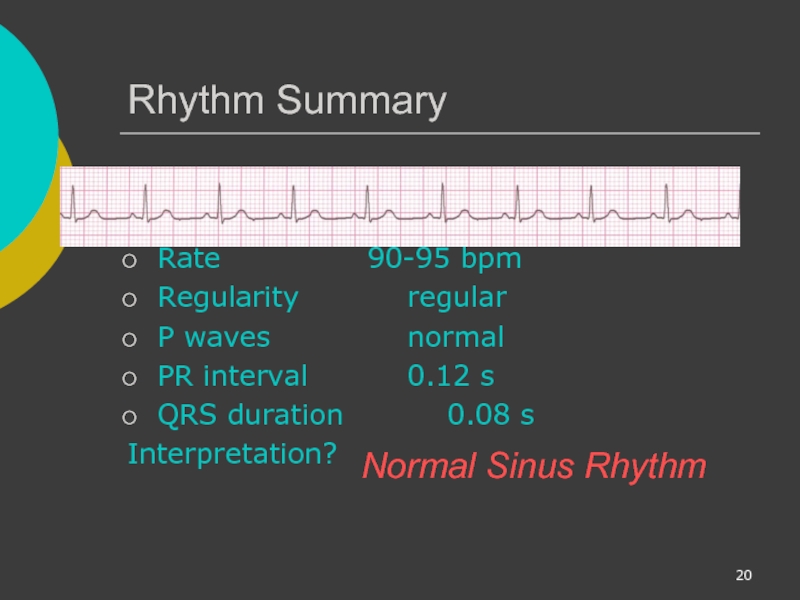
- 20. Rhythm Summary Rate 90-95 bpm Regularity regular
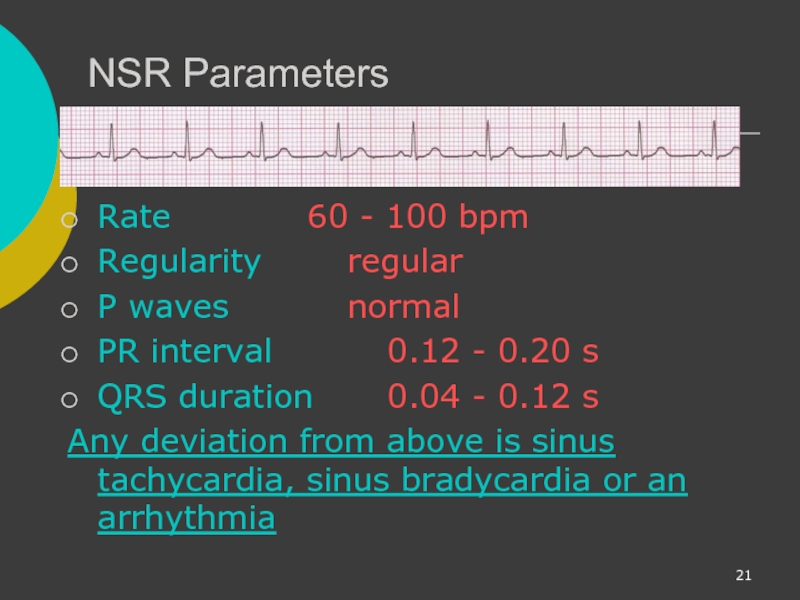
- 21. NSR Parameters Rate 60 - 100 bpm Regularity regular
- 22. Arrhythmia Formation Arrhythmias can arise from problems
- 23. SA Node Problems The SA Node can:
- 24. Atrial Cell Problems Atrial cells can: fire
- 25. Atrial Cell Problems Atrial cells can also:
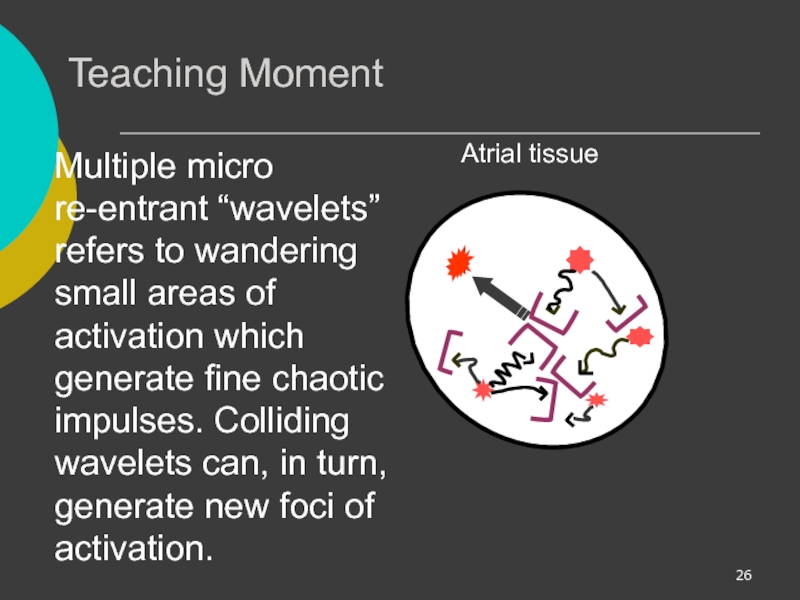
- 26. Teaching Moment Multiple micro re-entrant “wavelets” refers
- 27. AV Junctional Problems The AV junction can:
- 28. Ventricular Cell Problems Ventricular cells can: fire
- 29. Arrhythmias Sinus Rhythms Premature Beats Supraventricular Arrhythmias Ventricular Arrhythmias AV Junctional Blocks
- 30. Sinus Rhythms Sinus Bradycardia Sinus Tachycardia Sinus Arrest Normal Sinus Rhythm
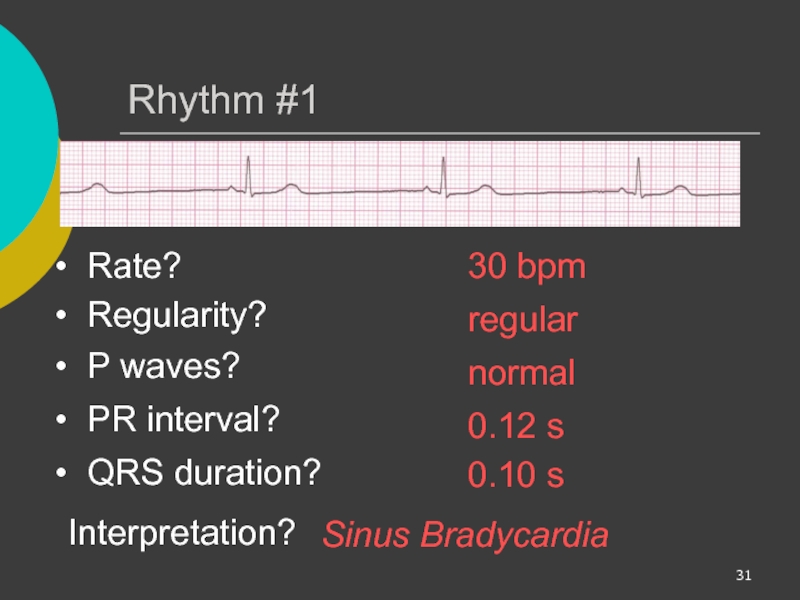
- 31. Rhythm #1 30 bpm Rate?
- 32. Sinus Bradycardia Deviation from NSR - Rate < 60 bpm
- 33. Sinus Bradycardia Etiology: SA node is
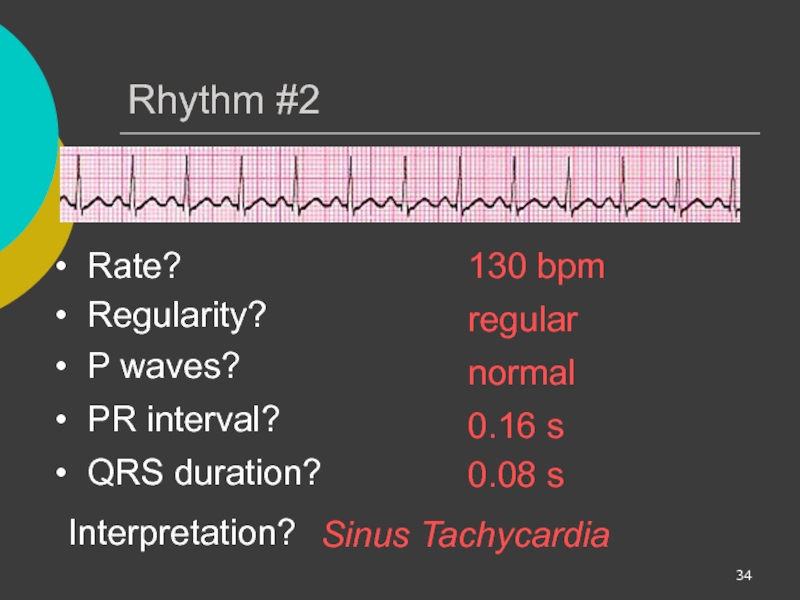
- 34. Rhythm #2 130 bpm Rate?
- 35. Sinus Tachycardia Deviation from NSR - Rate > 100 bpm
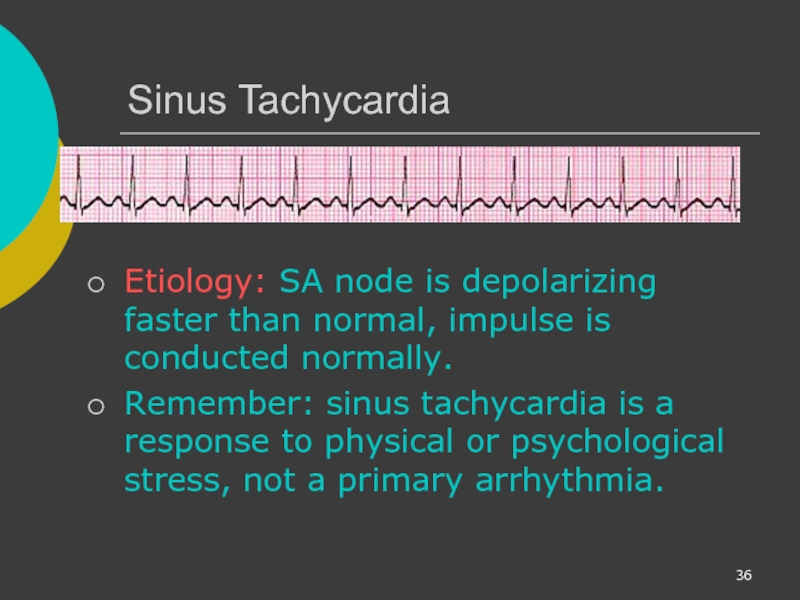
- 36. Sinus Tachycardia Etiology: SA node is
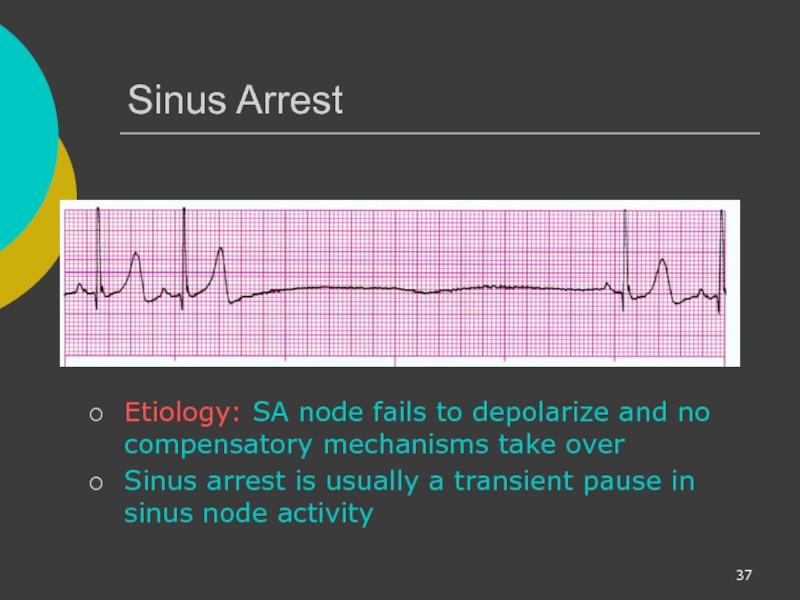
- 37. Sinus Arrest Etiology:
- 38. Premature Beats Premature Atrial Contractions (PACs) Premature Ventricular Contractions (PVCs)
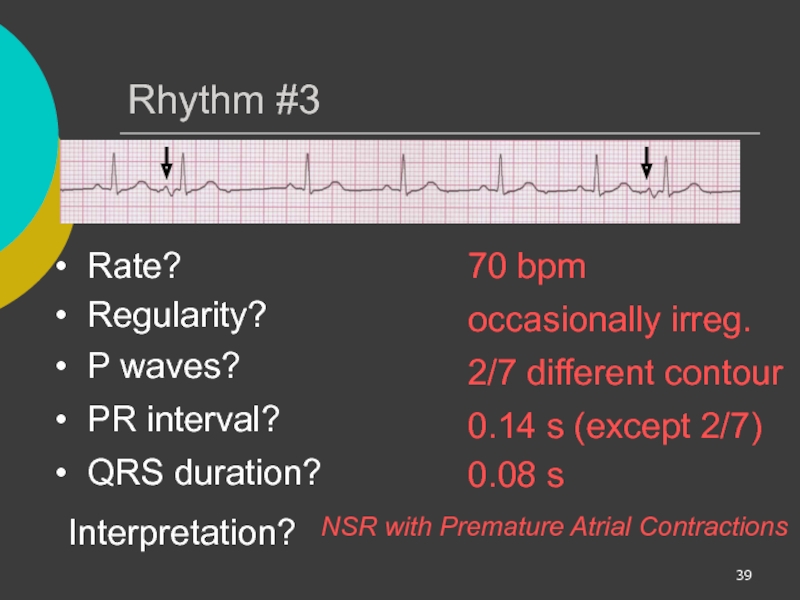
- 39. Rhythm #3 70 bpm Rate?
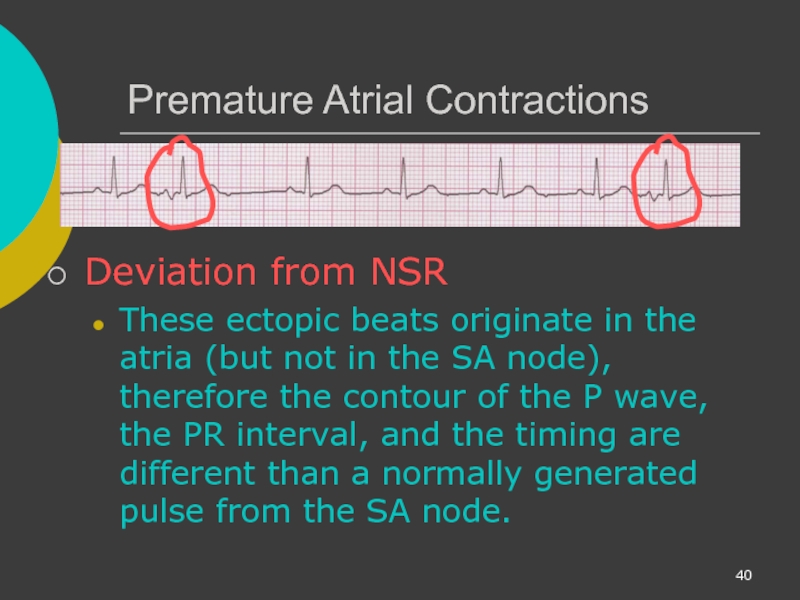
- 40. Premature Atrial Contractions Deviation from NSR
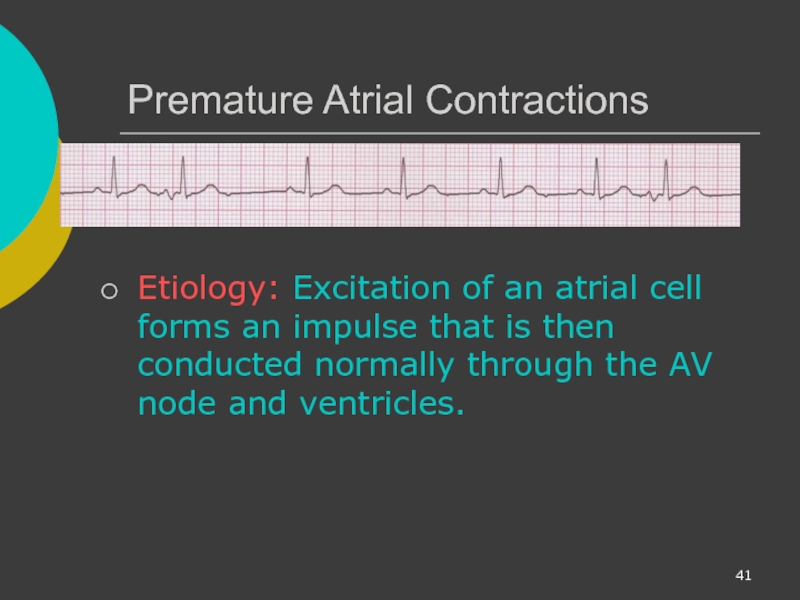
- 41. Premature Atrial Contractions Etiology: Excitation of
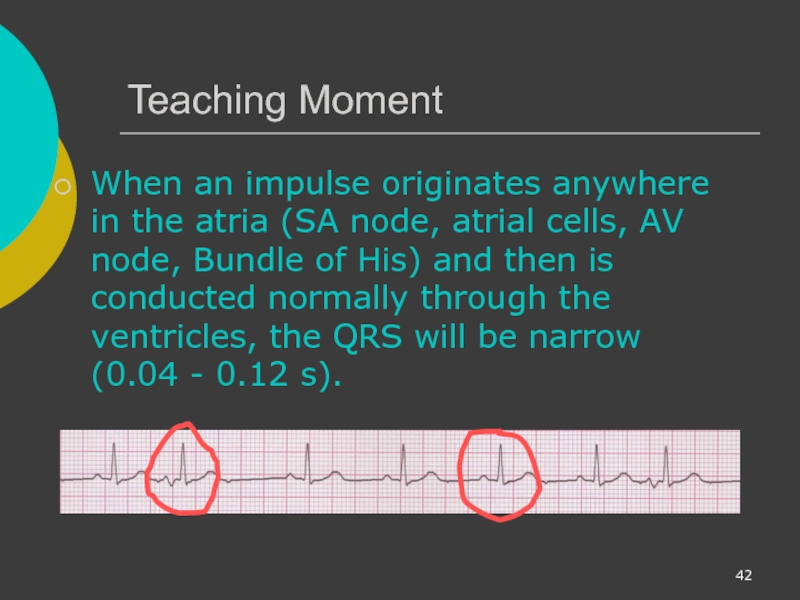
- 42. Teaching Moment When an impulse originates anywhere
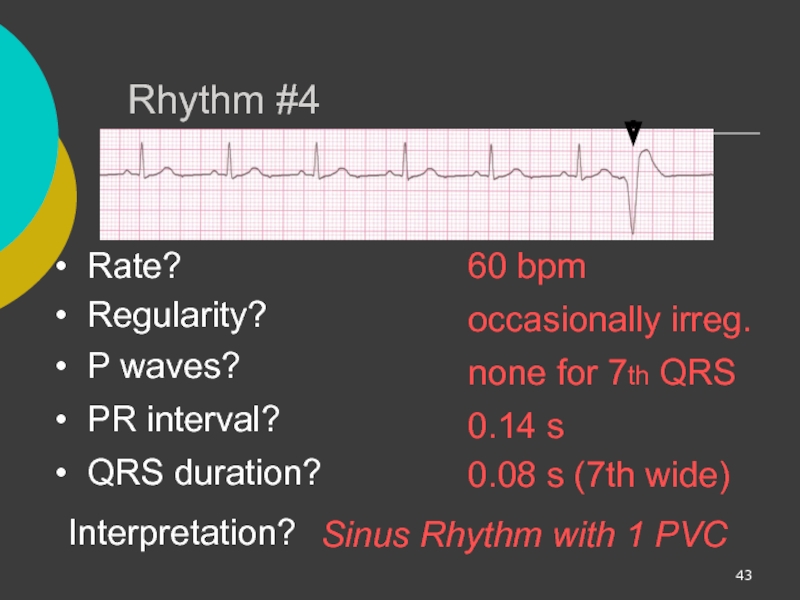
- 43. Rhythm #4 60 bpm Rate?
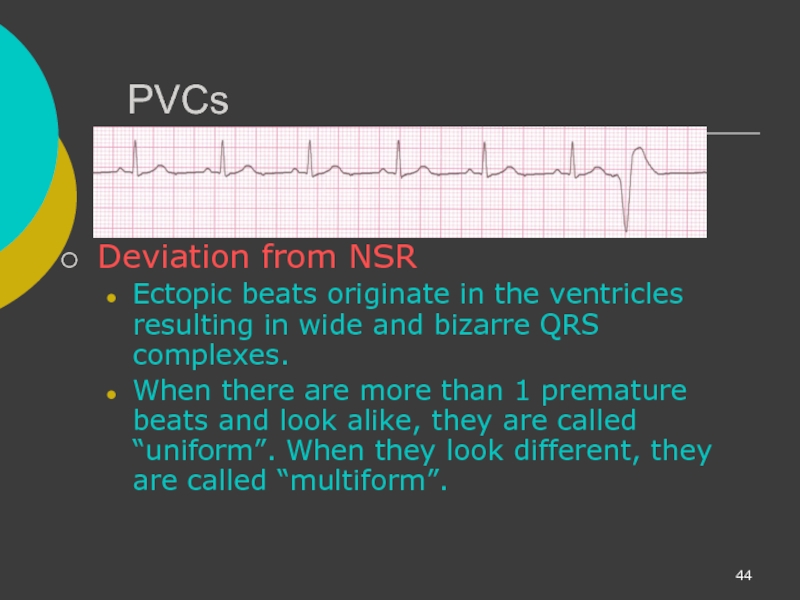
- 44. PVCs Deviation from NSR Ectopic beats
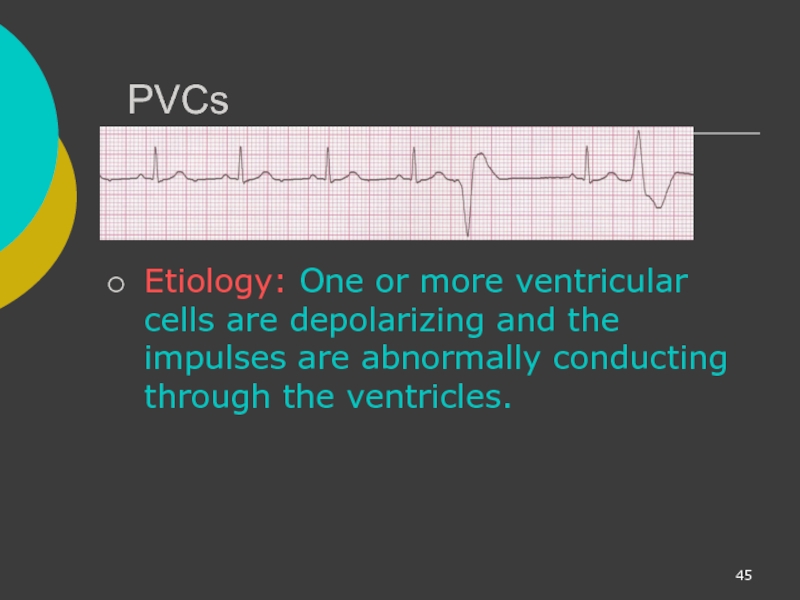
- 45. PVCs Etiology: One or more ventricular
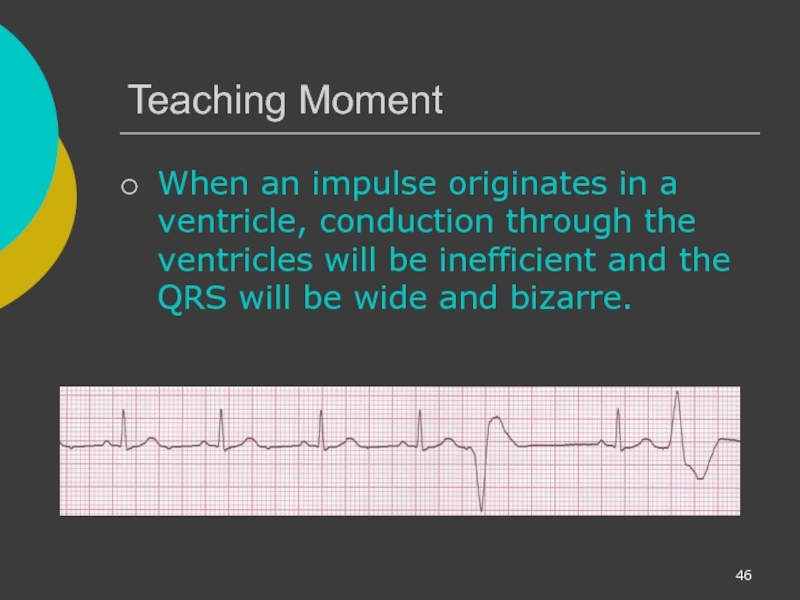
- 46. Teaching Moment When an impulse originates in
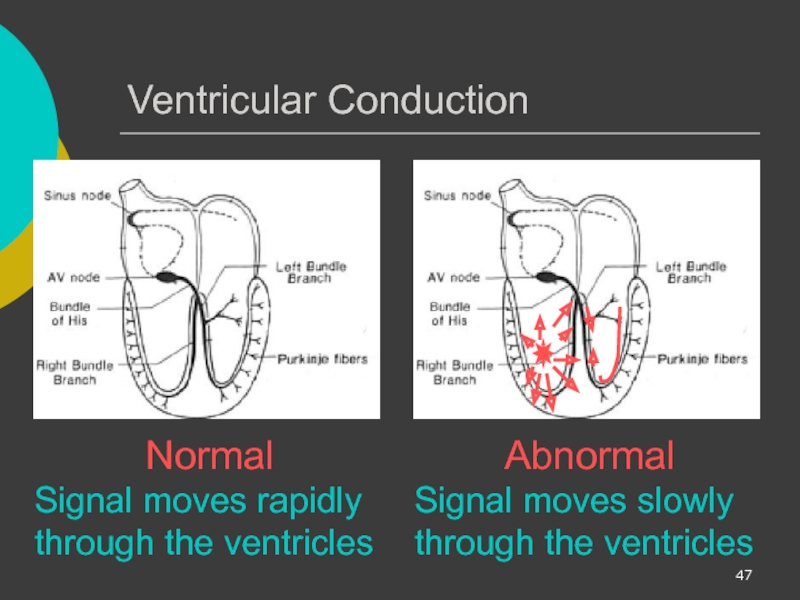
- 47. Ventricular Conduction Normal Signal moves rapidly through
- 48. Supraventricular Arrhythmias Atrial Fibrillation Atrial Flutter Paroxysmal Supra Ventricular Tachycardia (PSVT)
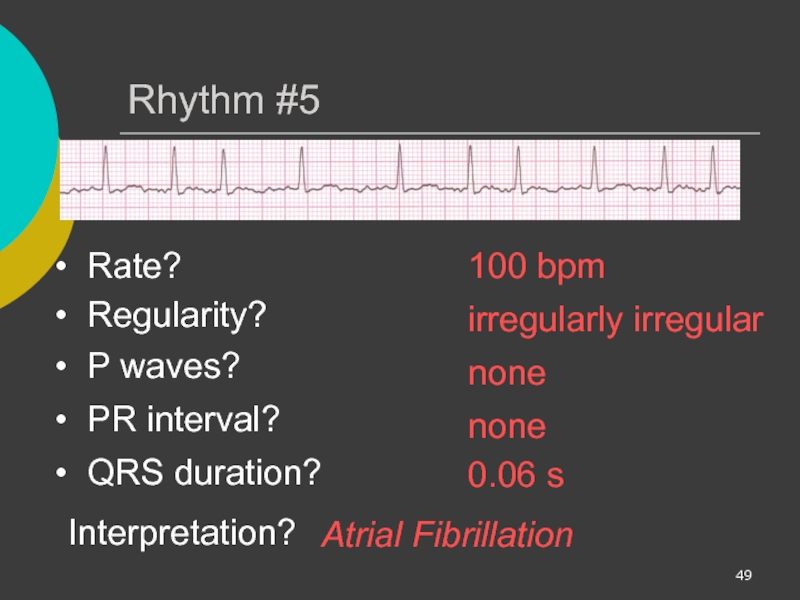
- 49. Rhythm #5 100 bpm Rate?
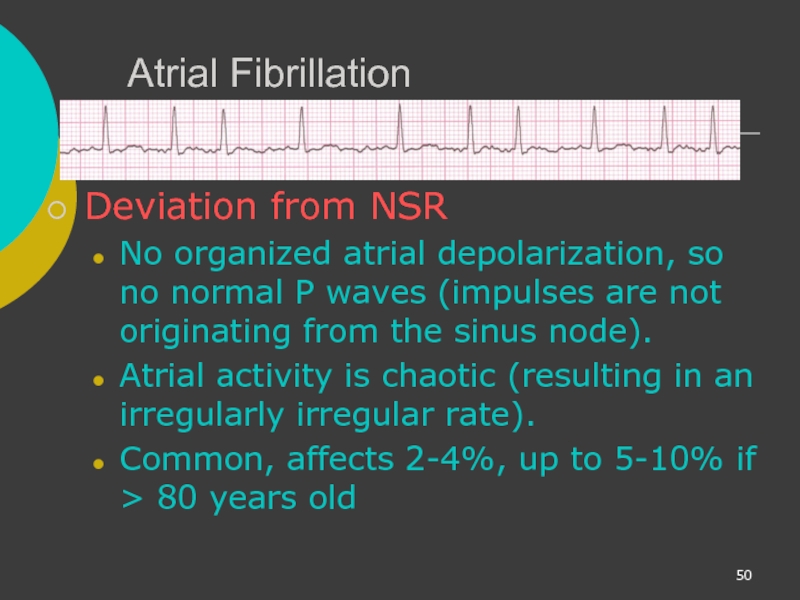
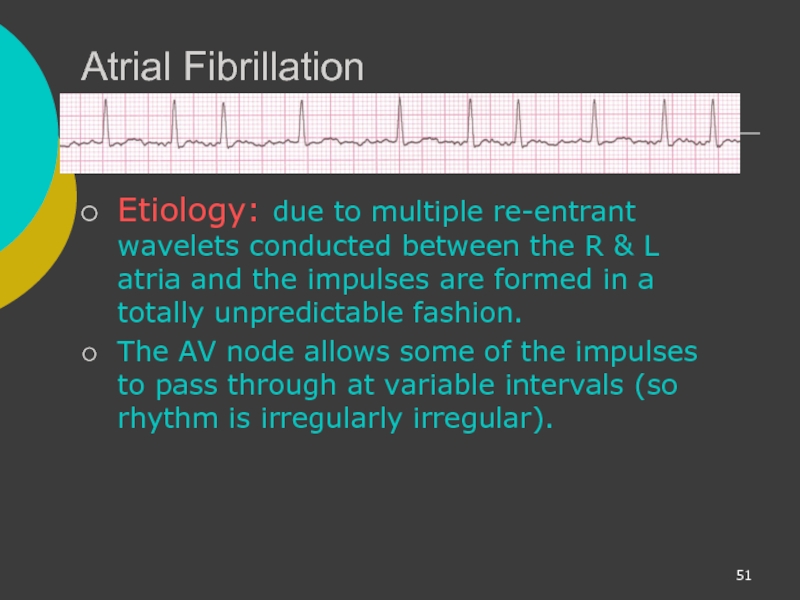
- 50. Atrial Fibrillation Deviation from NSR No organized
- 51. Atrial Fibrillation Etiology: due to multiple re-entrant
- 52. Rhythm #6 70 bpm Rate?
- 53. Atrial Flutter Deviation from NSR No
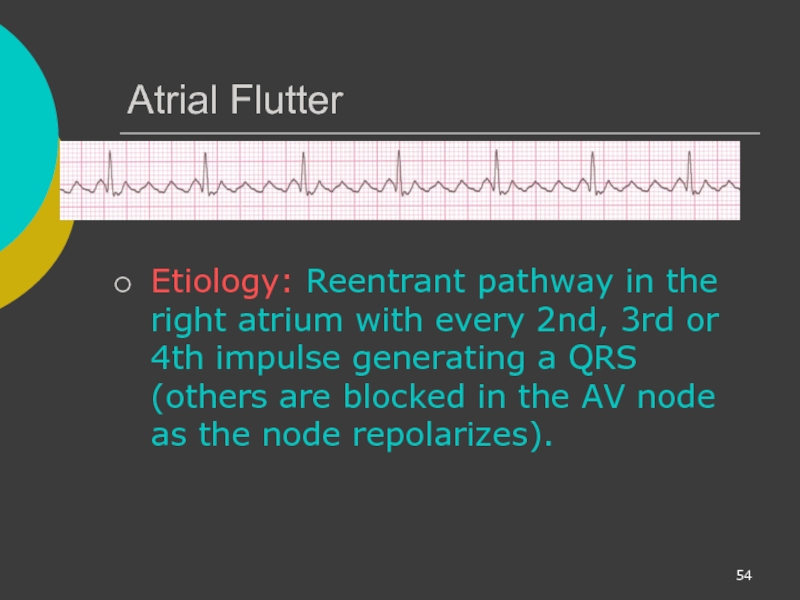
- 54. Atrial Flutter Etiology: Reentrant pathway in
- 55. Rhythm #7 74 ?148 bpm Rate?
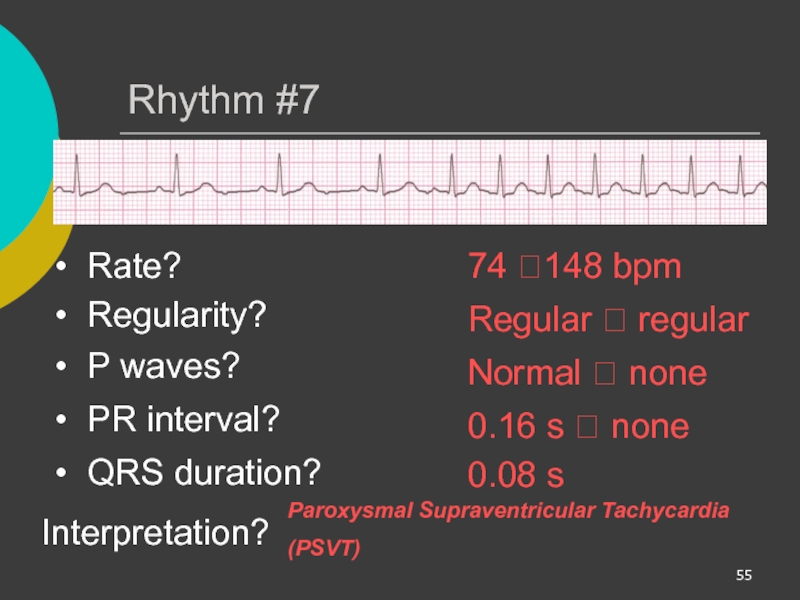
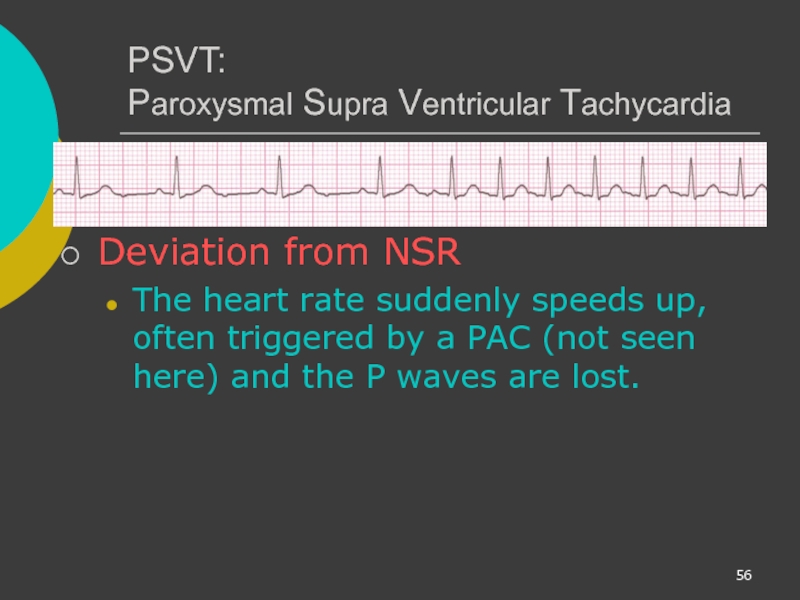
- 56. PSVT: Paroxysmal Supra Ventricular Tachycardia Deviation
- 57. AV Nodal Blocks 1st Degree AV Block
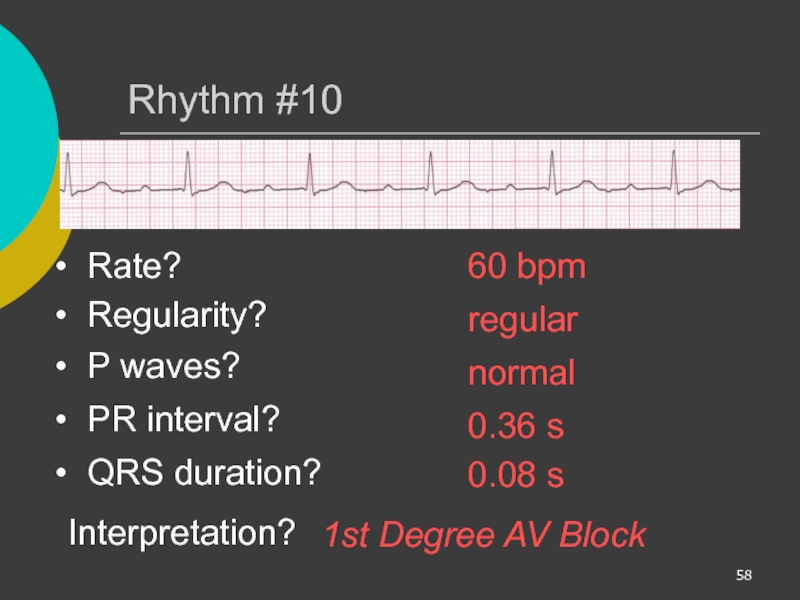
- 58. Rhythm #10 60 bpm Rate?
- 59. 1st Degree AV Block Deviation from NSR PR Interval > 0.20 s
- 60. 1st Degree AV Block Etiology: Prolonged
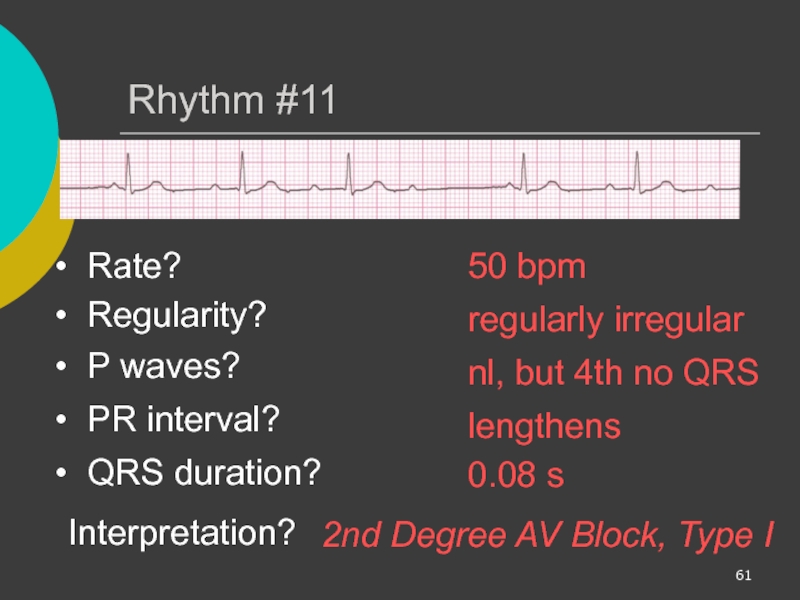
- 61. Rhythm #11 50 bpm Rate?
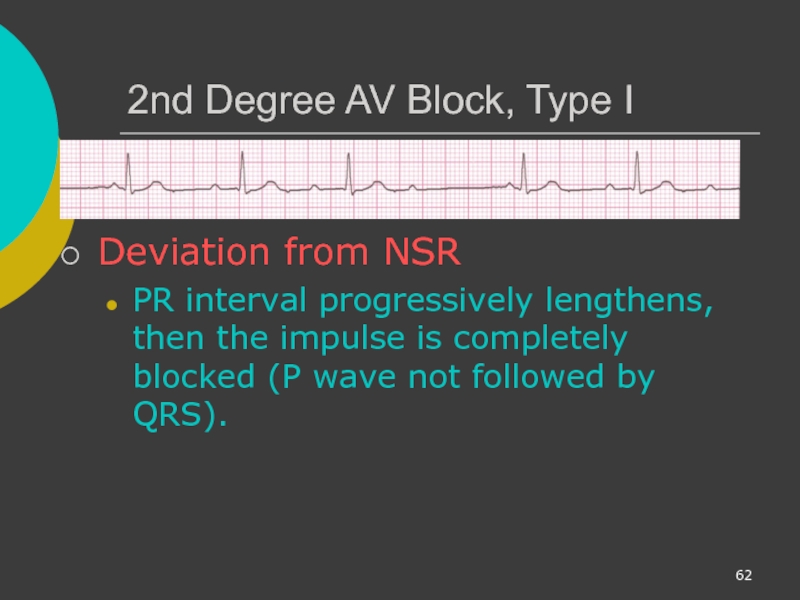
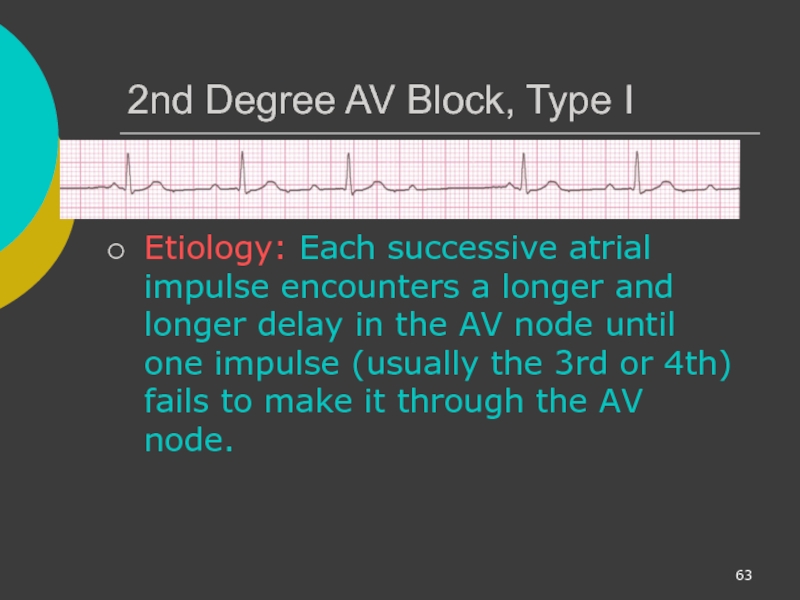
- 62. 2nd Degree AV Block, Type I
- 63. 2nd Degree AV Block, Type I
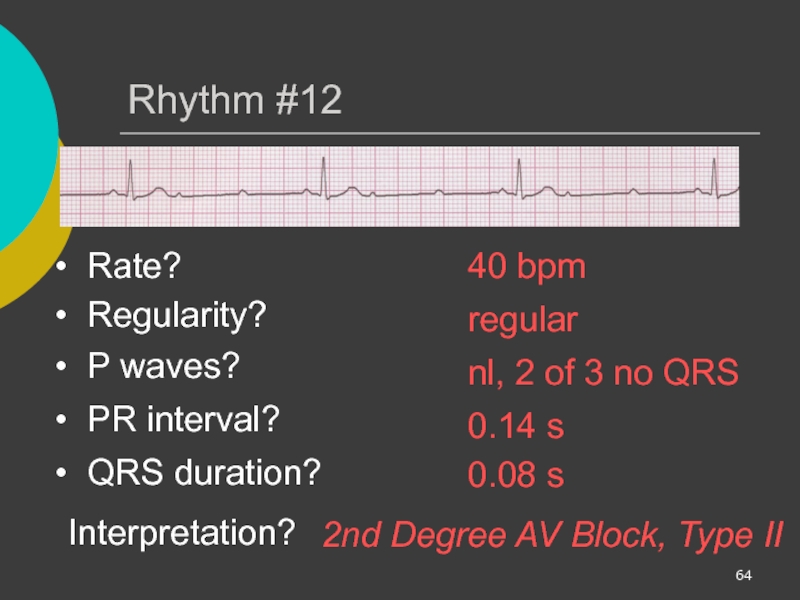
- 64. Rhythm #12 40 bpm Rate?
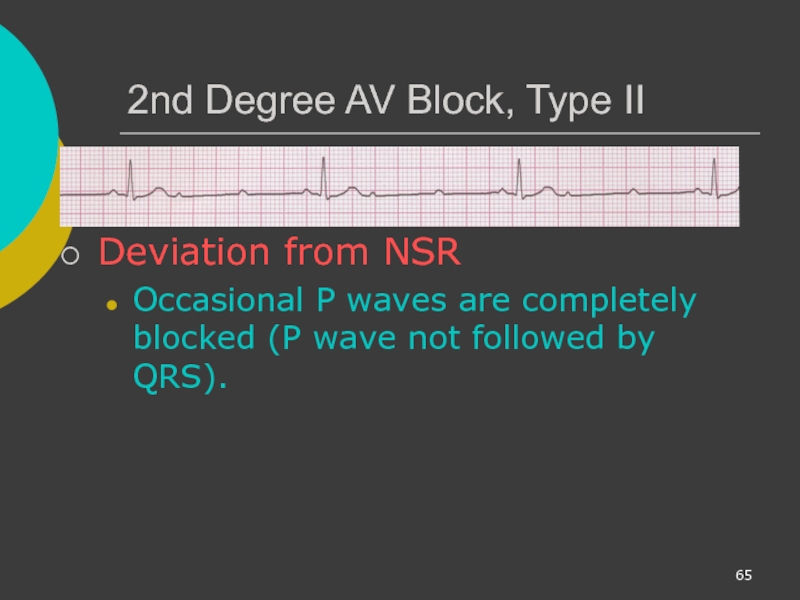
- 65. 2nd Degree AV Block, Type II
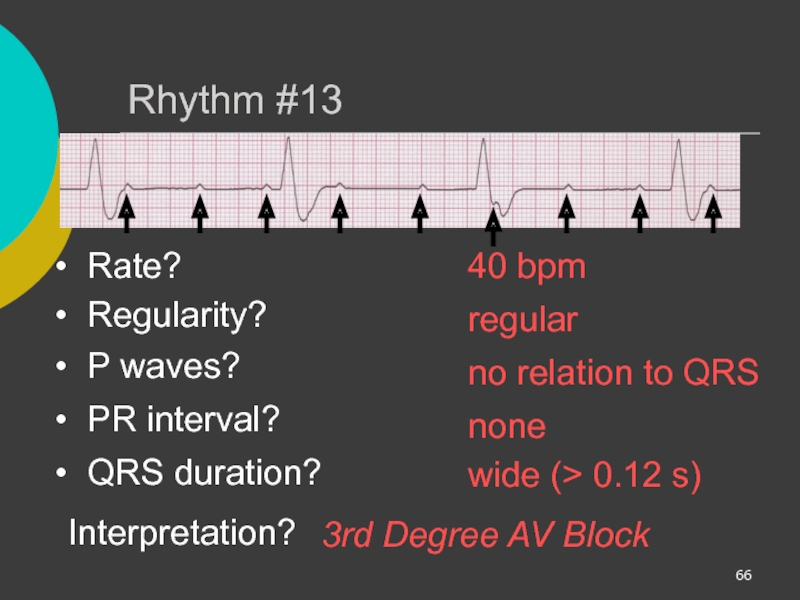
- 66. Rhythm #13 40 bpm Rate?
- 67. 3rd Degree AV Block Deviation from
- 68. 3rd Degree AV Block Etiology: There
- 69. Remember When an impulse originates in a
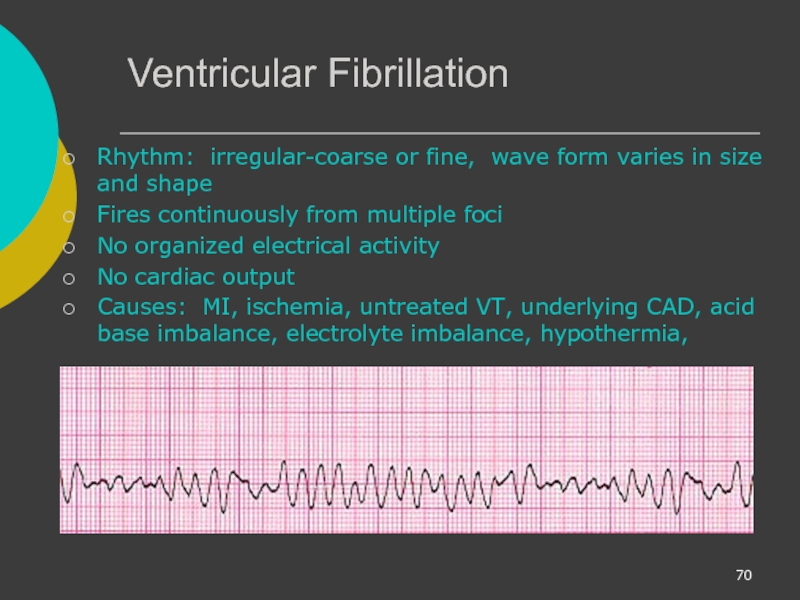
- 70. Ventricular Fibrillation Rhythm: irregular-coarse or fine, wave
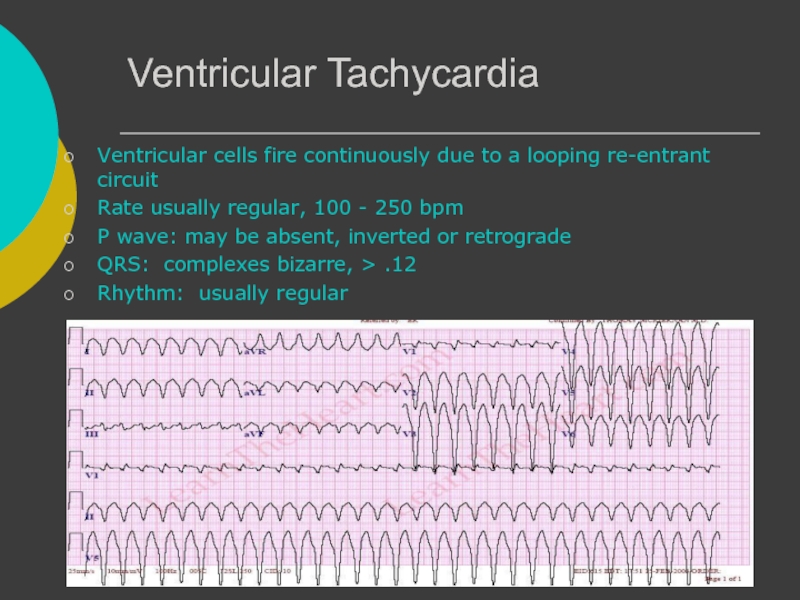
- 71. Ventricular Tachycardia Ventricular cells fire continuously due
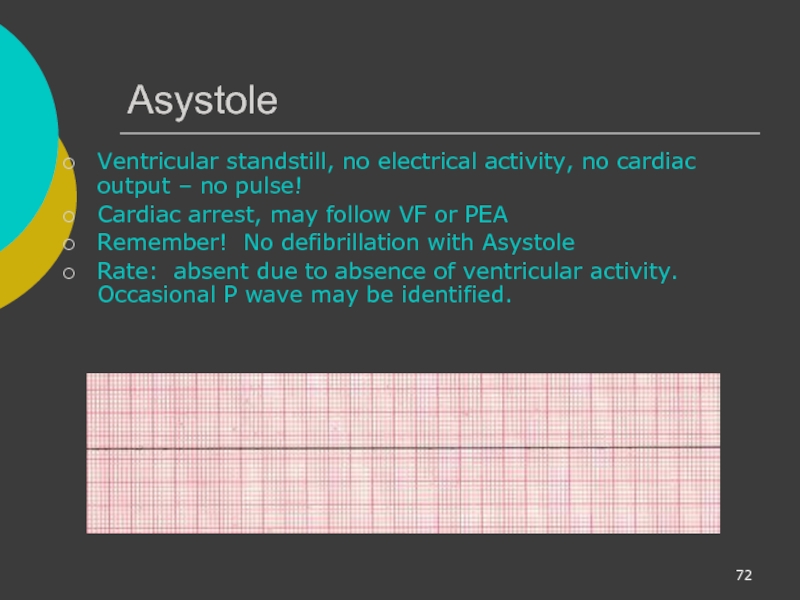
- 72. Asystole Ventricular standstill, no electrical activity, no
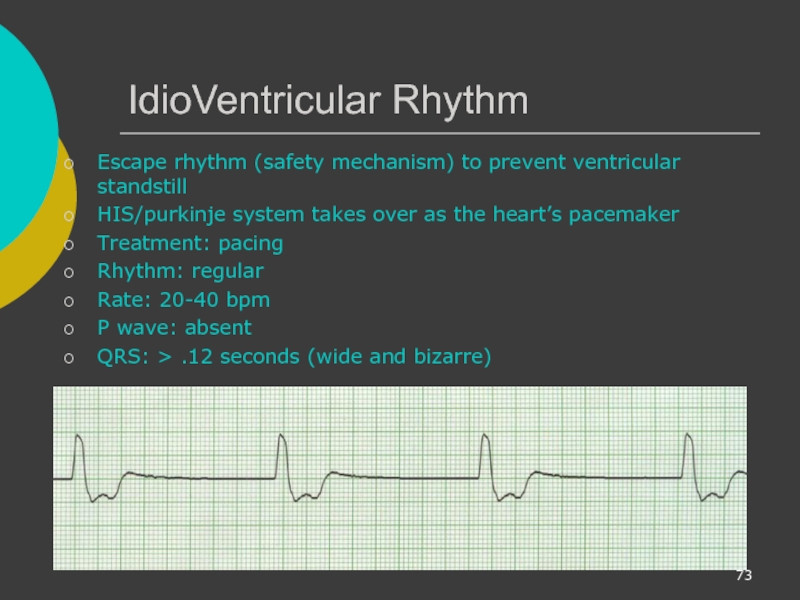
- 73. IdioVentricular Rhythm Escape rhythm (safety mechanism) to
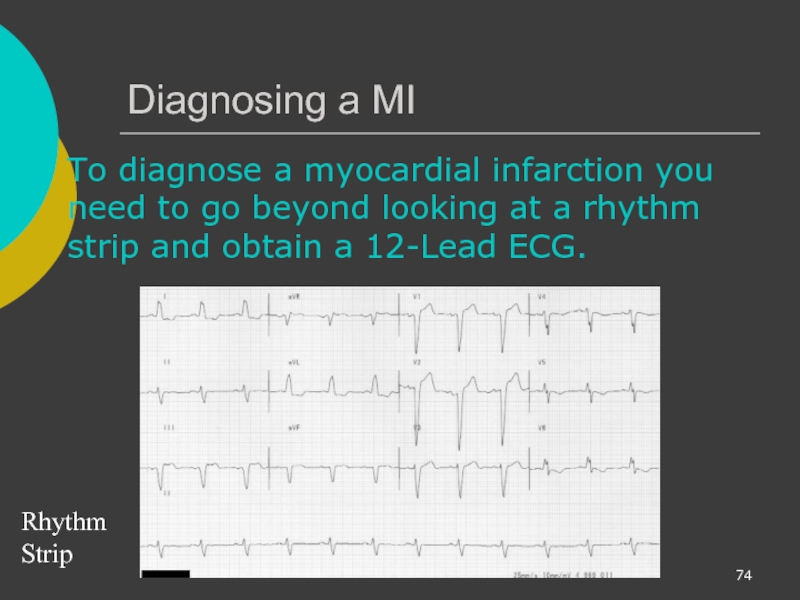
- 74. Diagnosing a MI To diagnose a myocardial
- 75. The 12-Lead ECG The 12-Lead ECG sees
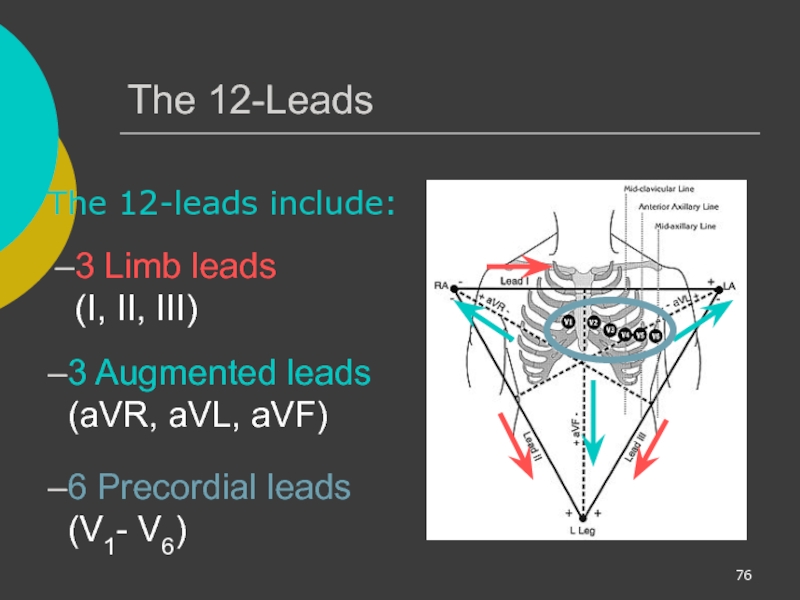
- 76. The 12-Leads The 12-leads include: 3 Limb
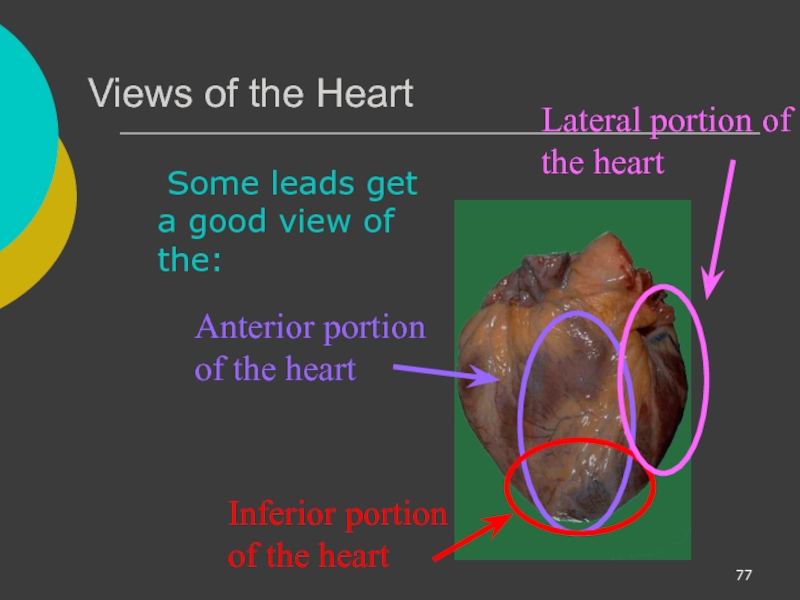
- 77. Views of the Heart Some leads get
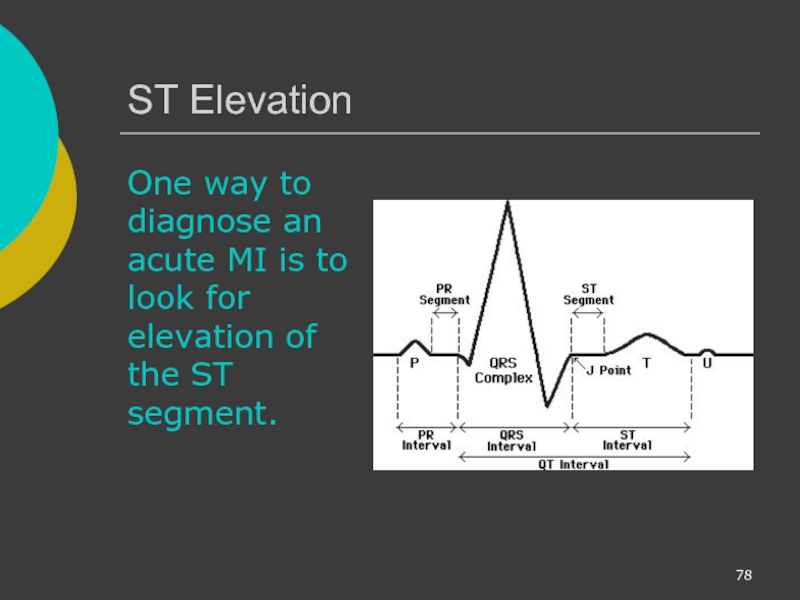
- 78. ST Elevation One way to diagnose an
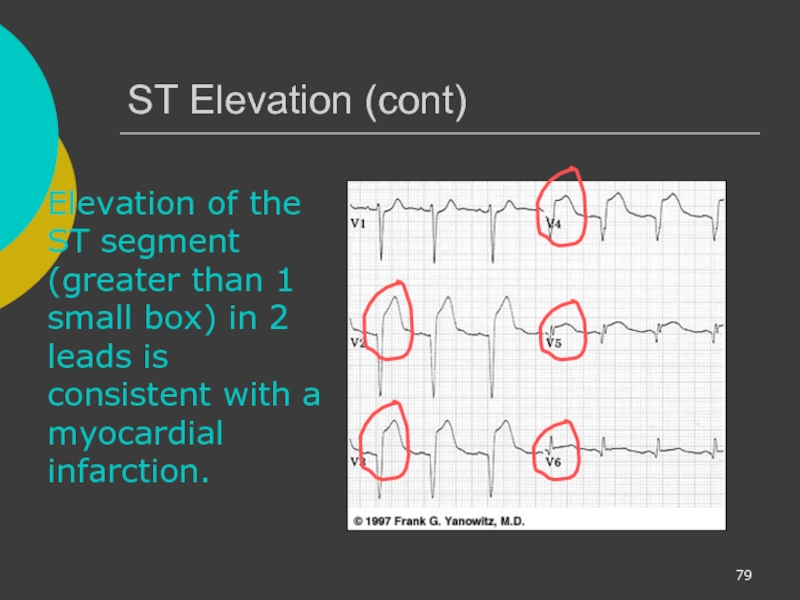
- 79. ST Elevation (cont) Elevation of the ST
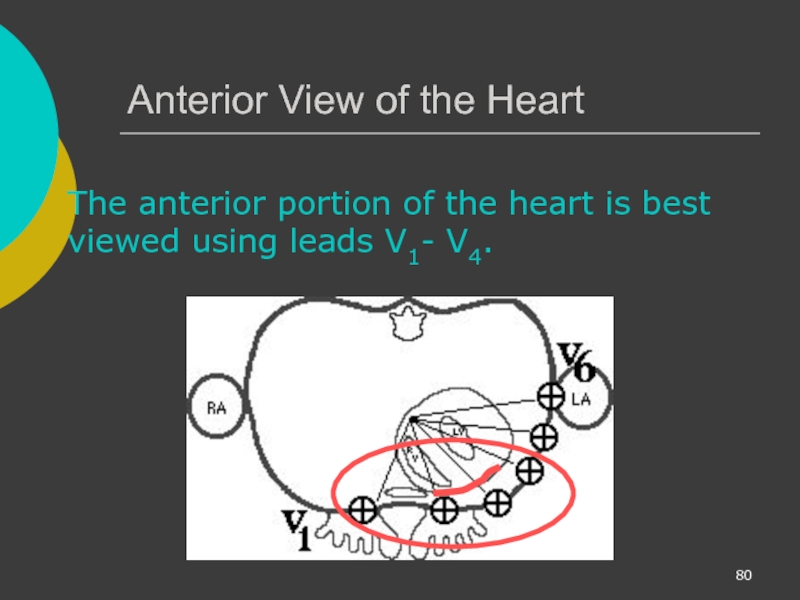
- 80. Anterior View of the Heart The anterior
- 81. Anterior Myocardial Infarction If you see changes
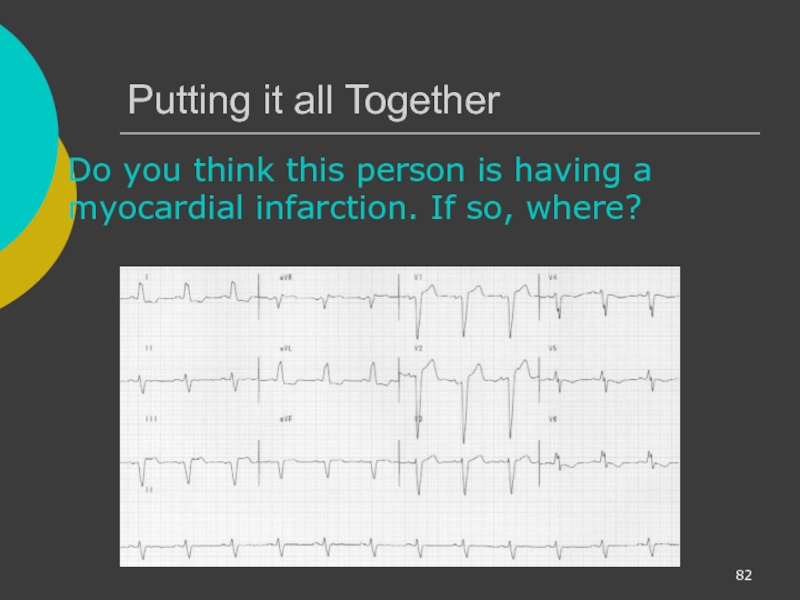
- 82. Putting it all Together Do you think
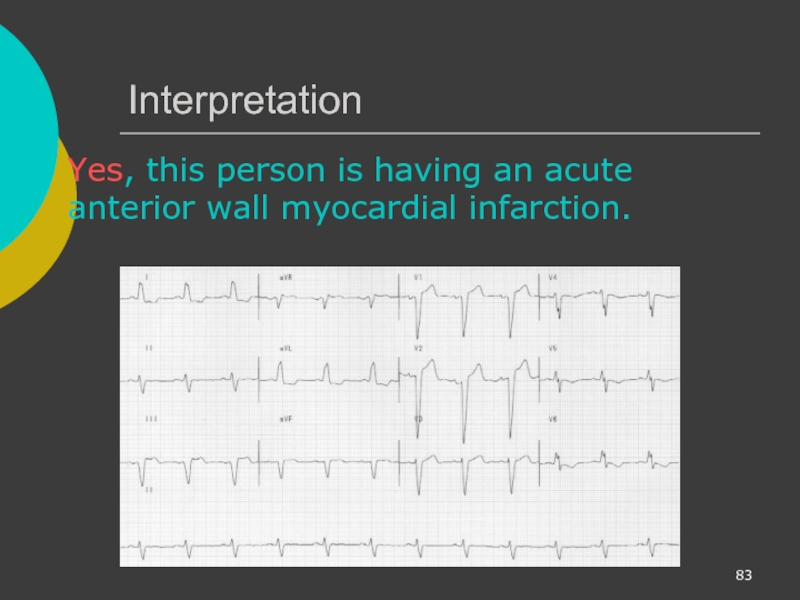
- 83. Interpretation Yes, this person is having an acute anterior wall myocardial infarction.
- 84. Other MI Locations Now that you know
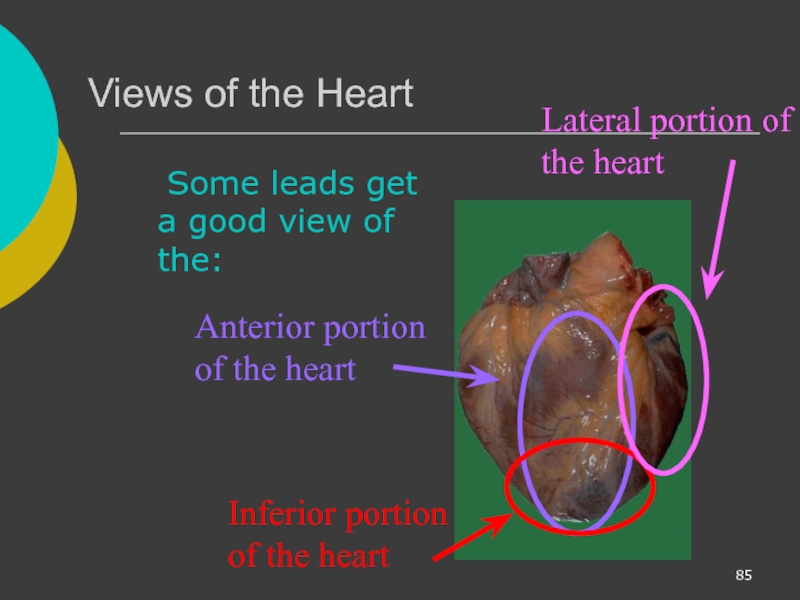
- 85. Views of the Heart Some leads get
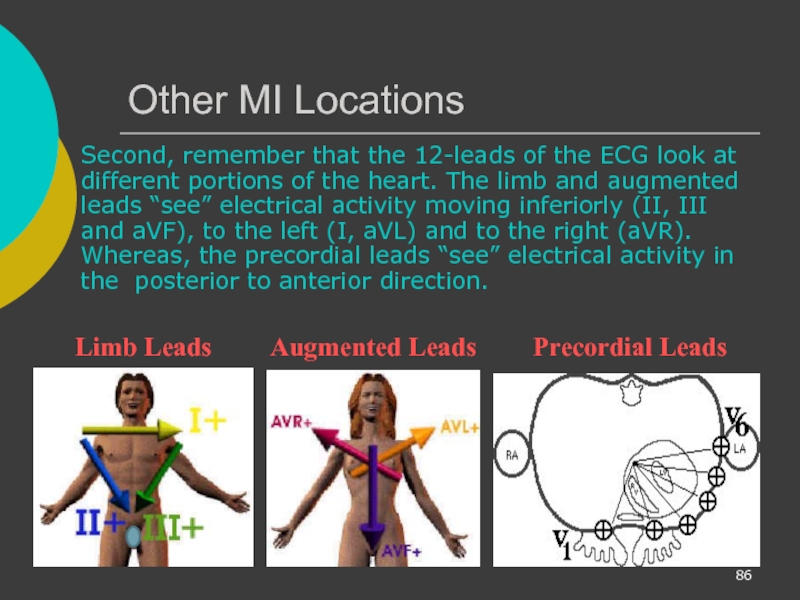
- 86. Other MI Locations Second, remember that the
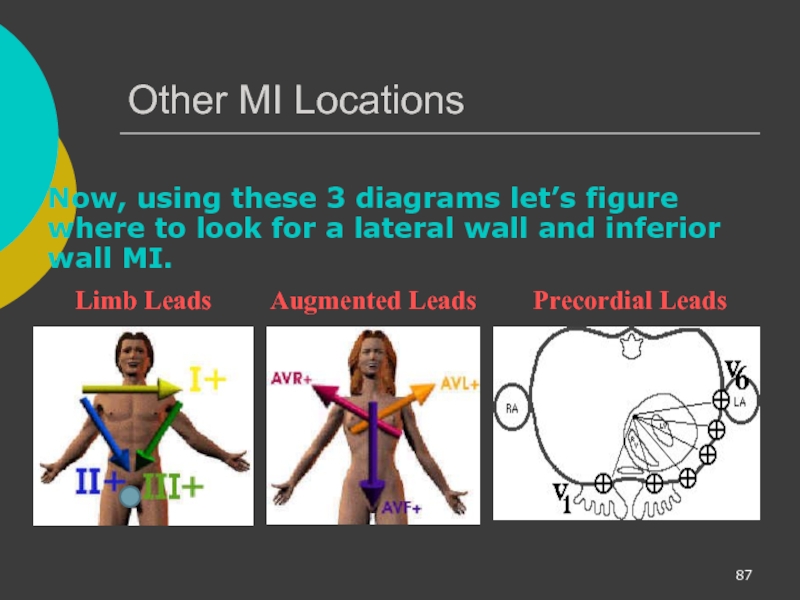
- 87. Other MI Locations Now, using these 3
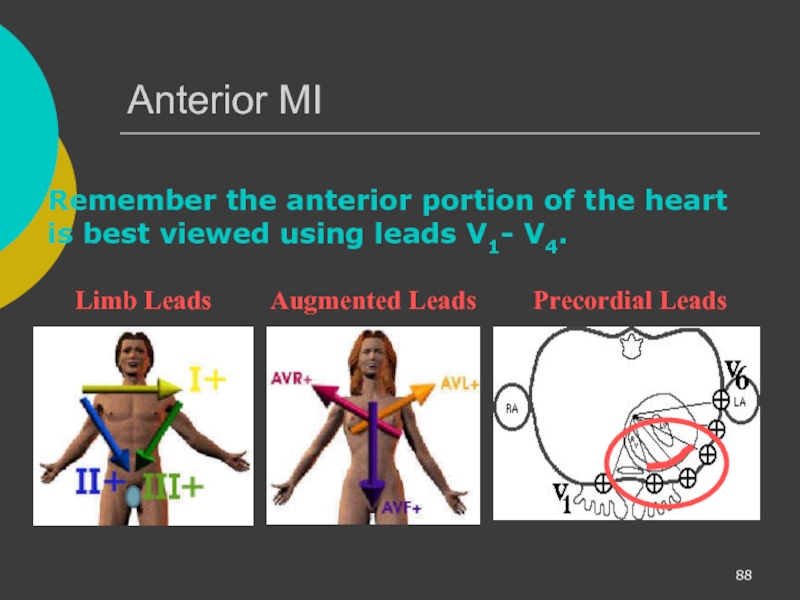
- 88. Anterior MI Remember the anterior portion of
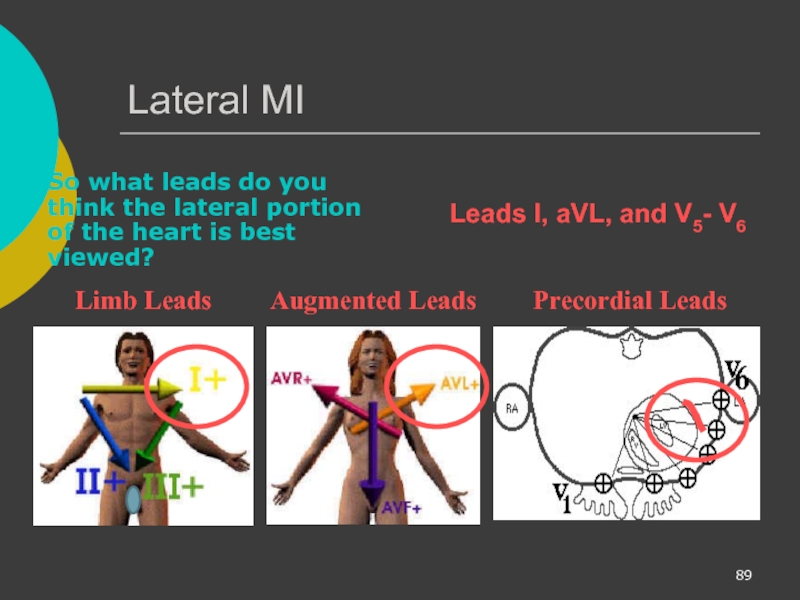
- 89. Lateral MI So what leads do you
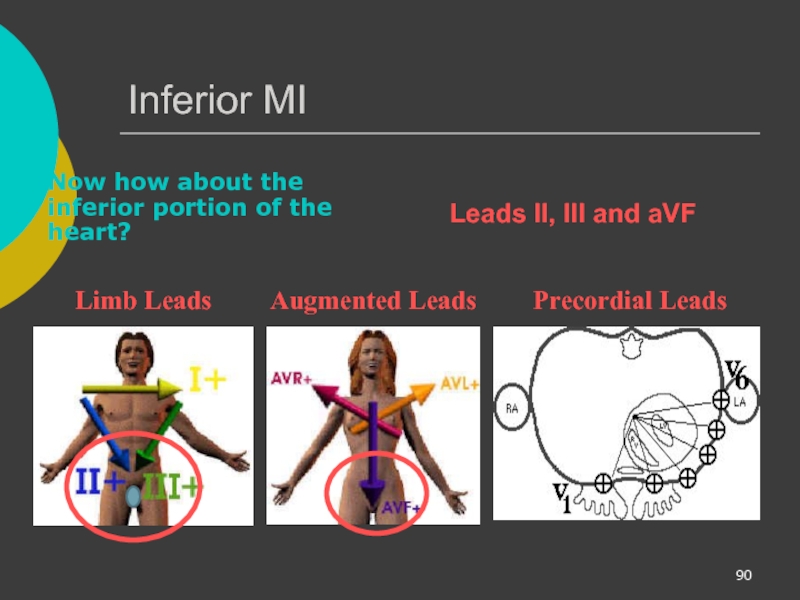
- 90. Inferior MI Now how about the inferior
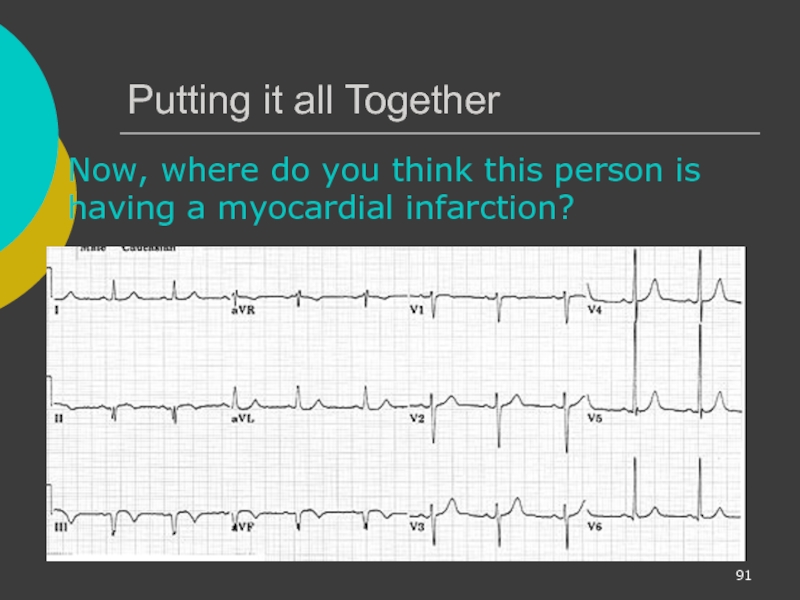
- 91. Putting it all Together Now, where do
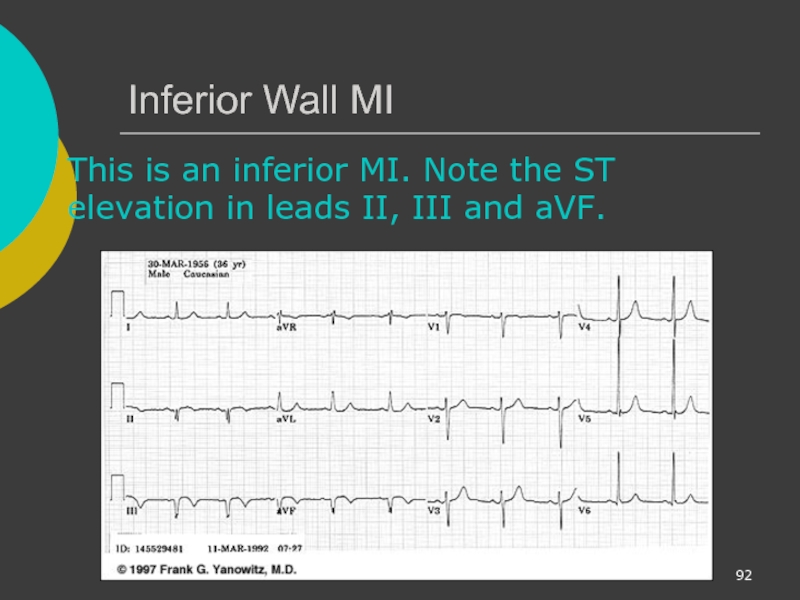
- 92. Inferior Wall MI This is an inferior
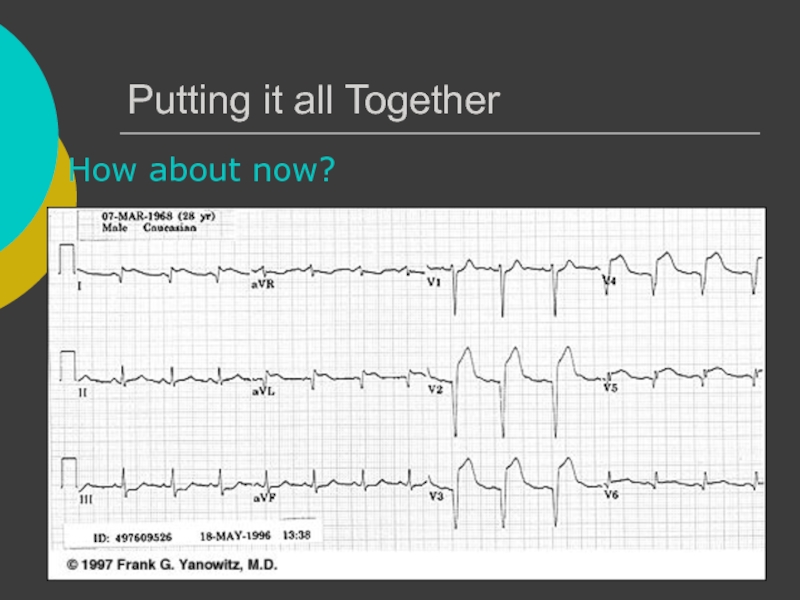
- 93. Putting it all Together How about now?
- 94. Anterolateral MI This person’s MI involves both
- 95. Reading 12-Lead ECGs The best way to
- 96. Rate Rhythm Axis Intervals Hypertrophy Infarct
- 97. Rate Rhythm Axis Intervals Hypertrophy Infarct If
Слайд 2Course Objectives
To recognize the normal rhythm of the heart - “Normal
To recognize the 17 most common rhythm disturbances (3-Lead)
To be shown an acute myocardial infarction on a 12-Lead ECG.
Слайд 3Learning Modules
ECG Basics
How to Analyze a Rhythm
Normal Sinus Rhythm
Heart Arrhythmias
Diagnosing a
Advanced 12-Lead Interpretation
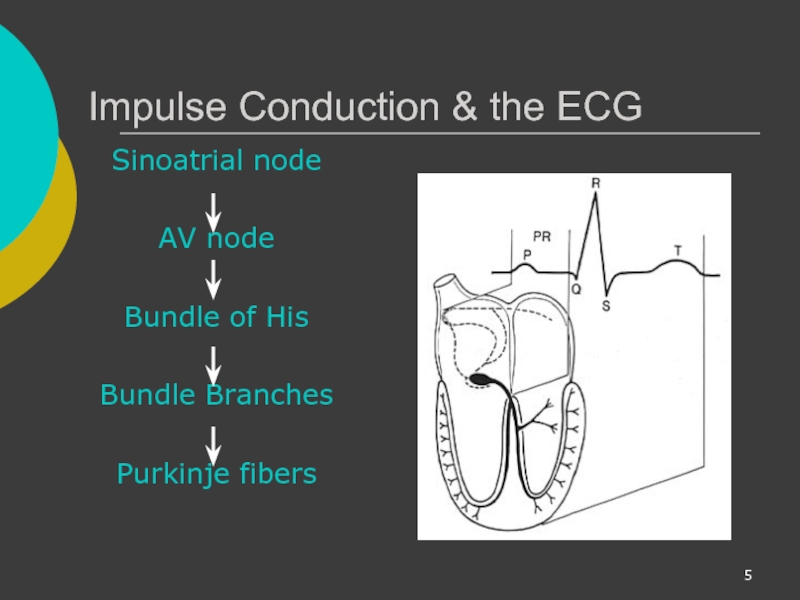
Слайд 5Impulse Conduction & the ECG
Sinoatrial node
AV node
Bundle of His
Bundle Branches
Purkinje fibers
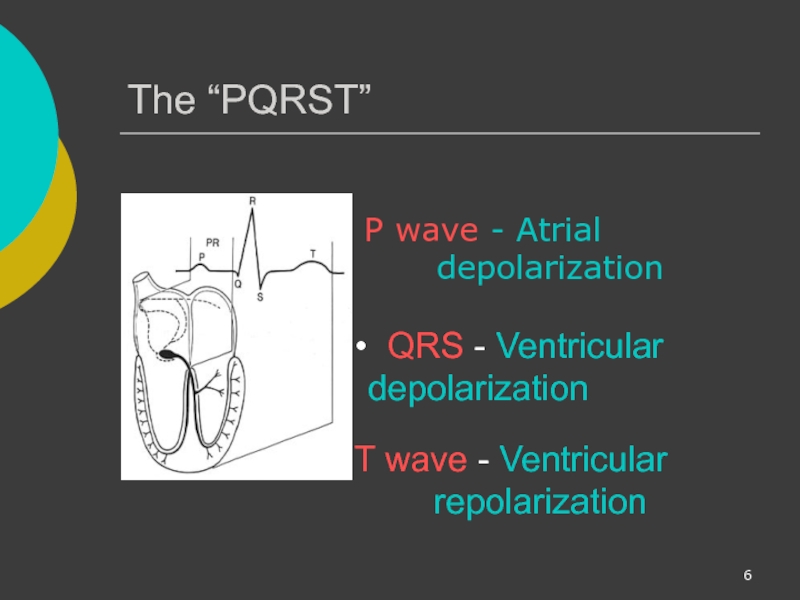
Слайд 6The “PQRST”
P wave - Atrial
T wave - Ventricular repolarization
QRS - Ventricular depolarization
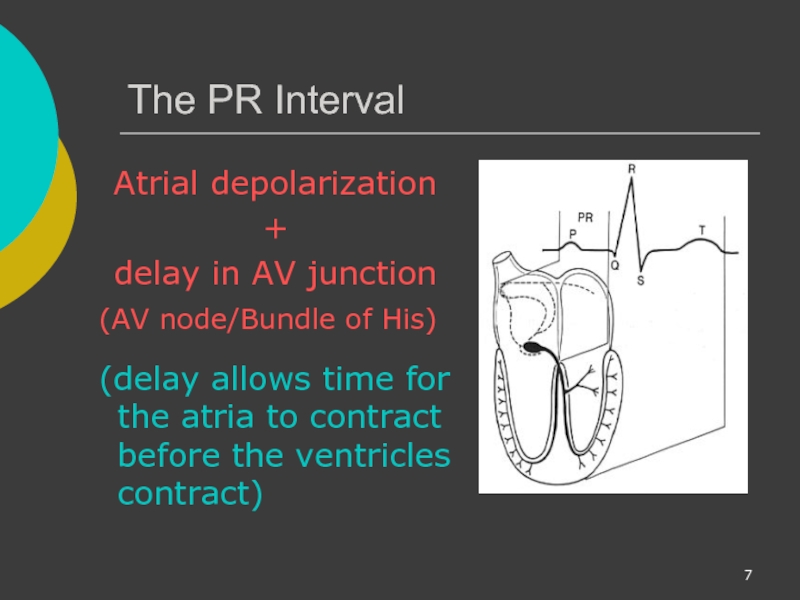
Слайд 7The PR Interval
Atrial depolarization
+
delay in AV junction
(AV node/Bundle of
(delay allows time for the atria to contract before the ventricles contract)
Слайд 8Pacemakers of the Heart
SA Node - Dominant pacemaker with an intrinsic
AV Node - Back-up pacemaker with an intrinsic rate of 40 - 60 beats/minute.
Ventricular cells - Back-up pacemaker with an intrinsic rate of 20 - 45 bpm.
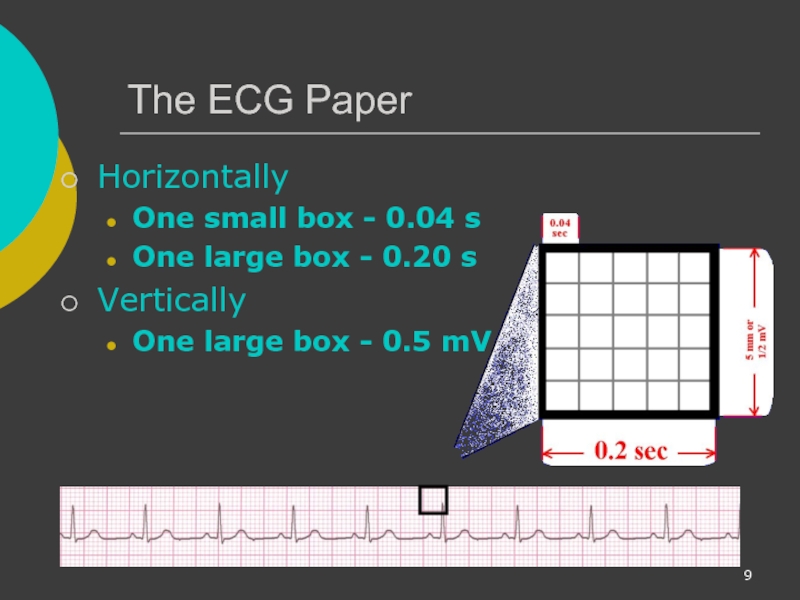
Слайд 9The ECG Paper
Horizontally
One small box - 0.04 s
One large box -
Vertically
One large box - 0.5 mV
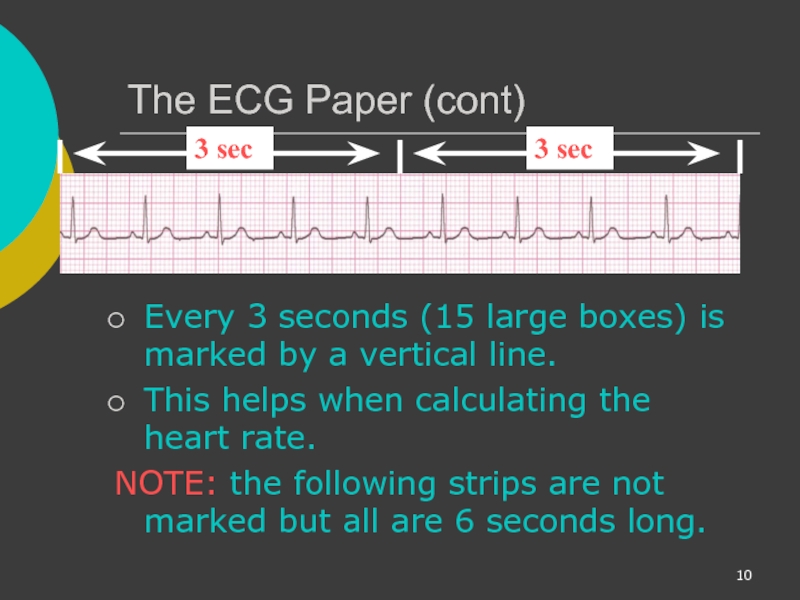
Слайд 10The ECG Paper (cont)
Every 3 seconds (15 large boxes) is marked
This helps when calculating the heart rate.
NOTE: the following strips are not marked but all are 6 seconds long.
3 sec
3 sec
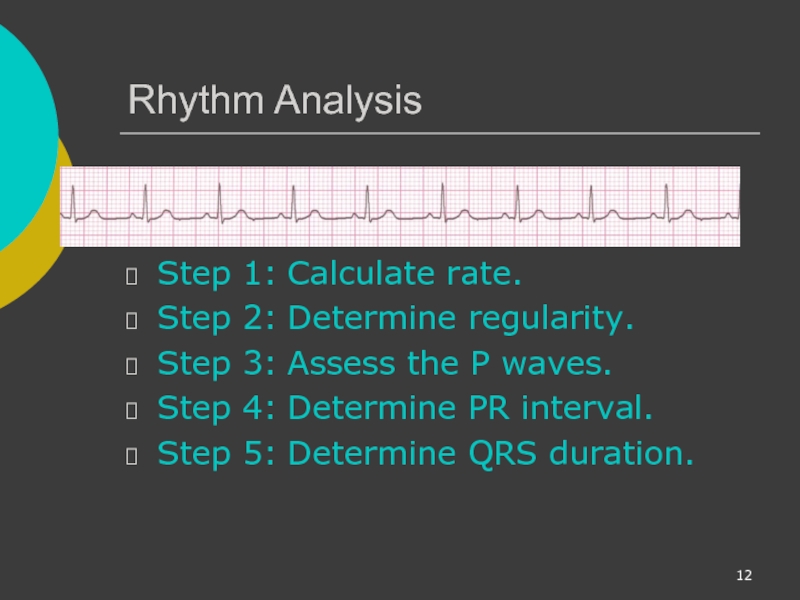
Слайд 12Rhythm Analysis
Step 1: Calculate rate.
Step 2: Determine regularity.
Step 3: Assess the P waves.
Step 4: Determine
Step 5: Determine QRS duration.
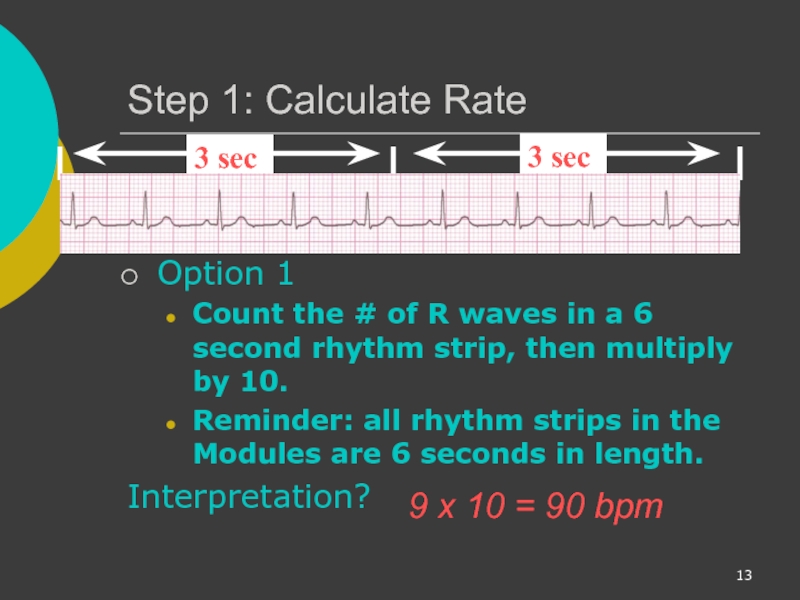
Слайд 13Step 1: Calculate Rate
Option 1
Count the # of R waves in
Reminder: all rhythm strips in the Modules are 6 seconds in length.
Interpretation?
9 x 10 = 90 bpm
3 sec
3 sec
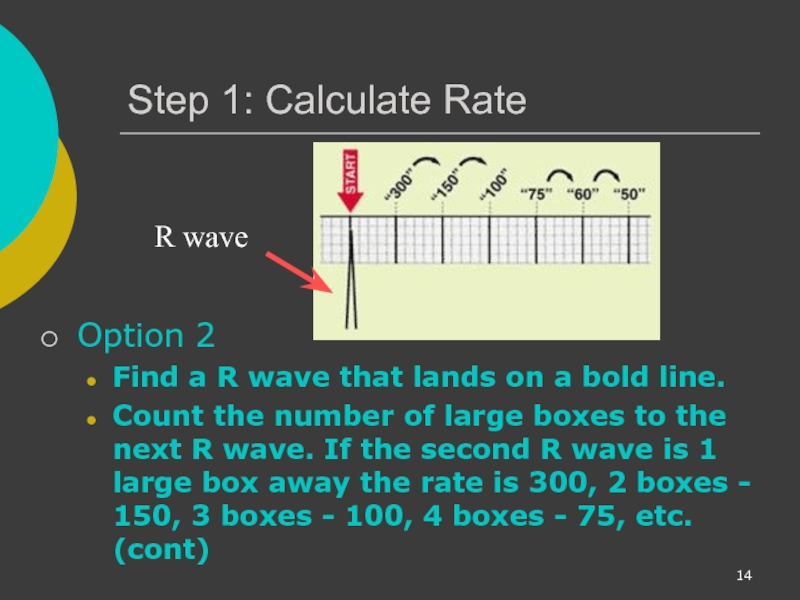
Слайд 14Step 1: Calculate Rate
Option 2
Find a R wave that lands
Count the number of large boxes to the next R wave. If the second R wave is 1 large box away the rate is 300, 2 boxes - 150, 3 boxes - 100, 4 boxes - 75, etc. (cont)
R wave
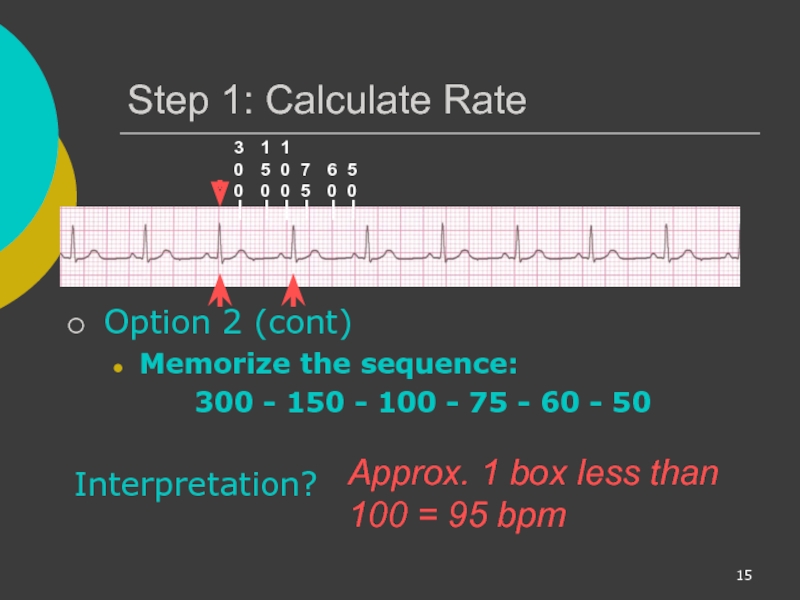
Слайд 15Step 1: Calculate Rate
Option 2 (cont)
Memorize the sequence:
300 - 150
Interpretation?
300
150
100
75
60
50
Approx. 1 box less than 100 = 95 bpm
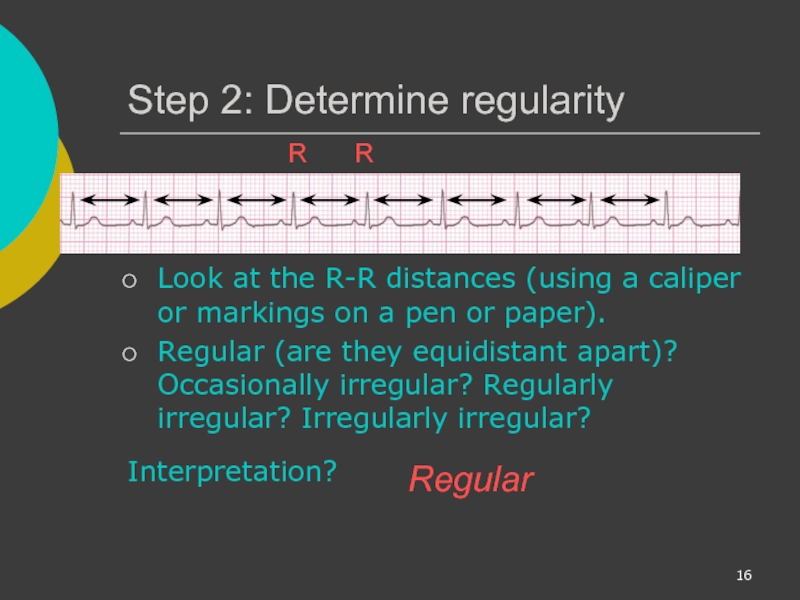
Слайд 16Step 2: Determine regularity
Look at the R-R distances (using a caliper
Regular (are they equidistant apart)? Occasionally irregular? Regularly irregular? Irregularly irregular?
Interpretation?
Regular
R
R
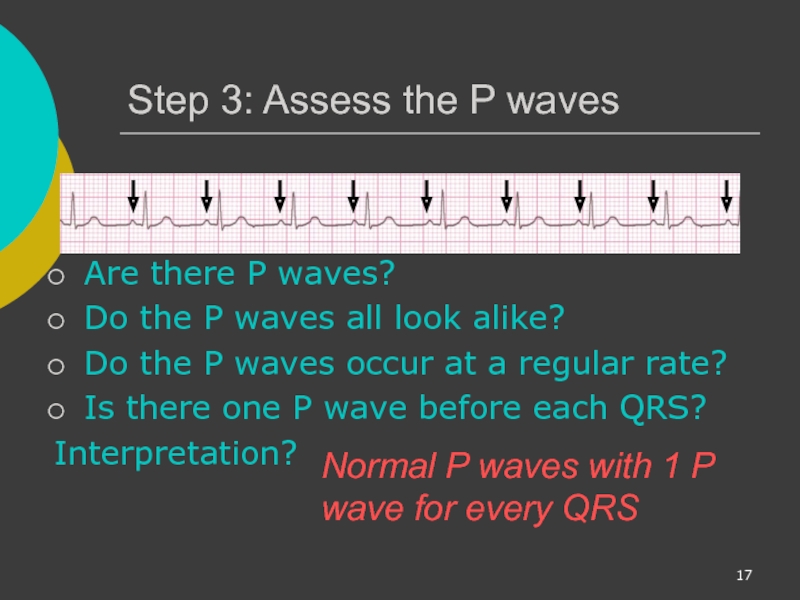
Слайд 17Step 3: Assess the P waves
Are there P waves?
Do the P
Do the P waves occur at a regular rate?
Is there one P wave before each QRS?
Interpretation?
Normal P waves with 1 P wave for every QRS
Слайд 18Step 4: Determine PR interval
Normal: 0.12 - 0.20 seconds.
Interpretation?
0.12 seconds
Слайд 20Rhythm Summary
Rate 90-95 bpm
Regularity regular
P waves normal
PR interval 0.12 s
QRS duration 0.08 s
Interpretation?
Normal Sinus Rhythm
Слайд 21NSR Parameters
Rate 60 - 100 bpm
Regularity regular
P waves normal
PR interval 0.12 - 0.20 s
QRS duration 0.04
Any deviation from above is sinus tachycardia, sinus bradycardia or an arrhythmia
Слайд 22Arrhythmia Formation
Arrhythmias can arise from problems in the:
Sinus node
Atrial cells
AV junction
Ventricular
Слайд 23SA Node Problems
The SA Node can:
fire too slow
fire too fast
Sinus Bradycardia
Sinus
*Sinus Tachycardia may be an appropriate response to stress.
Слайд 24Atrial Cell Problems
Atrial cells can:
fire occasionally from a focus
fire continuously
Premature Atrial Contractions (PACs)
Atrial Flutter
Слайд 25Atrial Cell Problems
Atrial cells can also:
• fire continuously from multiple foci
or
fire continuously due to multiple micro re-entrant “wavelets”
Atrial Fibrillation
Atrial Fibrillation
Слайд 26Teaching Moment
Multiple micro re-entrant “wavelets” refers to wandering small areas of
Atrial tissue
Слайд 27AV Junctional Problems
The AV junction can:
fire continuously due to a looping
block impulses coming from the SA Node
Paroxysmal Supraventricular Tachycardia
AV Junctional Blocks
Слайд 28Ventricular Cell Problems
Ventricular cells can:
fire occasionally from 1 or more foci
fire
fire continuously due to a looping re-entrant circuit
Premature Ventricular Contractions (PVCs)
Ventricular Fibrillation
Ventricular Tachycardia
Слайд 29Arrhythmias
Sinus Rhythms
Premature Beats
Supraventricular Arrhythmias
Ventricular Arrhythmias
AV Junctional Blocks
Слайд 31Rhythm #1
30 bpm
Rate?
Regularity?
regular
normal
0.10 s
P waves?
PR interval?
0.12 s
Interpretation?
Sinus Bradycardia
Слайд 33Sinus Bradycardia
Etiology: SA node is depolarizing slower than normal, impulse is
Слайд 34Rhythm #2
130 bpm
Rate?
Regularity?
regular
normal
0.08 s
P waves?
PR interval?
0.16 s
Interpretation?
Sinus Tachycardia
Слайд 36Sinus Tachycardia
Etiology: SA node is depolarizing faster than normal, impulse is
Remember: sinus tachycardia is a response to physical or psychological stress, not a primary arrhythmia.
Слайд 37Sinus Arrest
Etiology: SA node fails to depolarize and no compensatory mechanisms
Sinus arrest is usually a transient pause in sinus node activity
Слайд 38Premature Beats
Premature Atrial Contractions (PACs)
Premature Ventricular Contractions (PVCs)
Слайд 39Rhythm #3
70 bpm
Rate?
Regularity?
occasionally irreg.
2/7 different contour
0.08 s
P waves?
0.14 s (except 2/7)
QRS duration?
Interpretation?
NSR with Premature Atrial Contractions
Слайд 40Premature Atrial Contractions
Deviation from NSR
These ectopic beats originate in the atria
Слайд 41Premature Atrial Contractions
Etiology: Excitation of an atrial cell forms an impulse
Слайд 42Teaching Moment
When an impulse originates anywhere in the atria (SA node,
Слайд 43Rhythm #4
60 bpm
Rate?
Regularity?
occasionally irreg.
none for 7th QRS
0.08 s (7th
P waves?
PR interval?
0.14 s
QRS duration?
Interpretation?
Sinus Rhythm with 1 PVC
Слайд 44PVCs
Deviation from NSR
Ectopic beats originate in the ventricles resulting in wide
When there are more than 1 premature beats and look alike, they are called “uniform”. When they look different, they are called “multiform”.
Слайд 45PVCs
Etiology: One or more ventricular cells are depolarizing and the impulses
Слайд 46Teaching Moment
When an impulse originates in a ventricle, conduction through the
Слайд 47Ventricular Conduction
Normal
Signal moves rapidly through the ventricles
Abnormal
Signal moves slowly through the
Слайд 48Supraventricular Arrhythmias
Atrial Fibrillation
Atrial Flutter
Paroxysmal Supra Ventricular Tachycardia (PSVT)
Слайд 49Rhythm #5
100 bpm
Rate?
Regularity?
irregularly irregular
none
0.06 s
P waves?
PR interval?
none
Interpretation?
Atrial Fibrillation
Слайд 50Atrial Fibrillation
Deviation from NSR
No organized atrial depolarization, so no normal P
Atrial activity is chaotic (resulting in an irregularly irregular rate).
Common, affects 2-4%, up to 5-10% if > 80 years old
Слайд 51Atrial Fibrillation
Etiology: due to multiple re-entrant wavelets conducted between the R
The AV node allows some of the impulses to pass through at variable intervals (so rhythm is irregularly irregular).
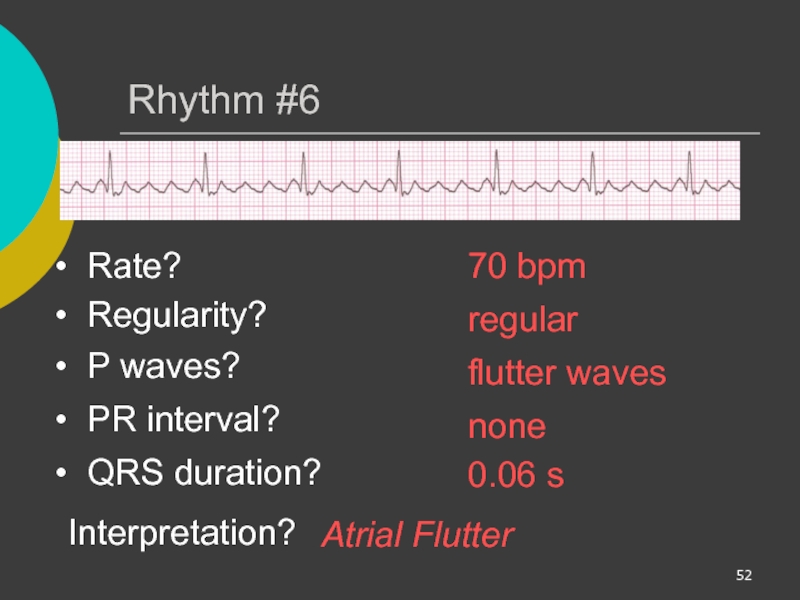
Слайд 52Rhythm #6
70 bpm
Rate?
Regularity?
regular
flutter waves
0.06 s
P waves?
PR interval?
none
Interpretation?
Atrial Flutter
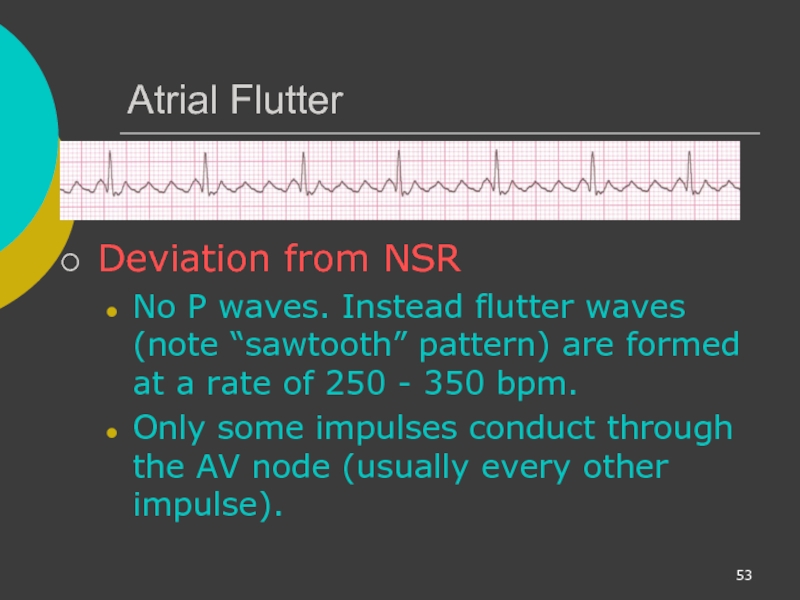
Слайд 53Atrial Flutter
Deviation from NSR
No P waves. Instead flutter waves (note “sawtooth”
Only some impulses conduct through the AV node (usually every other impulse).
Слайд 54Atrial Flutter
Etiology: Reentrant pathway in the right atrium with every 2nd,
Слайд 55Rhythm #7
74 ?148 bpm
Rate?
Regularity?
Regular ? regular
Normal ? none
0.08 s
PR interval?
0.16 s ? none
QRS duration?
Interpretation?
Paroxysmal Supraventricular Tachycardia
(PSVT)
Слайд 56PSVT:
Paroxysmal Supra Ventricular Tachycardia
Deviation from NSR
The heart rate suddenly speeds up,
Слайд 57AV Nodal Blocks
1st Degree AV Block
2nd Degree AV Block, Type I
2nd
3rd Degree AV Block
Слайд 58Rhythm #10
60 bpm
Rate?
Regularity?
regular
normal
0.08 s
P waves?
PR interval?
0.36 s
Interpretation?
1st Degree AV Block
Слайд 61Rhythm #11
50 bpm
Rate?
Regularity?
regularly irregular
nl, but 4th no QRS
0.08 s
PR interval?
lengthens
QRS duration?
Interpretation?
2nd Degree AV Block, Type I
Слайд 622nd Degree AV Block, Type I
Deviation from NSR
PR interval progressively lengthens,
Слайд 632nd Degree AV Block, Type I
Etiology: Each successive atrial impulse encounters
Слайд 64Rhythm #12
40 bpm
Rate?
Regularity?
regular
nl, 2 of 3 no QRS
0.08 s
PR interval?
0.14 s
QRS duration?
Interpretation?
2nd Degree AV Block, Type II
Слайд 652nd Degree AV Block, Type II
Deviation from NSR
Occasional P waves are
Слайд 66Rhythm #13
40 bpm
Rate?
Regularity?
regular
no relation to QRS
wide (> 0.12 s)
PR interval?
none
QRS duration?
Interpretation?
3rd Degree AV Block
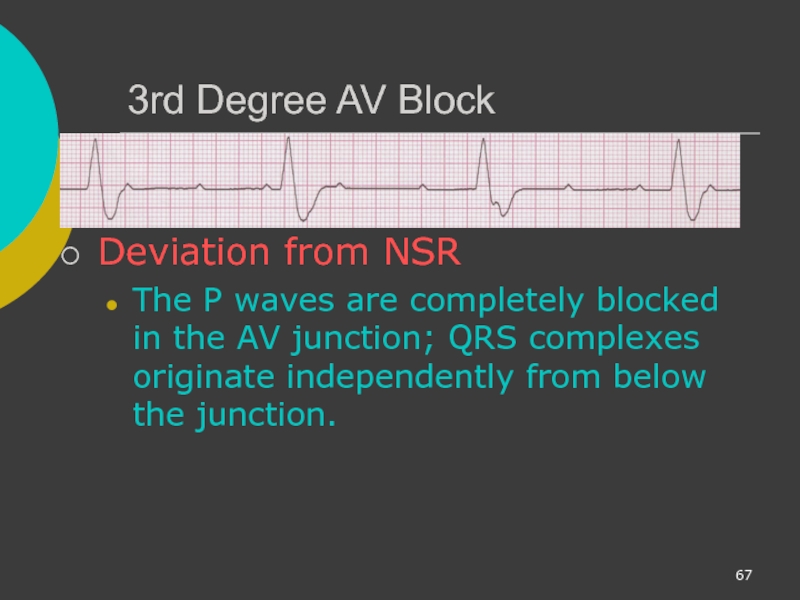
Слайд 673rd Degree AV Block
Deviation from NSR
The P waves are completely blocked
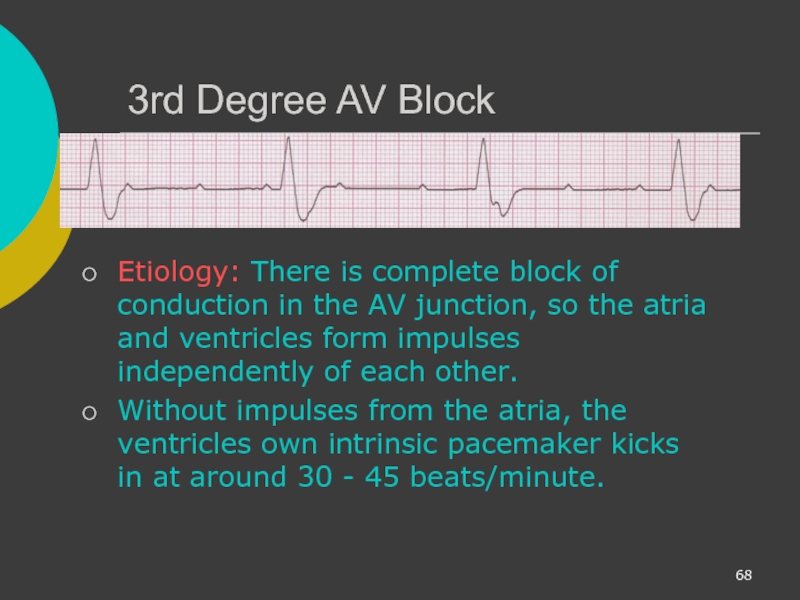
Слайд 683rd Degree AV Block
Etiology: There is complete block of conduction in
Without impulses from the atria, the ventricles own intrinsic pacemaker kicks in at around 30 - 45 beats/minute.
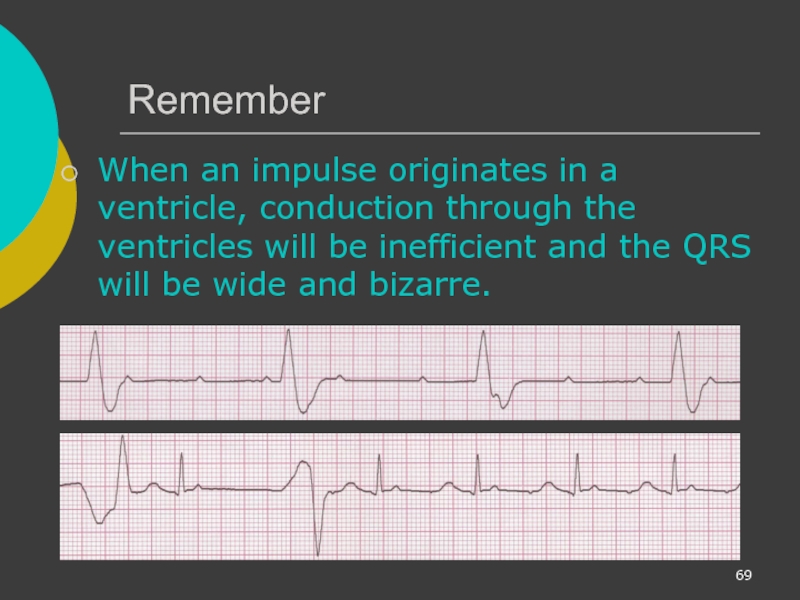
Слайд 69Remember
When an impulse originates in a ventricle, conduction through the ventricles
Слайд 70Ventricular Fibrillation
Rhythm: irregular-coarse or fine, wave form varies in size and
Fires continuously from multiple foci
No organized electrical activity
No cardiac output
Causes: MI, ischemia, untreated VT, underlying CAD, acid base imbalance, electrolyte imbalance, hypothermia,
Слайд 71Ventricular Tachycardia
Ventricular cells fire continuously due to a looping re-entrant circuit
Rate usually regular, 100 - 250 bpm
P wave: may be absent, inverted or retrograde
QRS: complexes bizarre, > .12
Rhythm: usually regular
Слайд 72Asystole
Ventricular standstill, no electrical activity, no cardiac output – no pulse!
Cardiac
Remember! No defibrillation with Asystole
Rate: absent due to absence of ventricular activity. Occasional P wave may be identified.
Слайд 73IdioVentricular Rhythm
Escape rhythm (safety mechanism) to prevent ventricular standstill
HIS/purkinje system takes
Treatment: pacing
Rhythm: regular
Rate: 20-40 bpm
P wave: absent
QRS: > .12 seconds (wide and bizarre)
Слайд 74Diagnosing a MI
To diagnose a myocardial infarction you need to go
Rhythm Strip
Слайд 75The 12-Lead ECG
The 12-Lead ECG sees the heart from 12 different
Therefore, the 12-Lead ECG helps you see what is happening in different portions of the heart.
The rhythm strip is only 1 of these 12 views.
Слайд 76The 12-Leads
The 12-leads include:
3 Limb leads
3 Augmented leads (aVR, aVL, aVF)
6 Precordial leads (V1- V6)
Слайд 77Views of the Heart
Some leads get a good view of the:
Anterior
Lateral portion of the heart
Inferior portion of the heart
Слайд 79ST Elevation (cont)
Elevation of the ST segment (greater than 1 small
Слайд 80Anterior View of the Heart
The anterior portion of the heart is
Слайд 81Anterior Myocardial Infarction
If you see changes in leads V1 - V4
Слайд 82Putting it all Together
Do you think this person is having a
Слайд 84Other MI Locations
Now that you know where to look for an
Слайд 85Views of the Heart
Some leads get a good view of the:
Anterior
Lateral portion of the heart
Inferior portion of the heart
Слайд 86Other MI Locations
Second, remember that the 12-leads of the ECG look
Limb Leads
Augmented Leads
Precordial Leads
Слайд 87Other MI Locations
Now, using these 3 diagrams let’s figure where to
Limb Leads
Augmented Leads
Precordial Leads
Слайд 88Anterior MI
Remember the anterior portion of the heart is best viewed
Limb Leads
Augmented Leads
Precordial Leads
Слайд 89Lateral MI
So what leads do you think the lateral portion of
Limb Leads
Augmented Leads
Precordial Leads
Leads I, aVL, and V5- V6
Слайд 90Inferior MI
Now how about the inferior portion of the heart?
Limb
Augmented Leads
Precordial Leads
Leads II, III and aVF
Слайд 91Putting it all Together
Now, where do you think this person is
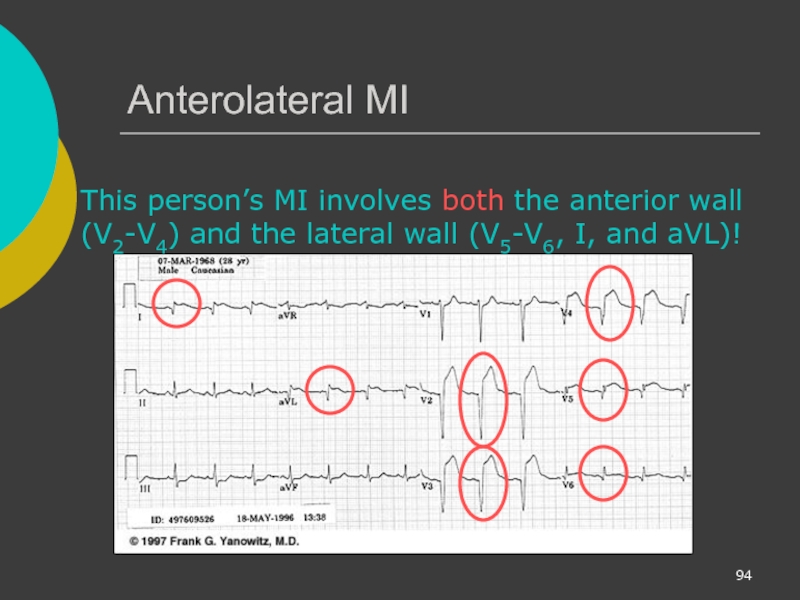
Слайд 94Anterolateral MI
This person’s MI involves both the anterior wall (V2-V4) and
Слайд 95Reading 12-Lead ECGs
The best way to read 12-lead ECGs is to
Calculate RATE
Determine RHYTHM
Determine QRS AXIS
Calculate INTERVALS
Assess for HYPERTROPHY
Look for evidence of INFARCTION
Слайд 96Rate Rhythm Axis Intervals Hypertrophy Infarct
In Module II you learned
There is one new thing to keep in mind when determining the rate in a 12-lead ECG…
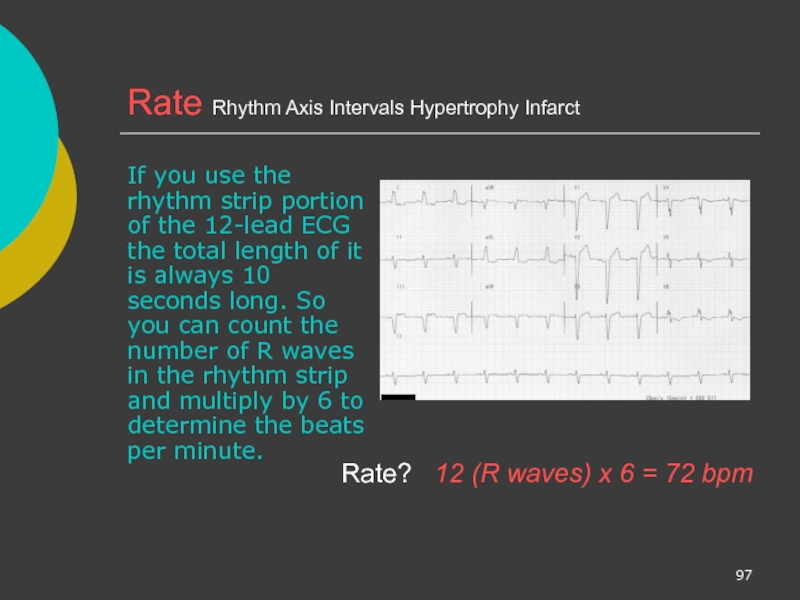
Слайд 97Rate Rhythm Axis Intervals Hypertrophy Infarct
If you use the rhythm strip
Rate?
12 (R waves) x 6 = 72 bpm