- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Bacterial infections, sepsis презентация
Содержание
- 1. Bacterial infections, sepsis
- 2. Background Neonatal sepsis may be categorized
- 3. Pathophysiology 1. Specific microbial factors - The
- 4. The microorganisms most commonly associated with early-onset
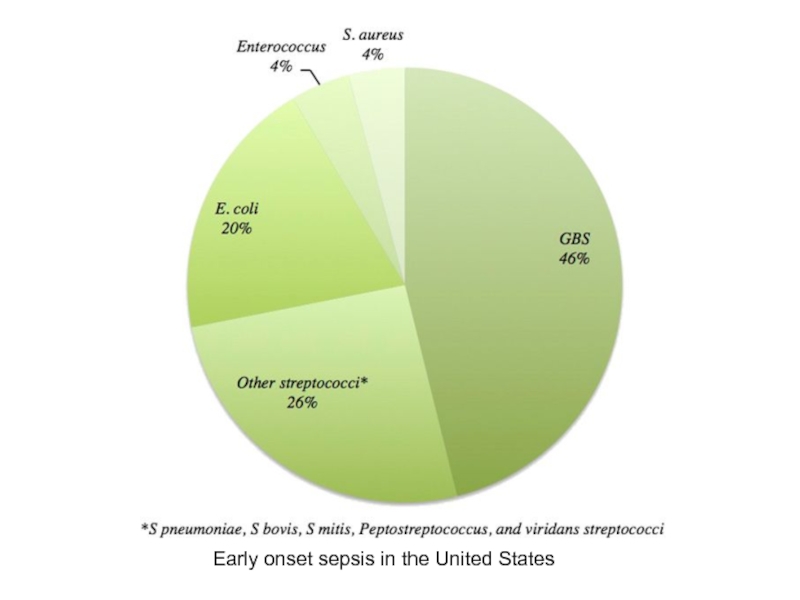
- 5. Early onset sepsis in the United States
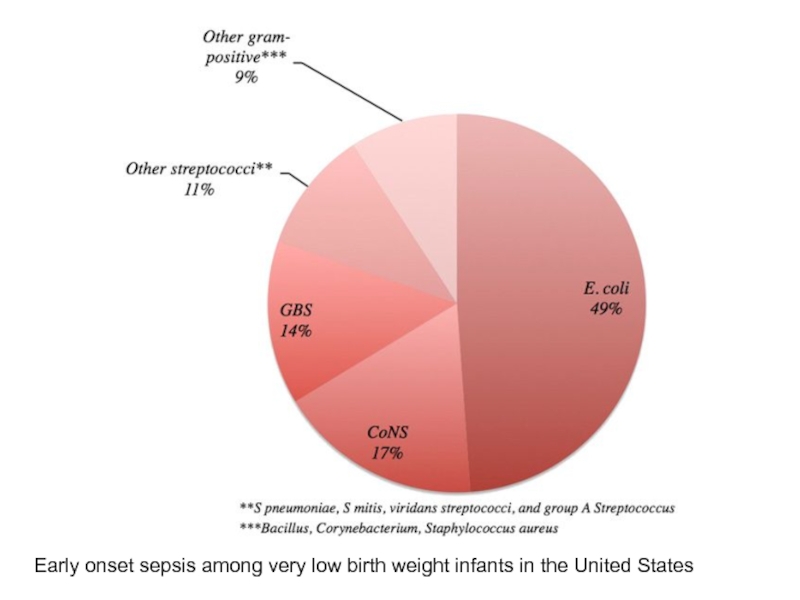
- 6. Early onset sepsis among very low birth weight infants in the United States
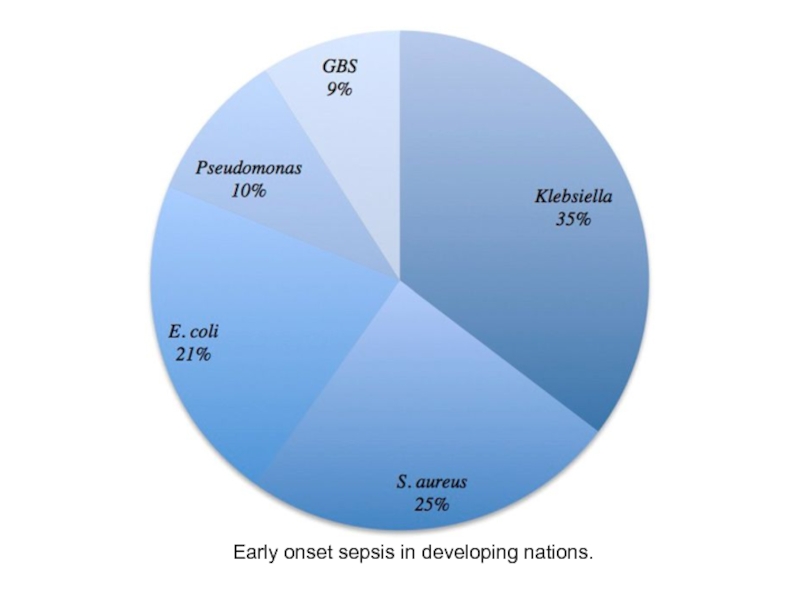
- 7. Early onset sepsis in developing nations.
- 8. The most common risk factors associated with
- 9. Other factors that are associated with or
- 10. Organisms that have been implicated in causing
- 11. Late-onset sepsis is associated with the following
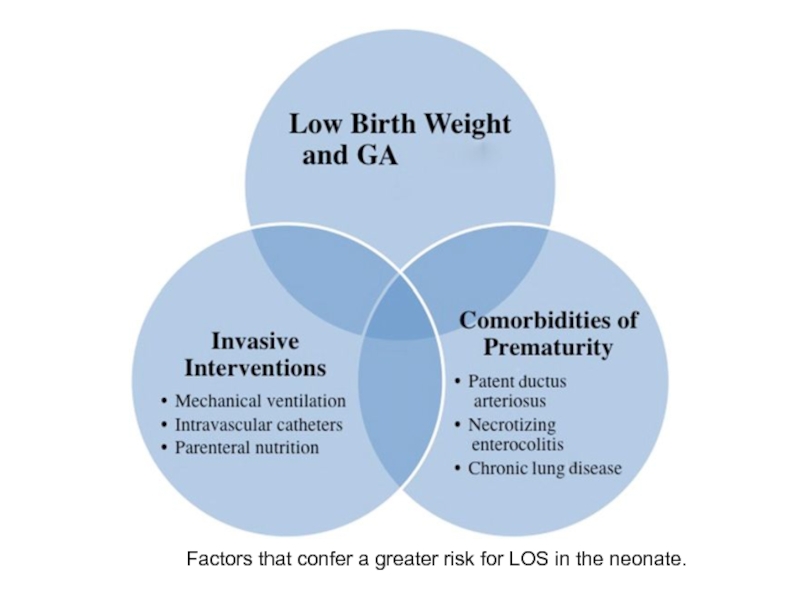
- 12. Factors that confer a greater risk for LOS in the neonate.
- 13. Meningitis The principal pathogens in neonatal
- 14. Meningitis Ventriculitis Arachnoiditis Vasculitis Cerebral edema Infarction
- 15. Epidemiology The incidence of culture-proven sepsis
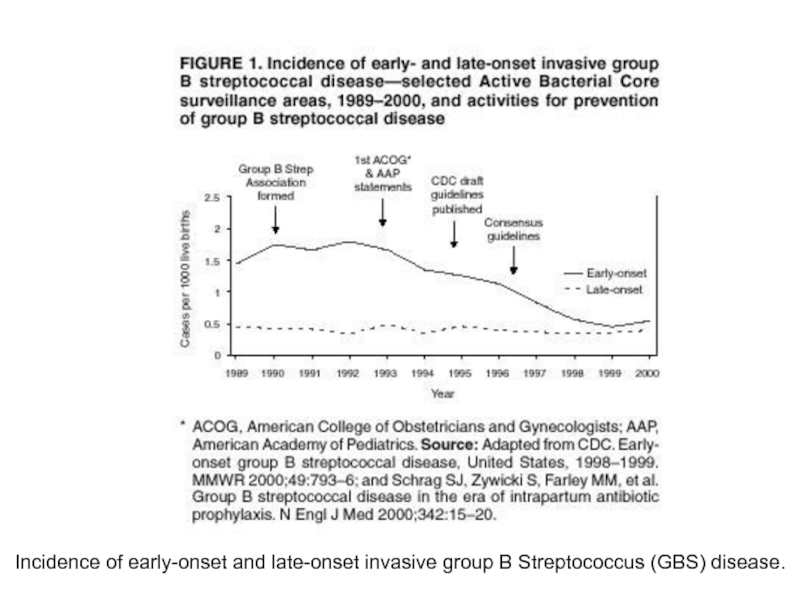
- 16. Incidence of early-onset and late-onset invasive group B Streptococcus (GBS) disease.
- 17. Age-, sex-, and race-related demographics Black
- 18. History Maternal group B Streptococcus (GBS)
- 19. Physical Examination nonspecific clinical signs of
- 20. Signs and symptoms of neonatal infection (most
- 21. Congenital pneumonia and intrauterine infection Tachypnea,
- 22. Cardiac signs In overwhelming sepsis,
- 23. Metabolic signs Hypoglycemia Hyperglycemia metabolic acidosis jaundice
- 24. Neurologic signs Impairment of consciousness (ie,
- 25. Differential Diagnoses Bowel Obstruction in the
- 26. Laboratory studies used to evaluate for sepsis
- 27. Hematologic signs Neutrophil ratios - the immature-to-total
- 28. CSF findings in infective neonatal meningitis
- 29. Approach Considerations When neonatal sepsis is
- 30. Antibiotic Therapy In the United States
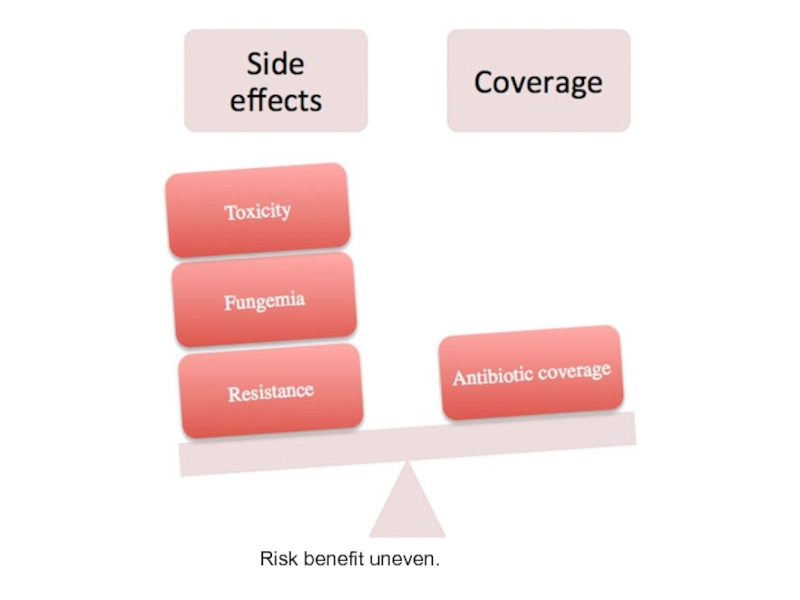
- 31. Risk benefit uneven.
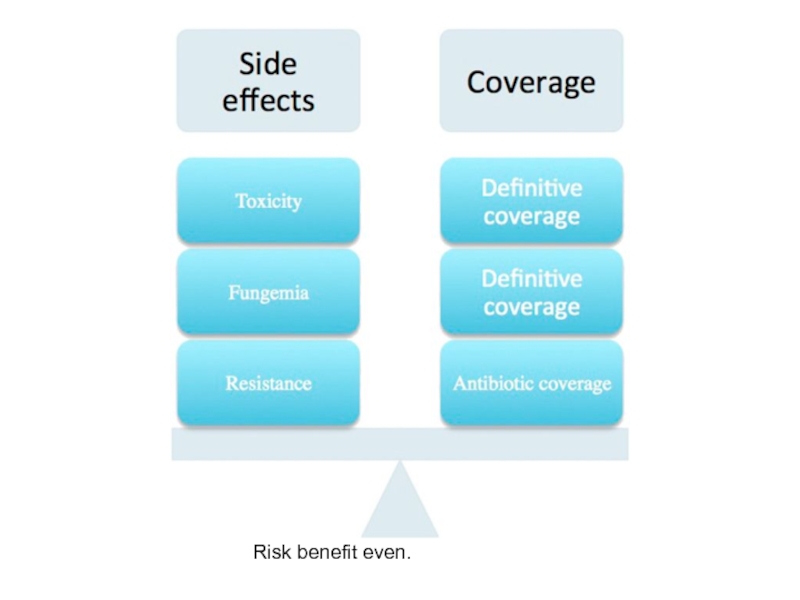
- 32. Risk benefit even.
- 33. The need for continued therapy should be
- 34. Additional therapies that have been investigated for
- 35. Prevention The Committee on Infectious Diseases
- 38. Imaging studies in the workup of neonatal
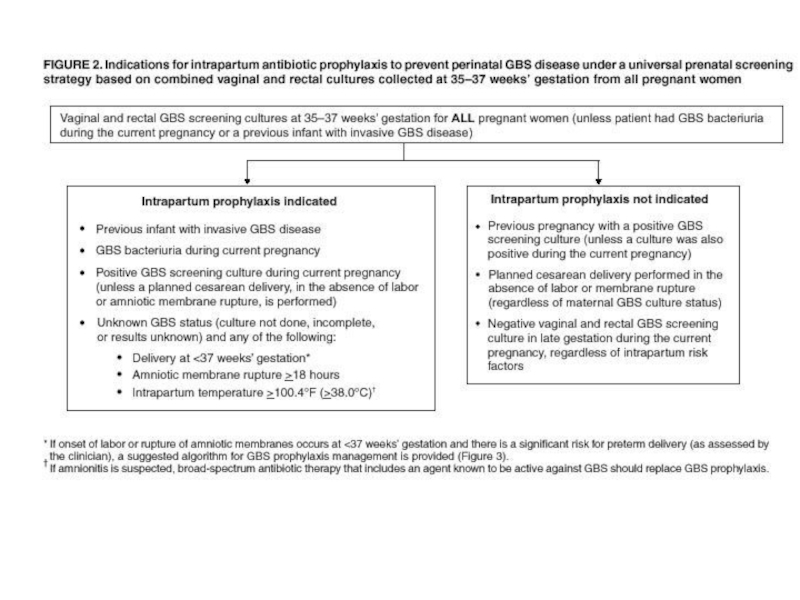
- 39. Algorithm for secondary prevention of early-onset group B Streptococcal disease among newborns.
- 40. Antibiotics Ampicillin Ampicillin is a beta-lactam
- 41. Antibiotics Gentamicin Gentamicin is an aminoglycoside that
- 42. Antibiotics Cefotaxime (Claforan) Cefotaxime is a third-generation
- 43. Antibiotics Vancomycin Vancomycin is a bactericidal agent
- 44. Antibiotics Chloramphenicol Chloramphenicol has been shown to
- 45. Antibiotics Metronidazole (Flagyl) Metronidazole is an antimicrobial
- 46. Antibiotics Erythromycin base (Erythrocin, Ery-Tab, EryPed, E.E.S.)
- 47. Antivirals Acyclovir (Zovirax) Acyclovir is used
- 48. Antifungals Fluconazole (Diflucan) Fluconazole is used
Слайд 2Background
Neonatal sepsis may be categorized as early-onset or late-onset. Of newborns
Onset is most rapid in premature neonates.
Early-onset sepsis is associated with acquisition of microorganisms from the mother.
Late-onset sepsis occurs at 4-90 days of life and is acquired from the caregiving environment.
Слайд 3Pathophysiology
1. Specific microbial factors - The bacterial capsule polysaccharide of Staphylococcus
2. Host factors that predispose the newborn to sepsis
cellular immunity
-neonatal PMNs are deficient in chemotaxis and killing capacity
-neutrophil reserves are easily depleted because of the diminished response of the bone marrow, especially in the premature infant
-Formation of antigen-specific memory function after primary infection is delayed
humoral immunity
-lower levels of immunoglobulins are found with increasing prematurity
-Mature complement activity is not reached until infants are aged 6-10 months.
barrier function.
-Skin and mucous membranes are broken down easily in the premature infant.
-Neonates who are ill, premature, or both are at additional risk because of the invasive procedures that breach their physical barriers to infection.
Слайд 4The microorganisms most commonly associated with early-onset infection
Group B Streptococcus
Escherichia coli
Coagulase-negative Staphylococcus
Haemophilus influenzae
Listeria monocytogenes
Слайд 8The most common risk factors associated with early-onset neonatal sepsis
Maternal
Premature rupture of membranes (PROM)
Preterm rupture of membranes
Prolonged rupture of membranes
Prematurity
Maternal urinary tract infection
Chorioamnionitis
Слайд 9Other factors that are associated with or predispose to early-onset neonatal
Low Apgar score (< 6 at 1 or 5 minutes)
Maternal fever greater than 38°C
Maternal urinary tract infection (UTI)
Poor prenatal care
Poor maternal nutrition
Low socioeconomic status
History of recurrent abortion
Maternal substance abuse
Low birth weight
Difficult delivery
Birth asphyxia
Meconium staining
Congenital anomalies
Слайд 10Organisms that have been implicated in causing late-onset sepsis
Coagulase-negative Staphylococcus
Staphylococcus
E coli
Klebsiella
Pseudomonas
Enterobacter
Candida
GBS
Serratia
Acinetobacter
Anaerobes
Слайд 11Late-onset sepsis is associated with the following risk factors
Prematurity
Central venous
Nasal cannula or continuous positive airway pressure (CPAP) use
H2 -receptor blocker or proton pump inhibitor (PPI) use
GI tract pathology
Слайд 13Meningitis
The principal pathogens in neonatal meningitis are GBS (36% of cases),
S pneumoniae
S aureus
S epidermidis
H influenzae
Pseudomonas species
Klebsiella species
Serratia species
Enterobacter species
Proteus species
Слайд 15Epidemiology
The incidence of culture-proven sepsis in the United States is approximately
Of the 7-13% of neonates who are evaluated for neonatal sepsis, only 3-8% have culture-proven sepsis.
Because early signs of sepsis in the newborn are nonspecific, diagnostic studies are often ordered and treatment initiated in neonates before the presence of sepsis has been proved.
Слайд 17Age-, sex-, and race-related demographics
Black infants have an increased incidence of
In all races, the incidence of bacterial sepsis and meningitis, especially with gram-negative enteric bacilli, is higher in males than in females.
Premature infants have an increased incidence of sepsis.
The risk of death or meningitis from sepsis is higher in infants with low birth weight than in full-term neonates.
Слайд 18History
Maternal group B Streptococcus (GBS) status
Premature rupture of membranes (PROM)
Prematurity
Chorioamnionitis
Слайд 19Physical Examination
nonspecific clinical signs of early sepsis are also associated with
In view of the nonspecificity of these signs, it is prudent to provide treatment for suspected neonatal sepsis while excluding other disease processes.
Слайд 20Signs and symptoms of neonatal infection (most are NONSPECIFIC):
Apnea and
Lethargy, poor color, hypoactivity, poor capillary refill.
Feeding intolerance (more than usual spit-up), abdominal distention.
Clinical appearance; doesn't look "good".
Tachypnea, temperature instability, look of distress.
NO GOLD STANDARD for the diagnosis of neonatal infection
Слайд 21Congenital pneumonia and intrauterine infection
Tachypnea, irregular respirations, moderate retracting, apnea,
The chest radiograph may depict bilateral consolidation or pleural effusions.
Klebsiella species and S aureus are especially likely to generate severe lung damage, producing microabscesses and empyema.
Early onset GBS pneumonia has a particularly fulminant course, with significant mortality in the first 48 hours of life.
Postnatally acquired pneumonia may occur at any age
If the infant has remained hospitalized in an NICU environment, especially with endotracheal intubation and mechanical ventilation, the organisms may include Staphylococcus or Pseudomonas species.
, these hospital-acquired organisms frequently demonstrate multiple antibiotic resistances.
Слайд 22Cardiac signs
In overwhelming sepsis, an initial early phase characterized by pulmonary
This phase is followed by further progressive decreases in cardiac output with bradycardia and systemic hypotension. The infant manifests overt shock with pallor, poor capillary perfusion, and edema.
Слайд 24Neurologic signs
Impairment of consciousness (ie, stupor with or without irritability)
Coma
Seizures
Bulging anterior
Extensor rigidity
Focal cerebral signs
Cranial nerve signs
Nuchal rigidity
Temperature instability
decreased tone
Lethargy
poor feeding
Слайд 25Differential Diagnoses
Bowel Obstruction in the Newborn
Congenital Diaphragmatic Hernia
Congenital Pneumonia
Heart Failure, Congestive
Hemolytic
Meconium Aspiration Syndrome
Necrotizing Enterocolitis
Pericarditis, Bacterial
Pulmonary Hypoplasia
Respiratory Distress Syndrome
Слайд 26Laboratory studies used to evaluate for sepsis
complete blood count (CBC)
blood and cerebrospinal fluid (CSF) cultures
measurement of levels of C-reactive protein (CRP) and other infection markers.
Coagulation studies (DIC - abnormalities in the prothrombin time (PT), the partial thromboplastin time (PTT), and fibrinogen and D-dimer levels)
Слайд 27Hematologic signs
Neutrophil ratios - the immature-to-total (I/T) ratio is the most
-the maximum acceptable ratio for excluding sepsis during the first 24 hours is 0.16.
-An I:T ratio of >0.2 has been considered abnormal
-Disseminated intravascular coagulation (DIC):abnormalities in prothrombin time (PT), partial thromboplastin time (PTT), and fibrinogen and D-dimer levels
If infants show signs consistent with impaired coagulation, including gastric blood, bleeding from intravenous or laboratory puncture sites, or other bleeding, evaluating coagulation by checking these values is important.
Слайд 28CSF findings in infective neonatal meningitis
Elevated WBC count (predominantly PMNs)
Elevated
Decreased glucose concentration
Positive culture results
Слайд 29Approach Considerations
When neonatal sepsis is suspected, treatment should be initiated immediately
Begin antibiotics as soon as diagnostic tests are performed
Monitoring of blood pressure, vital signs, hematocrit, platelets, and coagulation studies is vital.
An infant with temperature instability needs thermoregulatory support with a radiant warmer or incubator.
Слайд 30Antibiotic Therapy
In the United States and Canada, the current approach to
This provides coverage for gram-positive organisms, especially group B Streptococcus (GBS), and gram-negative bacteria, such as Escherichia coli.
If an infection appears to be nosocomial (late-onset sepsis), antibiotic coverage should be directed at organisms implicated in hospital-acquired infections, including S aureus, S epidermidis, and Pseudomonas species. Vancomycin and oxacillin has been favored for this coverage
Aminoglycosides and vancomycin both have the potential to produce ototoxicity and nephrotoxicity and should therefore be used with caution.
Слайд 33The need for continued therapy should be based not on the
Culture results
Maternal and intrapartum risk factors
CSF results
Complete blood cell (CBC) count and differential
C-reactive protein (CRP) trends
Radiographs
Clinical progress
Слайд 34Additional therapies that have been investigated for the treatment of neonatal
Granulocyte transfusion
IVIg infusion
Exchange transfusion
Recombinant cytokine administration
Слайд 35Prevention
The Committee on Infectious Diseases of the AAP recommends that obstetric
Women with GBS bacteriuria should be treated during pregnancy when the condition is diagnosed and during the intrapartum period.
Слайд 38Imaging studies in the workup of neonatal sepsis
chest radiography to
computed tomography (CT)
magnetic resonance imaging (MRI)
ultrasonography of the head in cases of meningitis.
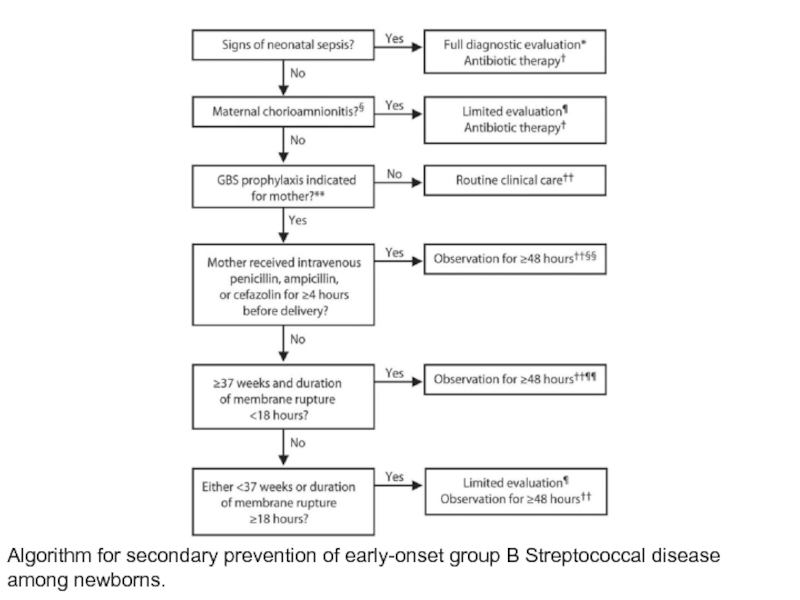
Слайд 39Algorithm for secondary prevention of early-onset group B Streptococcal disease among
Слайд 40Antibiotics
Ampicillin
Ampicillin is a beta-lactam antibiotic that is bactericidal for susceptible
Слайд 41Antibiotics
Gentamicin
Gentamicin is an aminoglycoside that is bactericidal for susceptible gram-negative organisms,
Слайд 42Antibiotics
Cefotaxime (Claforan)
Cefotaxime is a third-generation cephalosporin with excellent in vitro activity
Слайд 43Antibiotics
Vancomycin
Vancomycin is a bactericidal agent that is effective against most aerobic
Слайд 44Antibiotics
Chloramphenicol
Chloramphenicol has been shown to be effective in the treatment of
Oxacillin
Oxacillin is a bactericidal antibiotic that inhibits cell wall synthesis. It is used in the treatment of infections caused by penicillinase-producing staphylococci. It may be given as initial therapy when a staphylococcal infection is suspected.
Слайд 45Antibiotics
Metronidazole (Flagyl)
Metronidazole is an antimicrobial that has been shown to be
Piperacillin
Piperacillin is an acylampicillin with excellent activity against Pseudomonas aeruginosa. It is also effective against Klebsiella pneumoniae, Proteus mirabilis, B fragilis, Serratia marcescens, and many strains of Enterobacter. Administer it in combination with an aminoglycoside.
Слайд 46Antibiotics
Erythromycin base (Erythrocin, Ery-Tab, EryPed, E.E.S.)
Erythromycin is a macrolide antimicrobial agent
Trimethoprim/sulfamethoxazole (Bactrim DS, Septra DS)
Trimethoprim-sulfamethoxazole has been shown to be effective in the treatment of highly resistant bacterial meningitis. Trimethoprim-sulfamethoxazole inhibits bacterial growth by inhibiting the synthesis of dihydrofolic acid. Trimethoprim-sulfamethoxazole should not be used if hyperbilirubinemia and kernicterus are of concern in the newborn.
Слайд 47Antivirals
Acyclovir (Zovirax)
Acyclovir is used for treatment of mucosal, cutaneous, and
Zidovudine (Retrovir)
Zidovudine is a thymidine analogue that inhibits viral replication. It is used to treat patients with HIV infection.
Слайд 48Antifungals
Fluconazole (Diflucan)
Fluconazole is used to treat susceptible fungal infections, including
Amphotericin B (AmBisome)
Amphotericin B is used to treat severe systemic infections and meningitis caused by susceptible fungi, such as Candida and Aspergillus species, Histoplasma capsulatum, and Cryptococcus neoformans. This agent is a polyene produced by a strain of Streptomyces nodosus; it can be fungistatic or fungicidal. Amphotericin B binds to sterols, such as ergosterol, in the fungal cell membrane, causing intracellular components to leak and subsequent fungal cell death.
Liposomal amphotericin B (AmBisome) may be considered for patients with systemic fungal infections resistant to amphotericin B or for patients with renal or hepatic failure. This product consists of amphotericin B within a single-bilayer liposomal drug delivery system.