- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
- Юриспруденция
Опыт 30 радикальных простатэктомий презентация
Содержание
- 1. Опыт 30 радикальных простатэктомий
- 2. К этому нам еще предстоит пройти!
- 3. Лапароскопическая простатэктомия
- 4. Quality of Life after Radical Prostatectomy or
- 5. Variations in Morbidity after Radical Prostatectomy Colin
- 6. Наиболее значимые факторы для РП Стадия заболевания
- 7. Критерии оценки проведенной операции Время до появления
- 8. Необходимо помнить ! Для стадии Т1 и
- 9. Prevalence of Prostate Cancer among Men with
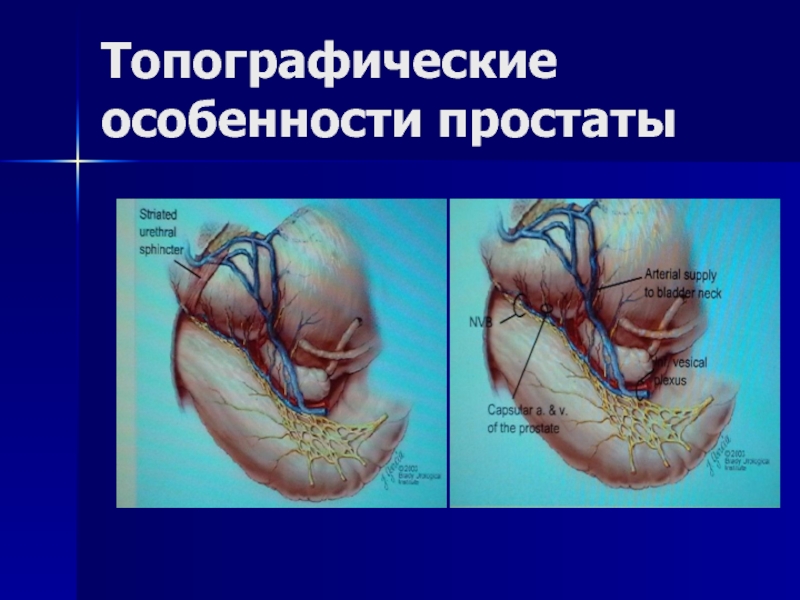
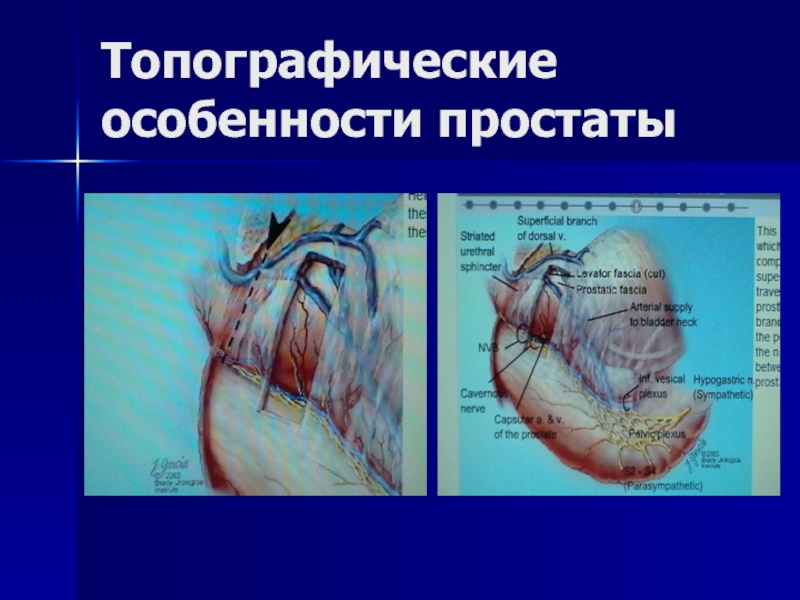
- 10. Топогрфо - анатомические особенности простаты
- 11. Топографические особенности простаты
- 12. Топографические особенности простаты
- 13. Топографические особенности простаты
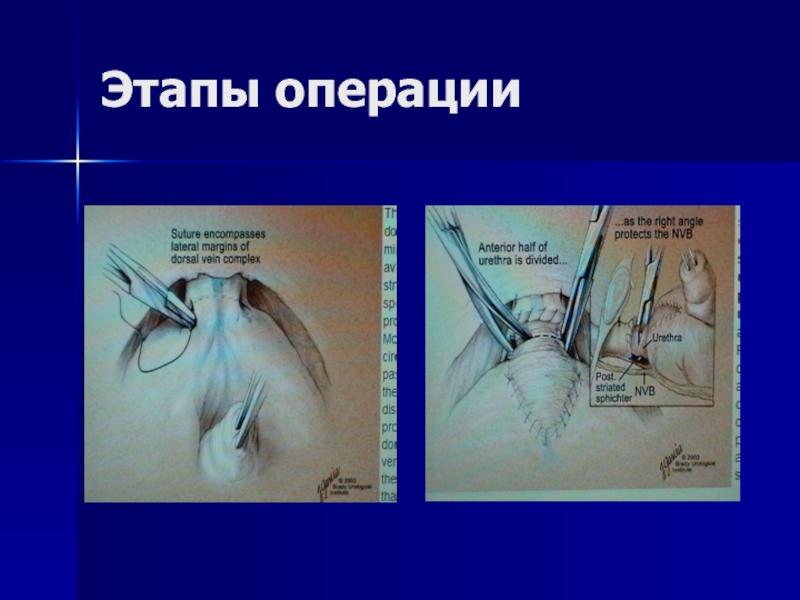
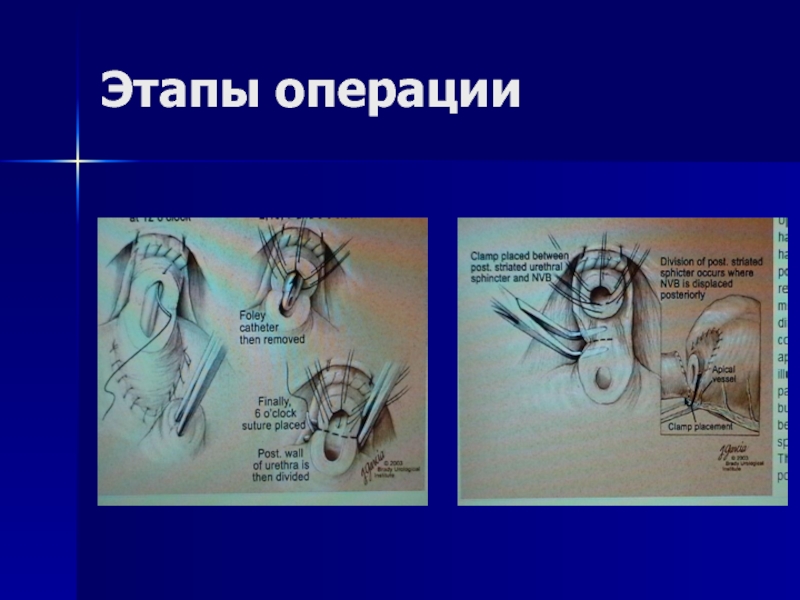
- 14. Этапы операции
- 15. Этапы операции
- 16. Ближайшие послеоперационные осложнения Интраоперационное кровотечение-3,33% (1) Несостоятельность уретровезикального анастомоза-13,3%(4) Раневая инфекция-0 Уретерогидронефроз-6,6%(2) Летальность-0%
- 17. Поздние осложнения Недержание мочи-0% Импотенция-56,6%(17) Стриктура анастомоза-6,6(2) Рецидив на месте-0% Метастазирование опухоли-0%
- 18. Анализ осложнений – предотвращение кровопотери Отработка техники
- 19. Анализ осложнений : травма устьев Бережное «вылущивание»
- 20. Анализ осложнений : несостоятельность анастомоза Для предотвращения
- 21. Анализ осложнений : недержание мочи Необходимо предварительное
- 22. Анализ осложнений : импотенция Недостаточность опыта в
- 23. Выводы Радикальная простатвезикулэктомия при правильном отборе больных
- 24. Выводы Нормализация уровня ПСА и отсутствие признаков
- 25. Рекомендации Считаю целесообразным проведение неоадьювантной гормонотерапии у
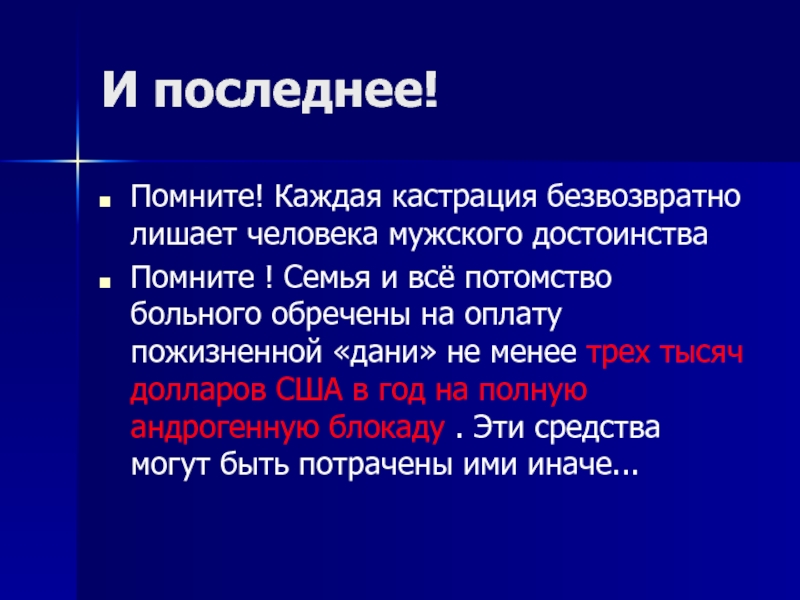
- 26. И последнее! Помните! Каждая кастрация безвозвратно лишает
Слайд 1Опыт 30 радикальных простатэктомий
Научно-практический руководитель урологической клиники МЦ «Эребуни»
Д.м.н. Арутюнян Е.С.
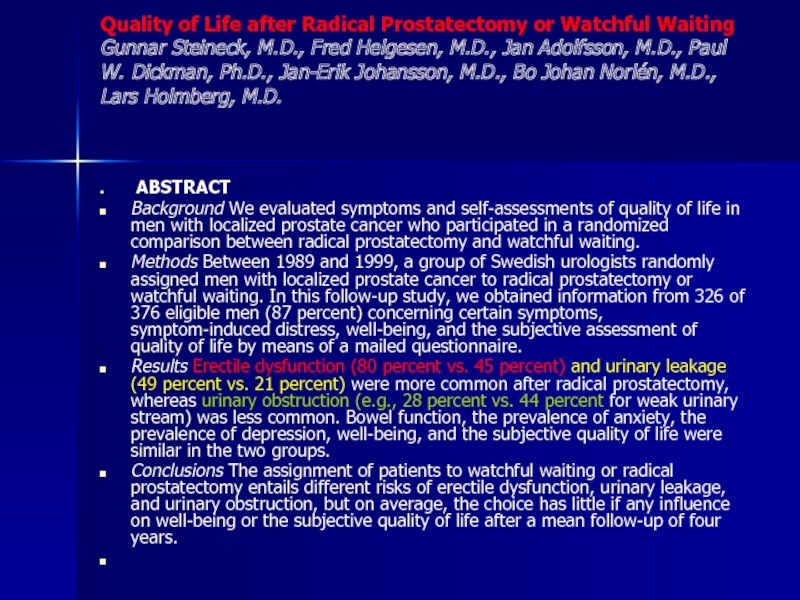
Слайд 4Quality of Life after Radical Prostatectomy or Watchful Waiting Gunnar Steineck, M.D.,
ABSTRACT
Background We evaluated symptoms and self-assessments of quality of life in men with localized prostate cancer who participated in a randomized comparison between radical prostatectomy and watchful waiting.
Methods Between 1989 and 1999, a group of Swedish urologists randomly assigned men with localized prostate cancer to radical prostatectomy or watchful waiting. In this follow-up study, we obtained information from 326 of 376 eligible men (87 percent) concerning certain symptoms, symptom-induced distress, well-being, and the subjective assessment of quality of life by means of a mailed questionnaire.
Results Erectile dysfunction (80 percent vs. 45 percent) and urinary leakage (49 percent vs. 21 percent) were more common after radical prostatectomy, whereas urinary obstruction (e.g., 28 percent vs. 44 percent for weak urinary stream) was less common. Bowel function, the prevalence of anxiety, the prevalence of depression, well-being, and the subjective quality of life were similar in the two groups.
Conclusions The assignment of patients to watchful waiting or radical prostatectomy entails different risks of erectile dysfunction, urinary leakage, and urinary obstruction, but on average, the choice has little if any influence on well-being or the subjective quality of life after a mean follow-up of four years.
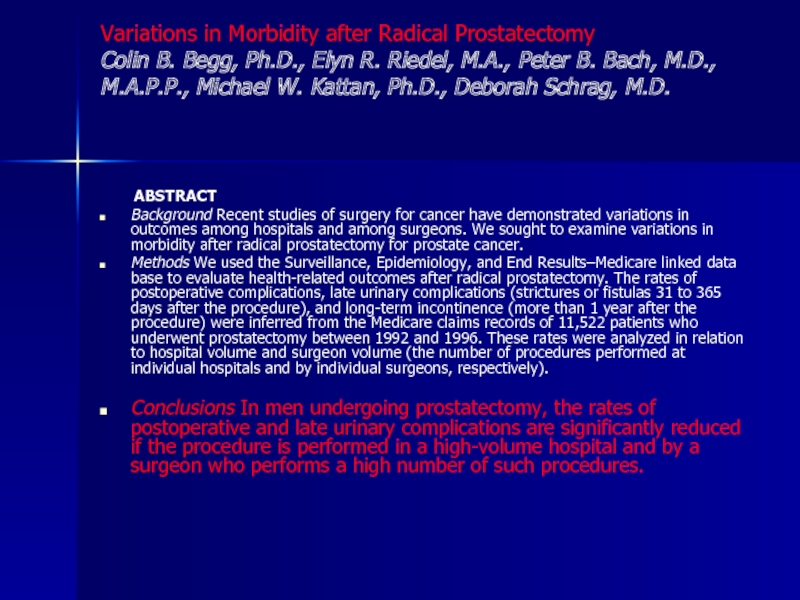
Слайд 5Variations in Morbidity after Radical Prostatectomy Colin B. Begg, Ph.D., Elyn R.
ABSTRACT
Background Recent studies of surgery for cancer have demonstrated variations in outcomes among hospitals and among surgeons. We sought to examine variations in morbidity after radical prostatectomy for prostate cancer.
Methods We used the Surveillance, Epidemiology, and End Results–Medicare linked data base to evaluate health-related outcomes after radical prostatectomy. The rates of postoperative complications, late urinary complications (strictures or fistulas 31 to 365 days after the procedure), and long-term incontinence (more than 1 year after the procedure) were inferred from the Medicare claims records of 11,522 patients who underwent prostatectomy between 1992 and 1996. These rates were analyzed in relation to hospital volume and surgeon volume (the number of procedures performed at individual hospitals and by individual surgeons, respectively).
Conclusions In men undergoing prostatectomy, the rates of postoperative and late urinary complications are significantly reduced if the procedure is performed in a high-volume hospital and by a surgeon who performs a high number of such procedures.
Слайд 6Наиболее значимые факторы для РП
Стадия заболевания
Ожидаемая продолжительность жизни больного
Степень злокачественности опухоли
Выбор
Знание анатомии таза
Высокий профессионализм и обученность «команды»
Слайд 7Критерии оценки проведенной операции
Время до появления признаков прогрессирования болезни (появление отдаленных
Динамика уровня простатспецифического антигена
Оценка качества мочеиспускания по данным урофлоуметрии.
Наличие местного рецидива в зоне операции
Слайд 8Необходимо помнить !
Для стадии Т1 и Т2 нет «золотого» стандарта в
Ищите рак при низких уровнях ПСА, пограничных с «нормой»,-это залог успеха радикальной простатэктомии
Клиническая стадия на ступень ниже окончательного диагноза
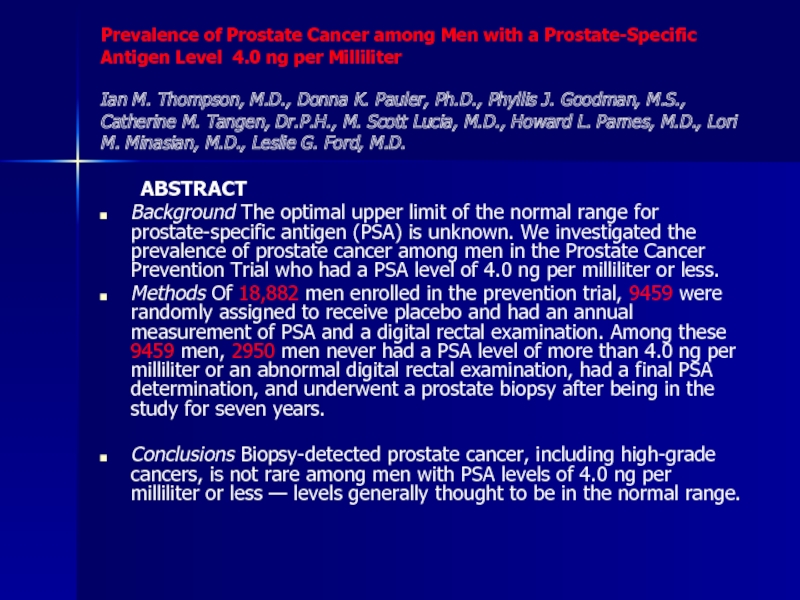
Слайд 9Prevalence of Prostate Cancer among Men with a Prostate-Specific Antigen Level
ABSTRACT
Background The optimal upper limit of the normal range for prostate-specific antigen (PSA) is unknown. We investigated the prevalence of prostate cancer among men in the Prostate Cancer Prevention Trial who had a PSA level of 4.0 ng per milliliter or less.
Methods Of 18,882 men enrolled in the prevention trial, 9459 were randomly assigned to receive placebo and had an annual measurement of PSA and a digital rectal examination. Among these 9459 men, 2950 men never had a PSA level of more than 4.0 ng per milliliter or an abnormal digital rectal examination, had a final PSA determination, and underwent a prostate biopsy after being in the study for seven years.
Conclusions Biopsy-detected prostate cancer, including high-grade cancers, is not rare among men with PSA levels of 4.0 ng per milliliter or less — levels generally thought to be in the normal range.
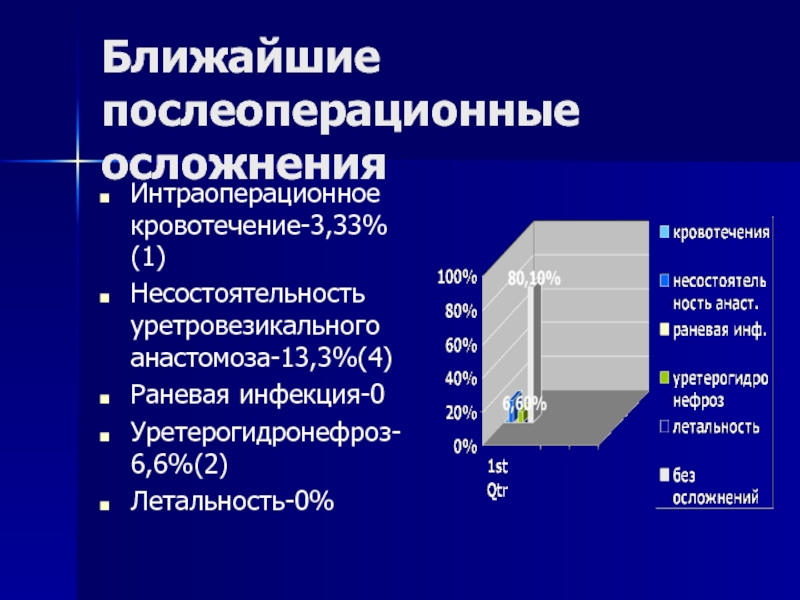
Слайд 16Ближайшие послеоперационные осложнения
Интраоперационное кровотечение-3,33% (1)
Несостоятельность уретровезикального анастомоза-13,3%(4)
Раневая инфекция-0
Уретерогидронефроз-6,6%(2)
Летальность-0%
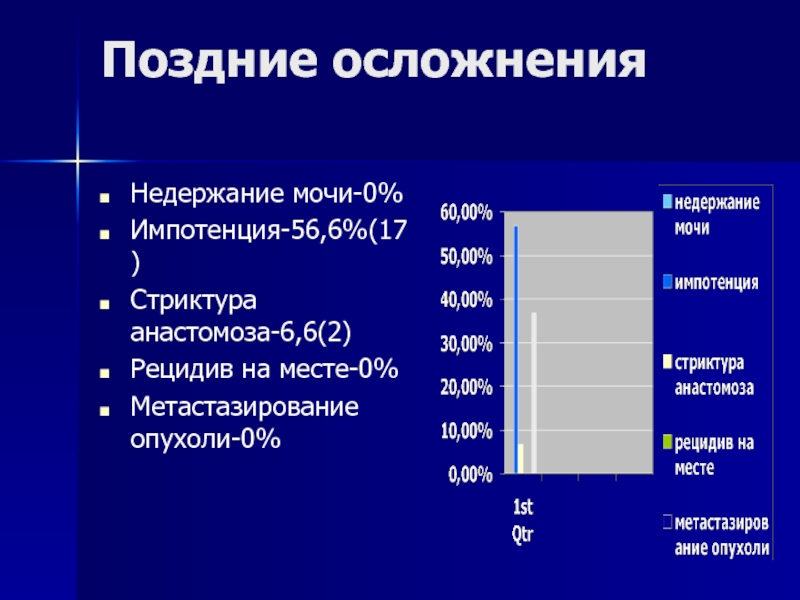
Слайд 17Поздние осложнения
Недержание мочи-0%
Импотенция-56,6%(17)
Стриктура анастомоза-6,6(2)
Рецидив на месте-0%
Метастазирование опухоли-0%
Слайд 18Анализ осложнений – предотвращение кровопотери
Отработка техники тщательного лигирования центральной вены и
Слайд 19Анализ осложнений : травма устьев
Бережное «вылущивание» простаты в едином комплексе с
Слайд 20Анализ осложнений : несостоятельность анастомоза
Для предотвращения несостоятельности анастомоза необходимо предварительное ушивание
Анастомоз ушивается 8-ю нитками викрила 2,0
Слайд 21Анализ осложнений : недержание мочи
Необходимо предварительное ушивание культи уретры до отсечения
Уретральный катетер не должен иметь размер более 18-20СН
Катетер удаляется не позднее 5-го дня простатэктомии, до удаления тазовых дренажей