Выполнил: Ермешев Ербулат
- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Безопасность длительного применения нимесулида в отношении побочных эффектов со стороны ЖКТ у людей, страдающих остеоартрозом презентация
Содержание
- 1. Безопасность длительного применения нимесулида в отношении побочных эффектов со стороны ЖКТ у людей, страдающих остеоартрозом
- 2. Остеоартроз - дегенеративно-дистрофическое заболевание суставов, причиной которого является
- 3. Актуальность: В настоящее время имеются множество заболеваний,
- 4. Цель исследования: Изучить безопасность длительного применения нимесулида
- 5. Задачи исследования: Изучить соответсвующую литературу. Определиться с
- 6. Дизайн исследования: Рандомизированное контролируемое клиническое исследование.
- 7. Тип выборки: Простая случайная. Мною было найдено
- 8. Критерии включения Наличие в анамнезе остеоартроза коленного сустава с болевым синдромом.
- 9. Критерии исключения длительность заболевания более 5
- 10. Безопасно ли длительное применение нимесулида в отношении
- 11. P-Мужчины и женщины в возрастных рамках от
- 12. BACKGROUND: Selective inhibitors of cyclooxygenase (COX)-2 may
- 13. Уменьшает ли применение нимесулида в сравнении с напроксеном повреждение слизистой оболочки желудка? Клинический вопрос
- 14. P- Здоровые добровольцы. I- нимесулид. C- напроксен.
- 15. Дизайн исследования: Рандомизированное контролируемое клиническое исследование.
- 16. Тридцать шесть здоровых добровольцев в возрасте 40-67
- 17. Критерии исключения наличие аллергической реакции на НПВП наличие язвенной болезни в анамнезе.
Слайд 1Западно-Казахстанский государственнный медицинский университет имени Марата Оспанова
Безопасность длительного применения нимесулида в
отношении побочных эффектов со стороны ЖКТ у людей страдающих остеоартрозом коленного сустава с болевым синдромом.
Слайд 2Остеоартроз - дегенеративно-дистрофическое заболевание суставов, причиной которого является поражение хрящевой ткани суставных поверхностей.
Нимесулид -
(НПВП) из класса сульфонанилидов. Является селективным конкурентным ингибитором циклооксигеназы-2 (ЦОГ-2) — фермента, участвующего в синтезе простагландинов, медиаторов отека, воспаления и боли. Оказывает противовоспалительное, анальгезирующее и жаропонижающее действие.
Слайд 3Актуальность:
В настоящее время имеются множество заболеваний, сопровождающихся хронической болью, вследствии чего
идет неконтролируемый прием НПВП, у которых наиболее часто встречающийся побочный эффект проявляется изъязвлением слизистой оболочки желудка. Поэтому актуален вопрос препаратов с меньшим проявлением побочных эффектов со стороны ЖКТ.
Слайд 4Цель исследования:
Изучить безопасность длительного применения нимесулида в отношении побочных эффектов со
стороны ЖКТ у людей страдающих остеоартрозом коленных суставов с болевым синдромом.
Слайд 5Задачи исследования:
Изучить соответсвующую литературу.
Определиться с совокупностью подходящих пациентов для дальнейшего формирования
выборки.
Проведение диагностических методов исследования для контроля состояния стенки желудка.
Произвести статистический анализ.
Проведение диагностических методов исследования для контроля состояния стенки желудка.
Произвести статистический анализ.
Слайд 7Тип выборки:
Простая случайная. Мною было найдено 250 больных с остеоартрозом коленного
сустава в возрастных рамках от 48 до 60 лет с хронической болью в коленном суставе. Каждый пациент был пронумерован и затем с помощью генерации случайного числа в программе excel были включены в выборку 150 человек, которые были поделены на контрольную и исследовательскую группы.
Слайд 9Критерии исключения
длительность заболевания более 5 лет
наличие хронической язвы в
анамнезе.
Hb- ассоциированные гастриты.
Hb- ассоциированные гастриты.
Слайд 10Безопасно ли длительное применение нимесулида в отношении побочных эффектов со стороны
ЖКТ у людей страдающих остеоартрозом коленного сустава с болевым синдромом в стравнении с неселективными НПВП у лиц в возрастных рамках от 48 до 60 лет?.
Клинический вопрос
Слайд 11 P-Мужчины и женщины в возрастных рамках от 48 до 60лет.
I- Нимесулид
C-
Неселективные НПВП.
О- Значительно меньшее число случаев повреждения слизистой оболочки желудка.
О- Значительно меньшее число случаев повреждения слизистой оболочки желудка.
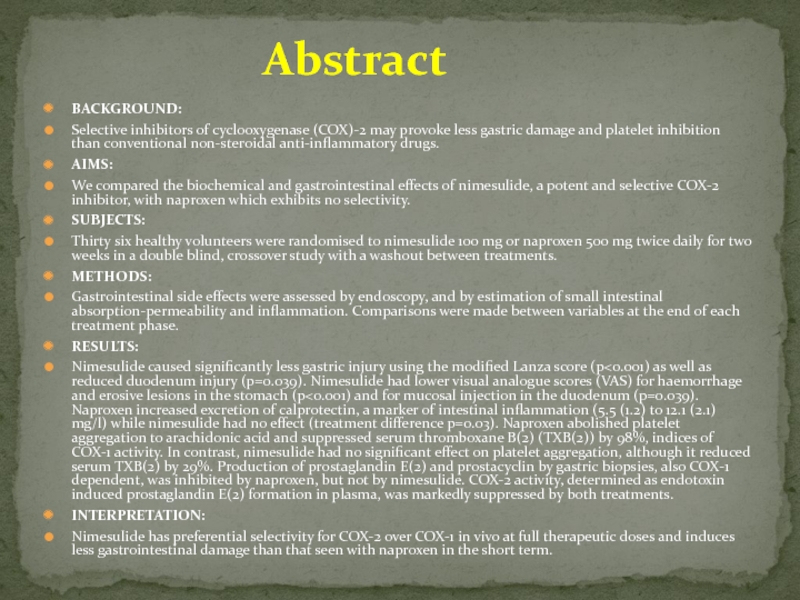
Слайд 12BACKGROUND:
Selective inhibitors of cyclooxygenase (COX)-2 may provoke less gastric damage and
platelet inhibition than conventional non-steroidal anti-inflammatory drugs.
AIMS:
We compared the biochemical and gastrointestinal effects of nimesulide, a potent and selective COX-2 inhibitor, with naproxen which exhibits no selectivity.
SUBJECTS:
Thirty six healthy volunteers were randomised to nimesulide 100 mg or naproxen 500 mg twice daily for two weeks in a double blind, crossover study with a washout between treatments.
METHODS:
Gastrointestinal side effects were assessed by endoscopy, and by estimation of small intestinal absorption-permeability and inflammation. Comparisons were made between variables at the end of each treatment phase.
RESULTS:
Nimesulide caused significantly less gastric injury using the modified Lanza score (p<0.001) as well as reduced duodenum injury (p=0.039). Nimesulide had lower visual analogue scores (VAS) for haemorrhage and erosive lesions in the stomach (p<0.001) and for mucosal injection in the duodenum (p=0.039). Naproxen increased excretion of calprotectin, a marker of intestinal inflammation (5.5 (1.2) to 12.1 (2.1) mg/l) while nimesulide had no effect (treatment difference p=0.03). Naproxen abolished platelet aggregation to arachidonic acid and suppressed serum thromboxane B(2) (TXB(2)) by 98%, indices of COX-1 activity. In contrast, nimesulide had no significant effect on platelet aggregation, although it reduced serum TXB(2) by 29%. Production of prostaglandin E(2) and prostacyclin by gastric biopsies, also COX-1 dependent, was inhibited by naproxen, but not by nimesulide. COX-2 activity, determined as endotoxin induced prostaglandin E(2) formation in plasma, was markedly suppressed by both treatments.
INTERPRETATION:
Nimesulide has preferential selectivity for COX-2 over COX-1 in vivo at full therapeutic doses and induces less gastrointestinal damage than that seen with naproxen in the short term.
AIMS:
We compared the biochemical and gastrointestinal effects of nimesulide, a potent and selective COX-2 inhibitor, with naproxen which exhibits no selectivity.
SUBJECTS:
Thirty six healthy volunteers were randomised to nimesulide 100 mg or naproxen 500 mg twice daily for two weeks in a double blind, crossover study with a washout between treatments.
METHODS:
Gastrointestinal side effects were assessed by endoscopy, and by estimation of small intestinal absorption-permeability and inflammation. Comparisons were made between variables at the end of each treatment phase.
RESULTS:
Nimesulide caused significantly less gastric injury using the modified Lanza score (p<0.001) as well as reduced duodenum injury (p=0.039). Nimesulide had lower visual analogue scores (VAS) for haemorrhage and erosive lesions in the stomach (p<0.001) and for mucosal injection in the duodenum (p=0.039). Naproxen increased excretion of calprotectin, a marker of intestinal inflammation (5.5 (1.2) to 12.1 (2.1) mg/l) while nimesulide had no effect (treatment difference p=0.03). Naproxen abolished platelet aggregation to arachidonic acid and suppressed serum thromboxane B(2) (TXB(2)) by 98%, indices of COX-1 activity. In contrast, nimesulide had no significant effect on platelet aggregation, although it reduced serum TXB(2) by 29%. Production of prostaglandin E(2) and prostacyclin by gastric biopsies, also COX-1 dependent, was inhibited by naproxen, but not by nimesulide. COX-2 activity, determined as endotoxin induced prostaglandin E(2) formation in plasma, was markedly suppressed by both treatments.
INTERPRETATION:
Nimesulide has preferential selectivity for COX-2 over COX-1 in vivo at full therapeutic doses and induces less gastrointestinal damage than that seen with naproxen in the short term.
Abstract
Слайд 13Уменьшает ли применение нимесулида в сравнении с напроксеном повреждение слизистой оболочки
желудка?
Клинический вопрос
Слайд 14P- Здоровые добровольцы.
I- нимесулид.
C- напроксен.
О- применение нимесулида в намного меньшей степени
повреждает слизистую желудка.
Слайд 16Тридцать шесть здоровых добровольцев в возрасте 40-67 лет были набраны из
двух центров: больницы Бомонта Дублин, Ирландия (n = 13) и университетской больницы Рейкьявик, Исландия (n = 23).
Способ формирования выборки.
Слайд 17Критерии исключения
наличие аллергической реакции на НПВП
наличие язвенной болезни в
анамнезе.