- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Alloimmune hemolytic disease of the fetus. Newborn: Rh Isoimmunization презентация
Содержание
- 1. Alloimmune hemolytic disease of the fetus. Newborn: Rh Isoimmunization
- 2. The Antibodies Arise In The Mother As
- 3. Antibodies That May Be Detected During Pregnancy:
- 4. ISO: is a prefix means similar, equal
- 5. RhD D negativity primarily occurs among Caucasians;
- 6. The RH Antigen – Biochemical and
- 7. The RH Antigen – Biochemical and Genetic Aspects
- 8. The Rh Antigen- Biochemical Aspects: The
- 9. The RH Antigen- Genetic Aspect The
- 10. Grades Of “Positively” Due To Variation In
- 11. Incomplete Expression Of The D Antigen Result
- 12. Factors Affect The Expression Of The Rh
- 14. Mechanism of Development of Maternal Rh Isoimmunization
- 15. The Mechanism of Development of the Rh
- 16. The Primary Response: Is a
- 17. Exposure to maternal antigen in utero “the
- 21. Natural History of Maternal isoimmunization /HD of the Newborn
- 22. Without treatment: less than 20% of
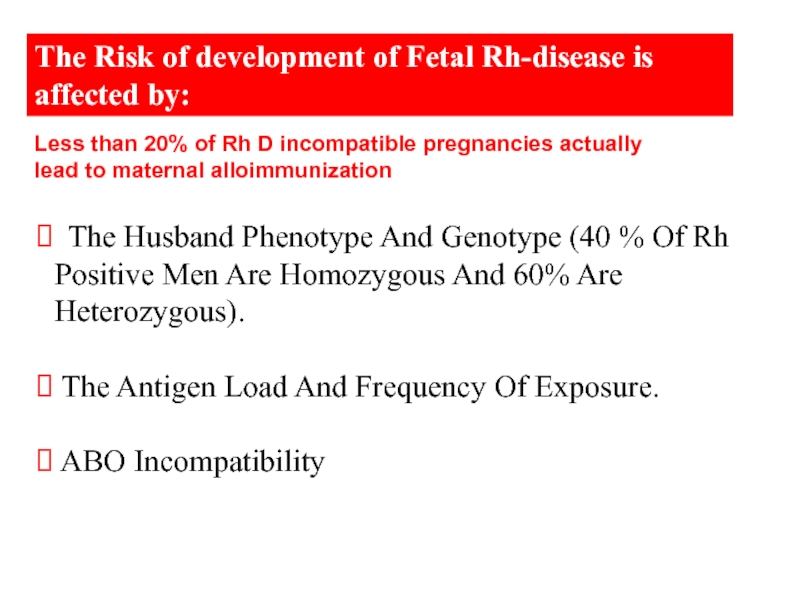
- 23. The Risk of development of Fetal Rh-disease
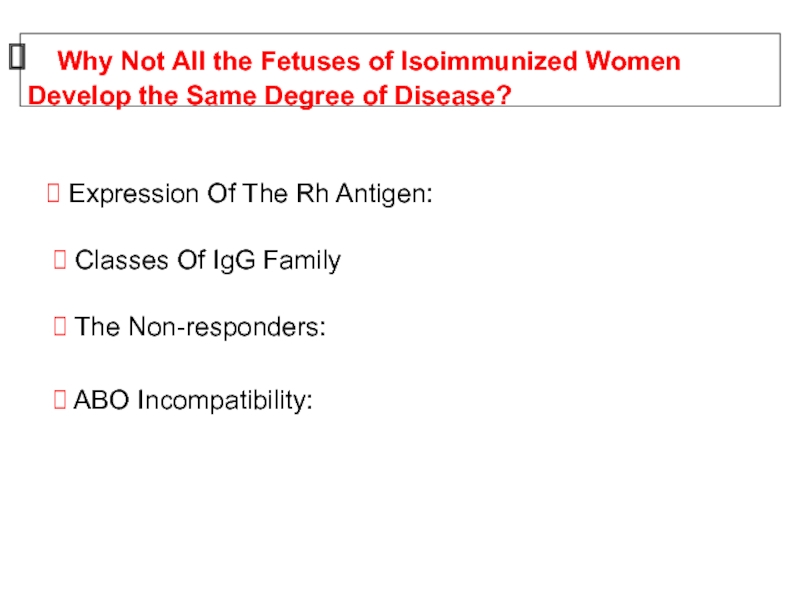
- 24. Why Not All the Fetuses
- 25. Pathogenesis of Fetal Erythroblastosis Fetalis
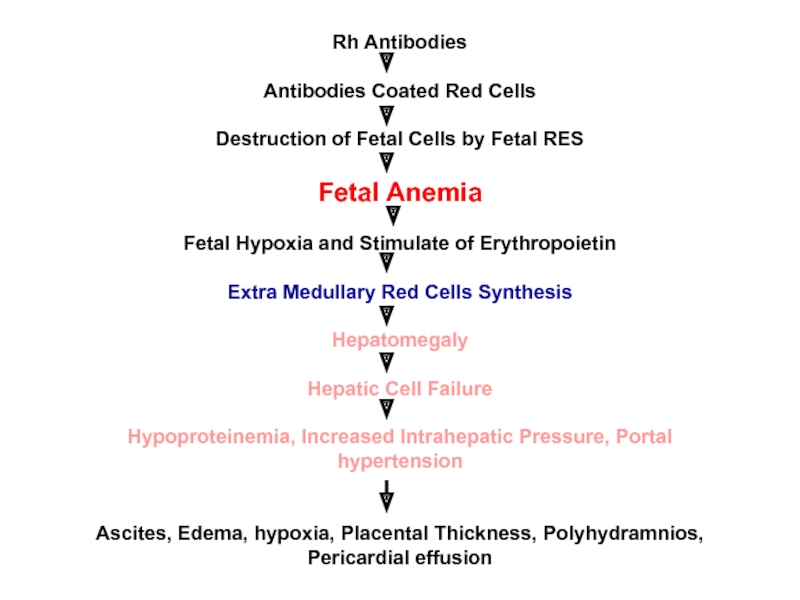
- 26. Rh Antibodies Antibodies Coated Red Cells
- 27. Complications of Fetal-Neonatal Anemia: Fetal Hydrops
- 28. Management - Prevention: Treatment:
- 29. Prevention of Rh Isoimmunization Screening all
- 30. 10 mcg of anti-D Ig should be
- 31. Most polyclonal RhiG comes from male volunteers
- 32. The amount of fetal cells in maternal blood: The Kleihauer-Braun-Betke Test
- 33. Management of cases of Rh isoimmunization Diagnosis Of RH Isoimmunization Evaluation of Fetal Condition
- 34. Diagnosis of Rh isoimmunization The diagnose is
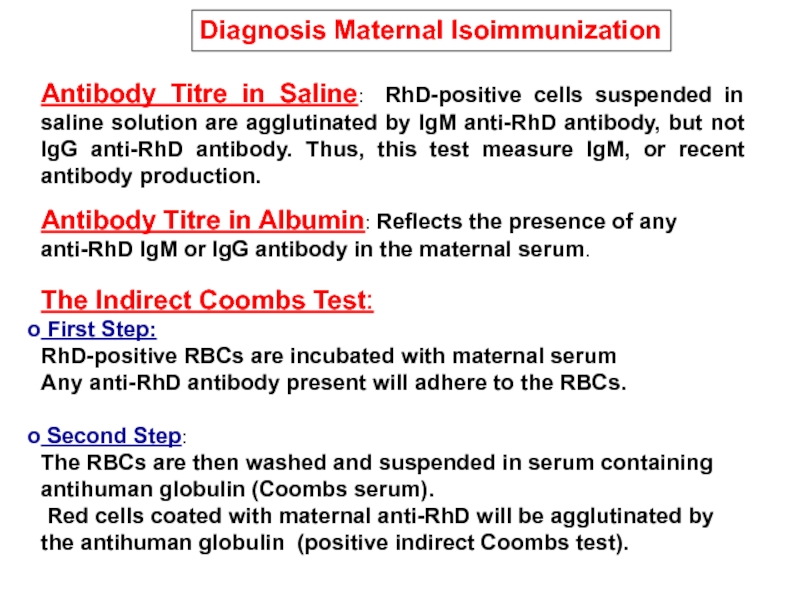
- 35. Antibody Titre in Saline: RhD-positive cells suspended
- 36. Is Done After Birth To Detect The
- 37. Fetal Rhesus Determination RHD Type And
- 38. Management of cases of Rh isoimmunization Diagnosis Of RH Isoimmunization Evaluation of Fetal Condition
- 39. Initially detecting fetal
- 40. Evaluation of Fetal Condition Measurements Of
- 41. Although not reliably accurate in predicting
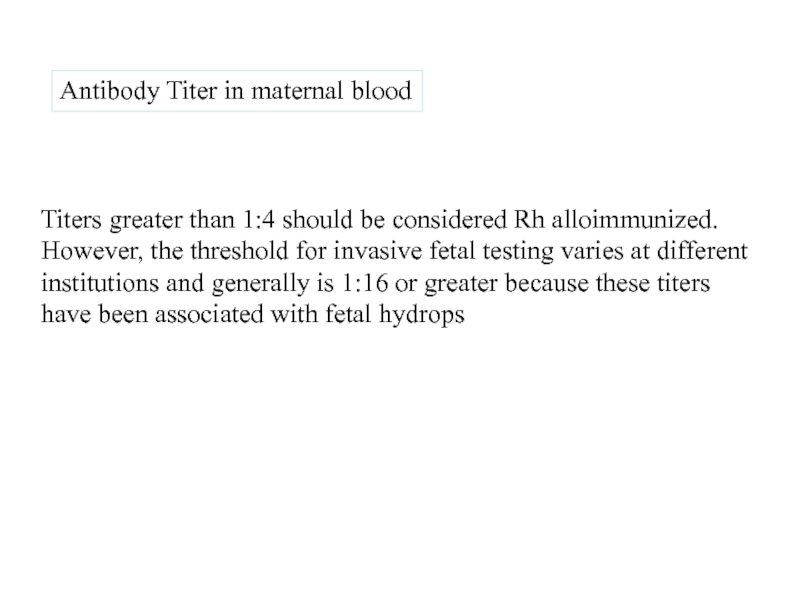
- 42. Maternal Anti-D Titer Antibody Titer
- 43. Ultrasound Image of Transabdominal Chorion Villus Sampling
- 44. To Establish The Correct Gestational Age.
- 45. Anemic Fetus Preserves Oxygen Delivery To The
- 46. Previous Seriously Affected Fetus
- 47. Amniocentesis Normally Bilirubin In Amniotic Fluid
- 48. Ultrasound image of amniocentesis at 16 weeks of gestation
- 49. Extended Liley graph.
- 50. Queenan curve (Deviation in amniotic fluid optical
- 51. Interpretation Of Amniotic Fluid Bilirubin:
- 52. Is the gold standard for detection of
- 53. Diagram of cordocentesis procedure Cordocentesis
- 54. Cordocentesis
- 55. Suggested management of the RhD-sensitized pregnancy
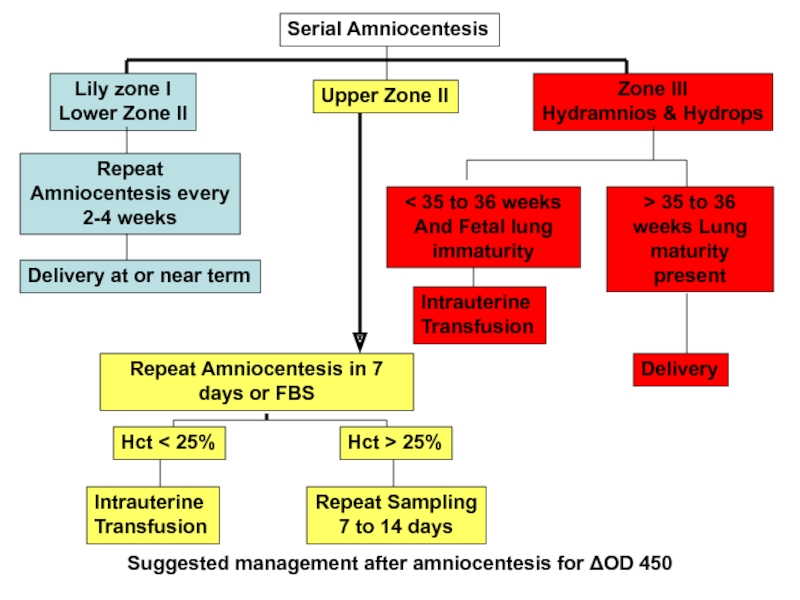
- 56. Suggested management after amniocentesis for ΔOD 450
- 57. Ultrasound-guided transabdominal fetocentesis
- 58. Titers greater than 1:4 should be
- 59. Because the wavelength at which bilirubin
- 60. Changes Since Introduction of Anti-D
- 61. DIAGNOSIS Blood and Rh(D) typing and
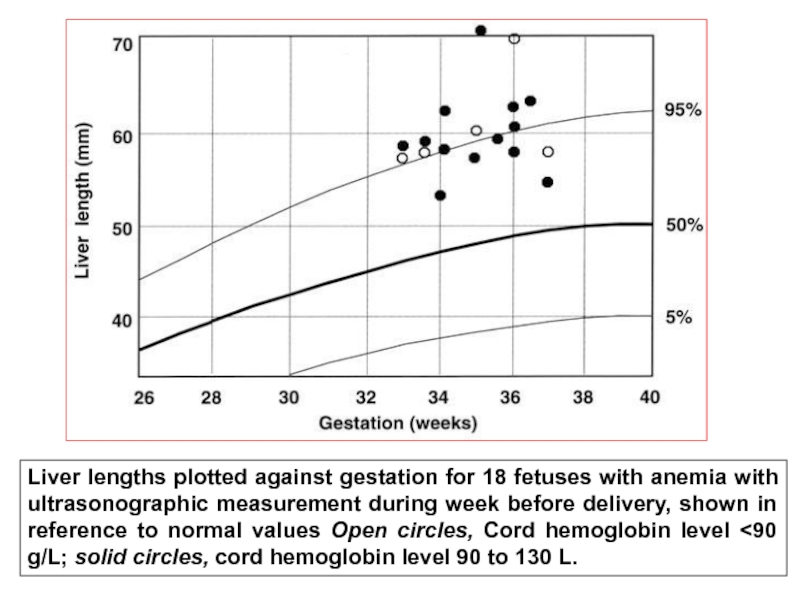
- 62. Liver lengths plotted against gestation for 18
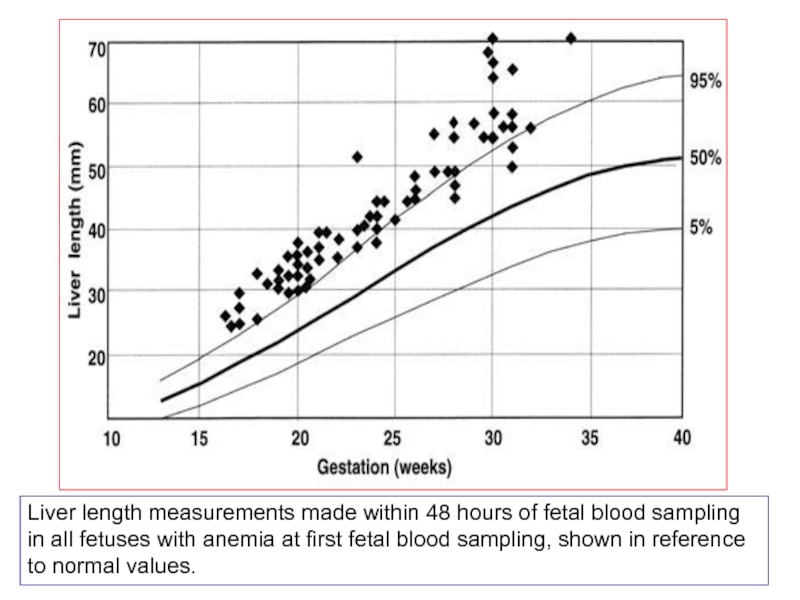
- 63. Liver length measurements made within 48 hours
Слайд 1Alloimmune Hemolytic Disease Of The Fetus / Newborn:
Rh Isoimmunization
Professor Hassan A
Department of Obstetrics and Gynecology
Faculty of Medicine
King Abdul-Aziz University
Слайд 2The Antibodies Arise In The Mother As The Direct Result Of
The mother become Isoimmunized.
In The Fetus: Erythroblastosis Fetalis
In The Newborn: HDN.
Alloimmune Hemolytic Disease Of The Fetus / Newborn:
Definition:
A condition in which the Red Cells Of The Fetus Or Newborn Are Destroyed By Maternally Derived Alloantibodies
Слайд 3Antibodies That May Be Detected During Pregnancy:
Innocuous Antibodies:
Most
Antibodies Capable Of Causing Significant Hemolytic Transfusion Reactions:
IgG antibodies, Their Corresponding Antigens Are Not Well Developed At Birth E.g. Lu (b), Yt (a), And VEL —
Antibodies That Are Responsible For HDN :
Anti-c, Anti-d, Anti-e, And Anti-k (Kell)
Слайд 4ISO: is a prefix means similar, equal or uniform.
Isoimmunization: is the
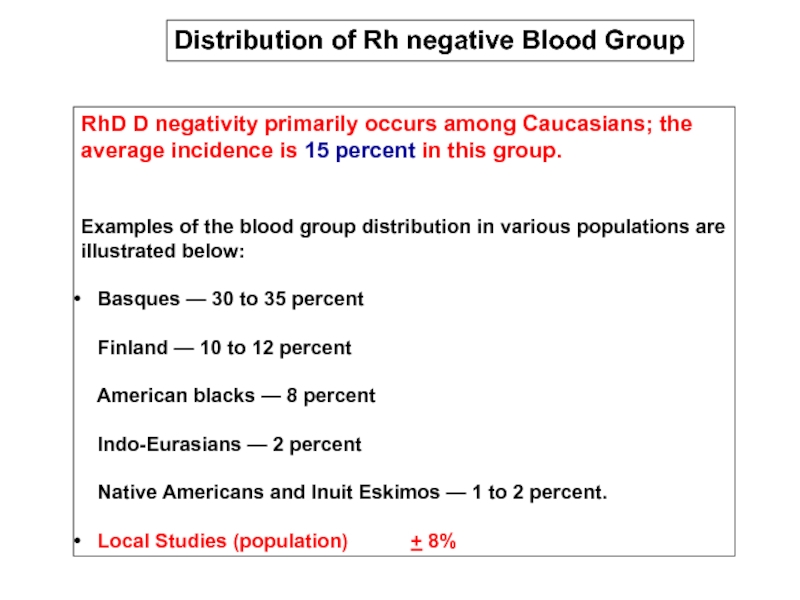
Слайд 5RhD D negativity primarily occurs among Caucasians; the average incidence is
Examples of the blood group distribution in various populations are illustrated below:
Basques — 30 to 35 percent Finland — 10 to 12 percent American blacks — 8 percent Indo-Eurasians — 2 percent Native Americans and Inuit Eskimos — 1 to 2 percent.
Local Studies (population) + 8%
Distribution of Rh negative Blood Group
Слайд 6 The RH Antigen – Biochemical and Genetic Aspects
Mechanism of
Natural History of Maternal isoimmunization /HD of the Newborn
Pathogenesis of Fetal Erythroblastosis Fetalis
Diagnosis of Rh isoimmunization
Слайд 8The Rh Antigen- Biochemical Aspects:
The Rh Antigen Is A Complex
It Can Not Be Seen By Routine Microscopy, But Can Be Identified By Specific Antisera
Function of the Rh antigen:
Its Precise Function Is Unknown.
Rh Null Erythrocytes Have Increased Osmotic Fragility And Abnormal Shapes.
Слайд 9The RH Antigen- Genetic Aspect
The Rh gene complex is located
A given Rh antigen complex is determined by a specific gene sequence inherited in a Mendelian fashion from the parents. one haploid from the mother and one from the father.
Three genetic loci, determine the Rh antigen (i.e. Rh blood group).
Each chromosome will be either D positive or D negative (there is no "d" antigen), C or c positive, and E or e positive.
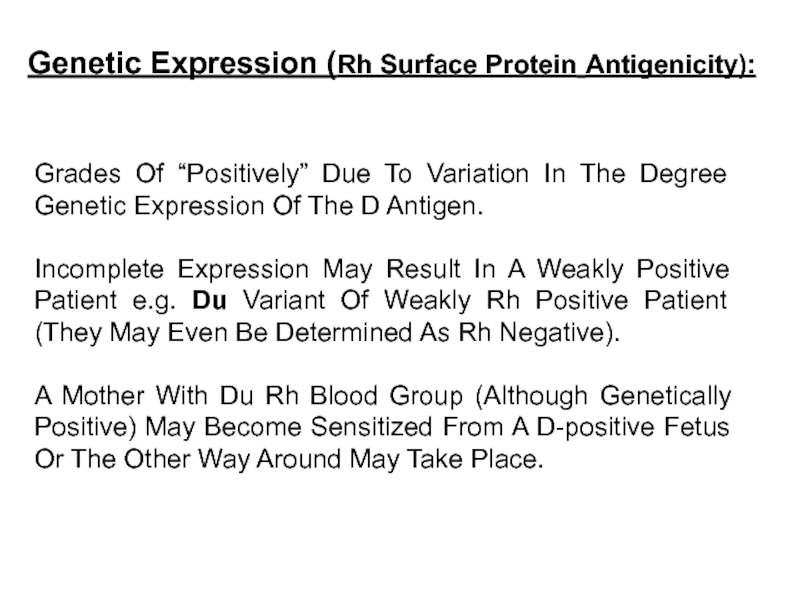
Слайд 10Grades Of “Positively” Due To Variation In The Degree Genetic Expression
Incomplete Expression May Result In A Weakly Positive Patient e.g. Du Variant Of Weakly Rh Positive Patient (They May Even Be Determined As Rh Negative).
A Mother With Du Rh Blood Group (Although Genetically Positive) May Become Sensitized From A D-positive Fetus Or The Other Way Around May Take Place.
Genetic Expression (Rh Surface Protein Antigenicity):
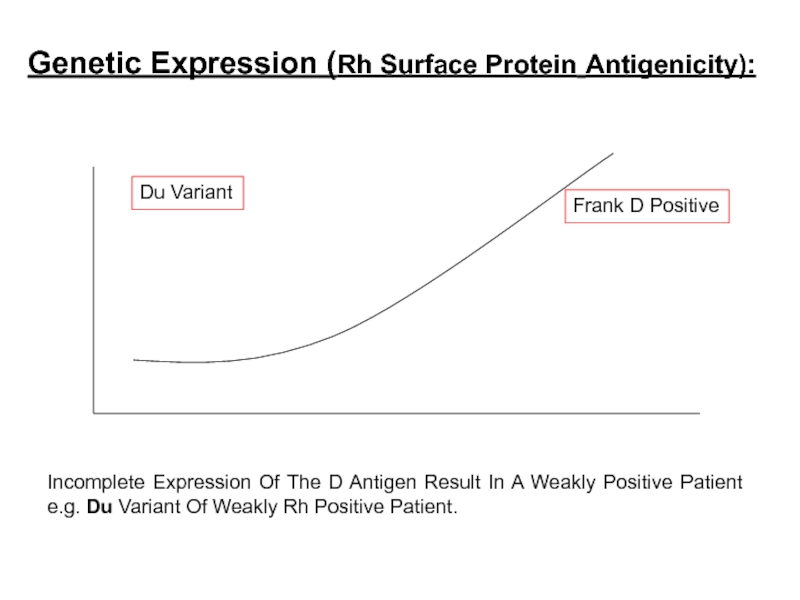
Слайд 11Incomplete Expression Of The D Antigen Result In A Weakly Positive
Genetic Expression (Rh Surface Protein Antigenicity):
Du Variant
Frank D Positive
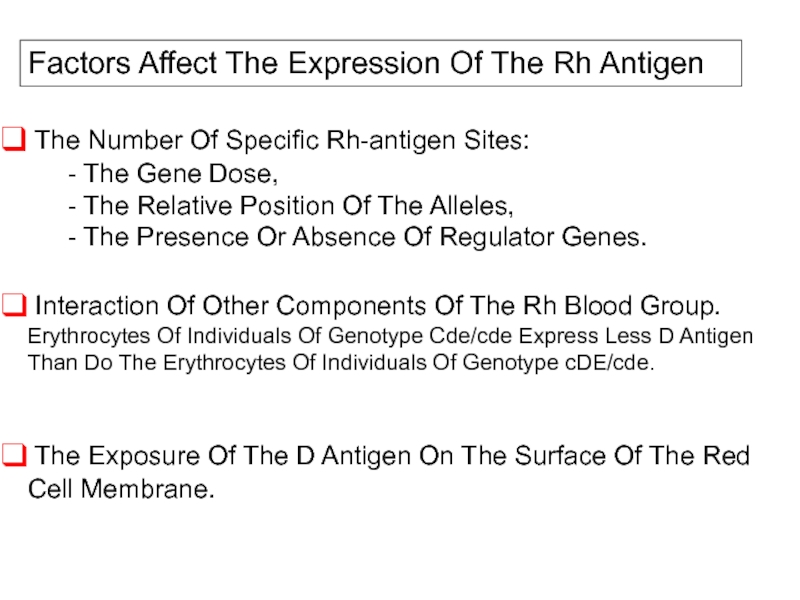
Слайд 12Factors Affect The Expression Of The Rh Antigen
The Number Of
- The Gene Dose,
- The Relative Position Of The Alleles,
- The Presence Or Absence Of Regulator Genes.
Interaction Of Other Components Of The Rh Blood Group. Erythrocytes Of Individuals Of Genotype Cde/cde Express Less D Antigen Than Do The Erythrocytes Of Individuals Of Genotype cDE/cde.
The Exposure Of The D Antigen On The Surface Of The Red Cell Membrane.
Слайд 13
D
c
E
e
C
d
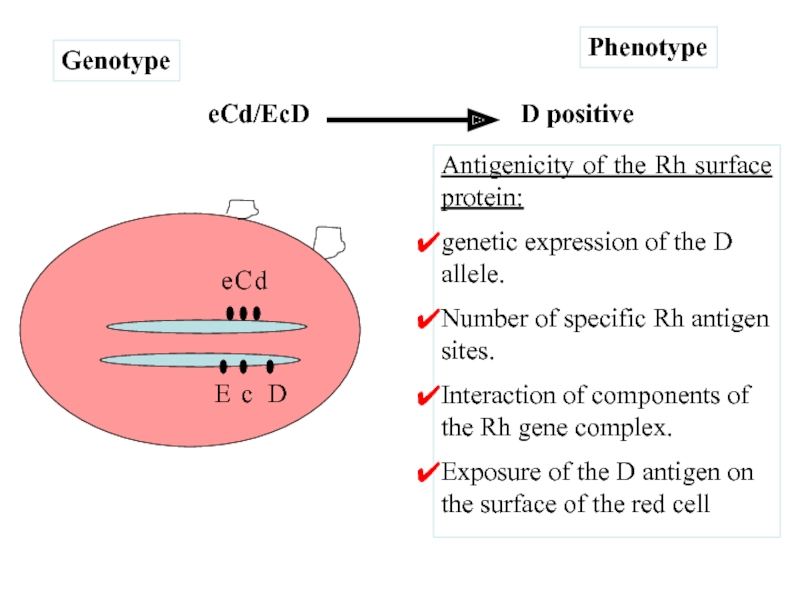
eCd/EcD
Phenotype
Genotype
D positive
Antigenicity of the Rh surface protein:
genetic expression of the D
Number of specific Rh antigen sites.
Interaction of components of the Rh gene complex.
Exposure of the D antigen on the surface of the red cell
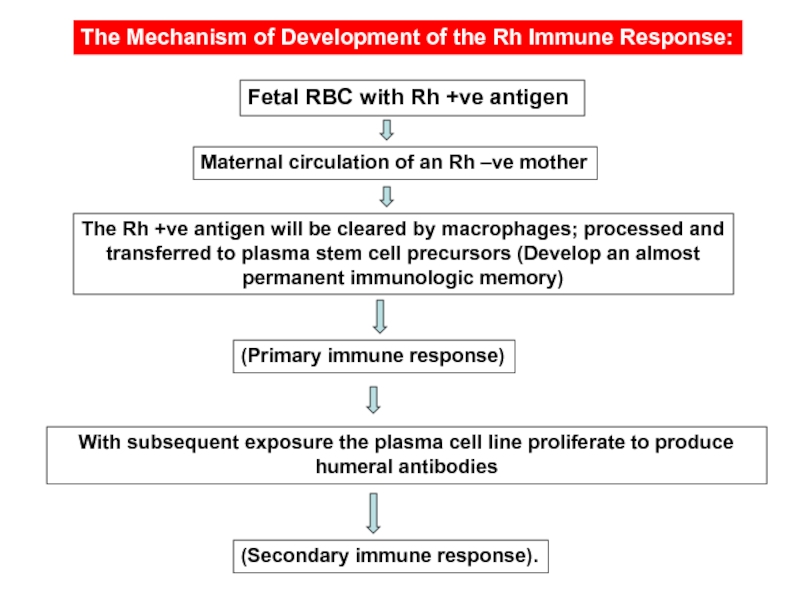
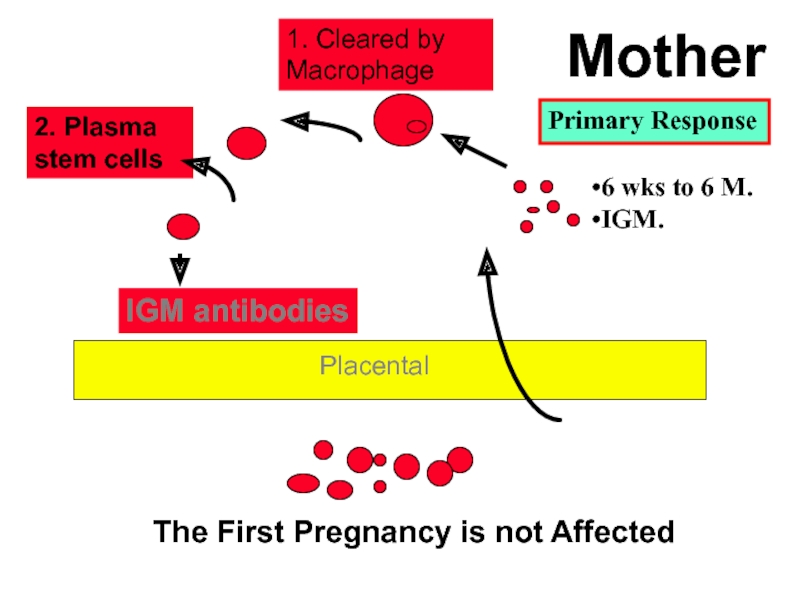
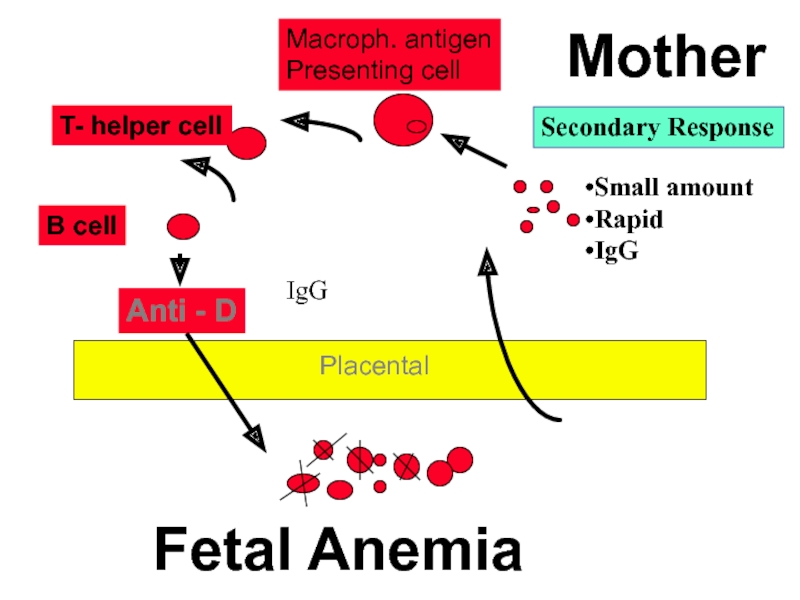
Слайд 15The Mechanism of Development of the Rh Immune Response:
Fetal RBC with
Maternal circulation of an Rh –ve mother
(Primary immune response)
The Rh +ve antigen will be cleared by macrophages; processed and transferred to plasma stem cell precursors (Develop an almost permanent immunologic memory)
With subsequent exposure the plasma cell line proliferate to produce humeral antibodies
(Secondary immune response).
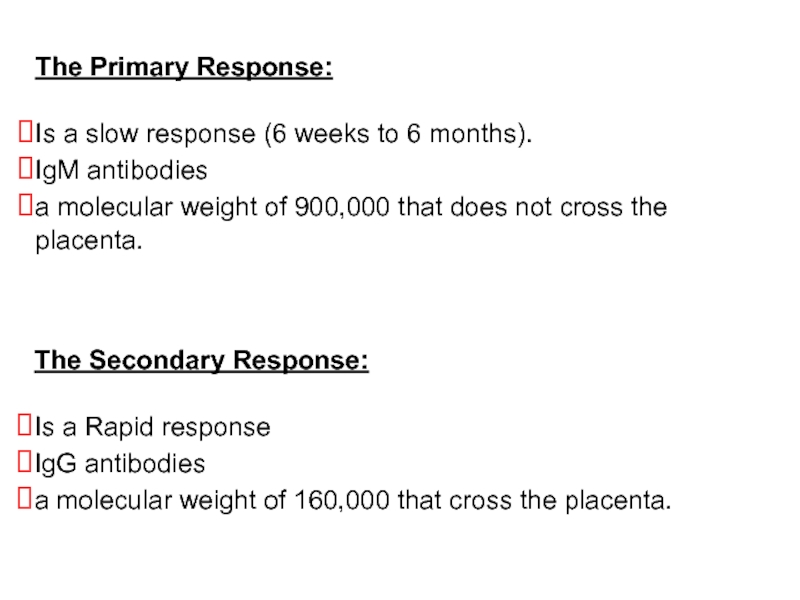
Слайд 16The Primary Response:
Is a slow response (6 weeks to 6
IgM antibodies
a molecular weight of 900,000 that does not cross the placenta.
The Secondary Response:
Is a Rapid response
IgG antibodies
a molecular weight of 160,000 that cross the placenta.
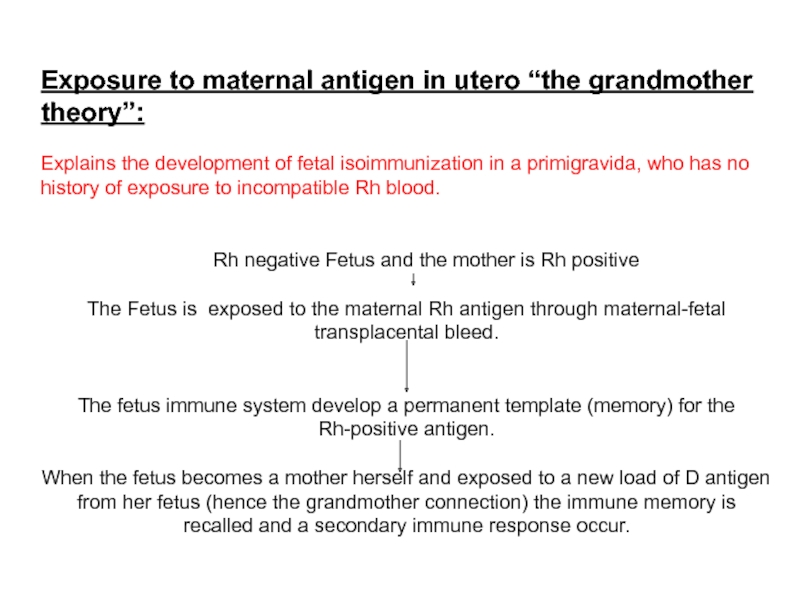
Слайд 17Exposure to maternal antigen in utero “the grandmother theory”:
Explains the development
Rh negative Fetus and the mother is Rh positive
The Fetus is exposed to the maternal Rh antigen through maternal-fetal transplacental bleed.
The fetus immune system develop a permanent template (memory) for the Rh-positive antigen.
When the fetus becomes a mother herself and exposed to a new load of D antigen from her fetus (hence the grandmother connection) the immune memory is recalled and a secondary immune response occur.
Слайд 18
IGM antibodies
1. Cleared by Macrophage
2. Plasma stem cells
The First Pregnancy is
Mother
Placental
Primary Response
6 wks to 6 M.
IGM.
Слайд 19
Anti - D
Macroph. antigen
Presenting cell
T- helper cell
B cell
Fetal Anemia
Mother
Placental
Secondary Response
Small amount
Rapid
IgG
IgG
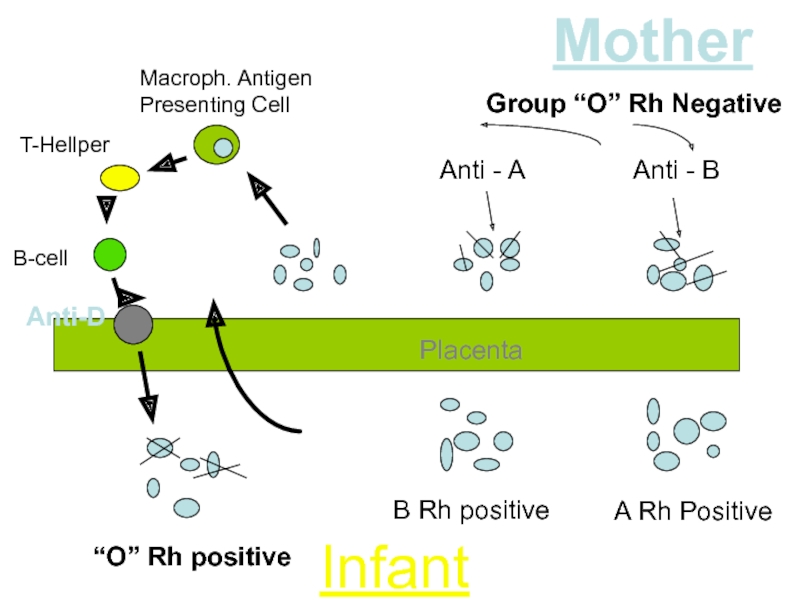
Слайд 20
Macroph. Antigen
Presenting Cell
T-Hellper
B-cell
Anti-D
Anti - A
Anti - B
Mother
Infant
B Rh positive
A Rh Positive
“O”
Group “O” Rh Negative
Placenta
Слайд 22Without treatment:
less than 20% of Rh D incompatible pregnancies actually
25-30% of the offspring will have some degree of hemolytic anemia and hyperbilirubinemia.
20-25% will be hydropic and often will die either in utero or in the neonatal period.
Cases of hemolysis in the newborn that do not result in fetal hydrops still can lead to kernicterus.
Natural History of Rh Isoimmunization And HD Fetus and Newborn
Слайд 23The Risk of development of Fetal Rh-disease is affected by:
The
The Antigen Load And Frequency Of Exposure.
ABO Incompatibility
Less than 20% of Rh D incompatible pregnancies actually
lead to maternal alloimmunization
Слайд 24 Why Not All the Fetuses of Isoimmunized Women Develop
The Non-responders:
ABO Incompatibility:
Expression Of The Rh Antigen:
Classes Of IgG Family
Слайд 26Rh Antibodies
Antibodies Coated Red Cells
Destruction of Fetal Cells by Fetal RES
Fetal
Fetal Hypoxia and Stimulate of Erythropoietin
Extra Medullary Red Cells Synthesis
Hepatomegaly
Hepatic Cell Failure
Hypoproteinemia, Increased Intrahepatic Pressure, Portal hypertension
Ascites, Edema, hypoxia, Placental Thickness, Polyhydramnios, Pericardial effusion
Слайд 27Complications of Fetal-Neonatal Anemia:
Fetal Hydrops And IUFD
Hepatosplenomegaly
Neonatal
Compilations Of Neonatal Kernicterus (Lethargy, Hypertonicity, Hearing Loss, Cerebral Palsy And Learning Disability)
Neonatal Anemia
Слайд 29Prevention of Rh Isoimmunization
Screening all women for D Factor and
Prophylaxis (Anti D Immunoglobulin) only for those who are negative for antibodies
The dose of Immunoglobulin depends the volume of Blood
Anti D Is given 72 hours after delivery, 28-32 weeks, and any other time when there is risk of Fetomaternal Bleeding
Слайд 3010 mcg of anti-D Ig should be administered for every mL
Thus, the 300-mcg dose covers hemorrhage volumes up to 30 mL of whole fetal blood.
In the less than 1% of cases where the volume of fetomaternal hemorrhage exceeds 30 mL, utilizing the Kleihauer-Betke test to quantitate the volume of fetal blood in the maternal circulation and administer the appropriate amount of anti-D.
Dose of prophylactic Anti-D Ig:
Слайд 31Most polyclonal RhiG comes from male volunteers who are intentionally exposed
Potential Problems:
infectious risk
solve supply problems.
ethical issues
MONOCLONAL ANTI-D
anti-D monoclonal antibody:
Although monoclonal anti-D is promising, it cannot be recommended at this time as a replacement for polyclonal RhIg.
Слайд 33Management of cases of Rh isoimmunization
Diagnosis Of RH Isoimmunization
Evaluation of Fetal
Слайд 34Diagnosis of Rh isoimmunization
The diagnose is Based on the presence of
The Enzymatic Method
The Antibody Titer In Saline, In Albumin
The Indirect Coombs Tests.
Methods of Detecting Anti D Antibodies in Maternal Serum:
Слайд 35Antibody Titre in Saline: RhD-positive cells suspended in saline solution are
Antibody Titre in Albumin: Reflects the presence of any anti-RhD IgM or IgG antibody in the maternal serum.
The Indirect Coombs Test:
First Step:
RhD-positive RBCs are incubated with maternal serum
Any anti-RhD antibody present will adhere to the RBCs.
Second Step:
The RBCs are then washed and suspended in serum containing antihuman globulin (Coombs serum).
Red cells coated with maternal anti-RhD will be agglutinated by the antihuman globulin (positive indirect Coombs test).
Diagnosis Maternal Isoimmunization
Слайд 36Is Done After Birth To Detect The Presence Of Maternal Antibody
The Infant's RBCs Are Placed In Coombs Serum.
If The Cells Are Agglutinated This Indicate The Presence Of Maternal Antibody
The Direct Coombs Test
Слайд 37Fetal Rhesus Determination
RHD Type And Zygosity (If RHD-positive) Of The
Amniocentesis To Determine The Fetal Blood Type Using The Polymerase Chain Reaction (PCR)
Detection Of Free Fetal RHD DNA (FDNA) Sequences In Maternal Plasma Or Serum Using PCR
Flow Cytometry Of Maternal Blood For Fetal Cells
Слайд 38Management of cases of Rh isoimmunization
Diagnosis Of RH Isoimmunization
Evaluation of Fetal
Слайд 39
Initially detecting fetal anemia prior to the occurrence of
Minimize fetal morbidity and mortality by correcting this anemia until fetal lung maturity and delivery can be achieved.
Goals of managing Fetal Alloimmunization:
Слайд 40Evaluation of Fetal Condition
Measurements Of Antibodies in Maternal Serum
Determination
Ultrasonography
Amniocentesis
Fetal Blood Sampling
Past Obstetric History
Слайд 41
Although not reliably accurate in predicting severity of fetal disease, past
Past Obstetric History:
Слайд 42Maternal Anti-D Titer
Antibody Titer Is A Screening Test.
A
Variation In Titer Results Between Laboratories And Intra Laboratory Is Common.
A Truly Stable Titer Should Not Vary By More Than One Dilution When Repeated In A Given Laboratory.
Слайд 44 To Establish The Correct Gestational Age.
In Guiding Invasive
Ultrasonographic Parameters To Determine Fetal Anemia:
Placental Thickness.
Umbilical Vein Diameter
Hepatic Size.
Splenic Size.
Polyhydramnios.
Fetal Hydrops (e.g. Ascites, Pleural Effusions, Skin Edema).
Ultrasonography:
Слайд 45Anemic Fetus Preserves Oxygen Delivery To The Brain By Increasing Cerebral
Doppler Velocimetry Of The Fetal Middle Cerebral Artery (MCA)
To Predict The Timing Of A Second Intrauterine Fetal Transfusion.
For Predicting Fetal Anemia
Слайд 46
Previous Seriously Affected Fetus Or Infant
(e.g. Intrauterine Fetal Transfusion,
A Critical Anti-D Titer:
I.E. A Titer Associated With A Significant Risk For Fetal Hydrops. Anti-D Titer Value Between 8 And 32
Invasive Techniques
( Amniocentesis and Fetal Blood Sampling):
Indications:
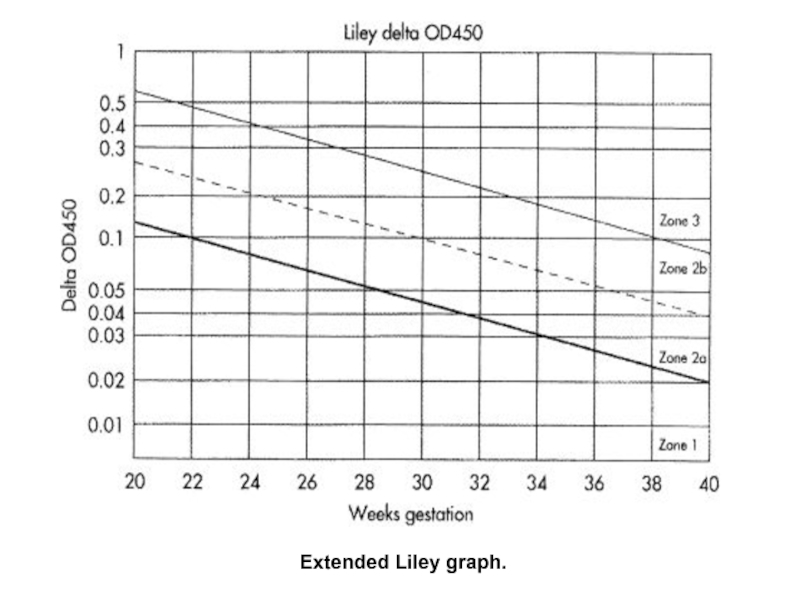
Слайд 47Amniocentesis
Normally Bilirubin In Amniotic Fluid Decreases With Advanced Gestation.
It
Its Level Rises in Correlation With Fetal Hemolysis.
Determination Of Amniotic Fluid Bilirubin:
By The Analysis Of The Change In Optical Density Of Amniotic Fluid At 450 nm On The Spectral Absorption Curve (delta OD450)
Procedures Are Undertaken At 10-15 Days Intervals Until Delivery Data Are Plotted On A Normative Curve Based Upon Gestational Age.
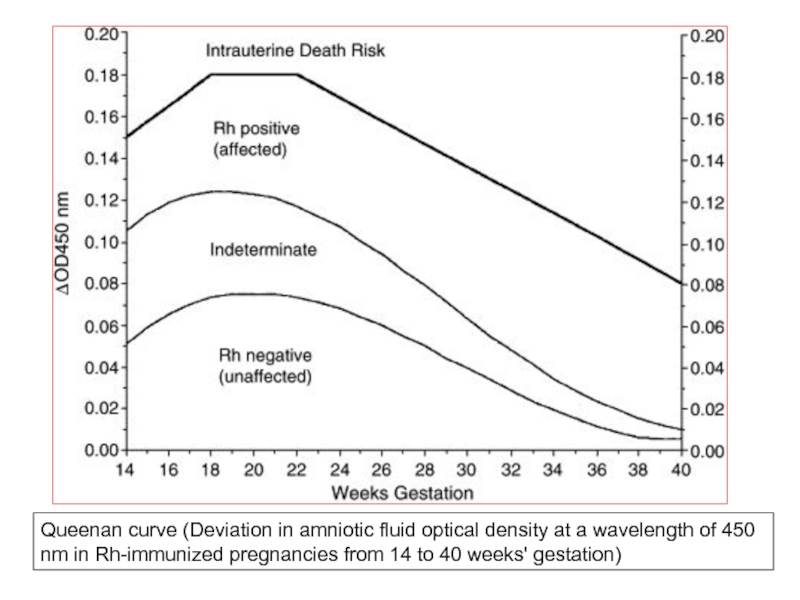
Слайд 50Queenan curve (Deviation in amniotic fluid optical density at a wavelength
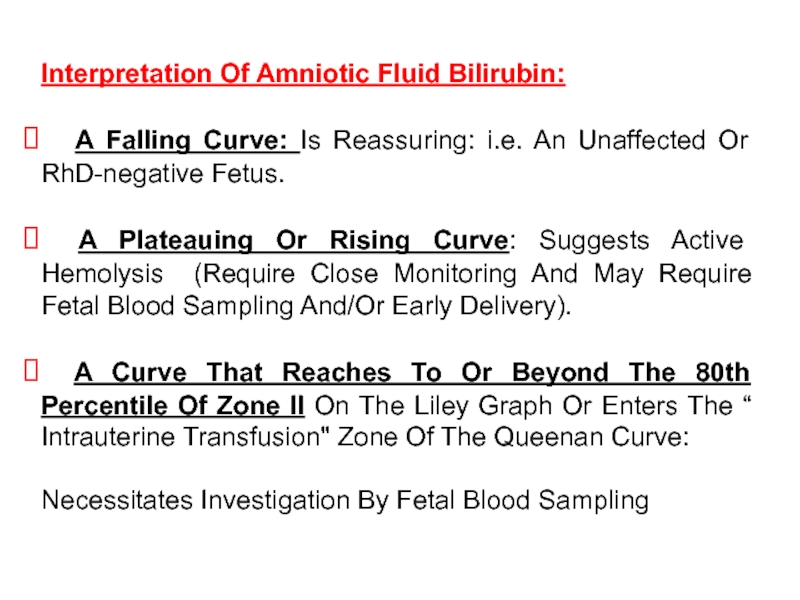
Слайд 51Interpretation Of Amniotic Fluid Bilirubin:
A Falling Curve: Is Reassuring: i.e.
A Plateauing Or Rising Curve: Suggests Active Hemolysis (Require Close Monitoring And May Require Fetal Blood Sampling And/Or Early Delivery).
A Curve That Reaches To Or Beyond The 80th Percentile Of Zone II On The Liley Graph Or Enters The “ Intrauterine Transfusion" Zone Of The Queenan Curve:
Necessitates Investigation By Fetal Blood Sampling
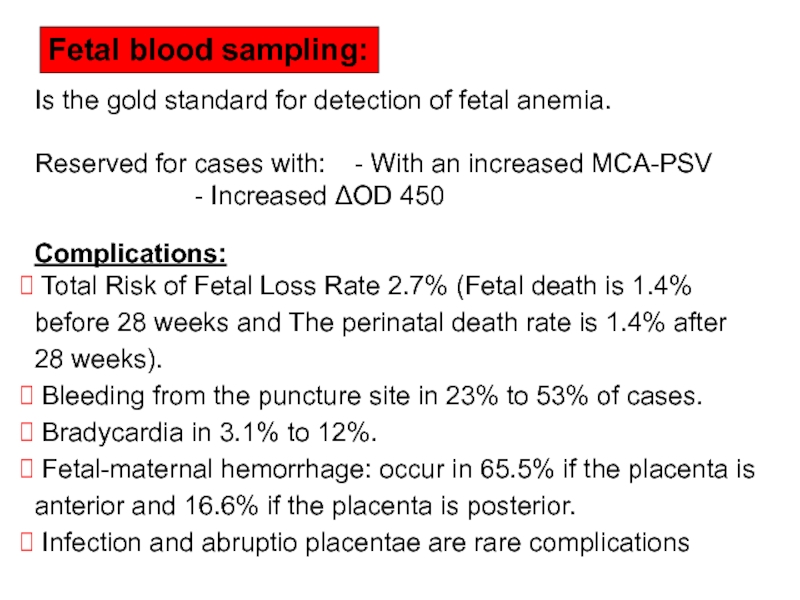
Слайд 52Is the gold standard for detection of fetal anemia.
Reserved for
- Increased ΔOD 450
Complications:
Total Risk of Fetal Loss Rate 2.7% (Fetal death is 1.4% before 28 weeks and The perinatal death rate is 1.4% after 28 weeks).
Bleeding from the puncture site in 23% to 53% of cases.
Bradycardia in 3.1% to 12%.
Fetal-maternal hemorrhage: occur in 65.5% if the placenta is anterior and 16.6% if the placenta is posterior.
Infection and abruptio placentae are rare complications
Fetal blood sampling:
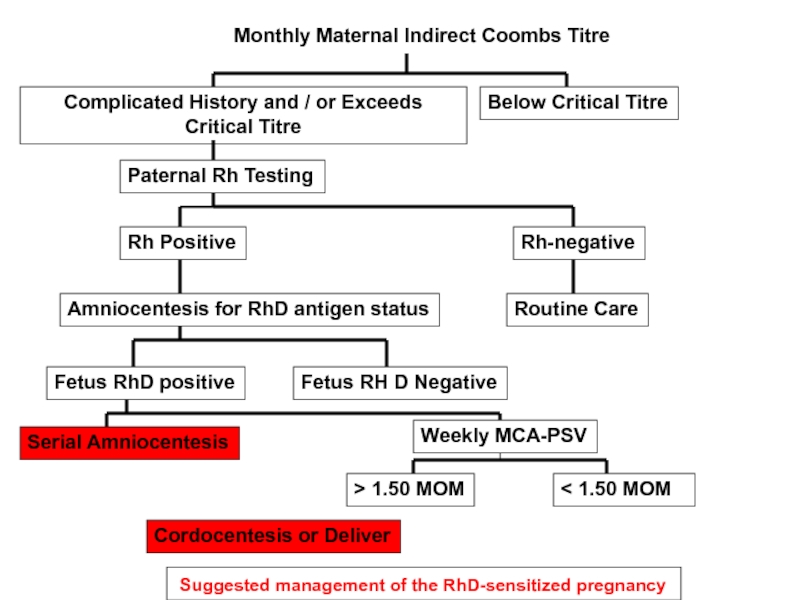
Слайд 55 Suggested management of the RhD-sensitized pregnancy
Monthly Maternal Indirect Coombs Titre
Below
Complicated History and / or Exceeds Critical Titre
Paternal Rh Testing
Rh Positive
Rh-negative
Amniocentesis for RhD antigen status
Routine Care
Fetus RhD positive
Fetus RH D Negative
Serial Amniocentesis
Weekly MCA-PSV
< 1.50 MOM
Cordocentesis or Deliver
> 1.50 MOM
Слайд 56Suggested management after amniocentesis for ΔOD 450
Serial Amniocentesis
Lily zone I
Lower
Upper Zone II
Zone III
Hydramnios & Hydrops
Repeat Amniocentesis every 2-4 weeks
Delivery at or near term
Repeat Amniocentesis in 7 days or FBS
Hct < 25%
Hct > 25%
Intrauterine
Transfusion
Repeat Sampling
7 to 14 days
< 35 to 36 weeks
And Fetal lung immaturity
> 35 to 36 weeks Lung maturity present
Intrauterine
Transfusion
Delivery
Слайд 58
Titers greater than 1:4 should be considered Rh alloimmunized. However, the
Antibody Titer in maternal blood
Слайд 59
Because the wavelength at which bilirubin absorbs light is 420-460 nm,
Modification of the Liley curve to adjust for the relative inaccuracy of D OD 450 readings in early-to-middle second trimester and the use of serial measurements has improved its accuracy.
spectrophotometric measurements of bilirubin in amniotic fluid