- Главная
- Разное
- Дизайн
- Бизнес и предпринимательство
- Аналитика
- Образование
- Развлечения
- Красота и здоровье
- Финансы
- Государство
- Путешествия
- Спорт
- Недвижимость
- Армия
- Графика
- Культурология
- Еда и кулинария
- Лингвистика
- Английский язык
- Астрономия
- Алгебра
- Биология
- География
- Детские презентации
- Информатика
- История
- Литература
- Маркетинг
- Математика
- Медицина
- Менеджмент
- Музыка
- МХК
- Немецкий язык
- ОБЖ
- Обществознание
- Окружающий мир
- Педагогика
- Русский язык
- Технология
- Физика
- Философия
- Химия
- Шаблоны, картинки для презентаций
- Экология
- Экономика
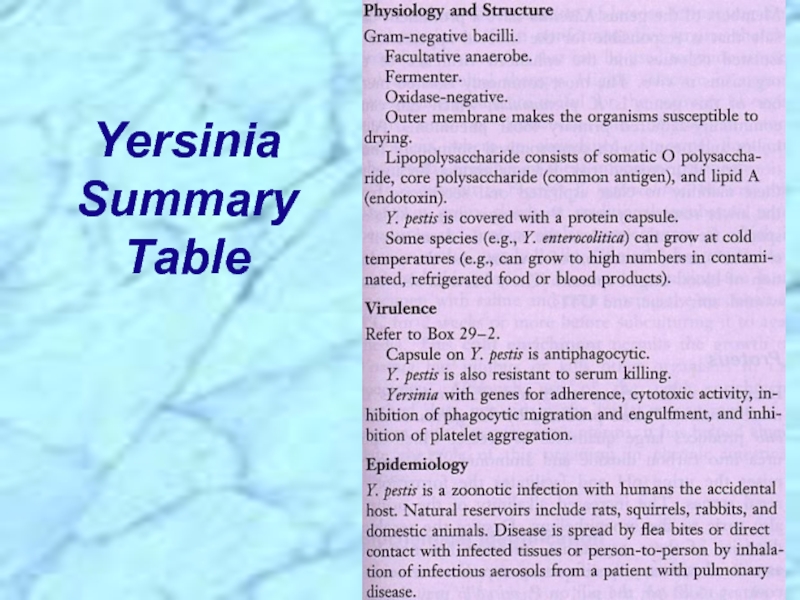
- Юриспруденция
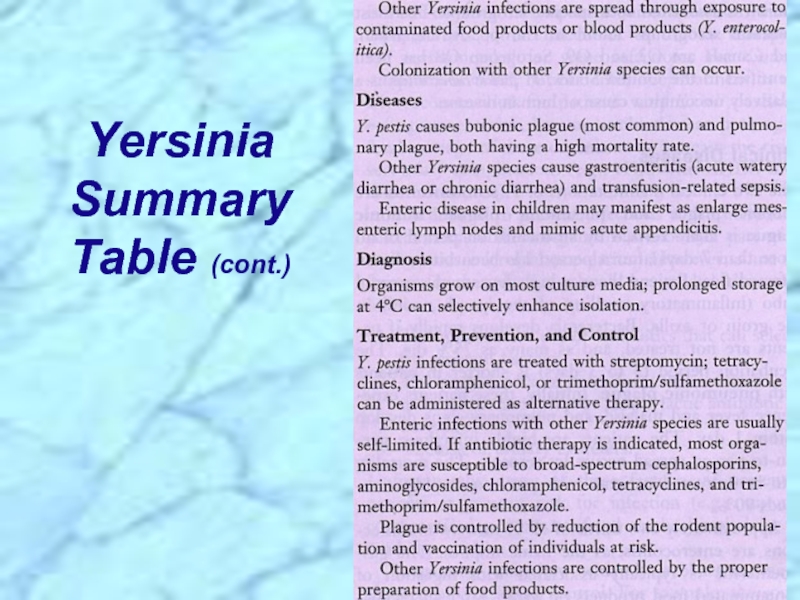
True Pathogens of the Enterobacteriaceae презентация
Содержание
- 2. True Pathogens of the Enterobacteriaceae: ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ Salmonella, Shigella & Yersinia
- 3. Digestive tract is a “tube” (from mouth
- 4. Mouth, pharynx, esophagus & esophageal sphincter
- 5. Coliform bacilli (enteric rods)
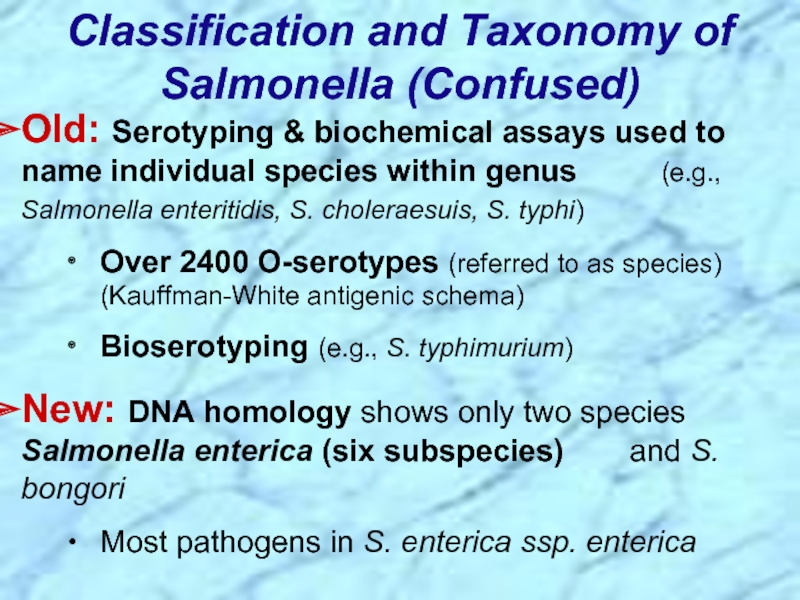
- 6. Classification and Taxonomy of Salmonella (Confused) Old:
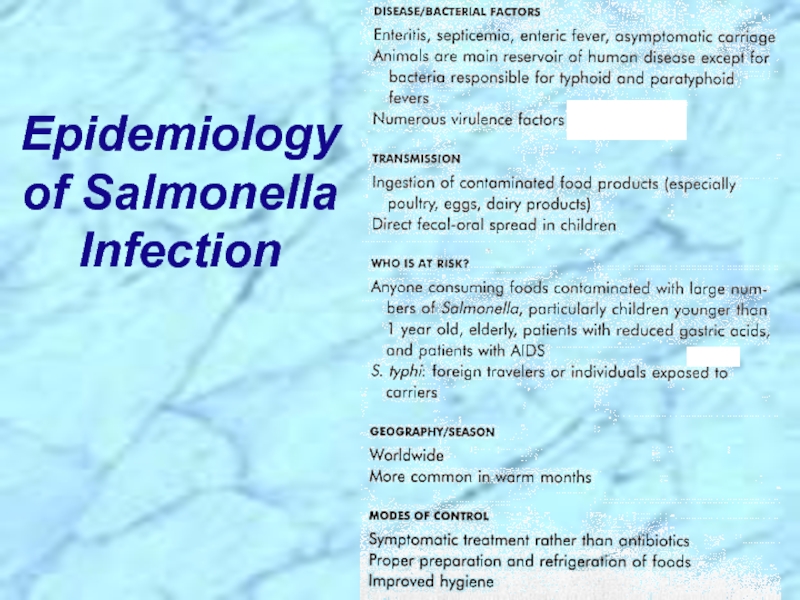
- 7. Epidemiology of Salmonella Infection
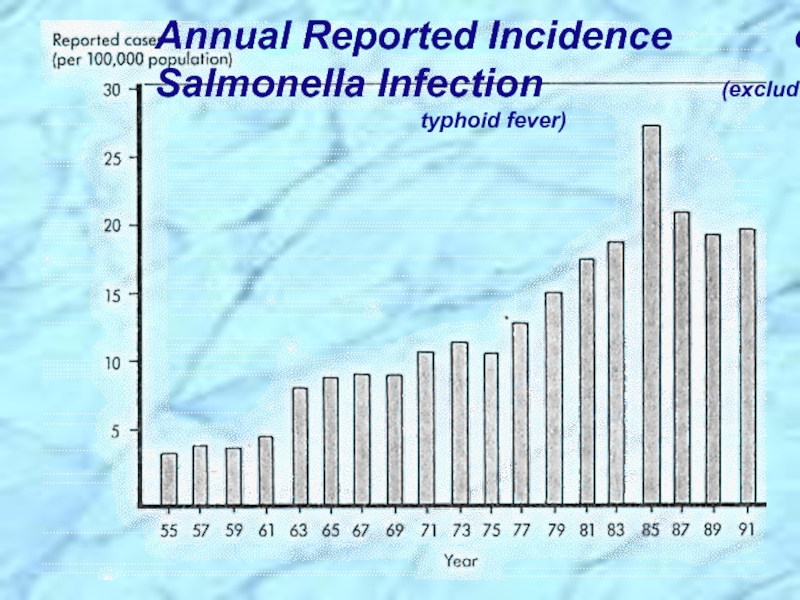
- 8. Annual Reported Incidence
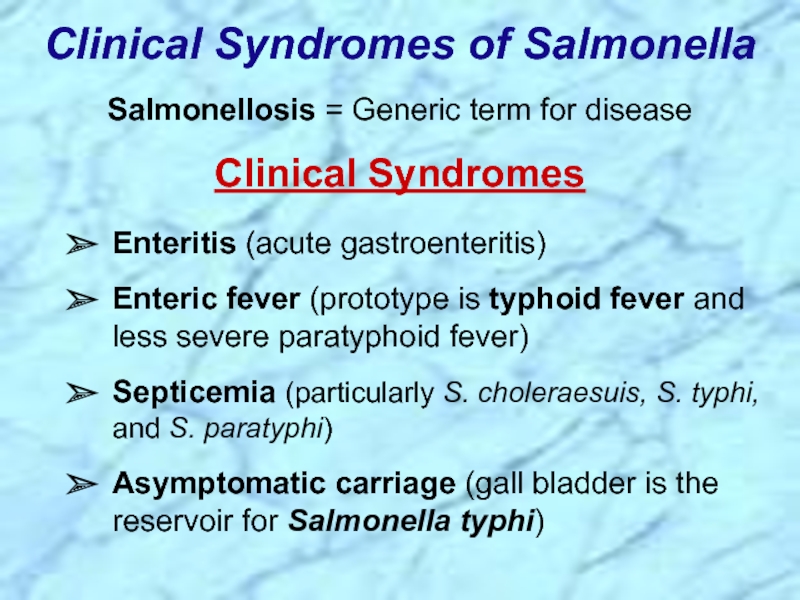
- 9. Clinical Syndromes of Salmonella Salmonellosis =
- 10. Epidemiology and Clinical Syndromes of Salmonella (cont.)
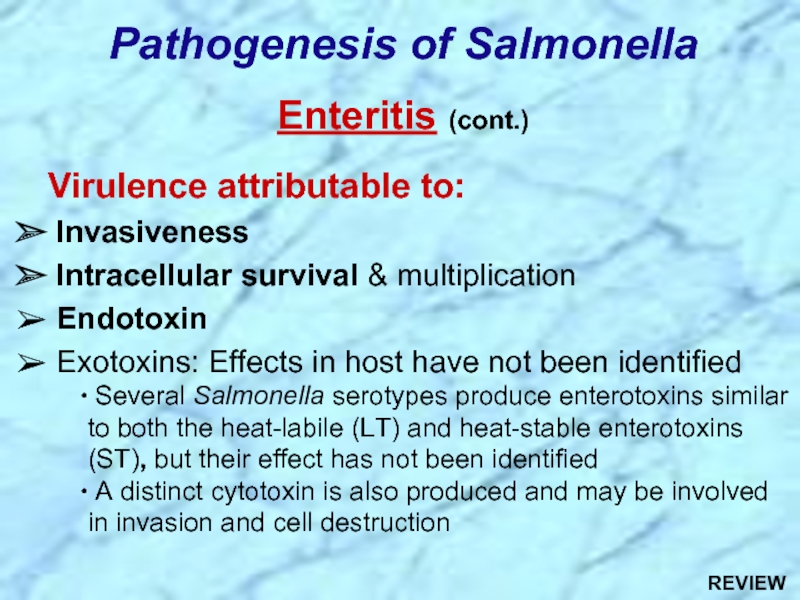
- 11. Virulence attributable to: Invasiveness Intracellular
- 12. Invasiveness in Enteritis (cont.) Penetrate mucus, adhere
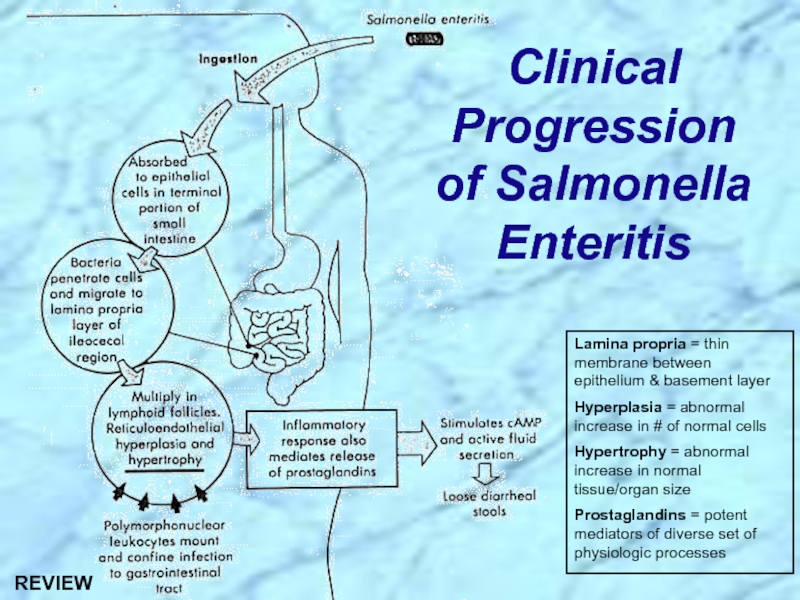
- 13. Clinical Progression of Salmonella Enteritis Lamina propria
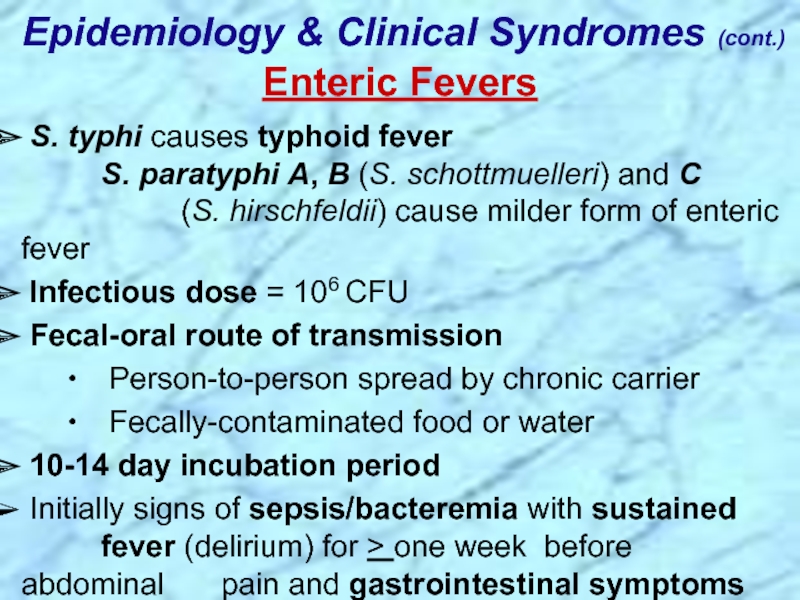
- 14. Epidemiology & Clinical Syndromes (cont.) Enteric
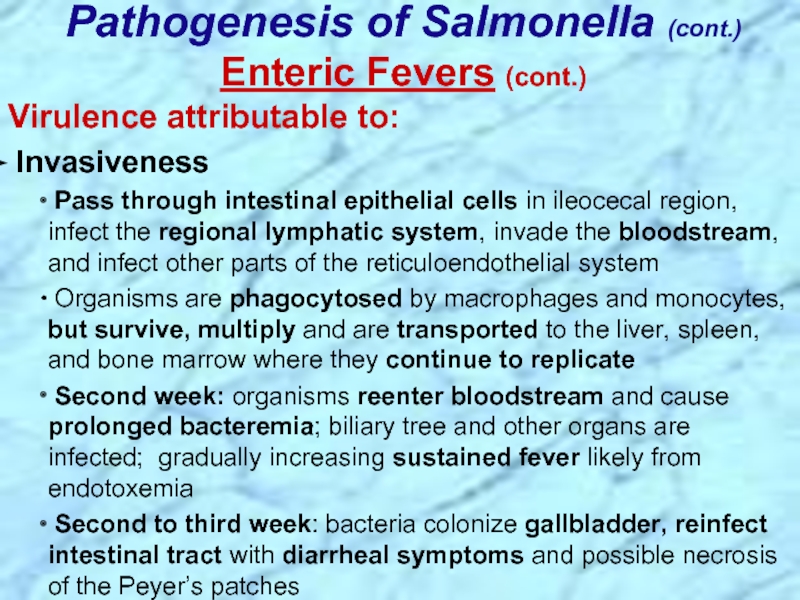
- 15. Pathogenesis of Salmonella (cont.) Enteric Fevers (cont.)
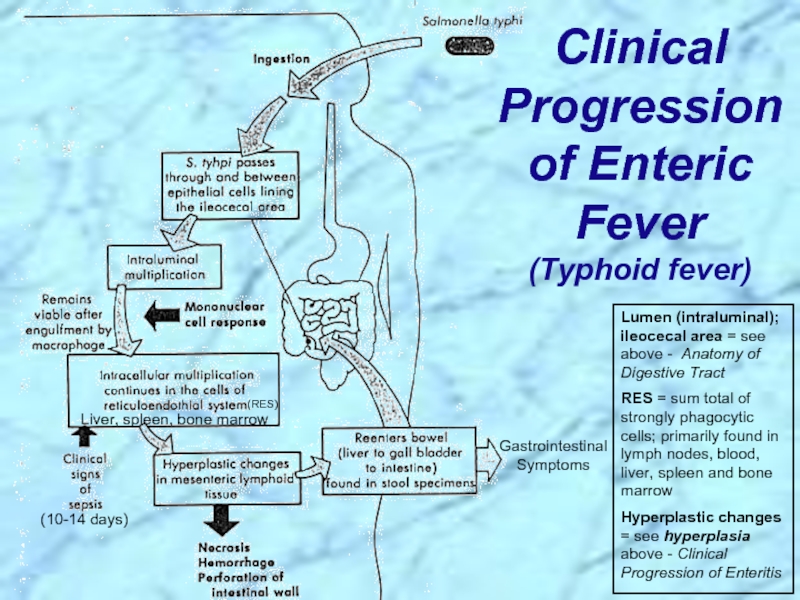
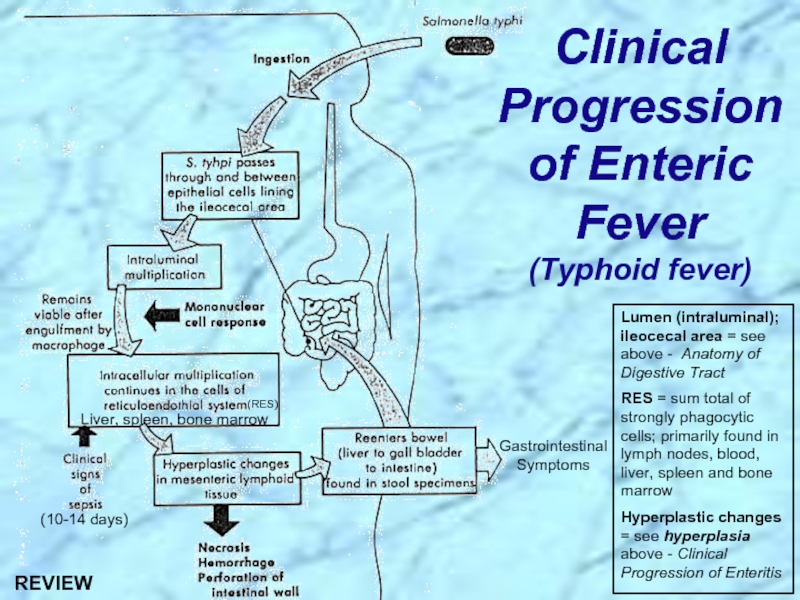
- 16. Clinical Progression of Enteric Fever
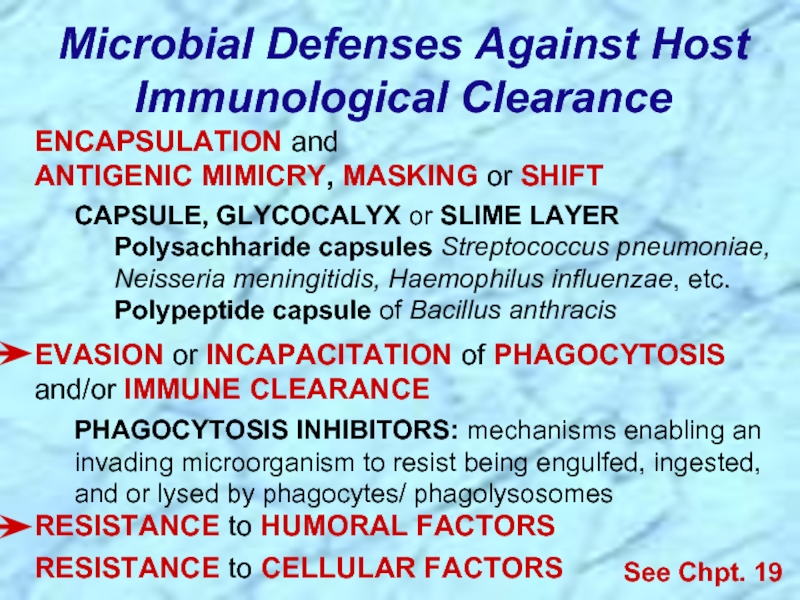
- 17. Microbial Defenses Against Host Immunological Clearance
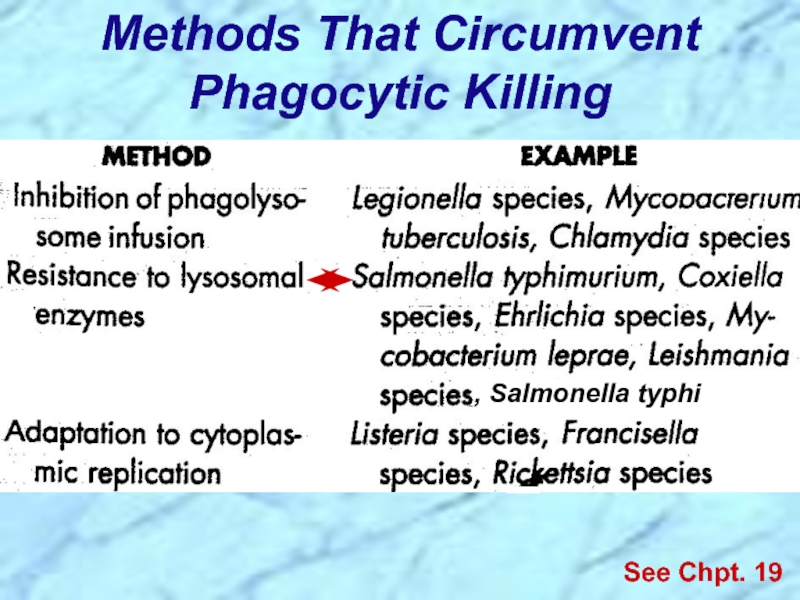
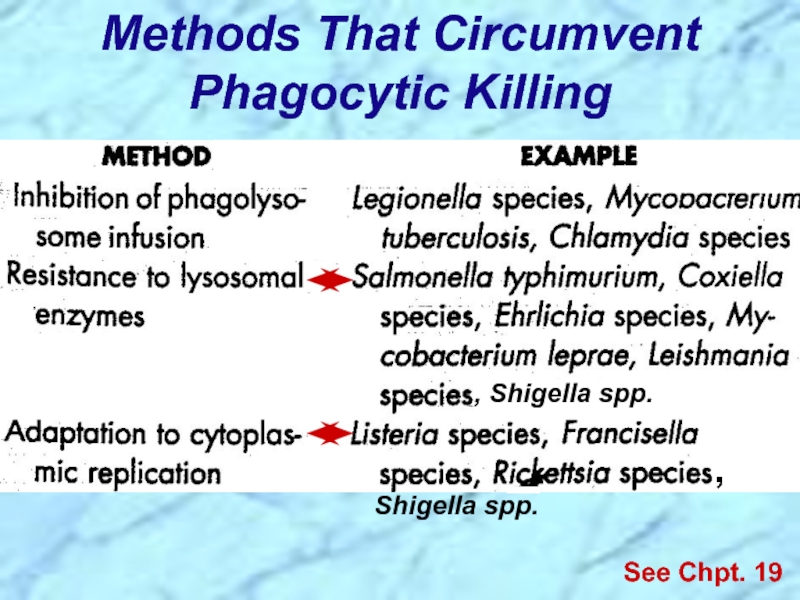
- 18. Methods That Circumvent Phagocytic Killing See Chpt. 19 , Salmonella typhi
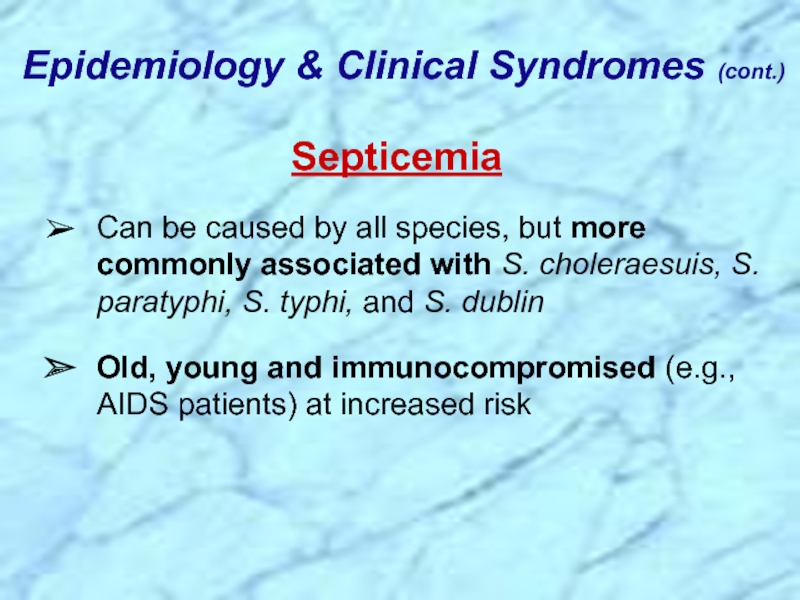
- 19. Septicemia Can be caused by
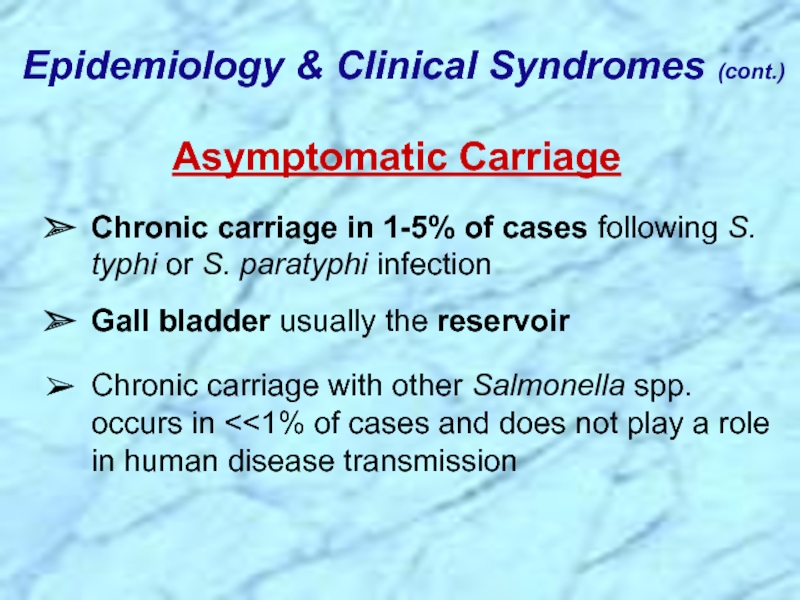
- 20. Asymptomatic Carriage Chronic carriage in
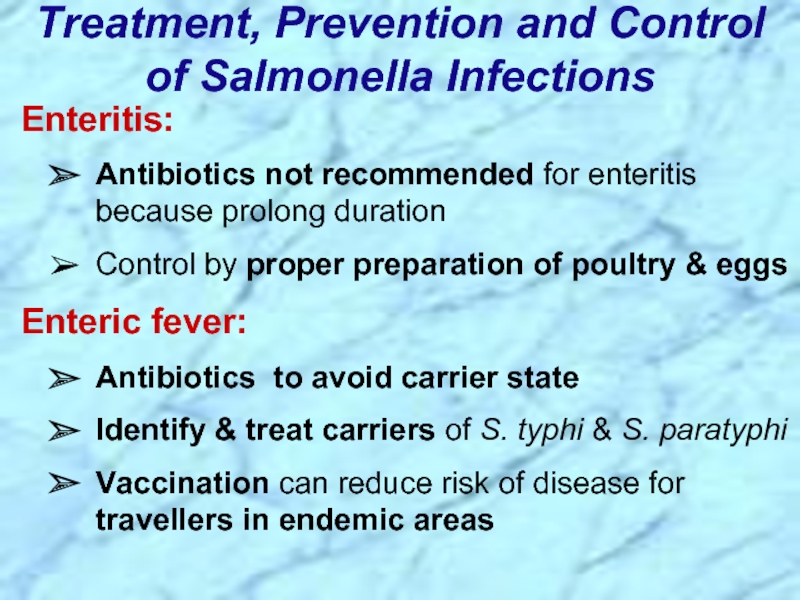
- 21. Treatment, Prevention and Control of Salmonella Infections
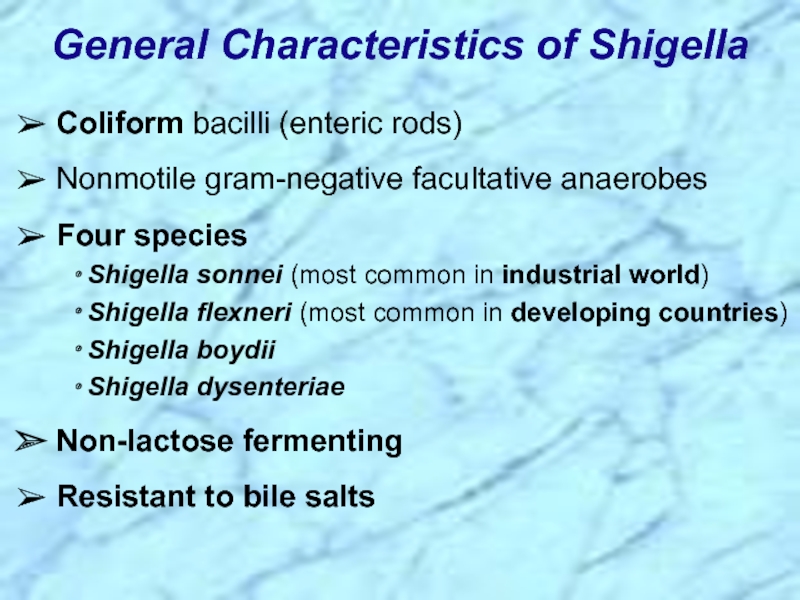
- 23. Coliform bacilli (enteric rods)
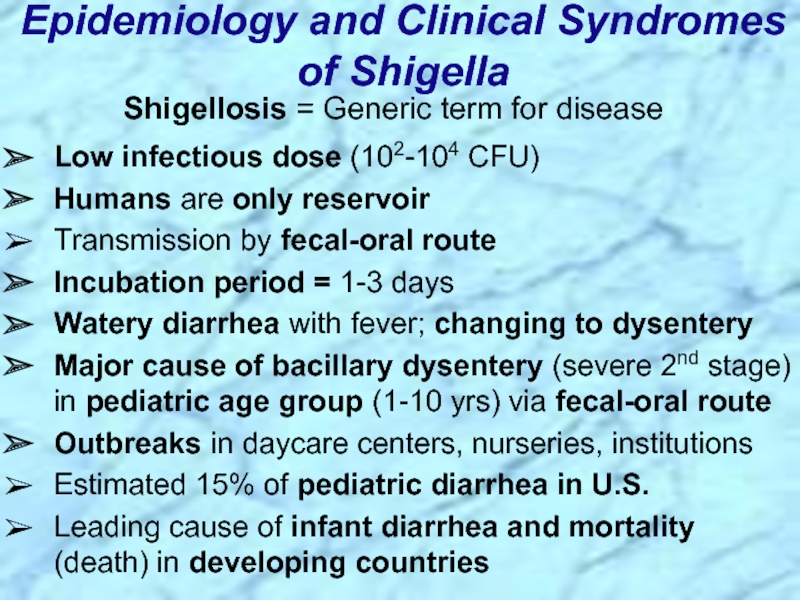
- 24. Shigellosis = Generic term for disease
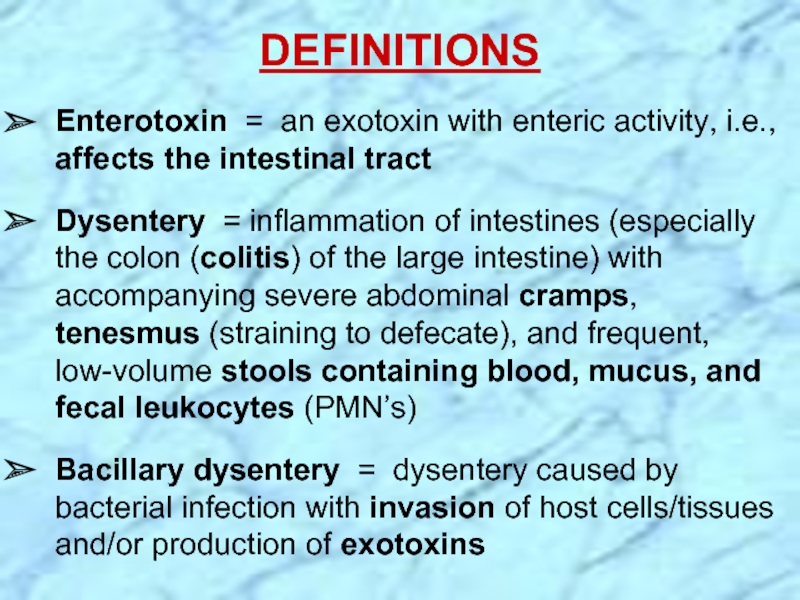
- 25. DEFINITIONS Enterotoxin = an exotoxin with
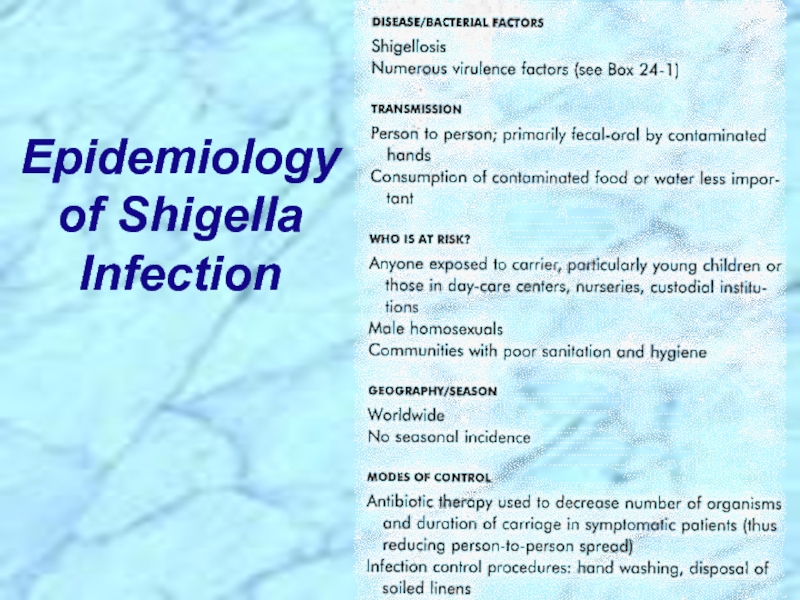
- 26. Epidemiology of Shigella Infection
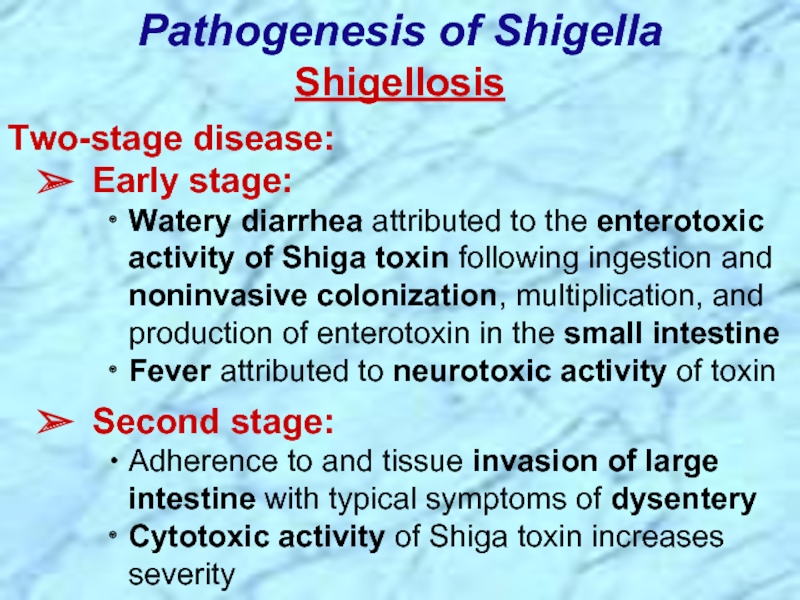
- 27. Shigellosis Two-stage disease: Early stage:
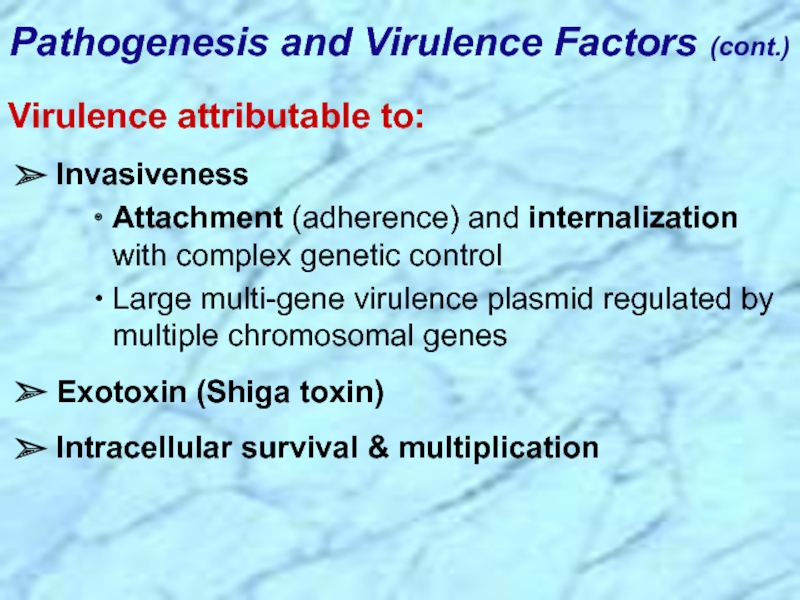
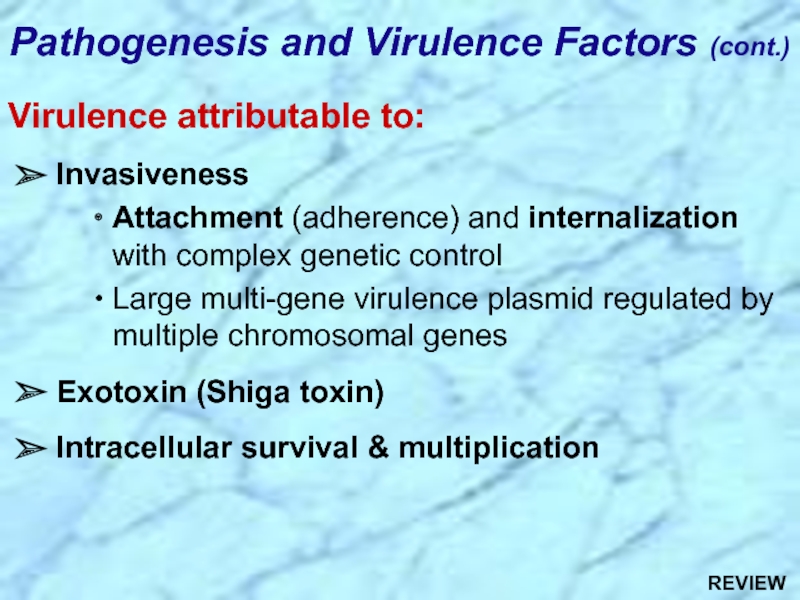
- 28. Pathogenesis and Virulence Factors (cont.) Virulence
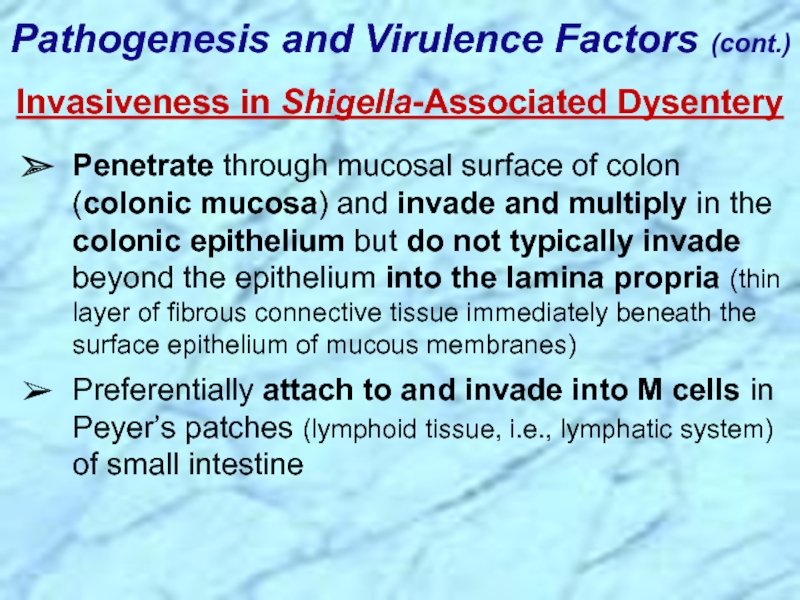
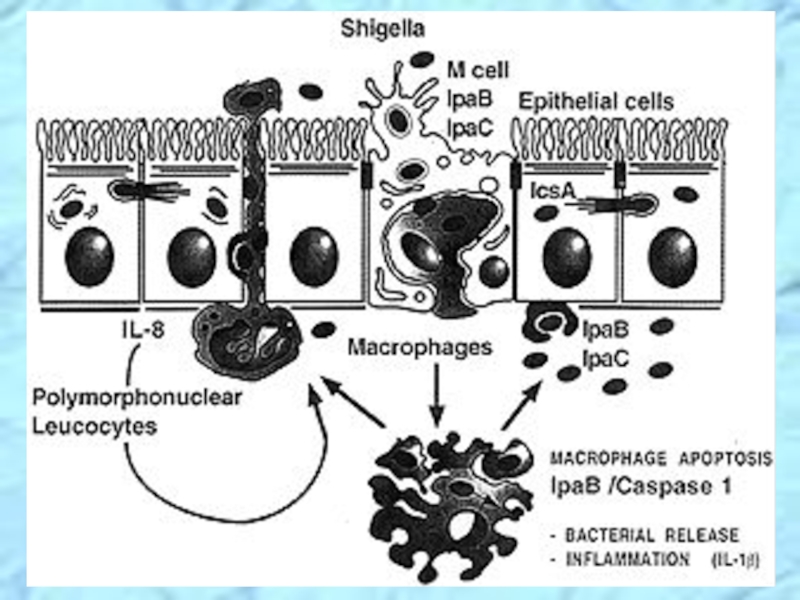
- 29. Penetrate through mucosal surface of colon (colonic
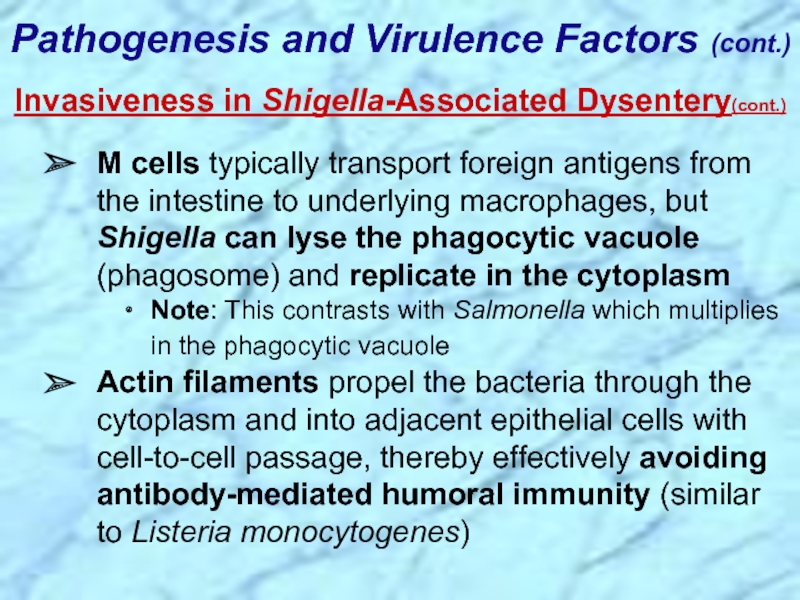
- 30. M cells typically transport foreign antigens from
- 32. Methods That Circumvent Phagocytic Killing See Chpt. 19 , Shigella spp. Shigella spp. ,
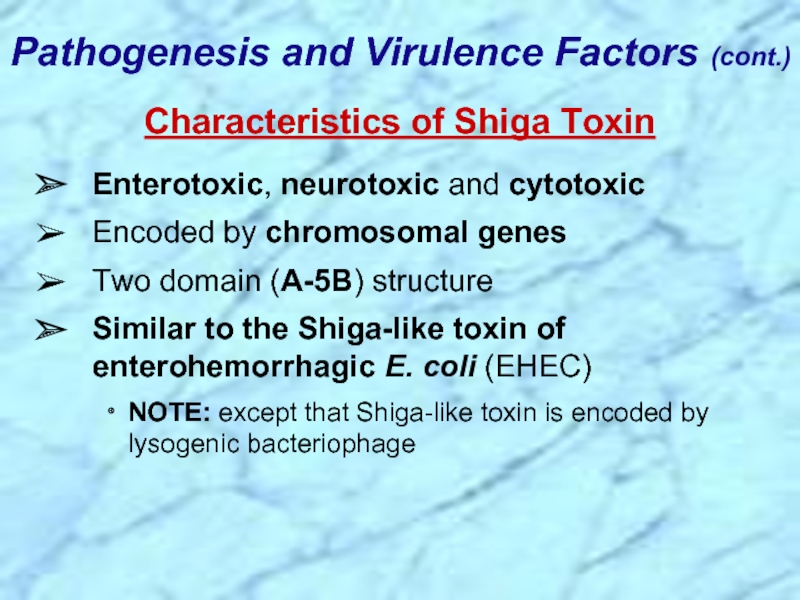
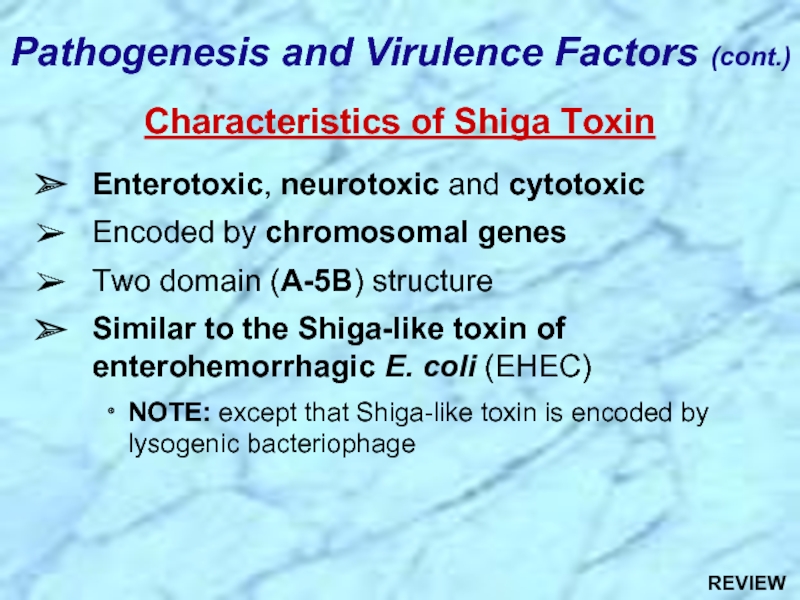
- 33. Enterotoxic, neurotoxic and cytotoxic Encoded by
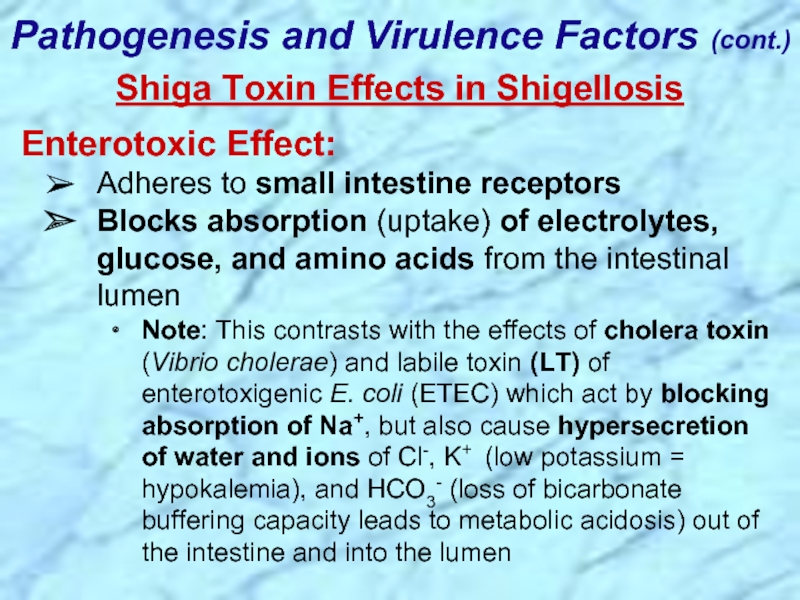
- 34. Shiga Toxin Effects in Shigellosis Enterotoxic Effect:
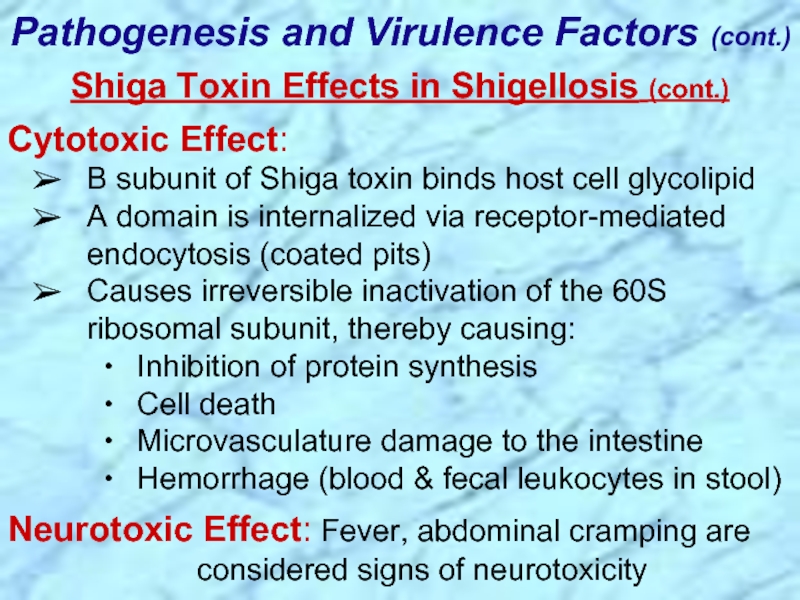
- 35. Cytotoxic Effect: B subunit of Shiga
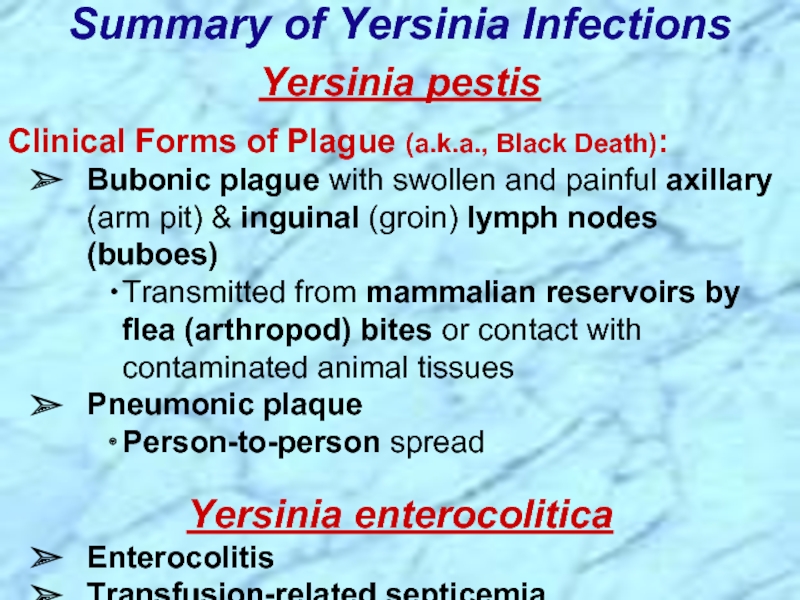
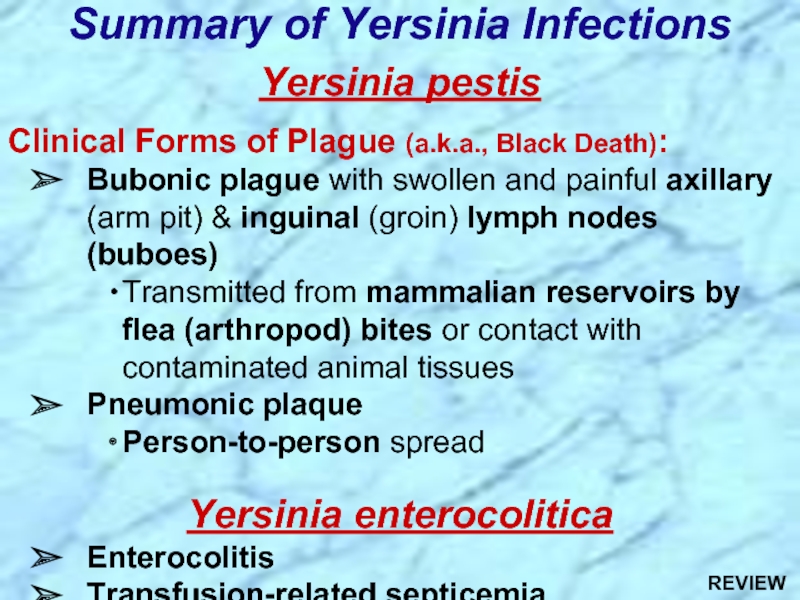
- 38. Yersinia pestis Clinical Forms of Plague
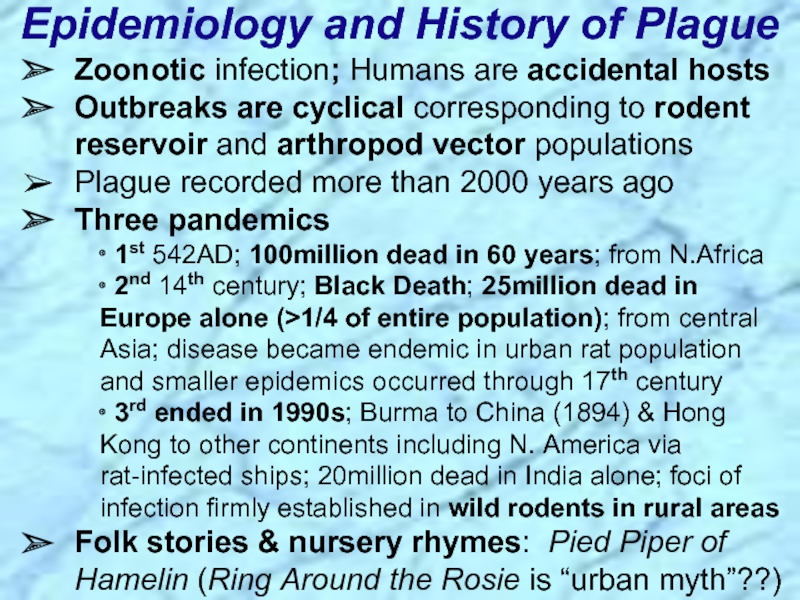
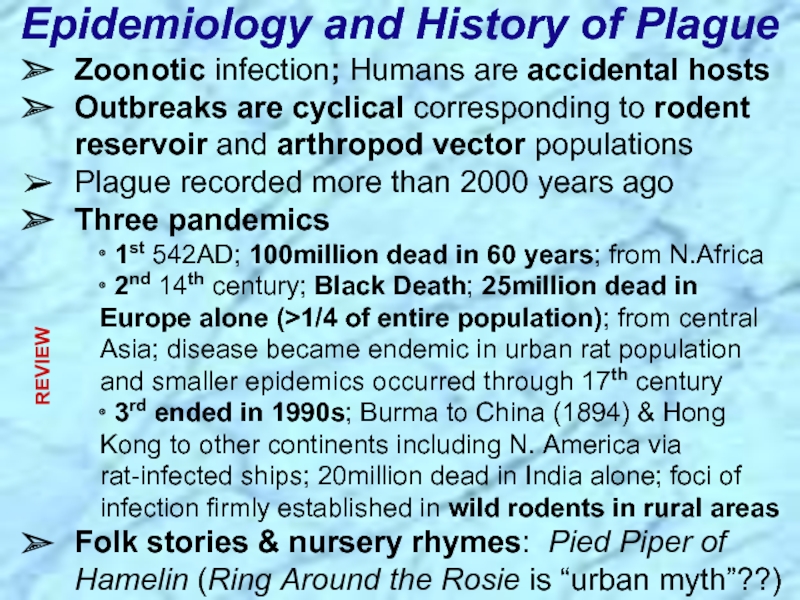
- 39. Epidemiology and History of Plague Zoonotic infection;
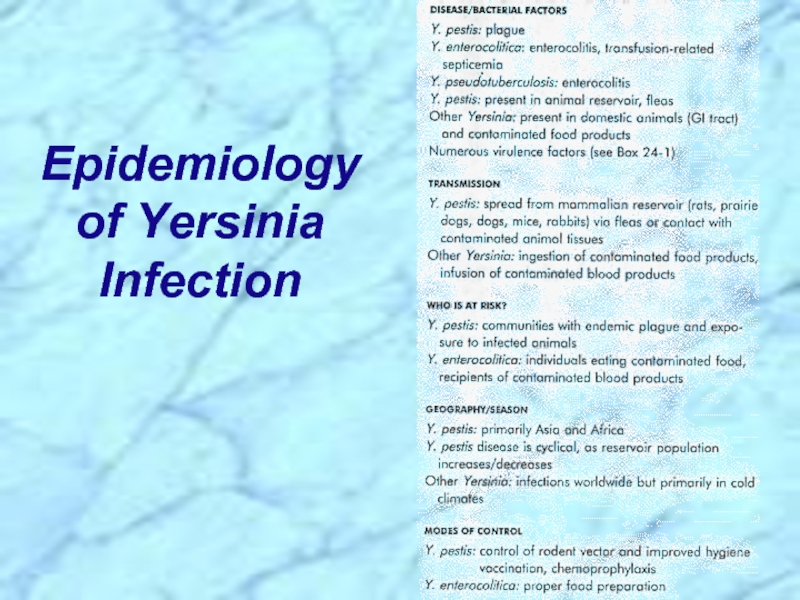
- 40. Epidemiology of Yersinia Infection
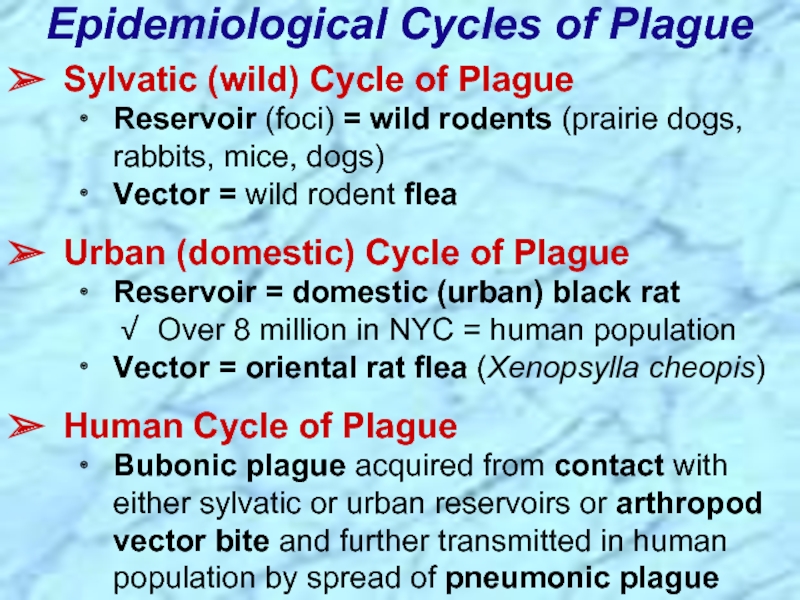
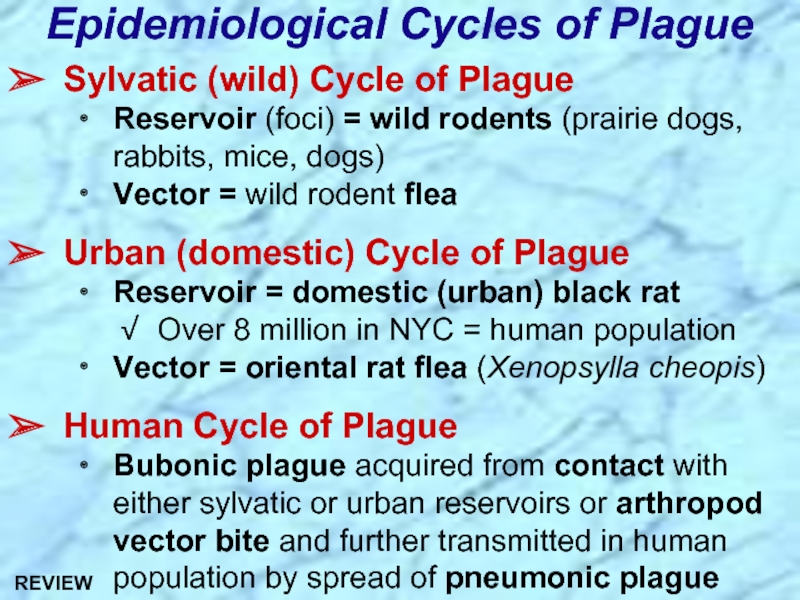
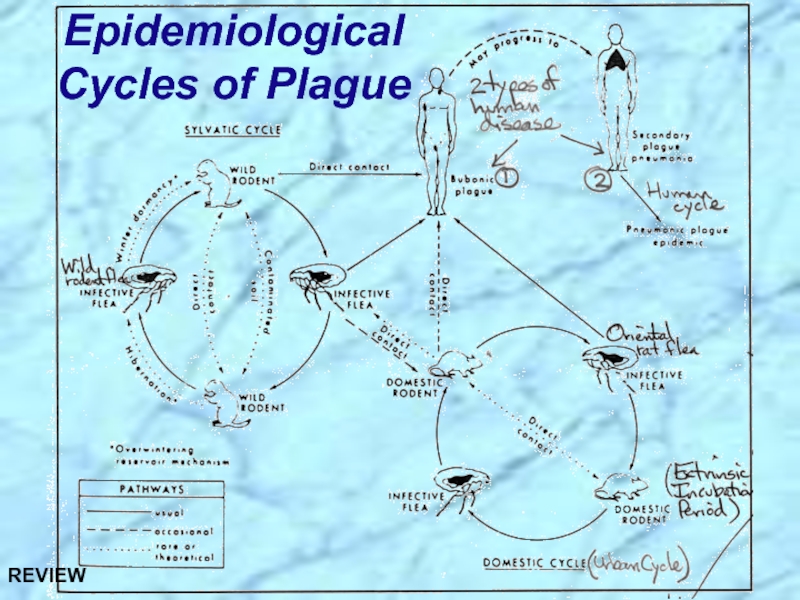
- 41. Epidemiological Cycles of Plague Sylvatic (wild) Cycle
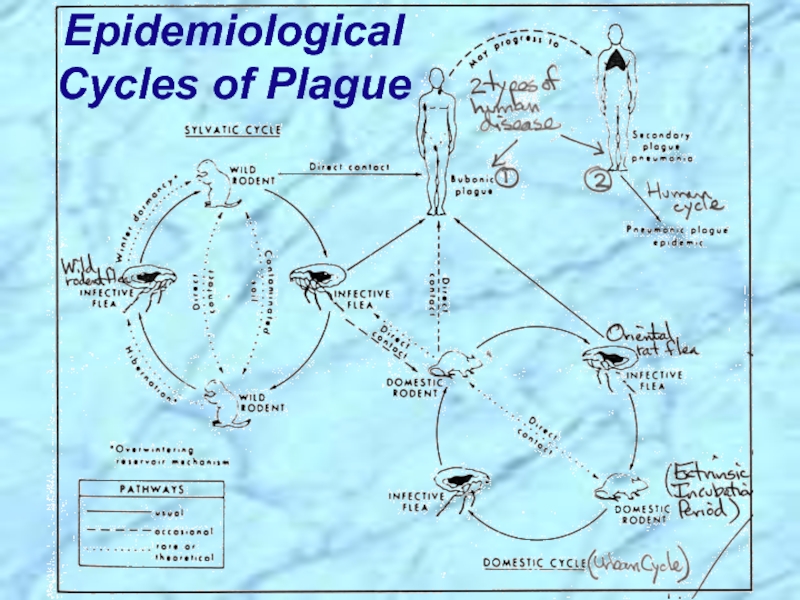
- 42. Epidemiological Cycles of Plague
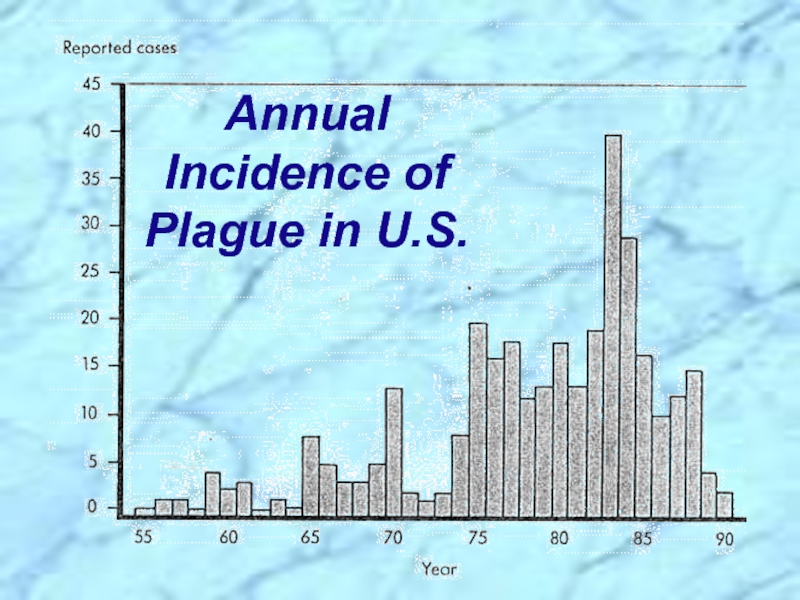
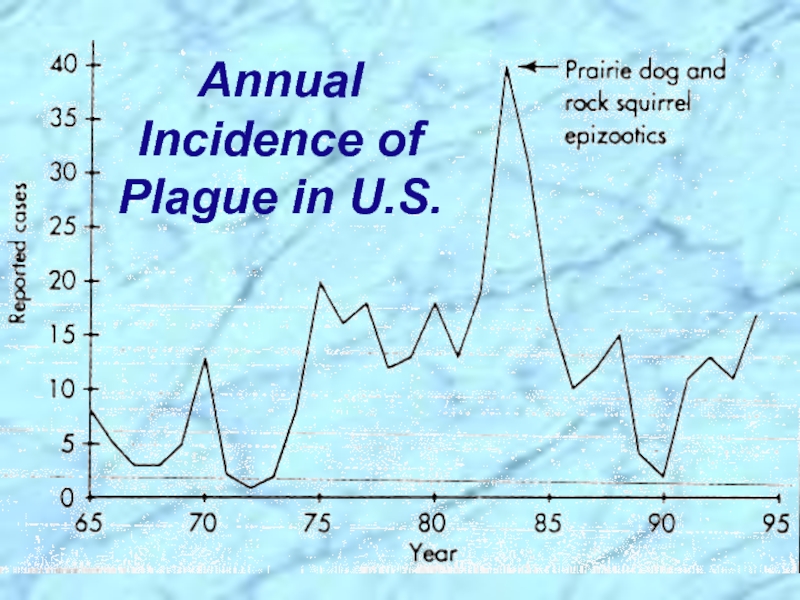
- 43. Annual Incidence of Plague in U.S.
- 44. Annual Incidence of Plague in U.S.
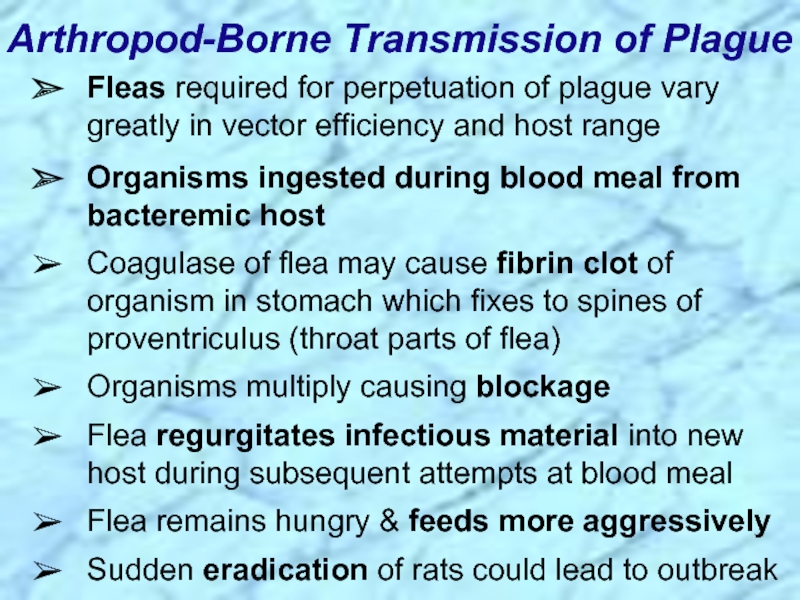
- 45. Arthropod-Borne Transmission of Plague Fleas required for
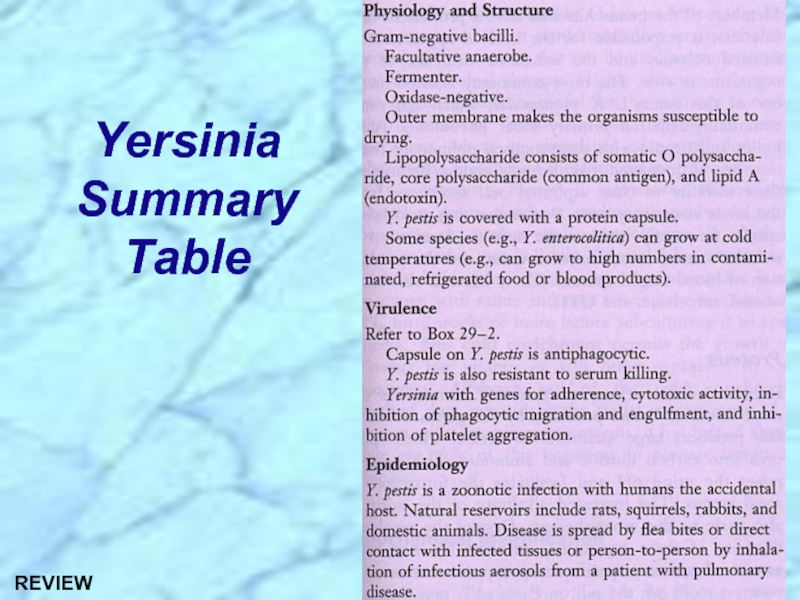
- 46. Yersinia Summary Table
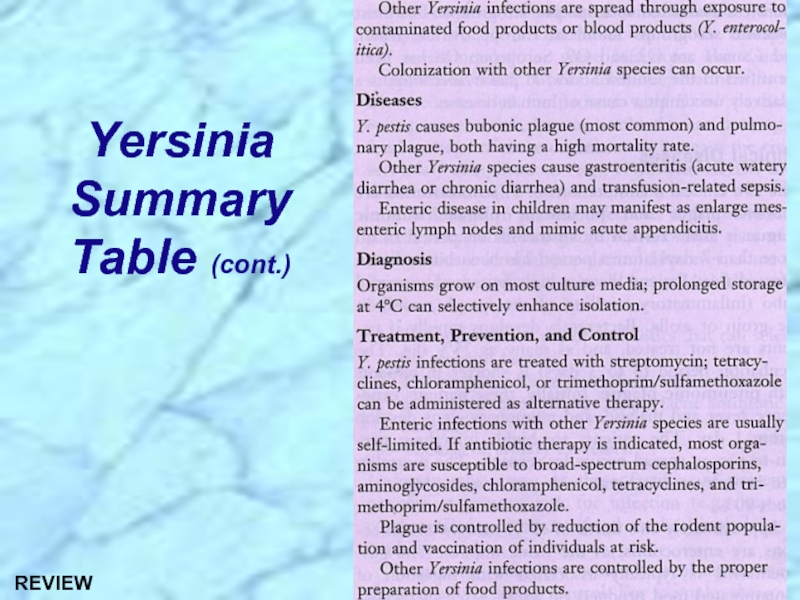
- 47. Yersinia Summary Table (cont.)
- 49. REVIEW
- 50. See Handouts REVIEW
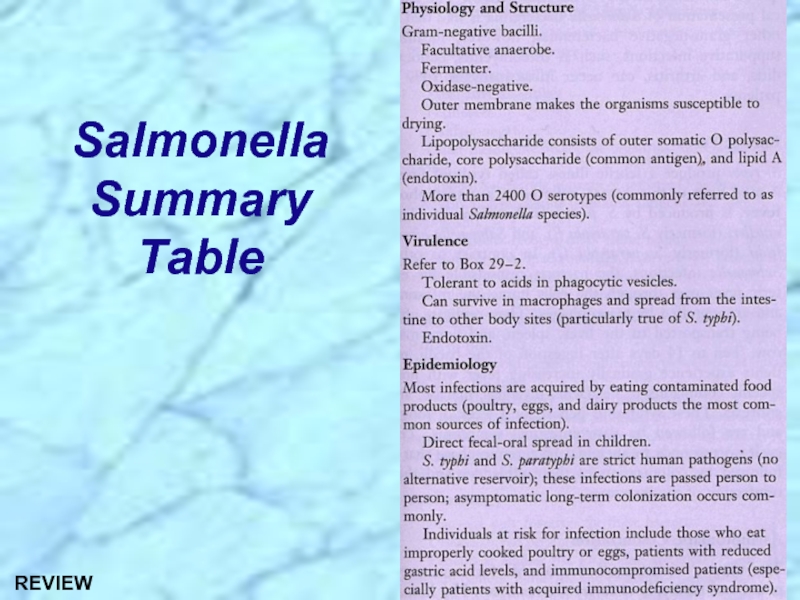
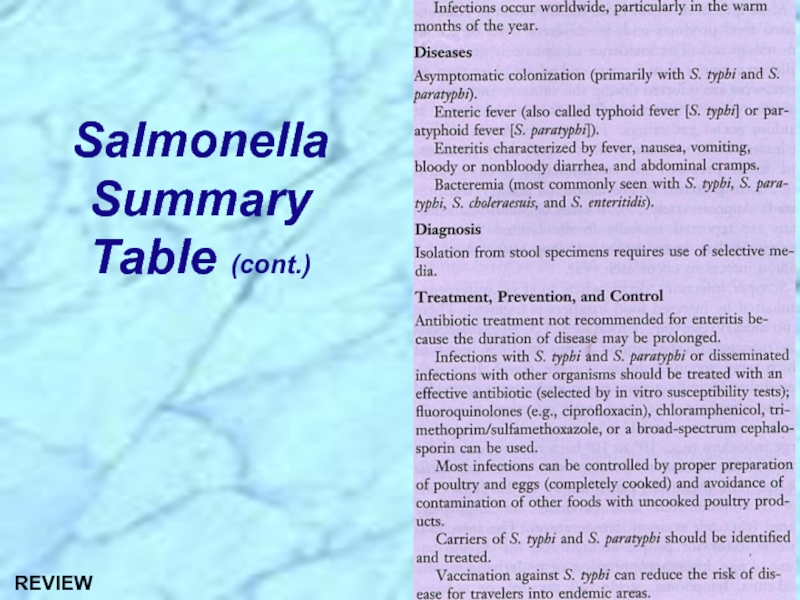
- 51. Salmonella Summary Table REVIEW
- 52. Salmonella Summary Table (cont.) REVIEW
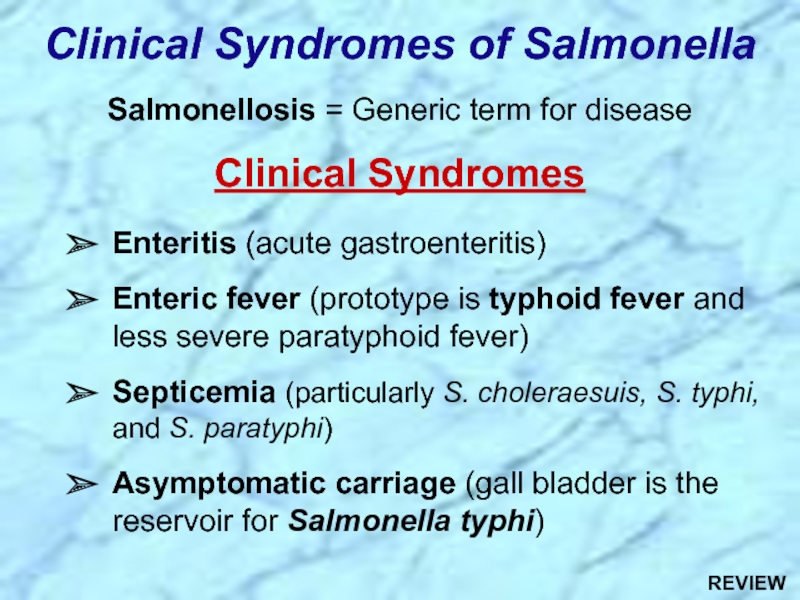
- 53. Clinical Syndromes of Salmonella Salmonellosis =
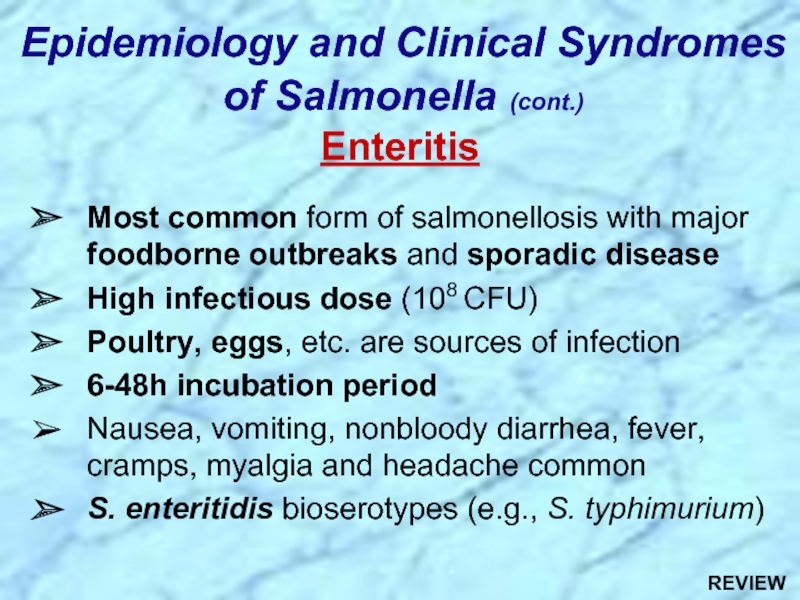
- 54. Epidemiology and Clinical Syndromes of Salmonella (cont.)
- 55. Virulence attributable to: Invasiveness Intracellular
- 56. Clinical Progression of Salmonella Enteritis Lamina propria
- 57. Clinical Progression of Enteric Fever
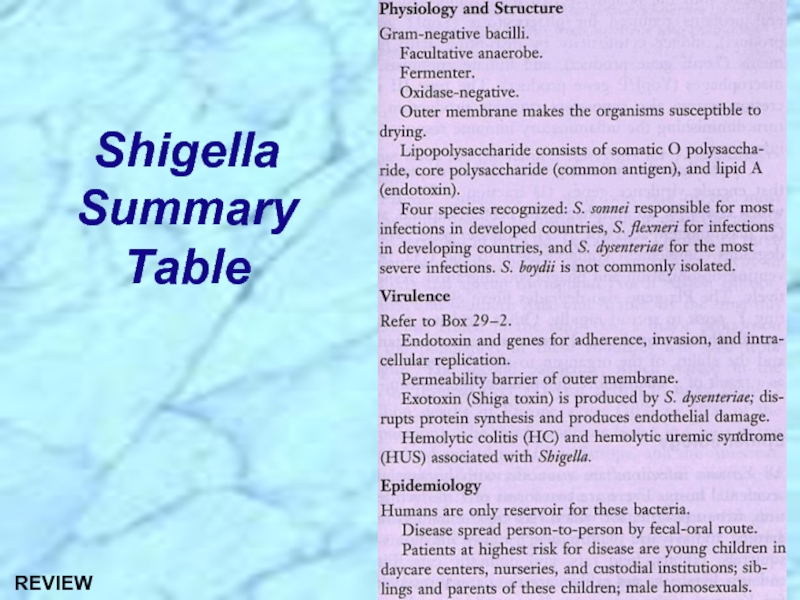
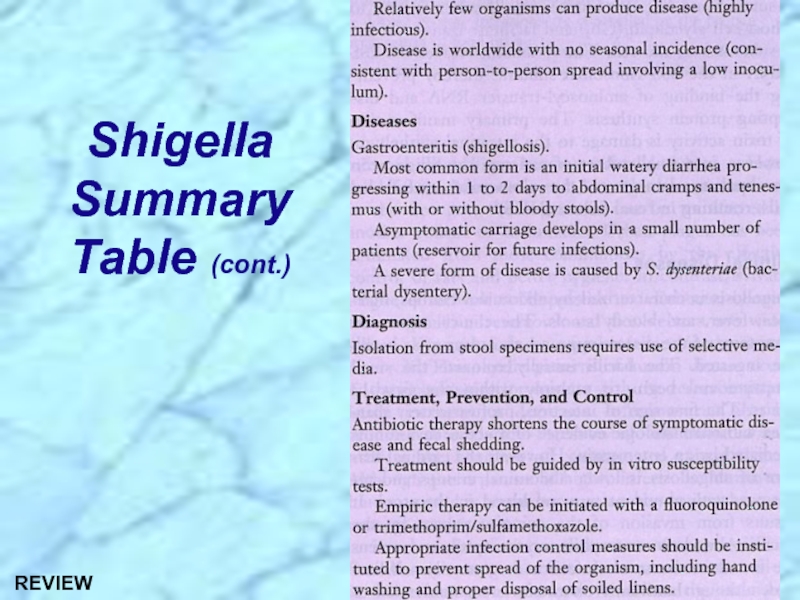
- 59. Shigella Summary Table REVIEW
- 60. Shigella Summary Table (cont.) REVIEW
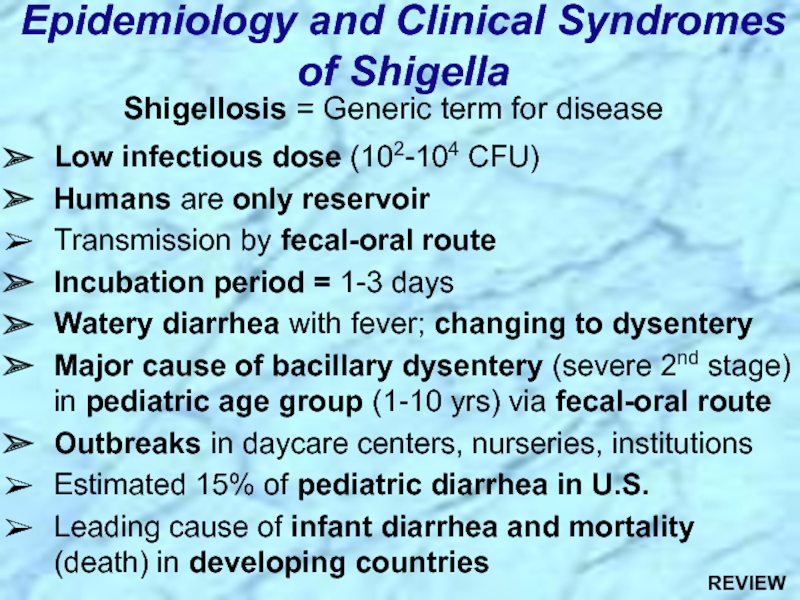
- 61. Shigellosis = Generic term for disease
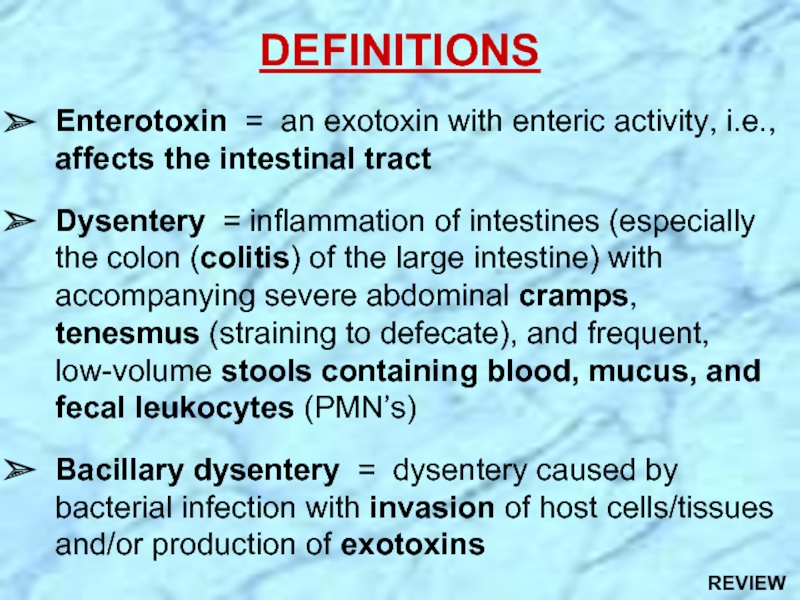
- 62. DEFINITIONS Enterotoxin = an exotoxin with
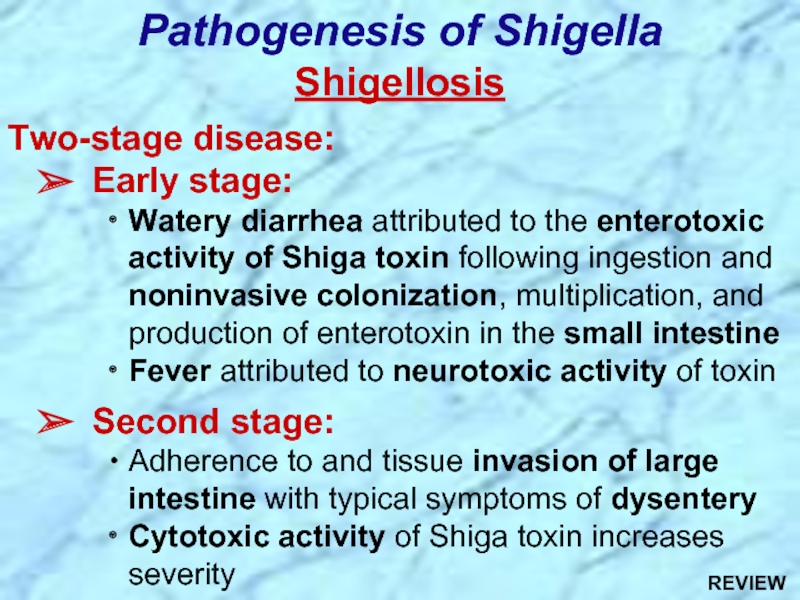
- 63. Shigellosis Two-stage disease: Early stage:
- 64. Pathogenesis and Virulence Factors (cont.) Virulence
- 65. Enterotoxic, neurotoxic and cytotoxic Encoded by
- 67. Yersinia Summary Table REVIEW
- 68. Yersinia Summary Table (cont.) REVIEW
- 69. Yersinia pestis Clinical Forms of Plague
- 70. Epidemiology and History of Plague Zoonotic infection;
- 71. Epidemiological Cycles of Plague Sylvatic (wild) Cycle
- 72. Epidemiological Cycles of Plague REVIEW
Слайд 2True Pathogens
of the Enterobacteriaceae:
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
Salmonella, Shigella & Yersinia
Слайд 3Digestive tract is a “tube” (from mouth to anus); technically “outside”
Lumen = space within tubular or hollow organ such as an artery, vein, or intestine
Intestinal lumen = the inside of the intestine
Mesentery = membrane attaching organ (e.g., intestine) to body wall; often has lymphoid tissue
Food is moved down tract via peristalsis
Entire length of digestive tract epithelium is covered by mucosal membrane (mucosa) with mucus that is secreted from specialized glands
Surface area of intestine increased by presence of villi (finger-like projections) and microvilli that absorb nutrients and other products of digestion
Anatomy of Digestive Tract
Слайд 4 Mouth, pharynx, esophagus & esophageal sphincter
Stomach and pyloric valve
Small intestine (about 23 feet in length)
Duodenum (~10” in length) (bile & pancreatic ducts carry digestive juices secreted by gall bladder, liver & pancreas)
Jejunum (~8 feet in length)
Ileum (final 3/5 of length) and ileocecal valve
Absorbs bile salts & nutrients, including vitamin B12
Large intestine
Cecum(caecum) (blind pouch where appendix also enters)
Colon (ascending, transverse, descending, sigmoid)
Rectum and anus (with internal and external sphincters)
Anatomy of Digestive Tract (cont.)
Слайд 5 Coliform bacilli (enteric rods)
Motile gram-negative facultative anaerobes
Non-lactose fermenting
H2S producing
General Characteristics of Salmonella
Слайд 6Classification and Taxonomy of Salmonella (Confused)
Old: Serotyping & biochemical assays used
Over 2400 O-serotypes (referred to as species) (Kauffman-White antigenic schema)
Bioserotyping (e.g., S. typhimurium)
New: DNA homology shows only two species Salmonella enterica (six subspecies) and S. bongori
Most pathogens in S. enterica ssp. enterica
Слайд 9Clinical Syndromes of Salmonella
Salmonellosis = Generic term for disease
Clinical Syndromes
Enteritis
Enteric fever (prototype is typhoid fever and less severe paratyphoid fever)
Septicemia (particularly S. choleraesuis, S. typhi, and S. paratyphi)
Asymptomatic carriage (gall bladder is the reservoir for Salmonella typhi)
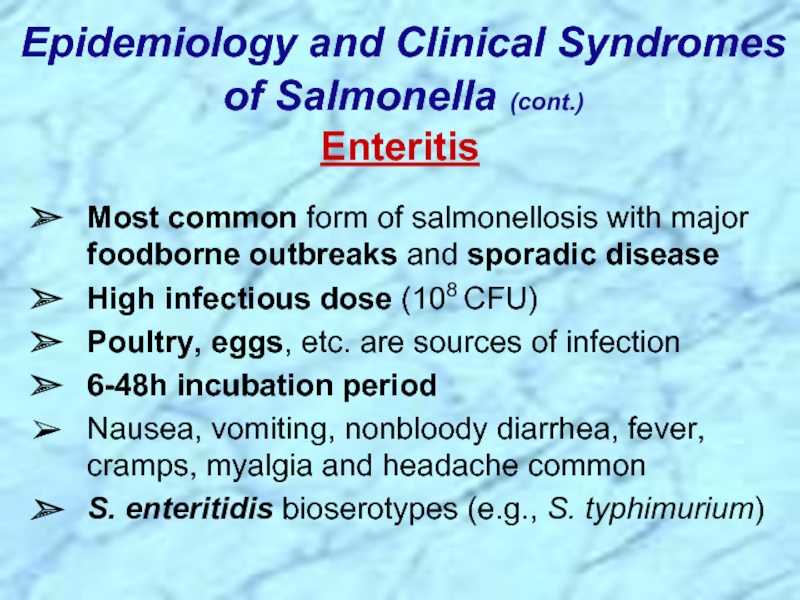
Слайд 10Epidemiology and Clinical Syndromes of Salmonella (cont.)
Enteritis
Most common form
High infectious dose (108 CFU)
Poultry, eggs, etc. are sources of infection
6-48h incubation period
Nausea, vomiting, nonbloody diarrhea, fever, cramps, myalgia and headache common
S. enteritidis bioserotypes (e.g., S. typhimurium)
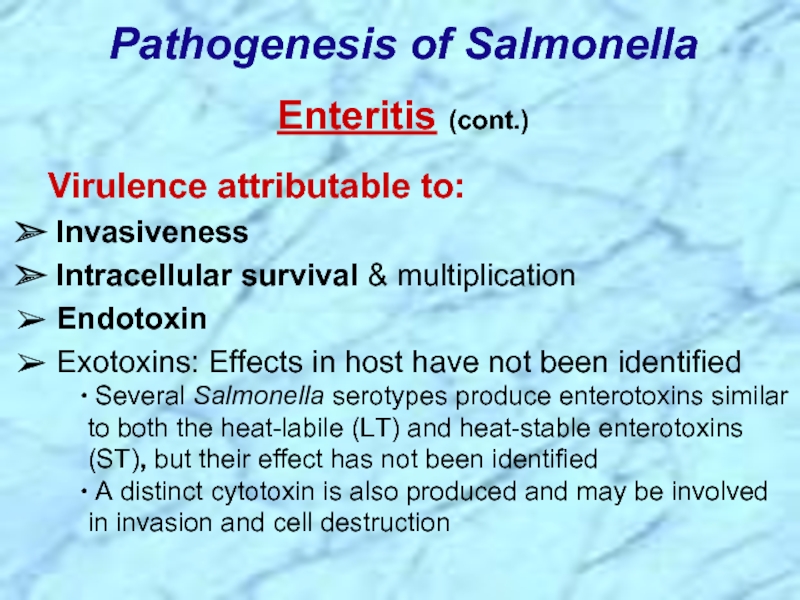
Слайд 11Virulence attributable to:
Invasiveness
Intracellular survival & multiplication
Endotoxin
Exotoxins: Effects
Several Salmonella serotypes produce enterotoxins similar to both the heat-labile (LT) and heat-stable enterotoxins (ST), but their effect has not been identified
A distinct cytotoxin is also produced and may be involved in invasion and cell destruction
Pathogenesis of Salmonella
Enteritis (cont.)
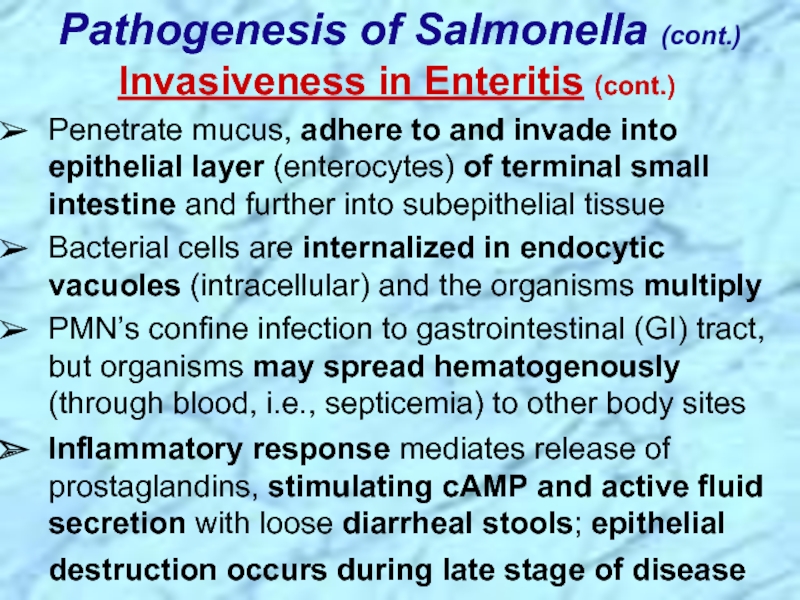
Слайд 12Invasiveness in Enteritis (cont.)
Penetrate mucus, adhere to and invade into epithelial
Bacterial cells are internalized in endocytic vacuoles (intracellular) and the organisms multiply
PMN’s confine infection to gastrointestinal (GI) tract, but organisms may spread hematogenously (through blood, i.e., septicemia) to other body sites
Inflammatory response mediates release of prostaglandins, stimulating cAMP and active fluid secretion with loose diarrheal stools; epithelial destruction occurs during late stage of disease
Pathogenesis of Salmonella (cont.)
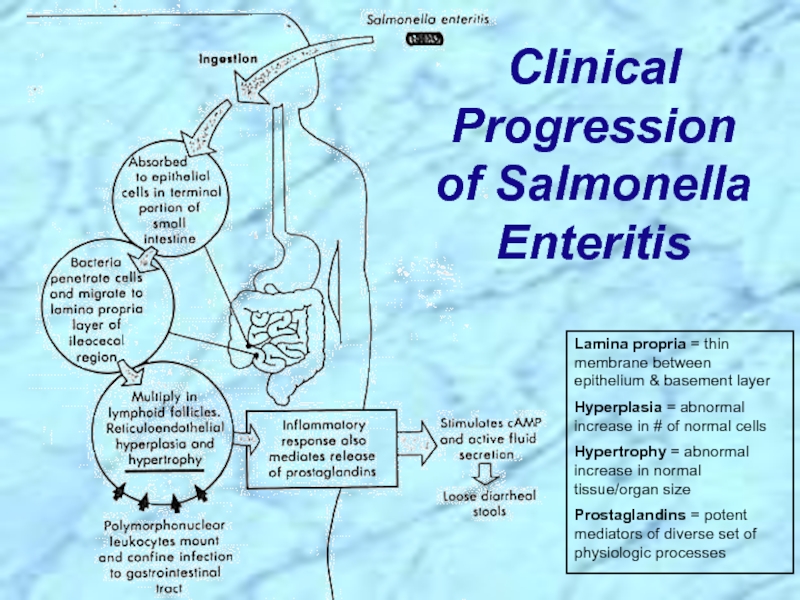
Слайд 13Clinical Progression of Salmonella Enteritis
Lamina propria = thin membrane between epithelium
Hyperplasia = abnormal increase in # of normal cells
Hypertrophy = abnormal increase in normal tissue/organ size
Prostaglandins = potent mediators of diverse set of physiologic processes
Слайд 14Epidemiology & Clinical Syndromes (cont.)
Enteric Fevers
S. typhi causes
Infectious dose = 106 CFU
Fecal-oral route of transmission
Person-to-person spread by chronic carrier
Fecally-contaminated food or water
10-14 day incubation period
Initially signs of sepsis/bacteremia with sustained fever (delirium) for > one week before abdominal pain and gastrointestinal symptoms
Слайд 15Pathogenesis of Salmonella (cont.) Enteric Fevers (cont.)
Virulence attributable to:
Invasiveness
Organisms are phagocytosed by macrophages and monocytes, but survive, multiply and are transported to the liver, spleen, and bone marrow where they continue to replicate
Second week: organisms reenter bloodstream and cause prolonged bacteremia; biliary tree and other organs are infected; gradually increasing sustained fever likely from endotoxemia
Second to third week: bacteria colonize gallbladder, reinfect intestinal tract with diarrheal symptoms and possible necrosis of the Peyer’s patches
Слайд 16Clinical Progression of Enteric Fever (Typhoid fever)
Lumen (intraluminal);
RES = sum total of strongly phagocytic cells; primarily found in lymph nodes, blood, liver, spleen and bone marrow
Hyperplastic changes = see hyperplasia above - Clinical Progression of Enteritis
Слайд 17
Microbial Defenses Against Host Immunological Clearance
ENCAPSULATION and
ANTIGENIC MIMICRY, MASKING or
CAPSULE, GLYCOCALYX or SLIME LAYER
Polysachharide capsules Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, etc.
Polypeptide capsule of Bacillus anthracis
EVASION or INCAPACITATION of PHAGOCYTOSIS and/or IMMUNE CLEARANCE
PHAGOCYTOSIS INHIBITORS: mechanisms enabling an invading microorganism to resist being engulfed, ingested, and or lysed by phagocytes/ phagolysosomes
RESISTANCE to HUMORAL FACTORS
RESISTANCE to CELLULAR FACTORS
See Chpt. 19
Слайд 19Septicemia
Can be caused by all species, but more commonly associated
Old, young and immunocompromised (e.g., AIDS patients) at increased risk
Epidemiology & Clinical Syndromes (cont.)
Слайд 20Asymptomatic Carriage
Chronic carriage in 1-5% of cases following S. typhi
Gall bladder usually the reservoir
Chronic carriage with other Salmonella spp. occurs in <<1% of cases and does not play a role in human disease transmission
Epidemiology & Clinical Syndromes (cont.)
Слайд 21Treatment, Prevention and Control of Salmonella Infections
Enteritis:
Antibiotics not recommended for enteritis
Control by proper preparation of poultry & eggs
Enteric fever:
Antibiotics to avoid carrier state
Identify & treat carriers of S. typhi & S. paratyphi
Vaccination can reduce risk of disease for travellers in endemic areas
Слайд 23 Coliform bacilli (enteric rods)
Nonmotile gram-negative facultative anaerobes
Four
Shigella sonnei (most common in industrial world)
Shigella flexneri (most common in developing countries)
Shigella boydii
Shigella dysenteriae
Non-lactose fermenting
Resistant to bile salts
General Characteristics of Shigella
Слайд 24
Shigellosis = Generic term for disease
Low infectious dose (102-104 CFU)
Humans are
Transmission by fecal-oral route
Incubation period = 1-3 days
Watery diarrhea with fever; changing to dysentery
Major cause of bacillary dysentery (severe 2nd stage) in pediatric age group (1-10 yrs) via fecal-oral route
Outbreaks in daycare centers, nurseries, institutions
Estimated 15% of pediatric diarrhea in U.S.
Leading cause of infant diarrhea and mortality (death) in developing countries
Epidemiology and Clinical Syndromes of Shigella
Слайд 25DEFINITIONS
Enterotoxin = an exotoxin with enteric activity, i.e., affects the intestinal
Dysentery = inflammation of intestines (especially the colon (colitis) of the large intestine) with accompanying severe abdominal cramps, tenesmus (straining to defecate), and frequent, low-volume stools containing blood, mucus, and fecal leukocytes (PMN’s)
Bacillary dysentery = dysentery caused by bacterial infection with invasion of host cells/tissues and/or production of exotoxins
Слайд 27Shigellosis
Two-stage disease:
Early stage:
Watery diarrhea attributed to the enterotoxic activity
Fever attributed to neurotoxic activity of toxin
Second stage:
Adherence to and tissue invasion of large intestine with typical symptoms of dysentery
Cytotoxic activity of Shiga toxin increases severity
Pathogenesis of Shigella
Слайд 28Pathogenesis and Virulence Factors (cont.)
Virulence attributable to:
Invasiveness
Attachment (adherence) and
Large multi-gene virulence plasmid regulated by multiple chromosomal genes
Exotoxin (Shiga toxin)
Intracellular survival & multiplication
Слайд 29Penetrate through mucosal surface of colon (colonic mucosa) and invade and
Preferentially attach to and invade into M cells in Peyer’s patches (lymphoid tissue, i.e., lymphatic system) of small intestine
Invasiveness in Shigella-Associated Dysentery
Pathogenesis and Virulence Factors (cont.)
Слайд 30M cells typically transport foreign antigens from the intestine to underlying
Note: This contrasts with Salmonella which multiplies in the phagocytic vacuole
Actin filaments propel the bacteria through the cytoplasm and into adjacent epithelial cells with cell-to-cell passage, thereby effectively avoiding antibody-mediated humoral immunity (similar to Listeria monocytogenes)
Pathogenesis and Virulence Factors (cont.)
Invasiveness in Shigella-Associated Dysentery(cont.)
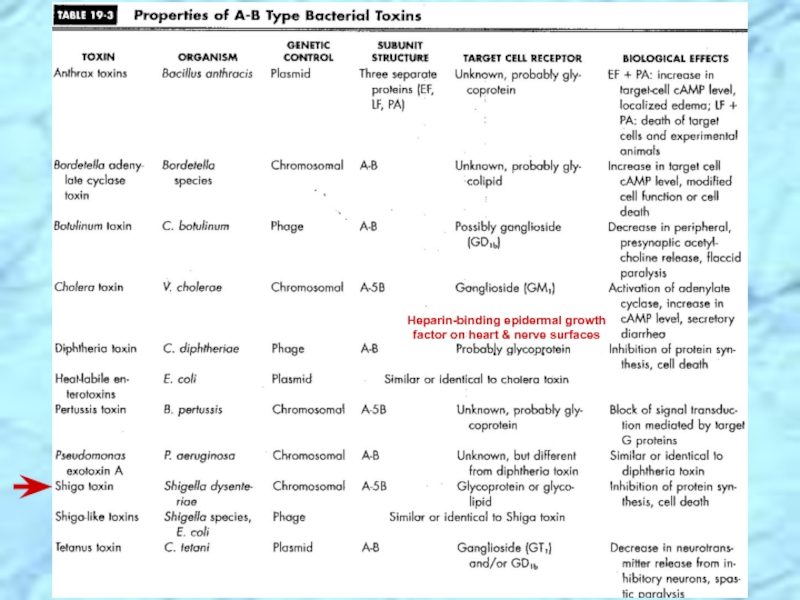
Слайд 33Enterotoxic, neurotoxic and cytotoxic
Encoded by chromosomal genes
Two domain (A-5B) structure
Similar to
NOTE: except that Shiga-like toxin is encoded by lysogenic bacteriophage
Pathogenesis and Virulence Factors (cont.)
Characteristics of Shiga Toxin
Слайд 34Shiga Toxin Effects in Shigellosis
Enterotoxic Effect:
Adheres to small intestine receptors
Blocks
Note: This contrasts with the effects of cholera toxin (Vibrio cholerae) and labile toxin (LT) of enterotoxigenic E. coli (ETEC) which act by blocking absorption of Na+, but also cause hypersecretion of water and ions of Cl-, K+ (low potassium = hypokalemia), and HCO3- (loss of bicarbonate buffering capacity leads to metabolic acidosis) out of the intestine and into the lumen
Pathogenesis and Virulence Factors (cont.)
Слайд 35Cytotoxic Effect:
B subunit of Shiga toxin binds host cell glycolipid
A
Causes irreversible inactivation of the 60S ribosomal subunit, thereby causing:
Inhibition of protein synthesis
Cell death
Microvasculature damage to the intestine
Hemorrhage (blood & fecal leukocytes in stool)
Neurotoxic Effect: Fever, abdominal cramping are
considered signs of neurotoxicity
Shiga Toxin Effects in Shigellosis (cont.)
Pathogenesis and Virulence Factors (cont.)
Слайд 38Yersinia pestis
Clinical Forms of Plague (a.k.a., Black Death):
Bubonic plague with swollen
Transmitted from mammalian reservoirs by flea (arthropod) bites or contact with contaminated animal tissues
Pneumonic plaque
Person-to-person spread
Yersinia enterocolitica
Enterocolitis
Transfusion-related septicemia
Summary of Yersinia Infections
Слайд 39Epidemiology and History of Plague
Zoonotic infection; Humans are accidental hosts
Outbreaks are
Plague recorded more than 2000 years ago
Three pandemics
1st 542AD; 100million dead in 60 years; from N.Africa
2nd 14th century; Black Death; 25million dead in Europe alone (>1/4 of entire population); from central Asia; disease became endemic in urban rat population and smaller epidemics occurred through 17th century
3rd ended in 1990s; Burma to China (1894) & Hong Kong to other continents including N. America via rat-infected ships; 20million dead in India alone; foci of infection firmly established in wild rodents in rural areas
Folk stories & nursery rhymes: Pied Piper of Hamelin (Ring Around the Rosie is “urban myth”??)
Слайд 41Epidemiological Cycles of Plague
Sylvatic (wild) Cycle of Plague
Reservoir (foci) = wild
Vector = wild rodent flea
Urban (domestic) Cycle of Plague
Reservoir = domestic (urban) black rat
Over 8 million in NYC = human population
Vector = oriental rat flea (Xenopsylla cheopis)
Human Cycle of Plague
Bubonic plague acquired from contact with either sylvatic or urban reservoirs or arthropod vector bite and further transmitted in human population by spread of pneumonic plague
Слайд 45Arthropod-Borne Transmission of Plague
Fleas required for perpetuation of plague vary greatly
Organisms ingested during blood meal from bacteremic host
Coagulase of flea may cause fibrin clot of organism in stomach which fixes to spines of proventriculus (throat parts of flea)
Organisms multiply causing blockage
Flea regurgitates infectious material into new host during subsequent attempts at blood meal
Flea remains hungry & feeds more aggressively
Sudden eradication of rats could lead to outbreak
Слайд 53Clinical Syndromes of Salmonella
Salmonellosis = Generic term for disease
Clinical Syndromes
Enteritis
Enteric fever (prototype is typhoid fever and less severe paratyphoid fever)
Septicemia (particularly S. choleraesuis, S. typhi, and S. paratyphi)
Asymptomatic carriage (gall bladder is the reservoir for Salmonella typhi)
REVIEW
Слайд 54Epidemiology and Clinical Syndromes of Salmonella (cont.)
Enteritis
Most common form
High infectious dose (108 CFU)
Poultry, eggs, etc. are sources of infection
6-48h incubation period
Nausea, vomiting, nonbloody diarrhea, fever, cramps, myalgia and headache common
S. enteritidis bioserotypes (e.g., S. typhimurium)
REVIEW
Слайд 55Virulence attributable to:
Invasiveness
Intracellular survival & multiplication
Endotoxin
Exotoxins: Effects
Several Salmonella serotypes produce enterotoxins similar to both the heat-labile (LT) and heat-stable enterotoxins (ST), but their effect has not been identified
A distinct cytotoxin is also produced and may be involved in invasion and cell destruction
Pathogenesis of Salmonella
Enteritis (cont.)
REVIEW
Слайд 56Clinical Progression of Salmonella Enteritis
Lamina propria = thin membrane between epithelium
Hyperplasia = abnormal increase in # of normal cells
Hypertrophy = abnormal increase in normal tissue/organ size
Prostaglandins = potent mediators of diverse set of physiologic processes
REVIEW
Слайд 57Clinical Progression of Enteric Fever (Typhoid fever)
Lumen (intraluminal);
RES = sum total of strongly phagocytic cells; primarily found in lymph nodes, blood, liver, spleen and bone marrow
Hyperplastic changes = see hyperplasia above - Clinical Progression of Enteritis
REVIEW
Слайд 61
Shigellosis = Generic term for disease
Low infectious dose (102-104 CFU)
Humans are
Transmission by fecal-oral route
Incubation period = 1-3 days
Watery diarrhea with fever; changing to dysentery
Major cause of bacillary dysentery (severe 2nd stage) in pediatric age group (1-10 yrs) via fecal-oral route
Outbreaks in daycare centers, nurseries, institutions
Estimated 15% of pediatric diarrhea in U.S.
Leading cause of infant diarrhea and mortality (death) in developing countries
Epidemiology and Clinical Syndromes of Shigella
REVIEW
Слайд 62DEFINITIONS
Enterotoxin = an exotoxin with enteric activity, i.e., affects the intestinal
Dysentery = inflammation of intestines (especially the colon (colitis) of the large intestine) with accompanying severe abdominal cramps, tenesmus (straining to defecate), and frequent, low-volume stools containing blood, mucus, and fecal leukocytes (PMN’s)
Bacillary dysentery = dysentery caused by bacterial infection with invasion of host cells/tissues and/or production of exotoxins
REVIEW
Слайд 63Shigellosis
Two-stage disease:
Early stage:
Watery diarrhea attributed to the enterotoxic activity
Fever attributed to neurotoxic activity of toxin
Second stage:
Adherence to and tissue invasion of large intestine with typical symptoms of dysentery
Cytotoxic activity of Shiga toxin increases severity
Pathogenesis of Shigella
REVIEW
Слайд 64Pathogenesis and Virulence Factors (cont.)
Virulence attributable to:
Invasiveness
Attachment (adherence) and
Large multi-gene virulence plasmid regulated by multiple chromosomal genes
Exotoxin (Shiga toxin)
Intracellular survival & multiplication
REVIEW
Слайд 65Enterotoxic, neurotoxic and cytotoxic
Encoded by chromosomal genes
Two domain (A-5B) structure
Similar to
NOTE: except that Shiga-like toxin is encoded by lysogenic bacteriophage
Pathogenesis and Virulence Factors (cont.)
Characteristics of Shiga Toxin
REVIEW
Слайд 69Yersinia pestis
Clinical Forms of Plague (a.k.a., Black Death):
Bubonic plague with swollen
Transmitted from mammalian reservoirs by flea (arthropod) bites or contact with contaminated animal tissues
Pneumonic plaque
Person-to-person spread
Yersinia enterocolitica
Enterocolitis
Transfusion-related septicemia
Summary of Yersinia Infections
REVIEW
Слайд 70Epidemiology and History of Plague
Zoonotic infection; Humans are accidental hosts
Outbreaks are
Plague recorded more than 2000 years ago
Three pandemics
1st 542AD; 100million dead in 60 years; from N.Africa
2nd 14th century; Black Death; 25million dead in Europe alone (>1/4 of entire population); from central Asia; disease became endemic in urban rat population and smaller epidemics occurred through 17th century
3rd ended in 1990s; Burma to China (1894) & Hong Kong to other continents including N. America via rat-infected ships; 20million dead in India alone; foci of infection firmly established in wild rodents in rural areas
Folk stories & nursery rhymes: Pied Piper of Hamelin (Ring Around the Rosie is “urban myth”??)
REVIEW
Слайд 71Epidemiological Cycles of Plague
Sylvatic (wild) Cycle of Plague
Reservoir (foci) = wild
Vector = wild rodent flea
Urban (domestic) Cycle of Plague
Reservoir = domestic (urban) black rat
Over 8 million in NYC = human population
Vector = oriental rat flea (Xenopsylla cheopis)
Human Cycle of Plague
Bubonic plague acquired from contact with either sylvatic or urban reservoirs or arthropod vector bite and further transmitted in human population by spread of pneumonic plague
REVIEW